Background
Human papilloma virus (HPV) is a well-established aetiological factor in oropharynx cancer (OPC) [Citation1,Citation2] and the global variation in the incidence of HPV + OPC is considerable. Countries with high age standardized incidence rates of the disease are located in Northern America and Europe [Citation3]. The prevalence of HPV among OPC is high in Denmark [Citation4] and a significant increase in the incidence of the disease has been observed over the last 40 years [Citation2,Citation5]. Previous randomised trials consistently demonstrated a very strong, independent prognostic impact of HPV-associated p16-expression, an established surrogate for tumour HPV in OPC, on outcome following definitive radiotherapy (RT) in OPC [Citation6–8]. However, infection with HPV is not restricted to oropharynx and high-risk HPV, predominantly HPV-16, has been found in squamous cell carcinoma from all head and neck sites although with a significantly higher prevalence in OPC compared to tumours arising outside the oropharyngeal region [Citation9,Citation10]. Moreover, outside OPC, the correlation between HPV and p16-expression is less robust and the prognostic significance of both markers seems less obvious.
A previous analysis on DAHANCA patients treated with definitive (chemo) radiation found no prognostic impact of p16-expression in non-OPC [Citation11], but other groups have reported conflicting findings [Citation12,Citation13]. Partly, this disagreement in observations can be explained by differences in patient populations, tumour-sites and treatment strategies among the studies. However, variations in the applied HPV detection methods also need to be taken into consideration and combined assays may represent a way to more reliably detect biologically relevant HPV infections in archival head and neck specimens, as proposed by Smeets et al. [Citation14].
With this study, we wanted to investigate the correlation between HPV and p16-expression in advanced larynx and hypopharynx cancer and furthermore to analyse the potential prognostic impact of both markers on overall survival after primary, curatively intended radiotherapy.
Materials/methods
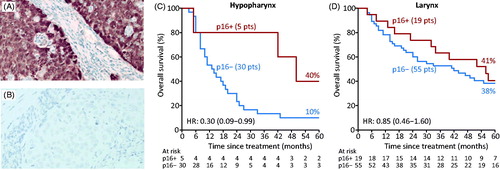
By use of the DAHANCA-database, we identified patients with stage III-IV larynx and hypopharynx cancer treated with definitive radiotherapy according to DAHANCA guidelines between 1986 and 2006. Pre-treatment tumour blocks were evaluated by immunohistochemistry for p16-expression and classified as positive in case of strong cytoplasmatic and nuclear staining in >70% of tumour cells and in consideration of the typical microscopic appearance of an HPV-related tumour [Citation15] (). HPV DNA and RNA was analysed by qPCR using specific primer sets for HPV16 E6 and E7 and HPV18 E6 and E7. Internal reference genes were ERV3-1 and HBB for DNA and ACTR3, NDFIP1, and RPL37A for RNA. Overall survival was estimated by the Kaplan–Meier product-limit analysis and hazard ratio (HR) was estimated using Cox proportional hazards models.
Results
A total of 109 patients were eligible including 74 patients with larynx cancer and 35 with hypopharynx cancer. p16-expression was found in 26% (19/74) of larynx cancers and 14% of hypopharynx cancers (5/35). Patient- and tumour characteristics stratified by site and p16-status are shown in . As can be seen, the five patients with p16- positive hypopharynx cancers were younger than the remaining part of the cohort, with a median age of 50 years, and the tumours all originated in the piriform sinus with no apparent involvement of the lateral pharyngeal wall nor overlapping into the oropharynx.
Table 1. Patient and tumour characteristics stratified by site and p16-status.
In hypopharynx all p16-positive tumours were also positive for both HPV DNA and RNA. Of the 19 p16-positive larynx cancers only 1 specimen was HPV DNA and RNA positive and 1 was HPV DNA positive but RNA negative. Only HPV subtype 16 was detected in case of HPV positivity. All p16-negative tumours were HPV-negative, regardless of tumour site. In univariate analysis overall survival was significantly associated with HPV/p16-status in hypophaynx: HR: 0.30 [95% CI: 0.09-0.99], which was maintained when adjusted for gender, median age and stage (HR:0.30 [0.09-0.97]), whereas in tumours of laryngeal origin no prognostic impact of p16-status was found: univariate HR 0.85 [0.46–1.60] ().
Discussion
In this study, we confirm the poor correlation between HPV DNA/RNA and p16-positivity in larynx cancer and accordingly no prognostic impact of p16-status on overall survival. On the contrary, we observed a strong correlation between HPV16 DNA/RNA and p16-expression in hypopharynx cancer, where our findings indicate a prognostic impact of the markers on overall survival after primary RT, comparable to what is seen in OPC. Whether this observation can be ascribed to the existence of ectopic tonsillar/lymphoid tissue in the hypopharynx remains debateable, but we find that there is a need for more investigation into the subject in order to properly define the group of patients with HPV-associated tumours and favourable prognosis, both in oropharynx and hypopharynx. Consequently, this finding suggests that optimisation of an HPV detection method with prognostic implications in head and neck squamous cell carcinomas comprises consideration for routine HPV/p16-testing of hypopharynx cancers. Ultimately, this may have implications for refinement and individualisation of treatment strategies for patients with hypopharynx cancer based on tumour HPV-status, similar to the ongoing investigation in oropharynx cancer.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709–720.
- Lassen P. The role of human papillomavirus in head and neck cancer and the impact on radiotherapy outcome. Radiother Oncol. 2010;95(3):371–380.
- de Martel C, Plummer M, Vignat J, et al. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664–670.
- ICO. Human Papillomavirus and Related Diseases Report 2016.
- Overgaard J, Jovanovic A, Godballe C, et al. The Danish head and neck cancer database clinical epidemiology series on clinical quality databases in Denmark. Clin Epidemiol. 2016;8:491–496.
- Lassen P, Eriksen JG, Hamilton-Dutoit S, et al. Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J Clin Oncol. 2009;27(12):1992–1998.
- Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35.
- Lassen P, Lacas B, Pignon JP, et al.; MARCH Collaborative Group. Prognostic impact of HPV-associated p16-expression and smoking status on outcomes following radiotherapy for oropharyngeal cancer: The MARCH-HPV project. Radiother Oncol. 2018;126(1):107–115.
- Kreimer AR, Clifford GM, Boyle P, et al. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: A systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14(2):467–475.
- Isayeva T, Li Y, Maswahu D, et al. Human papillomavirus in non-oropharyngeal head and neck cancers: a systematic literature review. Head and Neck Pathol. 2012;6(S1):104–120.
- Lassen P, Primdahl H, Johansen J, et al. Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother Oncol. 2014;113(3):310–316.
- Chung CH, Zhang Q, Kong CS, et al. P16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol. 2014;32(35):3930–3938.
- Marshall DC, Kao DD, Bakst R, et al. Prognostic role of human papilloma virus status in hypopharyngeal squamous cell carcinoma. Laryngoscope Investig Otolaryngol. 2020;5(5):860–867.
- Smeets SJ, Hesselink AT, Speel E-JM, et al. A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int J Cancer. 2007;121(11):2465–2472.
- Lassen P, Overgaard J. Scoring and classification of oropharyngeal carcinoma based on HPV-related p16-expression. Radiother Oncol. 2012;105(2):269–270.