Abstract
Background: Cervical cancer incidence in Sweden decreased from 24/100,000 in 1965 to 8/100,000 in 2011, but has from 2014 increased to 11/100,000. The increase appears to correlate to screening history. We perform a study of the cancer risk change in relation to screening history over two screening rounds to verify the correlation.
Material and methods: We studied the cohorts of all 3,047,850 individual women living in Sweden in each year from 2002–2015. Registry linkages between the Total Population Register, the Swedish National Cervical Screening Registry, the Swedish Cervical Cancer Audit database and the National Quality Register for Gynecological Cancer, defined the incidence rates of invasive cervical cancer comparing time periods 2002–2013 to 2014–2015, in women whose screening history in 2 screening intervals prior to each year were either (i) adequately screened with normal results (almost exclusively cytology, 52% of the population) or (ii) unscreened (13% of the population). We also investigated the incidence increase by time since a normal smear performed in 2002–2012.
Results: Among women adequately screened with normal results there was a strong incidence increase in 2014–2015 compared to previous years (Incidence rate ratio (IRR) = 1.59, 95%CI = 1.36–1.85), but no significant increase among unscreened women (IRR = 1.09, 95%CI = 0.94–1.27). There was no increase in incidence 0–2.5 years after a normal smear over the study period (IRR = 1.04, 95% CI = 0.88–1.24), but a strong increase 3–4 years after a normal smear since year 2009 (IRR = 1.52, 95% CI = 1.25–1.84).
Conclusion: The results suggest that the overall increase is associated with an increased cancer risk in women adequately screened with normal cytological results. Possibly, precursor lesions missed in one screening round might result in detection of early stage invasive cancer in the subsequent screening.
Introduction
Cervical screening prevents cancer by detecting and treating pre-cursor lesions. The incidence of invasive cervical cancer in Sweden decreased from 24/100,000 in 1965 to 8/100,000 in 2011. In 2010, cervical cancer incidence in Sweden was estimated to be only 35% of the projected incidence of a no screening scenario [Citation1]. However, from 2014 the incidence of cervical cancer in Sweden had an about 20% increase and is now 11/100,000 (Supplementary Figure 1), corresponding to approximately 100 extra annual new cases compared to the previous period [Citation2].
Our previous report indicated that the increase is mainly seen (i) in women aged below 65 (ii) in early FIGO stages (iii) only in some counties (laboratories) in Sweden and (iv) in women who have attended screening [Citation2]. These characteristics suggest that the increase may be associated more with cervical screening performance, rather than changes in overall risk factors such as HPV infection. Sweden has had an organised cervical screening programme since the 1960s, and current screening coverage is >80% in women aged 23–60 years [Citation3,Citation4]. The Swedish National Cervical Screening Registry (NKCx) conducts quality assurance of the cervical screening programme and has found a steadily improving screening coverage in recent years [Citation4,Citation5]. The unexpected incidence increase despite the non-inferior quality indicators of screening called for a detailed investigation.
To comprehensively investigate whether screening performance may be one of the reasons for the incidence increase, we examined cervical cancer incidence over 14 years in relation to screening history over two screening rounds for all women resident in Sweden, using individual-level registry linkages. A preliminary analysis over a single screening round was previously reported in Swedish [Citation2].
Material and methods
This study included the women aged between 29 and 65 who were resident in Sweden during 2002–2015. Total Population Register (TPR) [Citation6] was used to identify the age-eligible population living in Sweden in each year. Individual women’s screening history in the past two screening intervals prior to each calendar year were identified from the Swedish National Cervical Screening Registry (NKCx). NKCx records date and result of cervical screening tests performed in Sweden, reaching close to 100% coverage in entire country since 1995 [Citation7]. Diagnoses of invasive cervical cancer were retrieved from two sources: (1) in year 2002–2011 from the National Cervical Cancer Audit database, based on the National Cancer Registry (NCR) where all cases have undergone thorough clinical and pathological review [Citation8]; (2) in year 2012–2015 from the Swedish National Quality Register of Gynecological Cancer. The reason for using these databases is mainly that the cervical cancer diagnoses in the two databases have undergone rigorous reviews. The NCR contains data over the whole study period, but the cancer diagnoses are recorded at a more preliminary stage of the full diagnostic process and may be somewhat less accurate. Sensitivity analysis based on cervical cancers derived from NCR during the whole study period 2002–2015 was also performed to check whether the use of the rigorously reviewed data sources could affect the results. Individual-level data linkage was performed using the unique personal identification number each individual has in Sweden.
