Introduction
Functional outcome following treatment for colorectal cancer has received increasing attention, and it has been shown that bowel dysfunction is very common after rectal resection. However, little is still known about patients treated for right-sided colon cancer. In inflammatory bowel disease and polyposis, colon resections may be associated with a wide range of bowel problems [Citation1–4]. Right-sided colon resection may lead to increased stool frequency and loose stools due to disturbance of the bile acid reabsorption [Citation5,Citation6]. You would expect similar symptoms after treatment for right-sided colon cancer; still, no major studies have been conducted. Major abdominal surgery and impaired bowel function is showed to affect quality of life (QoL) [Citation7–9]. This calls for investigation of the increasing population of colon cancer survivors, where bowel dysfunction may be an overlooked problem.
The aim of this study was to investigate the prevalence of long-term bowel dysfunction and QoL in right-sided hemicolectomy patients treated for cancer compared to polypectomy patients.
Material and methods
Study design
This cross-sectional study was based on a national Danish cohort of patients with cancer in the cecum or ascending colon treated with right-sided hemicolectomy. The control group consisted of patients treated with an endoscopic polypectomy of a malignant colon polyp. All patients received a questionnaire regarding bowel function and QoL. Data from the questionnaire were compared to prospective data from the Danish Colorectal Cancer Group’s (DCCG) national database, where all patients diagnosed with colorectal cancer in Denmark since May 2001 are registered.
Patient details
Patients were identified through the DCCG’s database. The database contains information about patient characteristics, type of cancer, stage of disease, and treatment.
All Danish colon cancer patients diagnosed between May 2001 and December 2014 and treated with right-sided hemicolectomy, extended right-sided hemicolectomy, ileocecal resection, or polypectomy were invited. In the following, the term ‘right-sided hemicolectomy’ (RHC) includes all the right-sided resections. Resections were performed either with the laparoscopic, robot-assisted, or open approach. Polypectomies were performed with colonoscopy either by simple polypectomy, endoscopic mucosa resection or endoscopic submucosal dissection. Exclusion criteria were metastasis, recurrent disease, permanent stoma, radiation therapy and dementia. The DCCG data were compared to the Danish Civil Registration System to exclude patients who were dead or emigrated, and patients with research protection. The study was approved by the Danish Data Protection Agency and the Danish Health Authority.
The questionnaire
All patients received an invitation by letter with a link to an electronic survey. After three weeks, non-responders received the link once again as well as the survey in paper form plus a pre-paid return envelope. The letters included a phone number to a hotline in case of queries. All questionnaires were answered between mid-November 2015 and mid-February 2016. The study was part of a large questionnaire study on late sequelae to bowel cancer in general. The bowel function component of the questionnaire contained 23 items selected from validated scores including the Bristol stool chart (BSC) [Citation10–14] and a single anchor question asking; ‘Overall, how much does your bowel function affect your quality of life?’ [Citation15,Citation16]. All participants were asked to pick one out of the seven types on the BSC as their predominant stool type. Type 6 (fluffy or mushy) and type 7 (liquid) were used as indicators of watery and loose stool [Citation14,Citation17]. To investigate QoL, we used the validated Danish version of the EORTC QLQ-C30 questionnaire version 3.0 (European Organization for Research and Treatment of Cancer) [Citation18,Citation19], which includes one global health status, five functional subscales, three symptom scales and six single items addressing different aspects of QoL. The scales are ranging from 0–100 points. A mean difference of 5–10 points represents a ‘small’, 10–20 points a ‘moderate’ and ≥20 points a ‘major’ clinical difference [Citation20].
Study endpoints
The primary endpoints were the risk of loose stools (BSC type 6–7) among RHC patients compared to polypectomy patients, and its impact on QoL. The secondary endpoints were frequency of other bowel symptoms, including frequency of defecation, urgency and incontinence, among RHC patients compared to polypectomy patients. Finally, the long-term influence of adjuvant chemotherapy on bowel function and QoL was examined within the RHC group.
Statistical analysis
Student’s t-test or Mann-Whitney test was used for continuous data, and Chi2 test was used to compare proportions. Logistic regression was used to calculate the association between bowel dysfunction and type of treatment (RHC and polypectomy) adjusted for gender, age and time since treatment. The significance level was set at 0.05. Two researchers independently performed all analyses using STATA statistical software version 12 (StataCorp LP, College Station, Texas, USA).
Results
Patient characteristics
A total of 6188 patients were invited, and 3540 patients (3306 RHC and 234 polypectomy) answered the questionnaire, corresponding to a response rate of 61.5% in the RHC group and 47.5% in the polypectomy group. The flowchart is shown in Supplementary Figure 1.
