Abstract
Background
Complete macroscopic resection without any residual tumour after completion of surgery is a strong prognostic factor in advanced epithelial ovarian cancer (EOC). It has previously been reported that surgery performed later in the week is associated with failure to achieve complete macroscopic resection. Our objective was to examine if weekday of surgery influences oncologic outcome.
Materials and Methods
This population-based observational study included 100% of all women diagnosed with advanced-stage invasive epithelial ovarian cancer between 2009–2011 and 2014–2016 in the Stockholm/Gotland County of Sweden. The association between weekday of surgery and survival was analysed with proportional hazards regression yielding hazard ratios (HR) with 95% confidence intervals (CI), adjusted for predefined confounders.
Results
Out of 1066 identified women, 524 with advanced stage EOC treated with surgery were included in the final analysis. Surgery performed Wednesday to Thursday was associated with an increased hazard of death (HR 1.28, 95% CI 1.04–1.58, p-value 0.02). The trend of the hazard of surgery performed throughout the week from Monday through Thursday was also significant (p = 0.01).
Conclusion
The increased mortality associated with surgery that is performed later in the week suggests that surgery for advanced ovarian cancer is best conducted early in the week.
Introduction
The hallmark of epithelial ovarian cancer (EOC) is exfoliation to the peritoneal cavity with extensive shedding of the tumour to the peritoneum. For this reason, the majority of patients with EOC are diagnosed at an advanced stage with a dismal prognosis [Citation1,Citation2]. It is well-established that cytoreductive surgery followed by adjuvant platinum-based chemotherapy offers the best chance of prolonged survival [Citation3–6]. Complete macroscopic resection without any remaining residual tumour after completion of surgery is the strongest prognostic factor associated with favourable survival [Citation3,Citation7–10]. To achieve complete macroscopic resection, extensive surgery including multiple organ resections and large resections of the peritoneum is often required [Citation11–14]. Accordingly, a proficient surgical team with high endurance is imperative. It has been suggested that high-volume surgeons and centres increase the chance of favourable oncologic outcomes [Citation15–17]. Consequently, structural efforts have been made including policy changes to centralise complex cancer surgery and to increase surgical proficiency [Citation4,Citation18].
To assess oncologic outcome after any type of oncologic treatment is an essential and instinctive ascertainment of the quality or improvement of care. In contrast, when treatment is provided has not been evaluated to the same extent.
The “weekday effect” with higher morbidity and mortality when surgery is performed later in the week, particularly in complex and advanced procedures has been reported previously [Citation19–25]. Similarly, in advanced EOC, it has been suggested that cytoreductive surgery performed later in the week is associated with failure to achieve complete macroscopic resection [Citation26]. Nevertheless, if this association remains with survival as the outcome is yet to be investigated.
For this reason, our objective was to investigate the association between weekday of surgery and survival in women with advanced EOC with the hypothesis that surgery performed earlier in the week is associated with a better prognosis.
Patients and methods
This was an observational cohort study. Since 2004, all women with suspected EOC in the Stockholm–Gotland region in Sweden (2.4 million inhabitants), irrespective of which primary treatment is eligible for the individual patient, are referred to Karolinska University Hospital (KUH). Moreover, cancer care is publicly accessible for all residents in Sweden and no privately funded cancer care, by insurance or else, is available. The study was regarded as quality assurance and deemed exempt from review by the Regional Ethics Committee at Karolinska Institutet.
Patients
The included patients of this study were identified through the Stockholm Ovarian Cancer Project (STOOVCA), a registry-based observational cohort study to examine the effect on survival when abruptly changing surgical treatment algorithm in a population to upfront and ultra-radical surgery [Citation27]. Women with International Federation of Obstetrics and Gynaecology (FIGO) stages III and IV epithelial ovarian/fallopian tube/peritoneal cancer and cancer in the abdomen of unknown origin (epithelial ovarian cancer without a biopsy specifically from the adnexa) diagnosed between 2009–2011 and 2014–2016 and reported to the Swedish Quality Registry of Gynaecologic Cancer (SQRGC) were identified (2012–2013 were excluded and considered a washout period for surgical proficiency) and women scheduled for elective surgery were selected.
Women registered with invasive ovarian cancer in the National Cancer Registry (NCR) were cross-checked to the SQRGC with 100% coverage. Details on the registries, topographic and morphological ICD codes, validation of data, and how the final dataset was established are presented in considerable detail in the previous publication [Citation27]. The date of diagnosis was retrieved from the NCR and the status of survival was controlled against the Swedish Population Registry.
