Abstract
Introduction: Parents’ needs of support following the loss of a child to cancer and whether these needs are met are not fully known. This study aimed to describe parents’ needs, opportunity, and benefit of support from healthcare professionals and significant others from shortly after, up to five years after bereavement.
Material and methods: Data were collected at nine months (T5, n = 20), eighteen months (T6, n = 37), and five years after the child’s death (T7, n = 38). Parents answered questions via telephone about need, opportunity, and benefit of talking to psychologists, social workers, partners, and friends. Needs were examined in relation to parent and child characteristics, including sex, age, and parent posttraumatic stress symptoms (PTSS).
Results: The proportion reporting a need of support from psychologists varied from 56% and 46% at T5 to 20% and 6% at T7 (mothers and fathers, respectively). All mothers and 90% of fathers reported a need of support from social workers at T5. At T7, the corresponding percentages were 30% and 6%. More mothers than fathers reported a need of support from friends at T7 (p = .001). The proportion reporting a need of support from psychologists, social workers, and friends decreased over time (all p ≤ .050). Parents reporting a higher level of PTSS were more likely to report a need of support from social workers at T6 (p = .040) and from psychologists (p = .011) and social workers (p = .012) at T7. Opportunities for support from healthcare professionals varied, most reported need of and opportunity for support from significant others. Almost all reported benefit from received support.
Conclusion: Bereaved parents need and benefit of support from healthcare professionals and significant others. Results show a need for improved access to psychosocial services, even at five years post bereavement. Large-scale studies are needed to better understand the associations between parent and child characteristics and support needs.
Introduction
In Sweden, about one fifth of parents of children diagnosed with cancer will experience the death of their child to cancer [Citation1]. Losing a child is one of the most terrifying and overwhelming experiences for a parent. Research has shown that cancer-bereaved parents are at risk for psychological distress, including anxiety, depression, post-traumatic stress, prolonged grief, and separation distress [Citation2–5]. In addition, the death of a child is associated with an increased use of psychotropic medication among parents [Citation6,Citation7].
Psychosocial guidelines in childhood cancer recommend standardised psychosocial and financial risk assessments and referrals across the disease trajectory into survivorship or bereavement [Citation8,Citation9]. The literature in paediatric cancer settings has shown that support from psychologists and social support during the child’s end-of life period can promote better long-term adjustment among parents [Citation4,Citation10,Citation11]. Furthermore, essential components of parents’ successful psychosocial adaptation after a child’s death involves access to healthcare services after death [Citation11–13]. An American multicentre, cross-sectional study examining the use of bereavement mental health service shows that parents need, want, and often access such services [Citation14]. Having a supportive partner and social network (including friends and relatives) is important for bereavement adjustment [Citation13,Citation15]. It is however important to note that one’s partner may cope with the grief differently, which for some couples can be problematic. Research shows that partner relationships can either be strengthened or deteriorate following a child’s death [Citation13,Citation15], with a partner being as a source of support and stability or a source of distress.
We have shown that a substantial subgroup of Swedish parents of children undergoing cancer treatment reports a need to talk to psychologists, but few get the opportunity to do so [Citation16]. We have also reported that only a subgroup of those who report such a need after the end of successful treatment receives support [Citation17]. There is little research on parents’ perceptions of support following the loss of a child to cancer as well as on the potential association between needs of support and emotional distress. In addition, most previous studies on cancer-bereaved parents have had a retrospective and/or cross-sectional design [Citation3]. In Sweden, there is no formal model of psychosocial care following the loss of a child to cancer. Parents are usually provided the opportunity to talk to a social worker directly following the child’s death but are thereafter directed to primary care for psychosocial support. Services from a psychologist are rarely provided. Traditionally in Sweden, psychologists provide psychological support whereas social workers provide services related to social and practical (e.g., financial) aspects. Still, professional responsibilities and structures of support provided vary between the Swedish childhood cancer centres. Taken together there is a need of improved evidence on parents’ needs after bereavement to guide the development of bereavement support programmes [Citation10,Citation18]. The present study sought to add to the body of knowledge by describing parents’ need, opportunity, and benefit of support from both healthcare professionals and significant others. Support needs were studied from shortly after, up to five years after, the loss of a child to cancer. The following research questions (RQs) were posed:
How many parents report a need, an opportunity if a need, and benefit if an opportunity, to talk to psychologists, social workers, partners, and friends, respectively?