The study was built on multiple birth cohorts by calendar year. For each year from 2002–2015, women who lived in Sweden entered the cohort at the beginning of the year, and were followed until the diagnosis of invasive cervical cancer, emigration, death or end of the year whichever came first. Women in each year’s cohort were classified by screening history in the preceding two screening intervals. The length of recommended interval was based on age: 3 years for ages 23–50 and 5 years for ages 51–60, some counties invited women up to age 65. Therefore, two screening intervals were translated to six, eight or ten years for women aged 29–53, 54–58 and 59–65 at each study year respectively. For all cervical cancer cases, cervical tests within six months prior to cancer diagnosis was disregarded since they were diagnostic tests with no potential for cancer prevention. In the present study, women being adequately screened, i.e. being screened in both of the two intervals with only normal results (almost exclusively cytology, but including high-risk HPV negative results in primary screening, which for Sweden in the years under study was only present in a randomised implementation trial in Stockholm county launched in 2012 (Supplementary Table 1)), and women completely unscreened in any of the two intervals were included.
We present the proportion of women being adequately screened with normal results and women unscreened among total population by year from 2002–2015. We calculated yearly age-standardised incidence rates (IR) of invasive cervical cancer by the two screening history groups, standardised by the age distribution of the entire female population during 2002–2015. Incidence rate ratios (IRR) and 95% confidence interval (CI) of invasive cervical cancer comparing years 2014–2015 to 2002–2013 by the two screening history groups were estimated in Poisson regression models, adjusted for age group. In the sensitivity analysis, country of birth of women was also adjusted for. Among women adequately screened with normal results, we further estimated age-stratified IRs and IRRs. Furthermore, we plotted IR of cervical cancer over time following cytological normal screening results, by calendar year of the screening test in every two-year category. In the sensitivity analysis using NCR linked to comprehensive HPV vaccination registers [Citation9], we assessed the number of women being vaccinated and number of cervical cancer cases diagnosed after HPV vaccination during the study period, to investigate whether use of preventive vaccines could reasonably have affected our findings. Cervical screening is organised by 21 different regions in Sweden. Most regions have only a single laboratory, resulting in that effect of county and laboratory cannot be separated. We estimated IRRs by lab/county among women being adequately screened with normal results in supplementary analysis. In addition to IRR and CI for individual counties/labs, we also analysed whether the difference in IRRs across labs/counties is significant by testing the difference in model-fitting (likelihood-ratio test) between the models with and without the interaction term between lab and calendar year.
The Regional Ethics Committee in Stockholm, Sweden, granted ethical approval for this study and concluded that informed consent from the study subjects was not required.
Results
Study population
The study included 3,047,850 individual women. Number of women in each year’s cohort as well as number of women adequately screened and unscreened in the past two intervals, are presented in . The proportion of women adequately screened and unscreened in the population were generally stable over the study period. Among women adequately screened with normal results entering cohort 2014 and 2015, 99.5% and 98.8% were defined by cytology tests, respectively.
Table 1. Number of women and person-year of the study cohorts, in total and by screening history in the preceding two screening intervals.
Incidence rate over 2002–2015
Over the study period, the age-standardised incidence rate (ASIR) of invasive cervical cancer among women unscreened in the prior two screening intervals was as high as 30–40 per 100,000 person-years and fluctuated over time. No abrupt increase was observed from 2014 (). Whereas the ASIR in women adequately screened with normal results in the prior two intervals was relatively flat at around 6 per 100,000 person-years up to 2013 and strikingly increased to around 9 per 100,000 person-years in 2014-2015 ().
Figure 1. Age-standardised incidence rate of invasive cervical cancer 2002–2015 among women unscreened (a) and adequately screened (b) in the preceding two screening intervals.
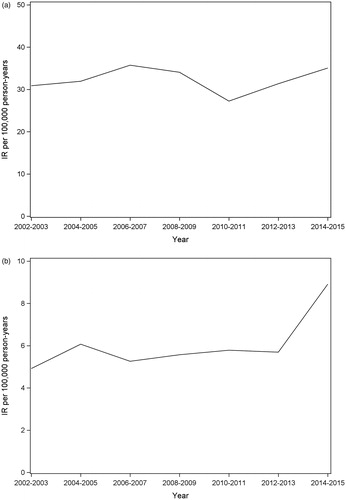
Among women adequately screened, the incidence in 2014–2015 was estimated to be 59% higher than the incidence in 2002–2013 after adjusting for age. This increase was statistically significant, while among women unscreened, there was no statistically significant increase in incidence comparing 2014–2015 to 2002–2013 (). The sensitivity analysis using cervical cancer cases derived from National Cancer Registry showed very similar results (Supplementary Table 2), and the sensitivity analysis adjusting for country of birth did not alter the estimates (Supplementary Table 2).