Exposure variable
The explanatory variable investigated was weekday of surgery categorised as early- (Monday to Tuesday) or late (Wednesday to Thursday) in the week or per weekday except for Friday (Monday, Tuesday, Wednesday, Thursday).
Outcome variable
Overall survival, collected from the Swedish Population Registry until 30 October 2020
Co-variables
Confounding variables were predefined and chosen based on known clinical association with survival; age in years, FIGO stage, the timing of surgery (upfront or after neoadjuvant chemotherapy), complete macroscopic resection, adjuvant chemotherapy, histologic subtype, operation time, Charlson comorbidity Index, Surgical Complexity Score (SCS) according to the Mayo clinic nomenclature and American Society of Anaesthesiologists physical status classification (ASA-score) [Citation28–30].
Statistical analyses
Descriptive statistics are presented with numbers and proportions, medians, and interquartile ranges (IQR) as appropriate. Distributional differences in clinical factors between women in whom surgery was performed early vs. late in the week were tested with Fisher’s exact test for categorical variables and Mann–Whitney U test for continuous variables.
The basic clinical model of the association between the predefined clinical factors and outcome consists of age (<60 vs. 60–69 and > 70), FIGO stage (IV vs. III), the timing of surgery (upfront vs. interval), complete macroscopic resection (yes vs. no), adjuvant chemotherapy (yes vs. no), histologic subtype (serous adenocarcinoma vs. other histologic subtypes), operation time (< 2.5 h vs. 2.5–4.5h and > 4.5 h), Charlson comorbidity index (0 vs. ≥ 1), SCS (continuous), ASA score (I-II vs. III-IV). Uni- and multivariable modelling of time to death was performed with proportional hazards regression. The proportional hazards assumption was tested in all included clinical variables, if the assumption was not met, the variable was included as strata in the final model. The reference categories for the exposure were set to Monday–Tuesday or Monday. The results from the models are presented as hazard ratios (HR) with associated 95% confidence intervals (CI) and Wald p-values. The median follow-up time was estimated with the reversed Kaplan–Meier method. The significance level was set to 5% and all reported p-values are two-sided. All statistical analysis was performed using the statistical software Stata version 16.
Results
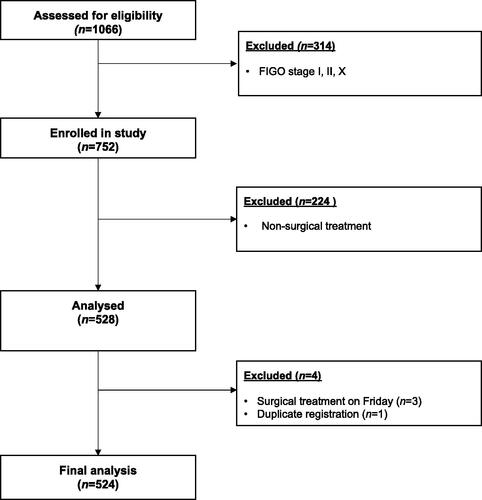
Between 2009–2011 and 2014–2016, 1066 women diagnosed with invasive EOC were assessed for inclusion and 752 women with FIGO stages III and IV were included, see . Of these women, 224 received non-surgical treatment and were excluded. Of the 528 women receiving surgical treatment, one duplicate registration was excluded and three women with surgery performed on a Friday were excluded, leaving 524 women for the final analysis ().
Figure 1. Selection of women for analysis from the Swedish Quality Registry of Gynaecologic Cancer. n: number; FIGO: International Federation of Gynaecology and Obstetrics. FIGO stage X refers to women in which stage has not been reported to the Swedish Quality registry of Gynaecologic Cancer.
Surgery was performed on Monday to Tuesday in 270 women whereas 254 women had surgery on a Wednesday to Thursday. A larger proportion of women subjected to surgery early in the week received adjuvant chemotherapy (99% vs. 95%), see . In the early-week group, three women did not receive adjuvant chemotherapy owing to; the patient’s own wish (n = 2) and postoperative deterioration/comorbidities deemed not compatible with adjuvant chemotherapy (n = 1). The corresponding number for the late week group was 13, reasons being; patient’s own wish (n = 4), postoperative deterioration/comorbidities deemed not compatible with adjuvant chemotherapy (n = 5), postoperative severe complications (n = 2) postoperative death (n = 1), moreover, in one patient it was decided that treatment for synchronous lung cancer should be prioritised after surgery for advanced ovarian cancer (n = 1).