Is there a difference with regard to the proportion of mothers and fathers who report a need, an opportunity if a need, and benefit if an opportunity, to talk to psychologists, social workers, partners, and friends, respectively?
Is there a difference between parental and child characteristics and parents’ self-reported posttraumatic stress with regard to the proportion of parents who report a need, an opportunity if a need, and benefit if an opportunity, to talk to psychologists, social workers, partners, and friends, respectively?
Is there a change over time with regard to the proportion of parents who report a need to talk to psychologists, social workers, partners, and friends, respectively?
Methods
Participants and procedure
This study is part of a Swedish longitudinal project investigating psychological and economic consequences of childhood cancer for parents. The project covers seven assessments from shortly after diagnosis to five years after end of treatment or child’s death. The present study is based on data from bereaved parents collected at nine months (T5), eighteen months (T6), and five years (T7) after the child’s death.
Parents (including step-parents) of children diagnosed with cancer were consecutively recruited shortly after the child’s diagnosis during an 18-month period between 2002 and 2004, with assessments at T7 until 2013. Children were treated at four Swedish paediatric oncology units and parents were included via each unit according to the following criteria: Swedish and/or English-speaking parent of a child (0-18 years at study-start), with a primary cancer diagnosis (≤14 days), scheduled for chemotherapy and/or radiotherapy (this criterion was not applied to parents of children diagnosed with a CNS tumour), and with access to a telephone. Eligible parents were provided with written and oral information about the study by a nurse at the respective unit within two weeks after the child’s diagnosis. The same nurse asked parents for oral informed consent to participate and permission to be contacted by telephone. At T1, 259 parents of 139 children participated. Data on parents’ need of support during treatment (T1–T3) and after end of successful treatment (T4-T7) have been reported [Citation16,Citation17]. Data collected among bereaved parents (T5–T7) are reported herein.
A research assistant and a PhD student collected data via telephone. They had no contact with the participants besides performing the interviews. Permission to contact the parent at the next data collection was acquired at the end of each interview. Child’s medical data was collected from medical charts in order to update the research team before each interview. See previous reports from the longitudinal study for detailed information about the study sample and study procedure [Citation5,Citation16].
Ethical approval was obtained by local ethical committees and the Regional Ethical Review Board in Uppsala.
Measures
Sociodemographic variables
Information on parents’ age, civil status, and work status, and children’s age and gender were obtained via telephone. Information on parents’ education level and age were collected at T1 only.
Support needs
Parents were asked via telephone about their need of, opportunity to, and benefit from talking with: psychologists, social workers, partners, and friends. For each source of support a first question identified parents’ need to talk about the child’s disease: How great need have you had to talk about your child’s disease with psychologists/social workers/partners/friends during the past month? The second question identified parents’ opportunity to talk about the child’s disease: How often have you had an opportunity to talk about your child’s disease with psychologists/social workers/partners/friends during the past month? The third question identified benefit from talking about the child’s disease: How much have you benefited from talking about your child’s disease with psychologists/social workers/partners/friends during the past month? The questions were answered on 5-point-response scales ranging from none/never (1) to very great/very often (5).
Posttraumatic stress
Posttraumatic stress symptoms (PTSS) was measured using the PTSD Checklist Civilian Version (PCL-C) [Citation19]. The PCL-C is a self-report measure that consists of 17 items corresponding to the B (re-experiencing), C (avoidance/numbing), and D (hyper-arousal) criteria for PTSD in the DSM-IV. Items are scored on a 5-point scale, ranging from 1 (not at all) to 5 (extremely) and designed to indicate how much the respondent has been bothered by each symptom during the last month. PTSS was assessed on a continuum, using the total score. The PCL-C has shown good test–retest reliability and convergent validity in trauma-exposed populations [Citation20] as well as among nonclinical samples [Citation21].
