Abstract
Purpose: Epithelioid hemangioendothelioma (EHE) is an ultra-rare vascular sarcoma with unique clinical features. EHE is characterized by an unpredictable, often protracted, clinical course and highly variable clinical presentation. Due to difficulty recruiting ultra-rare cancer patients, health-related quality of life (HRQoL) of EHE patients has not yet been studied. The aim of this study was to assess EHE symptom burden and its impact on HRQoL and psychological distress.
Methods: The study was initiated after EHE patients’ foundations approached our research group to study HRQoL. Patients were recruited from the international EHE Facebook group from May through October 2018. Data were collected using the online PROFILES registry. Latent class cluster analysis was performed to identify groups based on frequently reported symptoms. Differences in HRQoL (EORTC-QLQ-C30) and psychological distress (Hospital Anxiety and Depression Scale) between symptom-based clusters were examined.
Results: Among 115 EHE patients from 20 countries, three clusters were identified, with low-, intermediate- and high-symptom burden, respectively. Highly symptomatic patients (33%) had clinically relevantly lower scores on HRQoL compared to the other two groups (p < 0.001). These patients suffered mostly from pain, insomnia and fatigue. Symptom burden significantly correlated with reduced daily functioning and high levels of psychological distress. Only for highly symptomatic patients, HRQoL and symptom levels were worse compared to healthy individuals.
Conclusion: For the first time, we studied HRQoL in a large international cohort of ultra-rare cancer patients with distinct clinical characteristics, enabled by collaboration with patients and use of social media. We showed a considerable number of EHE patients were highly symptomatic, with a significant impact on HRQoL and psychological distress.
Introduction
About 20–25% of all cancer patients are diagnosed with a rare cancer, which is defined by an incidence of less than 6–15 per 100.000 persons per year [Citation1]. Rare cancers can pose many challenges, such as difficulty in training clinicians to adequately recognize and treat these cancers. Performing research is complicated by the limited availability of funding, tumor material and low patient accrual in clinical trials.
Epithelioid hemangioendothelioma (EHE) is an ultra-rare type of vascular sarcoma, with an estimated incidence of ≤1/1.000.000 persons per year [Citation2]. EHE patients are not just confronted with a very rare disease and resulting difficulties in finding expert clinicians, but also face a notoriously unpredictable and highly variable disease course, ranging from indolent to quickly progressive disease. Although reported five-year relative survival of all EHE patients is about 70% [Citation2,Citation3], a recent study showed that patients with pleural disease or lymph node metastases had a more aggressive clinical course with only 22–30% 5-year survival [Citation4]. Other possible risk factors associated with poorer survival include increasing mitotic activity and larger tumor size [Citation5]. EHE can occur at all ages but is mostly diagnosed after the second decade of life [Citation2]. Although EHE lesions can arise virtually anywhere in the body, they often present in liver, lungs, bone, skin and extremities [Citation6]. Approximately 30–50% of patients are asymptomatic and in the few available studies, pain is the most prevalent symptom among symptomatic patients (68–74%) [Citation2,Citation3]. The level of symptom burden per patient has not yet been studied.
EHE treatment is dependent on the localization, extent and clinical course of the disease and can consist of watchful waiting, localized treatment or systemic therapy [Citation7–9]. In case of uni- or multifocal disease limited to the liver, transplantation surgery with curative intent can be considered [Citation10]. As for systemic treatment, there is no standard regimen but patients can be treated with paclitaxel, doxorubicin, tyrosine kinase inhibitors, sirolimus or celecoxib [Citation11,Citation12].
The rarity, heterogeneity and unpredictable course of EHE not only result in uncertainty regarding treatment choices, but also in paucity of adequate supportive care for patients. To meet their need for support, EHE patients from across the world have connected through a closed community on social media platform Facebook. Within this Facebook group EHE patients and family members share knowledge and personal experiences reflecting the impact of EHE on daily life.
To date, the impact of EHE on daily life and health-related quality of life (HRQoL) has not yet been studied. To investigate this in the underexposed very rare sarcoma population, a representative of the EHE community approached us to initiate a study within their Facebook group. As EHE is known to have a highly variable clinical course with varying intensity of symptoms, we aimed to study HRQoL and psychological distress in relation to symptom burden. In addition, we intended to test the feasibility of a unique research method using a patient Facebook group to perform a global web-based HRQoL study in an ultra-rare cancer.