Table 1. Characteristics of 524 women subjected to surgery for advanced epithelial ovarian cancer between 2009–2011 and 2014–2016 in the Stockholm/Gotland region of Sweden.
There were no other distributional differences in clinical characteristics between the groups (). The Median follow-up time was 6.2 years (minimum 3.7, maximum 11.8).
Crude survival for surgery performed early and late in the week and for each weekday separately is presented in . The 5-year overall survival (OS) was 34% (95% CI: 29–40) when surgery was performed early in the week (Monday to Tuesday) as compared to 29% (95% CI: 22–34) later in the week (Wednesday to Thursday), yielding an absolute difference in survival at 5 years of −7% (). For each weekday the 5-year OS was: Monday 42% (95% CI: 31–52), Tuesday 31% (95% CI: 24–38), Wednesday 28% (95% CI: 21–36), Thursday 26% (95% CI: 18–34), yielding an absolute difference in survival at 5 years between surgery performed Monday vs. Thursday of −16% ().
Figure 2. Kaplan–Meier curves of crude survival of 524 women after surgery for advanced epithelial ovarian cancer between 2009–2011 and 2014–2016 in Stockholm/Gotland County in Sweden. (A) Surgery performed Monday to Tuesday compared with Wednesday to Thursday (B) Surgery performed each weekday (Monday through Thursday).
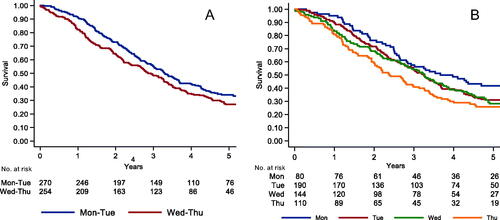
The uni- and multivariable regression analyses are presented in . In the adjusted analysis, the hazard of death increased by 28% (Hazard Ratio (HR) 1.28, 95% CI 1.04–1.58, p-value 0.02) if surgery was performed on a Wednesday to Thursday compared with Monday to Tuesday. When examining each weekday separately, surgery performed on Thursday as compared to Monday increased the adjusted hazard for death close to significantly (HR 1.42. 95% CI 0.98–2.06, p = 0.06). However, the trend of weekday of surgery from Monday through Thursday increased the adjusted hazard of death significantly (p = 0.01).
Table 2. Association between weekday of surgery and hazard of death in women with advanced epithelial ovarian cancer in the Stockholm/Gotland Region of Sweden.
Discussion
Our results indicate an independent association between weekday of surgery and hazard of death, where surgery performed early in the week confers the best survival.
It has previously been suggested that elective surgery performed later in the week or on the weekend is associated with an increased risk of short-term mortality and that cancer surgery performed later in the week may have a detrimental effect on prognosis [Citation19,Citation21,Citation23].
A previous population-based report investigated the association between weekday of surgery and survival in 10 differently categorised cancers including “ovary/uterus” [Citation24]. No “weekday effect” for cancer of the “ovary/uterus” was evident in contrast to cancer with origin in the gastrointestinal tract. However, it is highly invalid to group cancer of the ovary and uterus into one category, where the latter is often diagnosed at an early stage and requires much less complex surgical procedures, contrasting advanced EOC [Citation31]. On the other hand, Njølstad et al. investigated the “weekday effect” in a prospective cohort of >1000 women with endometrial cancer from 10 different countries and found an increased hazard of death, especially in advanced stages or with more complex surgery [Citation25].
The reasons behind the adverse outcomes associated with the “weekday effect” remain unknown. However, speculative explanations include reduced alertness of the surgeon during the week, that serious postoperative complications most often occur within 48 h (i.e., during the weekend if surgery is performed later in the week with a poorer availability of service and reduced staffing) or clinical selection bias with more frail patients scheduled for surgery later in the week [Citation21,Citation32,Citation33]. Data on postoperative complications is lacking in our study, however, the previously presented very low short-term mortality (1 < 30 days, 1 < 60 days, 2 < 90 days) may serve as a proxy for severe postoperative complications [Citation27].
