Introduction
Following the first case of acute respiratory syndrome coronavirus 2 (SARS-CoV-2, known as COVID-19) in Denmark at the end of February 2020, wide-spread social distancing was implemented and societal restrictions were imposed on March 11. At the same time, the World Health Organization (WHO) characterized COVID-19 as a global pandemic [Citation1]. In Denmark, the schools closed, civil servants with non-critical functions were sent home, and private employers were encouraged to apply for home-based work, and restaurants and shops, except for grocery stores and pharmacies, closed. Older citizens and citizens at increased risk for severe disease or death due to COVID-19 were advised to stay at home and limit social contacts. Citizens were not confined to their homes, but public gatherings were limited with an upper limit of 10 persons when the restrictions were most strict. Since 15 April 2020, Denmark has undergone a controlled reopening. Due to a second wave of infections in the autumn of 2020 additional restrictions have been implemented, including the use of face masks in public transportation and indoor public places and at restaurants while moving around. The test capacity is now abundant and in November 2020 more than 6 million tests have been performed, with 53% of the population tested at some point and 59,000 diagnosed with COVID-19 in the population of 5.8 million [Citation2–3].
WHO has demonstrated that in 92% of countries, health care staff have been reassigned to COVID-19 related services with anticipated negative effects on, e.g. cancer care, chronic diseases and rehabilitation [Citation4]. Danish health care authorities have also introduced significant adjustments to ensure sufficient resources for in-patient care of serious COVID-19 cases. On 13 March, the Danish National Board of Health instructed the hospitals to delay treatment for some patient groups during the COVID-19 pandemic, including non-acute or non-life-threatening conditions, and diseases for which delayed treatment was considered professionally justifiable [Citation5].
The first report of the consequences of COVID-19 revealed that all-cause mortality and mortality from chronic conditions during January to June, 2020, did not differ significantly from the previous five years [Citation6]. One study found that in mid-April 2020, the prevalence of antibodies against SARS-CoV-2 was 4% in health-care workers [Citation7]. Other studies have reported significant detrimental effects from the COVID-19 pandemic in several health care areas such as cardiology, surgery and cancer care with fewer acute admissions, delayed diagnoses and higher complication and mortality rates [Citation8–10].
To quantify undetected cancer cases entailing a risk of subsequently increased mortality, we investigated incident cancer diagnoses in Denmark during the first months of the COVID pandemic.
Material and methods
Information on incident first cancer diagnoses was ascertained from national Danish registries covering all Danish citizens. The Danish Cancer Registry [Citation11] was used for the period 2015–2018 and the National Patient Register for 2019 and 2020 [Citation12]. The Patient Register is the primary source of the Cancer Registry. Since 2004 all cancer diagnoses at in- and outpatient hospital settings have been registered in the Patient Register. The Danish Cancer Registry are based on registrations in the Patient Register, the Danish Pathology Register [Citation13] and the Danish Register of Causes of Death [Citation14]. To ensure completeness, quality and incorporation of all death certificates, the Cancer Registry is updated at the end of each calendar year and thus has a delay of one year. We therefore used the Patient Register for the period 2019 and 2020. Cancer diagnoses in the Patient Register have not been validated up against the Pathology Register and does not include histologic details and contributions of cancer deaths with no previous record. However, in Denmark, only a few (∼1–2%) cancer cases are registered based on death certificates only [Citation11,Citation13].
We defined ‘all cancer’ as ‘malignant neoplasms’ (except ‘non-melanoma skin cancer’), ‘polycythaemia vera’ and ‘myelodysplastic syndromes’ (ICD10 codes: C00–C96, except C44; D45-47). The most common cancers were defined as female breast cancer (C50), prostate cancer (C61), colon cancer (C18), and lung cancer (C33–34) [Citation15]. The patients were categorized in three age groups (<50 years; 50–69 years, and 70+ years) according to assumed age-related risk of severe COVID-19 infection, and by sex.
Numbers of incident cancer diagnoses were counted for each month for the period February to May 2020. For each month, the count was compared with incident cancer diagnoses in the previous 5 years (2015–2019), e.g. March 2020 was compared with the average of March 2015–2019. In addition, we compared the total number of incident cancer diagnoses during the lockdown, March–May, with the corresponding average number of diagnoses in March–May 2015–2019.
We estimated the changes in the number of cancer diagnoses in percentages, with 95% confidence intervals (CIs), in 2020 compared to 2015–2019 for each month separately and for March–May combined, using linear regression models for the log-transformed counts. In addition, we performed a post hoc sensitivity analysis to examine the high incidence found in March 2019.
Legal approval to use data was obtained from The Danish Health Data Authority. Ethical review is not required for registered based studies in Denmark. Statistical software SAS version 9.4 was used for data handling and analyses.