Methods
Setting and population
This cross-sectional study was initiated upon request of the EHE patient community. Based on input from EHE patients, EHE foundation members, clinician experts and HRQoL researchers, an HRQoL questionnaire was assembled. EHE patients (age ≥ 18 years) were invited to participate through posts in the Facebook group by one of the researchers (MW). In addition, the UK, US and Australian EHE foundations invited their members by email. Participants had to confirm they were indeed an EHE patient in the Informed Consent form and were asked in the questionnaire whether their EHE diagnosis was histologically confirmed. Only English questionnaires were used. Ethical approval for the study was obtained from the local certified Medical Ethics Committee of the Radboud University Medical Center, Nijmegen, The Netherlands (File number 2017-3922).
Data collection
Data collection was performed using the web-based Patient Reported Outcomes Following Initial treatment and Long-term Evaluation of Survivorship (PROFILES) registry, a data management system allowing secure data collection of patient-reported outcomes via online questionnaires [Citation13]. Patients were enrolled between May and October 2018.
Study measures
Sociodemographic and clinical characteristics
Clinical information was self-reported. Comorbidity at the time of survey was assessed by the Self-administered Comorbidity Questionnaire, evaluating the prevalence of 14 comorbidities [Citation14].
Health-related quality of life
HRQoL was measured by the European Organization for Research and Treatment of Cancer (EORTC) Core Quality of Life Questionnaire (EORTC-QLQ-C30) [Citation15]. This 30-item HRQoL questionnaire consists of five functional scales (physical, role, cognitive, emotional and social), a global quality of life scale (overall health and overall quality of life during the past week), three symptom scales and single items assessing symptoms and financial impact of the disease. After linear transformation, all scales and single-item measures ranged from 0-100. A higher score on the functional scales and global QoL means better functioning and HRQoL, whereas a higher score on the symptom scales means more complaints. Clinically important differences in functioning were determined according to the guidelines of the EORTC Quality of Life Group [Citation16] and divided into three size classes: large (representing unequivocal clinical relevance), medium (likely to be clinically relevant, but to a lesser extent), and small (subtle but, nevertheless, clinically relevant).
EHE-specific symptoms were added to the questionnaire based on input from posts within the Facebook group, EHE patients and expert clinicians. These symptoms were assessed by relevant items from the EORTC Item Library, which contains validated questions from HRQoL questionnaires [Citation17]. Linear transformation was applied to generate score ranges from 0-100.
Psychological distress
Since symptoms of cancer may overlap with somatic complaints of depression (e.g. fatigue or weight loss), we used the Hospital Anxiety and Depression Scale (HADS) to assess self-reported depressive symptoms such as anhedonia and loss of interest [Citation18]. The HADS consists of 14 items, 7 items for depressive symptoms and 7 items for anxiety, assessing levels of symptoms in the last week. Questions were answered on a 4-point Likert-scale and the total score for each scale could range from 0 to 21. Cutoff value for symptoms of anxiety and depression was indicated by a score ≥8 [Citation18–20]. Clinically relevant differences were determined according to Norman’s rule of thumb = 0.5 standard deviation [Citation21].
Statistical analysis
Latent class cluster analysis was performed to identify clusters of EHE patients based on symptom burden. Latent class modeling aims to classify similar objects through a data-driven approach, with respect to a set of variables, into mutually exclusive groups [Citation22]. Variables used to define symptom clusters were dichotomous symptom scores of ten relevant symptoms according to expert opinion, of which seven were derived from the QLQ-C30 and recoded into dichotomous scores (fatigue, nausea, appetite, insomnia, pain, constipation, diarrhea), with all positive answers ranging from ‘a little’ to ‘very much’ recoded into ‘yes’. Three additional symptoms from the EORTC Item Library were added (skin-, respiratory- and stomach problems). The optimal number of clusters was based on goodness-of-fit statistics. Bivariate residuals were assessed to check if the local independency assumption was met (values <3) [Citation22]. Cluster analyses were conducted with Latent GOLD version 5.2.0 (Statistical Innovations, Belmont, MA, USA). After cluster identification, differences between clusters were examined with t-tests or analysis of variance (ANOVA) for continuous variables and χ2-tests for categorical variables, where appropriate (SPSS Statistics, version 25.0, IBM SPSS, Chicago, IL, USA).