Statistical analysis
To allow comparability to previous reports of support needs among parents of children on treatment and off successful treatment [Citation16,Citation17], the 5-point-response scales were comprised to dichotomous variables: 1 = no/2–5 = yes. If a need was reported a score for opportunity was calculated, and if an opportunity was reported, a score for benefit was calculated. Some reported having had an opportunity for support, however expressed that they had not taken the opportunity. Their answers regarding benefit were not included in the analysis for benefit. Descriptive statistics were used to report the number reporting a need, an opportunity, and a benefit of support (from psychologists, social workers, partners, and friends) at T5-T7 (RQ 1).
Chi-square tests were used to examine differences with regard to: a) the proportion of mothers vs. fathers reporting a need, an opportunity, and benefit of support at the respective assessment (RQ 2); and b) the proportion of parents with different characteristics including child characteristics (parents: age, work, education, civil status, children: gender, age) reporting a need, an opportunity, and benefit of support at the respective assessments (RQ 3). Fisher's exact tests were used when the expected values were less than 5. Parents’ level of PTSS was measured as a continuous variable and for that reason we conducted univariate logistic regression models to examine associations between level of PTSS and reported need, opportunity, and benefit of support at the respective assessment. Variables with p ≤ .05 in bivariate analysis were entered into a multivariable model.
Cochran’s Q tests were conducted to investigate differences over time (T5–T7) with regard to the proportion reporting a need of support (RQ 4). The time-trend analyses were based on data from the subset of parents bereaved at T5 and who participated at all three assessments, conducted both on data from mothers and fathers as well as data for mothers and fathers respectively. McNemar tests were used for post-hoc analyses.
The significance level was set at p ≤ .05. Data was analysed using SPSS Statistics Version 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Sample characteristics
Consistent with the study design, the number of eligible and participating parents changed over the study period. In total, 48 parents lost their child during the course of the study. At T5, 24 parents were eligible. Fifteen parents lost their child between T5 and T6 (eligible for T6) and an additional nine lost their child between T6 and T7 (eligible for T7). The number of parents participating at the respective assessment was 20 at T5, 37 at T6, and 38 at T7. Of those participating at T5, one father participated only at T5, while 19 participated at all assessments (T5-T7). Study sample characteristics at T5-T7 respectively are presented in .
Table 1. Study sample characteristics at T5–T7, respectively.
Need, opportunity, and benefit of support
The proportion of parents reporting a need, opportunity if a need, and benefit of support from psychologists, social workers, partners, and friends at T5-T7 is presented in . The numbers presented in are based on all participating parents at each assessment point.
Figure 1. The proportion of bereaved mothers and fathers reporting a need, an opportunity, and a benefit of support from healthcare professionals and significant others at T5 (n = 20), T6 (n = 37) and T7 (n = 38). All respondent groups reported benefit of support from significant others at T5–T7.
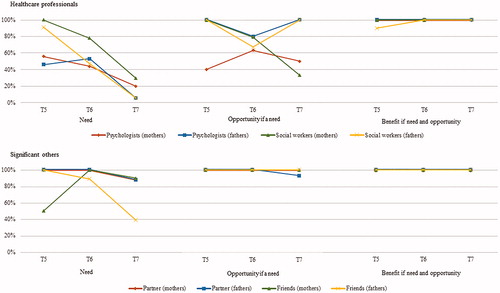
At T5, 56% of mothers and 46% of fathers reported a need of support from psychologists. The corresponding percentages at T7 were 20% and 6%, respectively. At T5, all mothers and 90% of fathers reported a need of support from social workers. At T7, the corresponding percentages were 30% and 6%, respectively. All mothers and fathers reported a need of support from their partner at T5 and T6. At T7, a need of support from partner was reported by 88% of mothers and fathers. At T5, all mothers and fathers reported a need of support from friends. At T6, all mothers and 89% of fathers reported a need of support from friends. The corresponding percentages at T7 were 90% and 39%, respectively.