Results
For incident cancer overall, there was a substantial reduction in the number of new cases in March, April and May 2020 (). The estimated reduction in 2020 compared to the previous five years ranged from approximately 800 incident cancers (24%; 95% CI: 2–41) in March, 900 incident cancers (34%; 95% CI: 26–42) in April, to 1,200 incident cancers (42%; 95% CI: 37–46) in May. The combined reduction for March to May was 33% [95% CI: 26–40] deriving from a total reduction of approximately 2800 undetected cancers (). We found similar reductions in incident cancer diagnoses in the three age groups, i.e. 33% [95% CI: 22–43] for patients below 50 years, 36% [95% CI: 31–41] for age 50–70 years and 30% [95% CI: 20–39] for patients older than 70 years. The reductions in cancer diagnoses were also similar for women (31%; 95% CI: 22–40) and men (35%; 95% CI: 30–40). Slight differences were seen for the common cancer types, i.e. female breast cancer (30%; 95% CI: 18–40), prostate cancer (42%; 95% CI: 37–47), colon cancer (43%; 95% CI: 33–52), and lung cancer (24%; 95% CI: 19–30) ( and Supplementary Figures S1–S4), but the overall pattern was a clear reduction in number of incident cancers. The number of cancer diagnoses per months varied slightly during the study period 2015–2020, although with larger variation in March and April. A sensitivity analysis excluding March 2019 showed a 20% [95% CI: 5–33] reduction in cancer diagnoses overall in March 2020 compared to March in the period 2015–2018.
Figure 1. Incident cancer diagnoses for the month before the COVID-19 lockdown (February) and the months after the lockdown on March 11, 2020. Green bars from the Cancer Registry (2015–2018); blue bars from the Patient Register (2019–2020).
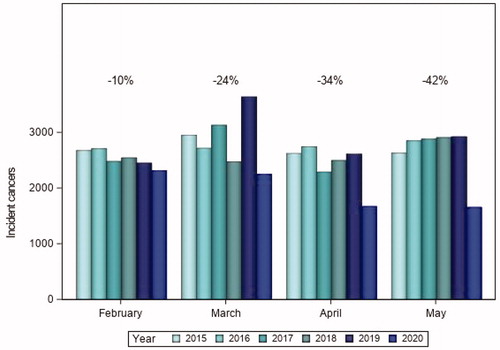
Table 1. Reduction in cancer incidence per month in the COVID-19 lockdown period compared with the same period in the previous 5 years.
Discussion
We found a substantial reduction in the number of incident cancer diagnoses by one-third during the first three months of the COVID-19 pandemic in Denmark compared to the previous years. The reductions in incident cancer diagnoses were seen across different age groups and in both sexes, and with similar reductions by 24–42% for the four most common cancer types. These findings are in line with a Dutch study that based on cancer registry data showed reductions in cancer diagnoses during March–April 2020 [Citation10]. The Dutch study also revealed consistent results across age groups and geographical regions. The largest reduction in cancer diagnoses was observed for skin cancers. In our study, melanoma skin cancer exhibited a similar reduction in diagnoses as the four most common cancer types. In Sweden, which has remained more open than most other countries, a reduction of 12% in cancer diagnoses was reported between March and August 2020 compared with the same period in 2019 [Citation16]. Observations based on analyses of pathology specimens in Northern Ireland also point in the same direction: the reduction in the number of cancer diagnoses based on pathology samples between weeks 10 and 20 was 29% [Citation17]. Data from the United States revealed a similar pattern with a significant decline in incidence for 6 common cancer types [Citation18]. The decrease in incidence ranged from 25% for pancreatic cancer to 52% for breast cancer.
The effects of COVID-19 on cancer detection in Denmark should be viewed against a background of non-suspended screening programs, unchanged cancer care pathways and adherence to the defined maximal lead times to start of treatment. Even so, participation rates in the screening programs for breast cancer and cervical cancer decreased somewhat (personal communication from screening services). Diagnostic cancer pathways could be accessed according to the same principles during the pandemic as before, although some of the clinical diagnosis-specific guidelines allowed for temporary deviations to minimize the risk of infection.
The reasons for the undetected cancer diagnoses in Denmark during the first three months of the COVID-19 pandemic remain to be identified but are likely multifactorial. Danish healthcare is public and predominantly tax-based, and based on universal access with gatekeeper functions to secondary care through general practitioners. Access to primary health care is generally good, but during the initial phases of the pandemic, it was more difficult to book a physical consultation in primary care. It is also likely that individuals with mild or unspecific symptoms have had a higher barrier for contacting their general practitioner due to perceived risk of infection, out of capacity considerations or due to difficulties in obtaining non-acute consultations. Danish authorities, like in many other countries [Citation19–20], have also advised elderly persons with comorbidities and individuals in risk groups to limit social contacts and self-isolate because of the high risk of severe COVID-19 infection. These considerations are reflected by a monthly reduction of 100,000–300,000 health care contacts in Denmark during March–May 2020 [Citation21].
In 2019, The National Patient Register launched a new registration system, LPR3, for in- and outpatient hospital contacts in Denmark. In the initial phase of LPR3 registration, there were challenges with the data quality and completeness, but in the latest report from July 2020, data quality and completeness of LPR3 were found to be at the same level as in the former Patient Register, LPR2 [Citation21]. This report also stated that the reduction in hospital activity during the period March to May 2020 was likely due to the changed activity to handle the COVID-19 pandemic. We found that the variation between the 5 years prior to 2020 varied for different months, being highest in March and April. This variation is compatible with lower hospital activity during vacation periods, notably Easter, in which some years are placed in March, some years in April and some years in late March and early April [Citation21]. The high incidence found in March 2019 could also to some extent be explained by the incidence that should have been allocated earlier in 2019, because not all hospitals started the new registration system primo January 2019. Therefore we conducted a sensitivity analysis to measure the effect of ‘March 2019’ and it showed no altered overall results.