Table 2. Incidence rate ratio of invasive cervical cancer in 2014–2015 compared to 2002–2013, among women adequately screened with normal results and women unscreened in the preceding two screening intervals.
Among women adequately screened with normal results, the increase of incidence from 2014 was mainly observed and statistically significant at ages 29–39 and 40–49 years (). The increase tended to vary across the >20 labs/counties over Sweden. Some counties had no increase in incidence in women adequately screened whereas some counties had highly statistically significant increases (Supplementary Table 3). The overall difference in IRRs across labs/counties was not statistically significant (p = .246, including all counties with >5 expected cases of invasive cervical cancer in 2014–2015 among women being adequately screened (Supplementary Table 4)).
Incidence rate over time since normal screening results
The incidence of invasive cervical cancer in the following 0–2.5 years after a normal screening test was very low, but 3–4 years after a normal screen it was substantial and increasing, thus indicating the cancers detected through screening tests at the subsequent screening interval. The incidence 3–4 years after normal screening result was higher when the initial normal smears were taken in 2009–2012 compared to smears taken in 2002–2008 (), corresponding to a statistically significant 52% higher incidence ().
Figure 2. Incidence rate of invasive cervical cancer over year since a normal smear, by year of the smear.
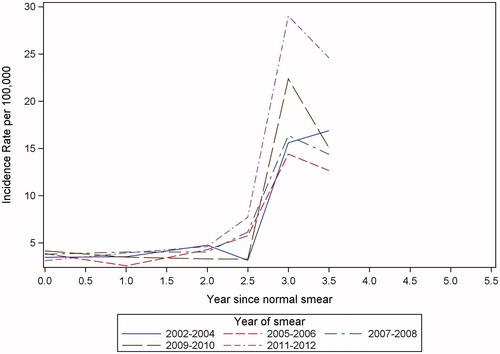
Table 3. Incidence rate ratio of invasive cervical cancer in different follow-up periods after a normal smear, comparing 2009–2012 to 2002–2008 at smear taken.
HPV vaccinations in the studied cohorts
The sensitivity analysis linking to HPV vaccination registers found that, <0.5% of women in the studied cohorts were HPV vaccinated. Among the 5615 vaccinated women entering cohorts 2014–2015, and the 3351 vaccinated women entering cohorts 2002–2013 who were adequately screened, only one woman had cervical cancer after the vaccination for each time period. Among unscreened women, no cervical cancer case was previously vaccinated.
Discussion
Main findings and interpretations
This study found that the increase of cervical cancer incidence in Sweden was particularly strong among women repeatedly screened with normal results, and not seen among unscreened women. The increased cancer risk in the next screening interval after a normal smear started with tests taken in 2009.
The reason behind the finding is most likely an insufficient detection of abnormalities in the cervical screening tests from 2009 and onwards. It is less likely to be mainly due to increased risk factors such as HPV infection in the population, because 1) the increase did not appear gradually but was rather steep since 2014; 2) no evident increase was observed among unscreened women 3) the increase in women adequately screened tended to vary across labs/counties (Sweden has regionalised medicine, where there is typically only one laboratory per county).
All labs in Sweden except one switched to liquid-based cytology (LBC) during 2008–2012. If this had resulted in an improved detection of prevalent cases, the incidence increase should have dropped down substantially after the 3-yearly screening interval. Instead, the higher incidence of cervical cancer has been maintained for 4 years according to the Swedish National Cancer Registry. Moreover, among labs/counties who have switched to LBC, some had increased incidence and some had not, and the only lab/county which did not switch to LBC also had a statistically significantly increased incidence in women adequately screened. However, because the switch to LBC largely overlapped with the two comparison periods, which are the studied exposure, it has not been possible to rule out an effect of LBC due to this extensive co-linearity.
The fact that the increase of cervical cancer was mainly on FIGO stage IA and IB [Citation2], which are often asymptomatic and usually detected in screening, goes hand in hand with the finding of increased cervical cancer in 3–4 years after a normal smear taken after 2009. They together imply that precursor lesions may have been missed in the recent ‘normal’ smears. In the subsequent screening round an early stage, asymptomatic invasive cervical cancer has then developed and was detected.