Among those reporting a need of support from psychologist at T5, 40% of mothers and all fathers reported an opportunity of psychologist support. At T6, the corresponding percentages were 63% and 80%, respectively, and at the five-year follow-up (T7) 50% of mothers and all fathers reported an opportunity. All mothers and fathers reported an opportunity for support from social workers at T5. At T6, the corresponding percentages were 79% and 67%, respectively. At T7, 33% of mothers and all fathers reported an opportunity for support from social workers. With the exception of that 7% of fathers reported no opportunity for support from partner at T7, at all assessments, all mothers and fathers reported an opportunity of support from partners and friends.
With the exception of that 10% of fathers reported no benefit from the support from social workers at T5, all parents who reported an opportunity to talk to psychologists, social workers, partners, and/or friends at T5–T7 reported having benefited from doing so.
Support needs in relation to parental and child characteristics
At T7 more mothers (n = 18; 90% of mothers) than fathers (n = 7; 39% of fathers) reported a need of support from friends (χ2 = 10.996, p = .001).
Parents reporting a higher level of PTSS were more likely to report a need of support from social workers at T6 (OR = 1.065, 95% CI 1.003–1.131, p = .040), from psychologist at T7 (OR = 1.166, 95% CI 1.036–1.313, p = .011), and from social workers at T7 (OR = 1.123, 95% CI 1.026–1.229, p = .012). Supplementary Table 1 shows the odds ratios and 95% confidence intervals for the association between level of PTSS and need of support.
More parents of younger children (<7 years old at T1, n = 16; 76% of parents with younger children) than parents of older children (≥7 years old at T1 n = 7; 44% of parents with older children) reported a need of support from social workers at T6 (χ2 = 4.063, p = .044). Among parents with a need of support from social workers at T6, more parents of a boy (n = 12; 100%) reported an opportunity for support than parents of a girl (n = 5; 45%) (p = .005, Fisher's exact test).
The multivariable logistic regression model including parent level of PTSS and child age as predictors showed that none independently predicted need of support from social workers at T6.
Differences over time
Differences over time were calculated for the subset of parents who participated at all assessments (n = 19). presents the proportion of parents who reported a need of support from psychologists, social workers, partners, and friends at the respective assessment. Among these, a decreasing proportion reported a need of support from psychologists (Q(2) 6.0, p = .050), social workers (Q(2) 19.0, p<.001), and friends (Q(2) 13.00, p = .002) over time. McNemar tests showed a decrease between T5 and T6 for need of support from social workers (p = .004) and a decrease between T6 and T7 for support from friends (p = .031).
Table 2. The proportion of mothers (n = 9) and fathers (n = 10) who participated at all three assessments and who reported a need of support from psychologists, social workers, partners, and friends at T5–T7, respectively.
Separate analyses for mothers (n = 9) and fathers (n = 10) showed that a decreasing proportion of fathers reported a need of support from psychologists (Q(2) 8.0, p = .018), social workers (Q(2) 14.9, p = .001), and friends (Q(2) 13.0, p = .002) over time. McNemar tests showed a decrease between T5 and T6 for need of support from social workers (p = .016) and a decrease between T6 and T7 for support from friends (p = .031).
Discussion
This study extends knowledge on parental bereavement support needs shortly after, up to five years after, the loss of a child to cancer. Results show that the absolute majority of parents reports a need of support from healthcare professionals and significant others after bereavement. The proportion expressing a need of support from psychologist, social workers, and friends decreased over time. The proportion who reported having had an opportunity of support from healthcare professionals varied, whereas support from significant others was available to almost everyone over the study period. The proportion reporting a need of support did not differ between mothers and fathers, with the exception of more mothers than fathers reporting a need of support from friends five years after the child’s death. Parents’ level of PTSS was associated with needs of support from healthcare professionals, with parents reporting a higher level of PTSS being more likely to report a need of support from healthcare professionals at eighteen months and five years after bereavement. More parents of younger children reported a need of support from social workers five years after a child’s death and more parents of boys reported an opportunity for support from social workers at eighteen months after the loss.