The same analytical techniques were used to determine differences in HRQoL between our study population and healthy controls [Citation23]. Healthy controls were randomly selected from a sample of 15,306 individuals from the EORTC Norm Data study [Citation23], containing people from across 11 European Union (EU) countries, Russia, Turkey, Canada and United States (n ≥ 1000/country). Since 27% of our patients came from other countries, we decided to match by age and sex only (matching ratio 1:18) to the entire EHE cohort and per symptom cluster. In addition we analyzed whether selection of only norm data from the USA, Canada and Europe (73% of our cohort) changed our findings.
Results
Patient characteristics
A total of 138 patients registered for participation. Twenty-one (15%) patients did not start the questionnaire and were excluded. Two patients did not complete the survey for unknown reasons. Therefore, 115 patients from 20 countries were available for analysis, with a mean age of 47 (range 17–81) years. The majority of patients was female (77%), lived in the USA (47%) and had no current treatment (80%) ( and Supplementary Table S1). All patients reported histological confirmation of their EHE diagnosis.
Table 1. Patient characteristics.
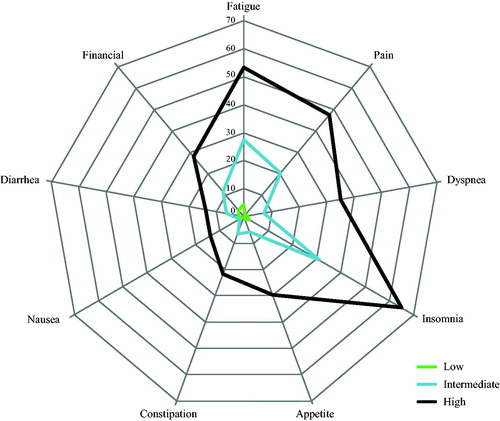
In latent class cluster analysis, the three-cluster model had the best model fit based on the more liberal goodness-of-fit statistics AICLL and AIC3LL, whereas the two-cluster model had the best model fit based on the more conservative BICLL and CAICLL indexes (Supplementary Table 2). We felt that the three-cluster model best described the variation of symptom burden in our population and was therefore more relevant to our research question. The three clusters consisted of EHE patients with low symptom burden (cluster 1, n = 31, 27%), intermediate symptom burden (cluster 2, n = 46, 40%) and high-symptom burden (cluster 3, n = 38, 33%). Among patients with low symptom burden, 48% (15/31) reported none of the 10 symptoms.
Mean age or gender distribution did not differ between the three clusters (). Patients in the highly symptomatic cluster more often reported not having a partner, having comorbid conditions, and bone and/or pleura lesions ( and Supplementary Table 1, p = 0.001). They also more frequently reported aggressive disease stage (p = 0.001) and fewer years since diagnosis (p = 0.044).
HRQoL differences between clusters
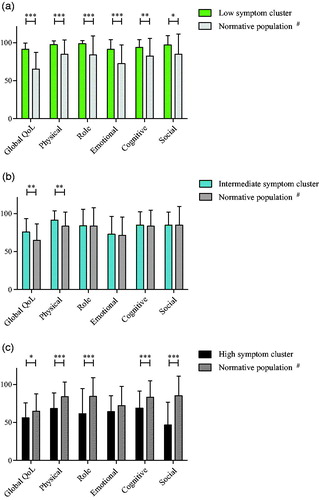
Global QoL was significantly lower in the intermediate (mean 75.9 ± 17.5 SD) and highly symptomatic cluster (56.1 ± 19.4 SD) compared to the low symptom burden cluster (91.7 ± 7.8 SD), with differences of large clinical importance [Citation16] between all three clusters (). Patients with a high symptom burden reported 25–30 points lower scores on physical, role, cognitive and social functioning scales; which are considered large clinical differences. Physical functioning also showed a large clinical difference between the intermediate and highly symptomatic cluster. Emotional functioning was significantly worse in the intermediate and highly symptomatic cluster compared to the low symptom burden cluster.
Table 2. EORTC-QLQ-C30 scores.
HRQoL differences between EHE patients and normative population
Overall, EHE patients reported similar levels of daily functioning compared to healthy controls (n = 2185), except for social functioning which was significantly worse for EHE patients (). Global QoL was significantly better for EHE patients than for the normative population. When comparing the symptom clusters to their respective normative populations, patients with low and intermediate symptom burden reported higher or similar functioning compared to their respective normative populations (n = 558 and n = 828) (). Highly symptomatic patients, however, had significantly lower global QoL and functioning than healthy controls in all domains except for emotional functioning (). In addition, we found that inclusion of only norm data from the USA, Canada and Europe did not significantly change our results.