To verify whether reduced sensitivity of screening test is the underlying reason, a re-review of all normal smears in Sweden, taken up to 10 years preceding a cervical cancer diagnosis during 2008–2016 is ongoing. Preliminary results based on 23 out of the 28 labs in Sweden revealed a higher false negative rate in recent years.
Strengths and limitations
The strengths of this study included that it uses the full population and all cervical cancer cases of the entire country, which were individually linked to the complete national registry of cervical screening, as well as population data on migration and death. These ensured unbiased evaluation, and the registers provided data for a sufficient period of time for comparisons.
Limitation of the study is mainly the different sources of cervical cancer diagnoses before and after 2012. There is slight discrepancy in number of cases between the National Cancer Registry and the national quality register for gynecological cancer, but sensitivity analyses found that use of case definitions for either source did not alter our results.
Comparison with other studies
Several countries also reported increased incidence of cervical cancer in recent years. UK’s incidence increase is limited to very young ages and could be due to changes in screening policies or data reporting [Citation10]. Norway had an overall incidence increase, with a varied increase between regions. Denmark also showed regional differences, where North Jutland and Southern Denmark region exhibited increases, but no increases were seen in the capital region [Citation11]. As far as we are aware, no other countries have as yet compared the incidence increase in relation to screening history.
Other considerations
The Swedish government mandated switching to HPV-based screening in 2015. Although several counties introduced this in 2016–2017, large parts of Sweden have not yet introduced HPV-based screening. Given the increased cervical cancer incidence after a normal cytological screening, an increased emphasis on switching to HPV-based screening is a health priority. Nevertheless, as cytology is used for triaging of HPV-positive women in the HPV-based screening programme, an intensification of the surveillance of the quality of cytology when used for triaging HPV-positive women may be warranted.
Comprehensive records of HPV vaccination found that <0.5% of the women were HPV vaccinated before entering the cohorts and only 2 cases of cervical cancers were HPV vaccinated prior to their cancer diagnosis. Therefore, we can rule out that HPV vaccination has had any impact on the recent increase in cervical cancer in Sweden.
Conclusion
This study finds a profound increase of cervical cancer incidence among women adequately screened with normal cytology results in the preceding two screening intervals. Although formal evidence from a re-review is pending, the finding suggests that an insufficient detection of cervical precursor lesions in screening from 2009 and onwards may be a cause of the increased incidence of cervical cancer.
Supplemental Material
Download MS Word (179.6 KB)Disclosure statement
JD has formerly been recipient of grants to his institution for research on HPV vaccines from a manufacturer of such vaccines (Merck). The other authors report no conflicts of interest.
Additional information
Funding
References
- Vaccarella S, Franceschi S, Engholm G, et al. 50 years of screening in the Nordic countries: quantifying the effects on cervical cancer incidence. Br J Cancer. 2014;111(5):965–969.
- Dillner J, Sparén P, Andrae B, et al. Livmoderhalscancer ökar hos kvinnor med normalt cellprov. [cited 2019 Jan 16]. Available from: http://lakartidningen.se/Klinik-och-vetenskap/Rapport/2018/06/Livmoderhalscancer-okar-hos-kvinnor-med-normalt-cellprov/.
- Basu P, Ponti A, Anttila A, et al. Status of implementation and organization of cancer screening in The European Union Member States – summary results from the second European screening report. Int J Cancer. 2018;142(1):44–56.
- Elfström KM, Sparén P, Olausson P, et al. Registry-based assessment of the status of cervical screening in Sweden. J Med Screen. 2016;23(4):217–226.
- Hortlund M, Elfström KM, Sparén P, et al. Cervical cancer screening in Sweden 2014–2016. Plos One. 2018;13(12):e0209003.
- Ludvigsson JF, Almqvist C, Bonamy A-K, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–136.
- Nationellt Kvalitetsregister för Cervixcancerprevention (NKCx). [cited 2015 Jun 15]. Available from: http://www.nkcx.se/index_e.htm.
- Wang J, Elfström KM, Andrae B, et al. Cervical cancer case–control audit: Results from routine evaluation of a nationwide cervical screening program. Int J Cancer. 2020;146:1230–1240.
- Wang J, Ploner A, Sparén P, et al. Mode of HPV vaccination delivery and equity in vaccine uptake: a nationwide cohort study. Prev Med. 2019;120:26–33.
- Castanon A, Sasieni P. Is the recent increase in cervical cancer in women aged 20–24years in England a cause for concern? Prev Med. 2018;107:21–28.
- NORDCAN. [cited 2019 Jan 1]. Available from: http://www-dep.iarc.fr/NORDCAN/english/frame.asp.