Previous reports from this longitudinal project indicate a long-term impact on bereaved parents not reported elsewhere: (i) the number of mothers reporting partial PTSD decreased between eighteen months and five years after death, whereas it did not for fathers [Citation5]; (ii) five years after death almost all mothers, whereas 63% of fathers, were able to report something positive regarding the child’s disease [Citation22]; (iii) the number of mothers reporting sick leave decreased between eighteen months and five years after death, whereas there was an opposite trend for fathers [Citation23]. Although the findings must be interpreted carefully due to the small sample, they point to a need to further explore fathers’ distress and needs of support. Results of this study do not indicate differences in support needs between bereaved mothers and fathers, expect for that more mothers than fathers reported a need of support from friends at the five-year follow-up. This contrast results of our previous report of parental support after end of successful treatment in which a gender difference appeared [Citation17], showing that more mothers reported a long-term need of support from friends and psychologists. Still, descriptive outcomes of this study should be taken into consideration. While 6% of fathers reported a need of support from psychologist and social workers respectively five years after bereavement the corresponding numbers for mothers was 20% (support from psychologists) and 30% (support from social workers). Furthermore, while all fathers who reported a need to talk to psychologists nine months after bereavement reported an opportunity to do so, only two fifths of mothers who had a need reported having access to professional psychological support at that time. Also, at five years after bereavement only about one third of mothers reported the opportunity for support from social workers. These results did not denote statistically significant differences between mothers and fathers but can be important to address in future studies with larger sample sizes.
Importantly, all parents who reported a need of support from social workers expressed that they had such opportunity nine months after bereavement. Moreover, parents reported that they had opportunities for support from friends and partners over the study period. An additional important finding of this study is that almost all parents perceived received support from healthcare professionals and significant others as beneficial. However, consistent with a previous American study on unmet needs of mental health services [Citation14], a substantial proportion of mothers reported unmet needs of support from healthcare professionals. This implies that there is room for improvements in regards to psychosocial care. The shown benefits of accessible bereavement care services on parents’ psychosocial adaptation [Citation11–13] should encourage further efforts to develop relevant and accessible bereavement services for parents. Furthermore, as evaluated parental grief interventions have shown no or only modest effect [Citation10,Citation18], models of assessment and delivery of psychosocial support are important targets for future studies. Previous findings from our group suggest that online psychological support can be effective in reducing depression, anxiety, and PTSS among parents of children on cancer treatment who report an increased level of PTSS [Citation24]. Moreover, an Australian study has shown promising results in terms of feasibility and acceptability for an online group-based psychological intervention for parents of survivors of childhood cancer [Citation25]. We have furthermore developed an internet-administered guided, CBT-based self-help intervention for parents whose children have ended successful treatment, which is currently tested in terms of feasibility [Citation26,Citation27]. Should the intervention be demonstrated to be clinically and cost-effective (or at least cost-neutral), the same intervention development process will be used for the development of an intervention for bereaved parents. Still, further investigation is encouraged to determine if the internet is a viable option to provide psychological support interventions for cancer-bereaved parents.
The longitudinal design of this study allows us to examine how perceived needs change from close to bereavement to five years after. The proportion of parents reporting needs of support from healthcare professionals and friends decreased with time since bereavement. However, the proportion reporting a need of support from partners did not change over the study period. The decrease in the proportion of parents reporting a need of support from healthcare professionals may be related to grief adjustment [Citation9], and suggests that some parents can rely solely on social support from friends and partners when years have passed since time of loss. Then again, our results show that a substantial subgroup of mothers reports a need of support from healthcare professionals still five years after bereavement. Previous studies have shown that having access to professional and social support is important for the successful psychosocial adaptation following bereavement [Citation2,Citation12,Citation13,Citation15], and our results point to the need of having psychosocial resources accessible even in the longer term. Study results furthermore show that, at the later assessment points, parents reporting a higher level of PTSS were more likely to report a need of support from healthcare professionals. To alleviate long-term psychological distress and promote healthy adaptation after bereavement it is key that necessary psychosocial services are easily accessible.