Figure 1. EORTC-QLQ-C30 functioning scores per symptom cluster and normative population. Bar charts showing EORTC-QLQ-C30 global QoL and functioning scores for (a) the low symptomatic cluster and its normative population, (b) for the intermediate symptom burden cluster and its normative population and (c) for the highly symptomatic cluster and its normative population. *p < 0.05, **p < 0.01, ***p < 0.001, #normative population for that particular symptom cluster.
Symptom burden
Insomnia, fatigue and pain were the most commonly reported symptoms for all patients ( and Supplementary Table S3). In the highly symptomatic cluster, mean scores on these symptoms varied from 47 (±28SD) on pain to 65 (±27SD) on insomnia and were significantly higher than in their normative population (n = 684, Data not shown). Patients in the intermediate or low symptom burden cluster reported similar or lower symptoms scores compared to their respective norm populations. For the entire EHE cohort, symptom scores were comparable to healthy controls (Supplementary Table S3).
Psychological distress
Higher levels of both anxiety and depression where observed when symptom burden was higher (). All of the differences in mean HADS scores between clusters were clinically relevant [Citation21]. When applying cutoff values for anxiety and depression, about one-third of highly symptomatic patients were depressed, and 50% experienced anxiety.
Table 3. Psychological distress.
Discussion
In this study, we demonstrated feasibility of an international HRQoL study in patients living with an extremely rare cancer. Only limited data is available on HRQoL of rare cancer patients, whereas the impact of more common cancers has been studied much more extensively. We cooperated with EHE patients and used a Facebook group for patient recruitment, yielding rapid inclusion of a large number of patients from 20 different countries worldwide. The PROFILES infrastructure was essential for secure data collection and feasibility of this global web-based study [Citation13]. By conventional research methods, performing a HRQoL study of this scale with these patients would have been too expensive and logistically extremely difficult.
We showed that EHE symptom burden varied strongly between patients, correlating with clinically large differences in HRQoL functioning scales, anxiety and depression. Although EHE is often reported to be heterogeneous [Citation7,Citation24], the present study is the first to demonstrate this diversity by identification of three symptom clusters. Previous data are limited to prevalence of symptoms rather than examining the symptom burden of individual patients [Citation2,Citation3,Citation25]. In the present study, 87% of patients reported one or more symptoms, compared to 45-72% symptomatic EHE patients in previous studies [Citation2,Citation3,Citation25].
EHE symptom burden was negatively correlated to HRQoL, with significant differences in global QoL and all functioning scales. The association between symptom level and HRQoL is well-known and has for instance been demonstrated in a large cohort of cancer survivors, showing lower functioning in patients with more severe symptoms [Citation26]. The very low levels of HRQoL scores reported by highly symptomatic EHE patients were remarkable. They reported comparable levels of physical and role functioning to cancer patients in the last 9-12 months of life, whereas emotional and cognitive functioning were strikingly similar to cancer patients in the last 3 months of life [Citation27]. Social functioning was even worse compared to cancer patients in the last 3 months of life [Citation27], although we cannot extract from our data whether patients in our cohort were in their final months of life.
Pain, fatigue and insomnia were the most prevalent symptoms in our cohort, with very high mean symptom scores in the highly symptomatic cluster. Scores on pain and insomnia were even higher among highly symptomatic EHE patients compared to cancer patients in their last 3 months of life [Citation27]. It is uncertain whether the high pain scores in our cohort are due to inadequate recognition in daily clinical practice or merely a reflection of the challenge to relieve EHE-related pain. Whereas patients scored high on fatigue in the present study, this is not in line with the previously (self)reported prevalence of only 3–9% in EHE patients [Citation2,Citation3].
Levels of depression and anxiety were significantly higher in patients with higher symptom burden. The prevalence of depression using a cutoff value of ≥8 points was 19% for the entire group, similar to the previously reported 18% in cancer patients in general [Citation28]. In highly EHE symptomatic patients, 34% were depressed. The co-occurrence of depression and physical symptoms such as pain and fatigue we found in our study, has been recognized before as a common symptom cluster in cancer patients [Citation29,Citation30]. Identification of symptom-based clusters can improve understanding of symptoms and how they correlate to each other. For future studies in EHE patients, it would therefore be of interest to examine whether certain symptoms co-occur and if an intervention targeting one symptom could alleviate related symptom(s) as well.