The median time since treatment was slightly longer in the RHC group compared to the polypectomy group (4.6 [range 0.8–14.7] years vs. 3.9 [range 1.0–14.2] years). As expected, more of the polypectomy patients were diagnosed by screening (16.7% vs. 3.3% in the RHC group). Patient characteristics are summarized in Supplementary Table 1.
Risk of loose stools and other bowel symptoms
In the RHC group, 15.5% [14.2–16.8%] of the patients had loose stools (BSC 6–7) compared to only 6.7% [3.8–10.8%] of polypectomy patients, p < .001. The odds ratio was 2.64 [1.52–4.59] after adjusting for age, gender and time since treatment.
A total of 20.2% [18.8–21.6%] of the RHC patients suffered from nocturnal defecation, and the odds were almost doubled compared to the polypectomy patients (adjusted OR 1.85 [1.23–2.79]). Additionally, RHC patients had a higher risk of alternating stool consistency, urgency, incontinence to liquid stool and need for using a pad. There was no difference in defecation frequency. Blood in the stools as well as strain to defecate were more common in the polypectomy group (both p .02). The prevalence of bowel symptoms is summarized in .
Table 1. Frequency of bowel symptoms in the right-sided hemicolectomy (RHC) and polypectomy group.
There were no differences between the two groups when investigating symptoms of obstruction, incomplete evacuation, use of laxatives and bloating (data not shown).
‘Overall, how much does your bowel function affect your quality of life?’
Overall, RHC patients reported a higher negative impact of bowel function on QoL compared to polypectomy patients (p < .001). Bowel function had a major impact on QoL in 40.3% of RHC patients with loose stool (BSC 6–7), while it was only the case for 12.8% of RHC patients with BSC 1–5 ().
EORTC quality of life scores
Clinical differences were seen between the RHC and polypectomy patients () on the diarrhea symptom score (mean difference 11.8, p < .001) and the fatigue score (mean difference 6.8, p < .001), while no clinically significant differences were seen in the other scales.
Figure 1. Mean scores of the EORTC QLQ-C30 functional and symptom scales presented as mean values and 95% confidence intervals. *Small clinically relevant difference, **Moderate clinically relevant difference, ***Major clinically relevant difference. (A) Right-sided hemicolectomy patients compared to polypectomy patients. (B) Right-sided hemicolectomy, comparison between patients with and without loose stools (Bristol stool chart 6–7 vs. Bristol stool chart 1–5).
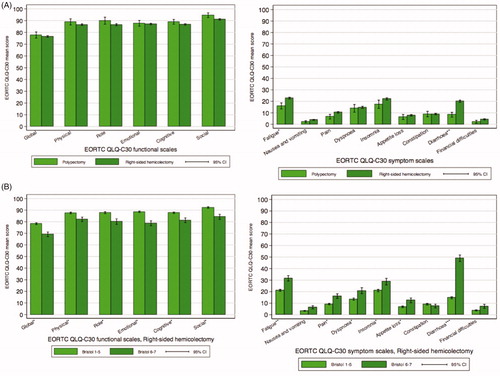
Looking at the RHC group only (), patients having loose stools (BSC 6–7) had significantly lower scores on all functional scales, lowest for the emotional functioning with a mean difference of 9.8 (p < .001). On the global quality of life score, the mean difference was 9.1 (p < .001). Furthermore, clinically significant differences were seen on most of the symptom scales. Patients with BSC 6–7 reported a much greater extent of fatigue and diarrhea (mean difference 10.4 and 34.3, respectively. Both p < .001).
Impact of adjuvant chemotherapy
Adjuvant chemotherapy was used in 1126 (34.2%) of the RHC patients (Supplementary Table 1). When comparing RHC patients with and without chemotherapy, the use of chemotherapy had no impact on the risk of loose stools (BSC 6–7) (OR 1.11 [0.91–1.36]) or in any other aspects of the bowel function. Additionally, chemotherapy had no long-term effect on QoL neither regarding our anchor question or the EORTC QLQ-C30.
Discussion
This study shows that cancer patients treated with RHC have increased risk of loose stools (BSC 6–7) (15.5%) compared to patients with local excision of a malignant colon polyp. The RHC patients with loose stools had impaired QoL.
Even though our RHC patients had a higher frequency of watery and loose stool, the defecation frequency was, surprisingly, the same as in the polypectomy group. This corresponds to the results from a Japanese study [Citation21], reporting loose stool among 38 right-sided hemicolectomy patients and no change in defecation frequency. In another publication arising from the same large survey, Elfeki et al. [Citation22] showed that, after resection of sigmoid colon, the risk of loose stools (BSC 6–7) was only 4.4%. This strongly support that the pattern of bowel dysfunction found in our study population is specific for RHC patients.