The impact of diagnostic delays in cancer varies between diagnoses and tumor subsets, emphasizing the need for studies of the influence of the COVID-19 pandemic on cancer detection. A very recent study from the United Kingdom (UK) reported that a four-week delay in cancer treatment was associated with increased mortality [Citation22]. A modeling study from the UK suggested a significant increase in cancer mortality due to the COVID-19 pandemic with 4.8–16.6% increase in the number of cancer deaths from breast cancer, colorectal cancer, lung cancer and esophageal cancer up to 5 years after diagnosis [Citation23]. The UK had a stricter lockdown than Denmark with suspension of screening programs and prioritization of urgent symptomatic cases with significant diagnostics delays for cancer patients, and the authors estimated that between 59,000 and 63,000 additional years of life will be lost to cancer in the UK due to the COVID-19 pandemic [Citation23]. Further studies are needed to examine the impact of delayed diagnosis of cancer due to the COVID-19 pandemic in Denmark.
In conclusion, an increasing number of countries, including Denmark, Sweden, the Netherlands, the UK and the US have documented negative effect from COVID-19 on the detection of new cancers, suggesting an increase in cancer deaths due to diagnostic delays. While the population has implemented social distancing and pandemic precautions it is important to consider that cancer does not pause. These observations call for policy interventions that may be particularly important and timely when several countries now experience a second wave of COVID-19 infection [Citation24]. To avoid serious effects from disruption of health services paradigms, individuals with symptoms of cancer or with continued unspecific symptoms should be encouraged to consult their general practitioner and follow established screening programs.
Supplemental Material
Download MS Word (279.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- WHO Director-General's opening remarks at the media briefing on COVID-19, March 11, 2020. World Health Organization.
- Statens Serum Institut. Available from: https://experience.arcgis.com/experience/aa41b29149f24e20a4007a0c4e13db1d.
- Danish Health Authorities. Available from: https://www.sst.dk/en/English/Corona-eng/COVID-19-updates-Statistics-and-charts.
- WHO Newsroom. COVID-19 significantly impacts health services for noncommunicable diseases; 2020 Jun 1 [cited 2020 Jul 10]. Available from: https://www.who.int/news-room/detail/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases.
- Danish Health Authorities. Notat om reduktion af hospitalsaktivitet ifm COVID-19. Danish Health Authorities; March 13, 2020.
- Mills EHA, Moller AL, Gnesin F, et al. National all-cause mortality during the COVID-19 pandemic: a Danish registry-based study. Eur J Epidemiol. 2020;35(11):1007–1013.
- Iversen K, Bundgaard H, Hasselbalch B, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet 2020;20(12):1401–1408.
- Sokolski M, Gajewski P, Zymlinski R, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on acute admissions at the emergency and cardiology departments across Europe. Am J Med. 2020. DOI:10.1016/j.amjmed.2020.08.043
- Mc Lean RC, Young J, Musbahi A, et al. A single-centre observational cohort study to evaluate volume and severity of emergency general surgery admissions during the COVID-19 pandemic: is there a ‘lockdown’ effect? Int J Surg. 2020;83:259–266.
- Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21(6):750–751.
- Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39(7 Suppl):42–45.
- Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin. Epidemiol. 2015;7:449–490.
- Bjerregaard B, Larsen OB. The Danish Pathology Register. Scand J Public Health. 2011;39(7 Suppl):72–74.
- Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(7 Suppl):26–29.
- The Danish Health Data Authority. Annual report 2018: “Nye kraefttilfaelde i Danmark 2018”. The Danish Health Data Authority; 2019.
- Uppskjuten cancervård, Jämförelse av antalet nyregistrerade cancerfall under covid-19-pandemin 2020 och motsvarande period 2019. Published Sep 27, 2020. Fastställd av Regionala cancercentrum i samverkan.
- Northern Ireland pathology reports. Available from: https://www.qub.ac.uk/research-centres/nicr/FileStore/PDF/Covid19/Filetoupload,986705,en.pdf.
- Kaufman HW, Chen Z, Niles J, et al. Changes in the number of US patients with newly identified cancer before and during the Coronavirus Disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;33(8):e2017267.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395(10223):507–513.
- Williamson EJ, 1, Walker AJ, 2,Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584(7821):430–436.
- Danish Health Authorities, LPR3 datakvalitetsrapport 11th July 2020. Available from: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygedomme-laegemidler-og-behandlinger/landspatientregisteret/landspatientregisteret-moderniseres.
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 2020;371:m4087.
- Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034.
- Cacciapaglia G, Cot C, Sannino F. Second wave COVID-19 pandemics in Europe: a temporal playbook. Sci Rep. 2020;10(1):15514.