Surprisingly, our total cohort of EHE patients had similar QoL, daily functioning and symptom levels compared to matched healthy controls. However, specific comparison of the symptom clusters with their respective normative populations revealed that only patients with high-symptom burden had significantly lower global QoL and functioning, and higher symptom scores than healthy controls. These results emphasize the difference in overall QoL between patients with low/intermediate symptom burden and those who are highly symptomatic, and illustrate the large heterogeneity between EHE patients.
Clinical implications
EHE patients in the highly symptomatic cluster more often had bone and/or pleural lesions. Highly symptomatic patients reported both high physical symptom burden and high levels of psychological distress. The co-occurrence of physical and psychological symptoms is a well-known phenomenon in cancer patients [Citation31], and their interaction is illustrated by the finding that treatment of physical symptoms can result in improved mood and vice versa [Citation32,Citation33]. Treatment of EHE-related pain can be challenging and therefore requires attention and early involvement of pain specialists. Use of analgesics could be complemented with psychosocial interventions, which can be effective in reducing cancer-related pain [Citation34]. To relieve fatigue in cancer patients in general, interventions specifically addressing fatigue were reported to be most promising [Citation35]. However, in case of co-occurrence of pain and fatigue, adequate pain control may already improve quality of sleep and reduce fatigue. Pharmacological or psychological interventions with regard to depression in cancer patients were reported to be effective only on the short term (up to 12 weeks), however, the use of a collaborative care approach appeared effective also on the long term [Citation36].
Strengths and limitations
A unique strength of the current patient-initiated study is that we were able to include a large number of ultra-rare cancer patients from 20 different countries by using a social media platform. The use of EORTC-QLQ-C30 to determine HRQoL made it possible to compare our results with normative data from healthy individuals and other cancer populations. However, due to the study design, all clinical characteristics were self-reported and could therefore not be checked for accuracy.
Identification of symptom clusters allowed us to assess relationships with symptom burden rather than individual symptoms. Although our design was cross-sectional and therefore limits causal associations, this is the first study that provides evidence on HRQoL of EHE patients. Our cohort may be relatively highly educated, related to internet use and a potential language barrier for patients from non-English-speaking countries. We possibly missed patients with aggressive disease due to quick deterioration. Although we were able to study a relatively large cohort of EHE patients, patient numbers were insufficient to perform multivariable analyses.
Future perspectives
Overall, our findings support the need to acknowledge highly symptomatic patients in the clinic and to provide appropriate supportive care for those patients. Further research into the cause of the severity of EHE-related pain could help to better intervene and treat the pain. Because of the often prolonged clinical course of EHE, performing longitudinal HRQoL research could provide valuable information about the clinical course over time, its relationship with HRQoL and therefore appropriate timing of supportive care interventions. Collection of additional clinical parameters in a future cohort study would enable for instance assessment of clinical risk scores and the correlation between clinical risk factors and HRQoL. For such a cohort study international collaboration would be necessary to establish a relatively large cohort of EHE patients. Furthermore, additional research can provide increased awareness among health care professionals, and assistance in information provision and decision-making.
Conclusion
In conclusion, we proved international HRQoL research in an ultra-care cancer feasible, facilitated by cooperation with patients and online secure data collection. With this study, we demonstrated that EHE patients can be divided into three symptom-based clusters, and that physical symptom burden was strongly associated with HRQoL and psychological distress. Acknowledgment of the existence of a group with highly symptomatic patients warrants further research in the optimal treatment of EHE-related pain.
Supplemental Material
Download MS Word (13.3 KB)Supplemental Material
Download MS Word (15.9 KB)Supplemental Material
Download MS Word (18.6 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Boyd N, Dancey JE, Gilks CB, et al. Rare cancers: a sea of opportunity. Lancet Oncol. 2016;17(2):e52–e61.
- Lau K, Massad M, Pollak C, et al. Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest. 2011;140(5):1312–1318.
- Shiba S, Imaoka H, Shioji K, et al. Clinical characteristics of Japanese patients with epithelioid hemangioendothelioma: a multicenter retrospective study. BMC Cancer. 2018;18(1):993.
- Rosenbaum E, Jadeja B, Xu B, et al. Prognostic stratification of clinical and molecular epithelioid hemangioendothelioma subsets. Mod Pathol. 2020;33(4):591–602.
- Deyrup AT, Tighiouart M, Montag AG, et al. Epithelioid hemangioendothelioma of soft tissue: a proposal for risk stratification based on 49 cases. Am J Surg Pathol. 2008;32(6):924–927.