Bowel symptoms are common in the background population. In our study, 6.7% of polypectomy patients had loose stool, corresponding to the prevalence of BSC 6–7 in the background population [Citation23].
Chronic watery and loose stool among RHC patients could result from decreased water absorption due to the shortened colon, or it could be caused by bile acid malabsorption [Citation24,Citation25]. Phillips et al. investigated bowel dysfunction in a mixed group of cancer survivors and showed that half of the patients referred with Bristol stool type 6 and 7, had bile acid malabsorption [Citation24]. Additionally, resection of the ileocecal valve can lead to retrograde passage of colonic bacteria, resulting in bacterial overgrowth in the small intestine and watery and loose stools [Citation3,Citation26,Citation27]. Resection of the terminal ileum is known to cause bile acid malabsorption and subsequently loose stools in patients treated for Crohn’s disease [Citation5]. Kurien et al. [Citation6] showed that even short resections of the terminal ileum could cause bile acid malabsorption.
In addition to loose stools, RHC patients suffered from alternating stool consistency, incontinence to liquid stool, need of using a pad, urgency, decreased ability to defer defecation and 20.2% had nocturnal defecation. By comparison, the Japanese study [Citation21] found a risk of 13.2% of nightly defecation after RHC, which was significantly greater than for patients with left-sided resection. A total of 28.8% of our RHC patients suffered from incontinence to liquid stool, which is almost twice as many as reported in a study of 315 patients comparing the outcome of different segmental colon resections, where 16.4% of RHC patients had occasional liquid soiling [Citation28].
RHC patients reported a higher impact of bowel function on QoL than polypectomy patients in our anchor question. Likewise, the RHC group had higher scores on both the diarrhea symptom scale and the fatigue scale on the EORTC QLQ-C30. Furthermore, according to the EORTC QLQ-C30 and our anchor question, RHC patients suffering from watery and loose stools had a markedly decreased QoL compared to RHC patients with BSC 1–5. This corresponds to previous studies showing that suffering from impaired bowel function negatively impacts the QoL [Citation28,Citation29].
We found no long-term impact of adjuvant chemotherapy on bowel function or QoL after RHC, which corresponds to the few studies published on this subject [Citation30,Citation31].
All cancer patients in Denmark treated with RHC or polypectomy were invited from the DCCG database, which has high completeness and a high validity of data. However, the response rate among polypectomy patients (47.5%) was slightly lower than we expected (61.5% among RHC patients), which is a substantial limitation to the study. Non-responders were older (median age 5 years older) and had more comorbidity. Because of the cross-sectional study design, it was not possible to investigate change over time in postoperative bowel function or to adjust for baseline function, and thereby identify changes due to surgery. However, such analysis might be confounded by baseline symptoms due to presence of the cancer. Instead, we compared the RHC patients to the control group of polypectomy patients to identify functional problems most likely associated with resection of the right colon. We grouped all right-sided resections (hemicolectomy, extended hemicolectomy, ileocecal resection) together, since there were no differences between the groups (data not shown). No information regarding length of the resected bowel was available. Fiber intake and use of antidiarrheal medication might have influenced the patients’ bowel function, but unfortunately, no information was available regarding this.
In conclusion, RHC patients treated for cancer had a higher risk of loose stool and several other bowel symptoms compared to polypectomy patients. RHC patients with loose stools reported a substantially decreased QoL. Interestingly, use of adjuvant chemotherapy in RHC patients had no impact on long-term bowel function or QoL. Large prospective studies are ongoing regarding identification and treatment of RHC patients with loose stools.
Supplemental Material
Download MS Word (13.6 KB)Supplemental Material
Download JPEG Image (95.6 KB)Disclosure statement
The authors report no conflicts of interest. The study was approved by the Danish Data Protection Agency and the Danish Health Authority.
Additional information
Funding
References
- Duclos J, Lefevre JH, Lefrancois M, et al. Immediate outcome, long-term function and quality of life after extended colectomy with ileorectal or ileosigmoid anastomosis. Colorectal Dis. 2014;16(8):O288–96.
- Newton CR, Baker WN. Comparison of bowel function after ileorectal anastomosis for ulcerative colitis and colonic polyposis. Gut. 1975;16(10):785–791.
- Eu KW, Lim SL, Seow-Choen F, et al. Clinical outcome and bowel function following total abdominal colectomy and ileorectal anastomosis in the Oriental population. Dis Colon Rectum. 1998;41(2):215–218.