We have successfully included fathers in our research. However, fathers are under-represented in the wider literature. This circumstance together with the fact that masculinity and care is under-researched [Citation28] and recent findings [Citation29] suggesting an impact of gender roles on fathers’ experiences of parenting a child with cancer point to the importance of examining experiences of fathers. In this smaller-scale study, only one statistically significant difference was found between mothers’ and fathers’ perceived needs of support. Taken together, this indicates a need for large-scale studies that further examine fathers’ experiences of distress and needs of support when a child is diagnosed with cancer. Further large-scale studies are moreover necessary to understand the findings regarding the relationship between perceived support from social workers and the child’s sex and age, respectively. It should however be mentioned that studying cancer-related bereavement outcomes in parents is challenging. Thanks to treatment advances, the number of children dying from cancer is falling and this makes the evaluable population of bereaved parents comparatively small. Despite being a multi-site prospective study with a consecutive recruitment of participants over a relatively long period of time the study is limited by its small sample size, which has implications on the power of the tests. Indeed, the results of the multivariable model indicates that our sample size was too small for such analysis. Still, this study provides important understanding of the prevalence of support needs among bereaved parents and identify areas of improvements for bereavement support.
Conclusions
Parents who have lost a child to cancer are in need of support from healthcare professionals and/or significant others. Almost all reported that the support received had been beneficial. Although the proportion of parents who had a need of support from healthcare professionals declined over time, a substantial subgroup reported a need of such support eighteen months and even five years after bereavement. The need of support from psychologists and social workers was at these time points more likely to be reported by parents reporting a high level of PTSS. The substantial proportion of parents who reported unmet support needs from healthcare professionals shows that bereavement support services could be improved in Sweden. Standardised psychosocial of bereavement support care practises and follow-up services should build on existing evidence and correspond to existing standards of psychosocial care [Citation9,Citation30]. Our results show that the access to professional support services needs to increase and be available also when several years have passed since the child’s death.
Supplemental Material
Download MS Word (17.9 KB)Acknowledgements
The authors would like to thank all study participants, the coordinating nurses at the paediatric oncology centres, Susanne Lorenz for performing the interviews, and Professor Johan Lyhagen for statistical advice.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Gustafsson G, Kogner P, Heyman M. Childhood cancer incidence and survival in Sweden 1984-2010. Report from the Swedish Childhood Cancer Registry. Stockholm: Karolinska Institutet; 2013.
- Kreicbergs U, Valdimarsdottir U, Onelov E, et al. Anxiety and depression in parents 4-9 years after the loss of a child owing to a malignancy: a population-based follow-up. Psychol Med. 2004;34(8):1431–1441.
- Rosenberg AR, Baker KS, Syrjala K, et al. Systematic review of psychosocial morbidities among bereaved parents of children with cancer. Pediatr Blood Cancer. 2012;58(4):503–512.
- McCarthy MC, Clarke NE, Ting CL, et al. Prevalence and predictors of parental grief and depression after the death of a child from cancer. J Palliat Med. 2010;13(11):1321–1326.
- Ljungman L, Hovén E, Ljungman G, et al. Does time heal all wounds? A longitudinal study of the development of posttraumatic stress symptoms in parents of survivors of childhood cancer and bereaved parents. Psychooncology. 2015;24(12):1792–1798.
- Rostila M, Mäki N, Martikainen P. Does the death of a child influence parental use of psychotropic medication? A follow-up register study from Finland. PLoS One. 2018;13(5):e0195500.
- Salem H, Andersen EW, Dalton SO, et al. Psychotropic medication use in parents of children diagnosed with cancer. Pediatrics. 2019;143(5):e20182605.
- Pelletier W, Bona K. Assessment of financial burden as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(S5):S619–S631.
- Wiener L, Kazak AE, Noll RB, et al. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer. 2015;62(S5):S419–S424.