- Yousaf N, Harris S, Martin-Liberal J, et al. First line palliative chemotherapy in elderly patients with advanced soft tissue sarcoma. Clin Sarcoma Res. 2015;5:10.
- Sardaro A, Bardoscia L, Petruzzelli MF, et al. Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev. 2014;8(2):259.
- Davis AT, Guo AM, Phillips NJ, et al. A novel treatment for bone lesions of multifocal epithelioid sarcoma-like hemangioendothelioma. Skeletal Radiol. 2015;44(7):1013–1019.
- Thomas RM, Aloia TA, Truty MJ, et al. Treatment sequencing strategy for hepatic epithelioid haemangioendothelioma. HPB. 2014;16(7):677–685.
- Jung DH, Hwang S, Hong SM, et al. Clinicopathological features and prognosis of hepatic epithelioid hemangioendothelioma after liver resection and transplantation. Ann Transplant. 2016;21:784–790.
- Maruzzo M, Martin-Liberal J, Messiou C, et al. Systemic treatment options for epithelioid haemangioendothelioma: the Royal Marsden Hospital experience. Clin Sarcoma Res. 2015;5(1):5–80.
- Stacchiotti S, Provenzano S, Dagrada G, et al. Sirolimus in advanced epithelioid hemangioendothelioma: a retrospective case-series analysis from the italian rare cancer network database. Ann Surg Oncol. 2016;23(9):2735–2744.
- van de Poll-Franse LV, , Horevoorts N, van Eenbergen M, et al.; Profiles Registry Group. The patient reported outcomes following initial treatment and long term evaluation of survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer. 2011;47(14):2188–2194.
- Sangha O, Stucki G, Liang MH, et al. The self-administered comorbidity questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–163.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376.
- Cocks K, King MT, Velikova G, et al. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29(1):89–96.
- Available from: https://www.eortc.be/itemlibrary/. [Last accessed on April 2017].
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Olsson I, Mykletun A, Dahl AA. The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5:46.
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592.
- Vermunt JMJ. Latent GOLD 4.0 User’s Guide. Belmont (MA): Statistical Innovations; 2005.
- Nolte S, EORTC Quality of Life Group, Liegl G, Petersen MA, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur J Cancer. 2019;107:153–163.
- Rosenberg A, Agulnik M. Epithelioid Hemangioendothelioma: Update on Diagnosis and Treatment. Curr Treat Options Oncol. 2018;19(4):19.
- Wu X, Li B, Zheng C, et al. Clinical characteristics of epithelioid hemangioendothelioma: a single-center retrospective study. Eur J Med Res. 2019;24(1):16.
- Kjaer TK, Johansen C, Ibfelt E, et al. Impact of symptom burden on health related quality of life of cancer survivors in a Danish cancer rehabilitation program: a longitudinal study. Acta Oncol. 2011;50(2):223–232.
- Raijmakers NJH, Zijlstra M, van Roij J, et al. Health-related quality of life among cancer patients in their last year of life: results from the PROFILES registry. Support Care Cancer. 2018;26(10):3397–3404.
- Krebber AM, Buffart LM, Kleijn G, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology. 2014;23(2):121–130.
- Barsevick AM. The elusive concept of the symptom cluster. Oncol Nurs Forum. 2007;34(5):971–980.
- Kirkova J, Walsh D, Aktas A, et al. Cancer symptom clusters: old concept but new data. Am J Hosp Palliat Care. 2010; Jun 27(4):282–288.
- Fitzgerald P, Lo C, Li M, et al. The relationship between depression and physical symptom burden in advanced cancer. BMJ Support Palliat Care. 2015;5(4):381–388.
- Given C, Given B, Rahbar M, et al. Effect of a cognitive behavioral intervention on reducing symptom severity during chemotherapy. J Clin Oncol. 2004;22(3):507–516.
- Sheinfeld Gorin S, Krebs P, Badr H, et al. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. JCO. 2012;30(5):539–547.
- Syrjala KL, Jensen MP, Mendoza ME, et al. Psychological and behavioral approaches to cancer pain management. J Clin Oncol. 2014;32(16):1703–1711.
- Goedendorp MM, Gielissen MF, Verhagen CA, et al. Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst Rev. 2009;(1):CD006953.
- Li M, Kennedy EB, Byrne N, et al. Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psychooncology. 2017;26(5):573–587.