- Phipps E, Braitman LE, Stites S, et al. Quality of life and symptom attribution in long-term colon cancer survivors. J Eval Clin Pract. 2008;14(2):254–258.
- Eusufzai S. Bile acid malabsorption: mechanisms and treatment. Dig Dis. 1995;13(5):312–321.
- Kurien M, Evans KE, Leeds JS, et al. Bile acid malabsorption: an under-investigated differential diagnosis in patients presenting with diarrhea predominant irritable bowel syndrome type symptoms. Scand J Gastroenterol. 2011;46(7–8):818–822.
- Andreyev HJ, Davidson SE, Gillespie C, et al. Practice guidance on the management of acute and chronic gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61(2):179–192.
- Douma KF, Bleiker EM, Vasen HF, et al. Quality of life and consequences for daily life of familial adenomatous polyposis (FAP) family members. Colorectal Dis. 2011;13(6):669–677.
- Wolf ND, Kadmon M, Wolf RC, et al. Quality of life after restorative proctocolectomy and ileal pouch-anal anastomosis in patients with familial adenomatous polyposis: a matter of adjustment. Colorectal Dis. 2011;13(11):e358–65.
- Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36(1):77–97.
- Agachan F, Chen T, Pfeifer J, et al. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39(6):681–685.
- Vaizey CJ, Carapeti E, Cahill JA, et al. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44(1):77–80.
- Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012;255(5):922–928.
- Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–924.
- Emmertsen KJ, the Rectal Cancer Function Study Group Impact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancer. Br J Surg. 2013;100(10):1377–1387.
- Battersby NJ, Juul T, Christensen P, et al. Predicting the risk of bowel-related quality-of-life impairment after restorative resection for rectal cancer: a multicenter cross-sectional study. Dis Colon Rectum. 2016;59(4):270–280.
- O'Donnell LJ, Virjee J, Heaton KW. Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit rate. BMJ. 1990;300(6722):439–440.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376.
- Groenvold M, Klee MC, Sprangers MA, et al. Validation of the EORTC QLQ-C30 quality of life questionnaire through combined qualitative and quantitative assessment of patient-observer agreement. J Clin Epidemiol. 1997;50(4):441–450.
- Osoba D, Rodrigues G, Myles J, et al. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16(1):139–144.
- Ohigashi S, Hoshino Y, Ohde S, et al. Functional outcome, quality of life, and efficacy of probiotics in postoperative patients with colorectal cancer. Surg Today. 2011;41(9):1200–1206.
- Elfeki H, Larsen HM, Emmertsen KJ, et al. Bowel dysfunction after sigmoid resection for cancer and its impact on quality of life. Br J Surg. 2019;106(1):142–151.
- Heaton KW, Radvan J, Cripps H, et al. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992;33(6):818–824.
- Phillips F, Muls AC, Lalji A, et al. Are bile acid malabsorption and bile acid diarrhoea an important cause of diarrhoea complicating cancer therapy? Colorectal Dis. 2015;17(8):730–734.
- Jewkes AJ, Windsor CW, Ward RS, et al. Relationship between bile acid malabsorption using the 75Se homocholic acid taurine scanning method and diarrhoea following right hemicolectomy. Br J Surg. 1989;76(7):707–708.
- Wedlake L, Thomas K, Lalji A, et al. Effectiveness and tolerability of colesevelam hydrochloride for bile-acid malabsorption in patients with cancer: a retrospective chart review and patient questionnaire. Clin Ther. 2009;31(11):2549–2558.
- Elphick DA, Chew TS, Higham SE, et al. Small bowel bacterial overgrowth in symptomatic older people: can it be diagnosed earlier? Gerontology. 2005;51(6):396–401.
- Ho YH, Low D, Goh HS. Bowel function survey after segmental colorectal resections [Conference Paper. Dis Colon Rectum. 1996;39(3):307–310.
- Magdeburg J, Glatz N, Post S, et al. Long-term functional outcome of colonic resections: how much does faecal impairment influence quality of life? Colorectal Dis. 2016;18(11):O405–O413.
- Theodoropoulos GE, Karantanos T, Stamopoulos P, et al. Prospective evaluation of health-related quality of life after laparoscopic colectomy for cancer. Tech Coloproctol. 2013;17(1):27–38.
- Sclafani F, Peckitt C, Cunningham D, et al. Short- and long-term quality of life and bowel function in patients with mri-defined, high-risk, locally advanced rectal cancer treated with an intensified neoadjuvant strategy in the randomized Phase 2 EXPERT-C trial. Int J Radiat Oncol Biol Phys. 2015;93(2):303–312.