- Donovan LA, Wakefield CE, Russell V, et al. Hospital-based bereavement services following the death of a child: a mixed study review. Palliat Med. 2015;29(3):193–210.
- Kreicbergs UC, Lannen P, Onelov E, et al. Parental grief after losing a child to cancer: impact of professional and social support on long-term outcomes. J Clin Oncol. 2007;25(22):3307–3312.
- Dias N, Docherty S, Brandon D. Parental bereavement: looking beyond grief. Death Stud. 2017;41(5):318–327.
- Stevenson M, Achille M, Liben S, et al. Understanding how bereaved parents cope with their grief to inform the services provided to them. Qual Health Res. 2017;27(5):649–664.
- Lichtenthal WG, Corner GW, Sweeney CR, et al. Mental health services for parents who lost a child to cancer: if we build them, will they come? J Clin Oncol. 2015;33(20):2246–2253.
- Barrera M, O'Connor K, D'Agostino NM, et al. Early parental adjustment and bereavement after childhood cancer death. Death Stud. 2009;33(6):497–520.
- Pöder U, von Essen L. Perceptions of support among Swedish parents of children on cancer treatment: a prospective, longitudinal study. Eur J Cancer Care (Engl). 2009;18(4):350–357.
- Kukkola L, Hovén E, Cernvall M, et al. Perceptions of support among Swedish parents of children after end of successful cancer treatment: a prospective, longitudinal study. Acta Oncol. 2017;56(12):1705–1711.
- Mitchell M, Coombs M, Wetzig K. The provision of family-centred intensive care bereavement support in Australia and New Zealand: results of a cross sectional explorative descriptive survey. Aust Crit Care. 2017;30(3):139–144.
- Weathers FW, Litz BT, Herman DS, et al. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at the 9th Annual Conference of the ISTSS; San Antonio, TX, 1993.
- Adkins JW, Weathers FW, McDevitt-Murphy M, et al. Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. J Anxiety Disord. 2008;22(8):1393–1402.
- Conybeare D, Behar E, Solomon A, et al. The PTSD Checklist-Civilian Version: reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol. 2012;68(6):699–713.
- Ljungman L, Boger M, Ander M, et al. Impressions that last: particularly negative and positive experiences reported by parents five years after the end of a child's successful cancer treatment or death. PLoS One. 2016;11(6):e0157076.
- Wikman A, Hovén E, Cernvall M, et al. Parents of children diagnosed with cancer: work situation and sick leave, a five-year post end-of-treatment or a child's death follow-up study. Acta Oncol. 2016;55(9-10):1152–1157.
- Cernvall M, Carlbring P, Wikman A, et al. Twelve-month follow-up of a randomized controlled trial of internet-based guided self-help for parents of children on cancer treatment. J Med Internet Res. 2017;19(7):e273.
- Wakefield CE, Sansom-Daly UM, McGill BC, et al. Acceptability and feasibility of an e-mental health intervention for parents of childhood cancer survivors: “Cascade”. Support Care Cancer. 2016;24(6):2685–2694.
- Wikman A, Kukkola L, Börjesson H, et al. Development of an internet-administered cognitive behavior therapy program (ENGAGE) for parents of children previously treated for cancer: participatory action research approach. J Med Internet Res. 2018;20(4):e133.
- Woodford J, Wikman A, Cernvall M, et al. Study protocol for a feasibility study of an internet-administered, guided, CBT-based, self-help intervention (ENGAGE) for parents of children previously treated for cancer. BMJ Open. 2018;8(6):e023708.
- Hanlon N. Masculinities, care and equality: identity and nurture in men’s lives. Basingstoke: Palgrave MacMillan; 2012.
- Polita NB, Alvarenga WA, Leite A, et al. Care provided by the father to the child with cancer under the influence of masculinities: qualitative meta-synthesis. Rev Bras Enferm. 2018;71(1):185–194.
- Weaver MS, Heinze KE, Bell CJ, et al. Establishing psychosocial palliative care standards for children and adolescents with cancer and their families: an integrative review. Palliat Med. 2016; 30(3):212–223.