The present study included only women with advanced stages of EOC where surgery is complex, unstandardised, and physically demanding. In addition, there is a need for continuous risk-benefit considerations during the course of the surgical procedure requiring both a high mental and physical stamina. Decreased surgeon alertness or exhaustion during the course of the week is therefore expected. Moreover, our study corroborates a previous report suggesting an association between the “weekday effect” and failure to achieve complete macroscopic resection [Citation26]. In the setting of the present study, the surgical team comprises few surgeons who perform surgeries from two to all days of the week and randomly without any defined weekdays for any surgeon. However, the workload of a surgeon does not only include surgeries, in fact, all other aspects included in caring for women with malignancies (in-patient care, out-patient care, multidisciplinary decisions, emergency complications and administration) may be even more strenuous. These factors combined are difficult to quantify. For these reasons, our findings may not be applicable to other organisational settings. Furthermore, the perioperative team also include staff in the operating theatre, postoperative- and in-patient ward, including anaesthesiologist. Their workload and experience may also affect the outcome, as recently suggested [Citation34]. In any case, a well-rested state with a balanced distribution of the workload during the course of the week should be a priority in all health care settings.
It may not feasible to conduct a randomised controlled trial to investigate the “weekday effect” and there are certainly limitations to our study mainly about its observational and retrospective design, leaving possibilities for selection bias, confounding and loss to follow-up. However, these concerns have been addressed to the best of our ability. Selection bias has been minimised by the population-based design accounting for all women with advanced EOC in the population in contrast to a sample of the population. By utilising the Swedish population-based registries and unique personal identification numbers to cross-check the registries, there was no loss to follow-up. Moreover, the exposure variable investigated (weekday of surgery) and outcome (death/survival) are accurate. In addition, all known potential confounders were controlled for with few missing data. In combination with the unique setting where the entire population was treated at one tertiary referral centre by the same team of surgeons, a high internal validity must be expected. Nonetheless, the generalisability may only extend to similar surgeon workload, health care systems, and settings.
In conclusion, our results indicate that surgery for advanced EOC conducted later in the week is associated with a detrimental effect on survival and for this reason suggests that women would benefit from surgery scheduled early in the week. Before any definitive clinical recommendation to reschedule surgery, our results need to be confirmed in a similar setting. At the same time, rescheduling should not be a demanding task with any associated health care costs or need of structural changes in any health care system.
Acknowledgements
We would like to thank the Swedish Quality Registry of Gynaecologic Cancer including the Regional Cancer Centre in Stockholm/Gotland, The Swedish National Board of Health and Welfare and all colleagues who have been collecting the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA A Cancer J Clin. 2020;70(1):7–30.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
- Bookman MA, Brady MF, McGuire WP, et al. Evaluation of new platinum-based treatment regimens in advanced-stage ovarian cancer: a phase III trial of the gynecologic cancer intergroup. J Clin Oncol. 2009;27(9):1419–1425.
- Querleu D, Planchamp F, Chiva L, et al. European society of gynaecologic oncology quality indicators for advanced ovarian cancer surgery. Int J Gynecol Cancer. 2016;26(7):1354–1363.
- Wright AA, Bohlke K, Armstrong DK, et al. Neoadjuvant chemotherapy for newly diagnosed, advanced ovarian cancer: society of gynecologic oncology and American society of clinical oncology clinical practice guideline. Gynecol Oncol. 2016;143(1):3–15.
- Rauh-Hain JA, Melamed A, Wright A, et al. Overall survival following neoadjuvant chemotherapy vs primary cytoreductive surgery in women with epithelial ovarian cancer: analysis of the national cancer database. JAMA Oncol. 2017;3(1):76–82.
- Aletti GD, Dowdy SC, Gostout BS, et al. Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol. 2006;107(1):77–85.
- Chi DS, Eisenhauer EL, Lang J, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol. 2006;103(2):559–564.
- Vergote I, NCIC Clinical Trials Group, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363(10):943–953.
- Du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the arbeitsgemeinschaft gynaekologische onkologie studiengruppe ovarialkarzinom (AGO-OVAR) and the groupe d'Investigateurs nationaux pour les etudes des cancers de l'Ovaire (GINECO. Cancer. 2009;115(6):1234–1244.
- Harter P, Sehouli J, Lorusso D, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Engl J Med. 2019;380(9):822–832.
- Eisenhauer EL, Abu-Rustum NR, Sonoda Y, et al. The addition of extensive upper abdominal surgery to achieve optimal cytoreduction improves survival in patients with stages IIIC-IV epithelial ovarian cancer. Gynecol Oncol. 2006;103(3):1083–1090.
- Peiretti M, Bristow RE, Zapardiel I, et al. Rectosigmoid resection at the time of primary cytoreduction for advanced ovarian cancer. A multi-center analysis of surgical and oncological outcomes. Gynecol Oncol. 2012;126(2):220–223.
- Zapardiel I, Peiretti M, Zanagnolo V, et al. Splenectomy as part of primary cytoreductive surgery for advanced ovarian cancer: a retrospective cohort study. Int J Gynecol Cancer. 2012;22(6):968–973.
- Bristow RE, Santillan A, Diaz-Montes TP, et al. Centralization of care for patients with advanced-stage ovarian cancer: a cost-effectiveness analysis. Cancer. 2007;109(8):1513–1522.
- Leandersson P, Granåsen G, Borgfeldt C. Ovarian cancer surgery - a population-based registry study. Anticancer Res. 2017;37(4):1837–1845.
- Dahm-Kähler P, Palmqvist C, Staf C, et al. Centralized primary care of advanced ovarian cancer improves complete cytoreduction and survival – a population-based cohort study. Gynecol Oncol. 2016;142(2):211–216.
- RCC. Nationellt Vårdprogram Epitelial Äggstockscancer; Underlag för nivåstrukturering: Regionalt Cancer Centrum; 2019. Available from: https://kunskapsbanken.cancercentrum.se/diagnoser/aggstockscancer-epitelial/vardprogram/underlag-for-nivastrukturering/.
- Aylin P, Alexandrescu R, Jen MH, et al. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ. 2013;346:f2424.
- Zare MM, Itani KM, Schifftner TL, et al. Mortality after nonemergent major surgery performed on friday versus monday through wednesday. Ann Surg. 2007;246(5):866–874.
- McIsaac DI, Bryson GL, van Walraven C. Elective, major noncardiac surgery on the weekend: a population-based cohort study of 30-day mortality. Med Care. 2014;52(6):557–564.
- Li R, Leng AM, Liu T, et al. Weekday of surgery affects postoperative complications and long-term survival of Chinese gastric cancer patients after curative gastrectomy. Biomed Res Int. 2017;2017:5090534.
- Lagergren J, Mattsson F, Lagergren P. Weekday of esophageal cancer surgery and its relation to prognosis. Ann Surg. 2016;263(6):1133–1137.
- Lagergren J, Mattsson F, Lagergren P. Weekday of cancer surgery in relation to prognosis. Br J Surg. 2017;104(12):1735–1743.
- Njølstad TS, Werner HM, Marcickiewicz J, et al. Late-week surgical treatment of endometrial cancer is associated with worse long-term outcome: Results from a prospective, multicenter study. PLoS One. 2017;12(8):e0182223.
- Palsdottir K, Joneborg U, Hasselgren E, et al. Surgery performed later in the week is associated with failure to achieve complete radical surgical resection in advanced ovarian cancer. Acta Oncol. 2020;59(7):760–765.
- Falconer H, Joneborg U, Krawiec K, et al. Ultra-radical upfront surgery does not improve survival in women with advanced epithelial ovarian cancer; a natural experiment in a complete population. Gynecol Oncol. 2020;159(1):58–65.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- Aletti GD, Dowdy SC, Podratz KC, et al. Relationship among surgical complexity, short-term morbidity, and overall survival in primary surgery for advanced ovarian cancer. Am J Obstet Gynecol. 2007;197(6):676.e1-7–676.e7.
- Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status – historical perspectives and modern developments. Anaesthesia. 2019;74(3):373–379.
- RCC. Nationellt vårdprogram Endometriecancer: Regionalt Cancer Centrum; 2020. Available from: https://kunskapsbanken.cancercentrum.se/globalassets/cancerdiagnoser/gynekologi/livmoderkroppscancer/vardprogram/nationellt-vardprogram-endometriecancer.pdf.
- Cavaliere F, Conti G, Costa R, et al. Intensive care after elective surgery: a survey on 30-day postoperative mortality and morbidity. Minerva Anestesiol. 2008;74(9):459–468.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668.
- Hallet J, Jerath A, Turgeon AF, et al. Association between anesthesiologist volume and short-term outcomes in complex gastrointestinal cancer surgery. JAMA Surg. 2021;156(5):479–487.
