 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Days Alive and Out of Hospital (DAOH) is a recently introduced, readily obtainable postoperative outcome measure method that expresses procedure and disease-associated morbidity and mortality. In this study, we evaluated DAOH with 30- and 365-days follow-up periods after primary surgery (DAOH30 and DAOH365, respectively) for patients with oral cavity squamous cell carcinoma (OSCC). The aim of this study is to identify patient-, procedure- and disease-associated risk factors for patients treated with primary surgery for primary OSCC.
Material and methods
This retrospective cohort study from a prospective collected database represents patients from Eastern Denmark surgically treated for primary OSCC in the period 2000–2014. DAOH30 and DAOH365 were calculated and associations with patient characteristics including comorbidity, tumor characteristics, clinical outcomes such as length of stay, readmission, and mortality were evaluated. Tests for difference and significance between groups were assessed with Mann–Whitney U test and quantile linear regression.
Results
We included 867 patients (63% males, median age: 63 years (IQR 56–70 years)). Median DAOH30 and DAOH365 after OSCC surgery were 25 days (IQR 21–27 days) and 356 days (IQR 336–360 days), respectively. Alcohol consumption had a significant association with a lower DAOH365, p < 0.01, but not with DAOH30. Advanced T-stage, adjuvant radiotherapy (RT) and increased Charlson Comorbidity Index (CCI) score was significantly associated with a lower DAOH30 and DAOH365.
Conclusion
In this population-based study in OSCC patients treated with primary surgery, we found that DAOH after 30 days was 25 days (83%), while DAOH after 365 days was 356 days (98%). Advanced T-stage acts as a predictor for significant DAOH30 and DAOH365 reduction while excessive alcohol consumption predicts a significant DAOH365 reduction. Readmission within 30 days following surgery was associated with further readmission within one year.
Introduction
Cancer of the oral cavity is one of the most frequent malignancies, and with 405,000 new cases per year, oral squamous cell carcinoma (OSCC) is the sixth most common malignancy worldwide [Citation1–4]. Although surgical techniques and multimodal therapy have improved, the survival rates among patients undergoing OSCC surgery have not changed significantly in the last decade, with 5-year survival rates of 50% [Citation5–7]. Peri- and postoperative complications are yet dominating factors impairing patient recovery resulting in prolonged hospital stay, hospital readmission, and reduced survival [Citation8,Citation9].
Postoperative complications occur in up to 28% of all patients undergoing surgery for OSCC [Citation10]. A commonly used method to report postoperative complications is the Clavien-Dindo Classification system, where the complications are evaluated and graded from I-V according to severity [Citation11]. However, simply grading postoperative complications is unlikely to capture the full patient experience and patients’ recovery after surgery [Citation12]. As a result, a variety of outcome measures have been proposed to quantify the patients perceived postoperative experience, and only a few provide a strong and patient-centered perspective of effective and efficient postoperative care needed in value-based healthcare [Citation12–16]. Recent studies have documented that patients consider readmission due to postoperative complications as a major issue resulting in reduced quality of life and loss of independence, and is a strong predictor of postoperative mortality in elderly patients [Citation9, Citation17–20].
Days Alive and Out of Hospital (DAOH) is a measure of days spent in the hospital following index surgery and has been shown to be a readily obtainable and efficient patient-centered outcome measure in perioperative clinical trials [Citation8, Citation21]. DAOH has previously been described in patients undergoing transoral robotic surgery for oropharyngeal cancer [Citation22,Citation23], but never in patients surgically treated for OSCC. DAOH was first introduced in studies on heart disease and stroke [Citation24,Citation25] but has also proved a strong correlation between postoperative complications and fewer days at home in patients undergoing a wide variety of surgical procedures [Citation8,Citation9, Citation21, Citation26–28]. DAOH provides a measure to detect clinically important differences in outcome, including primary length of hospital stay (LOS), readmission to hospital, and death [Citation29,Citation30]. DAOH is highly sensitive to comorbidity, differences in surgical risk, and the impact of perioperative complications and is also associated with mortality up to 1 year after surgery [Citation9]. DAOH has been used to report on the postoperative course up to 30 and 90 days after surgery but rarely with 365 days follow-up.
The aim of this study was to evaluate DAOH following primary surgery for OSCC (DAOH30 and DAOH365) to describe the disease and procedure related morbidity and mortality. Further, the association between DAOH30/365 and pre- and periprocedural factors, including comorbidity score, OSCC tumor stage, N-stage, adjuvant radiotherapy (RT), LOS, readmission, reoperation, and mortality, were analyzed.
Materials and methods
This retrospective cohort study was conducted on patients treated with primary surgery identified through the Copenhagen Oral Cavity Squamous Cell Carcinoma (COrCa) database [Citation31]. The COrCa database contains information on all OSCC patients diagnosed in Eastern Denmark in the period 2000–2014. Additional patient information was obtained from the Central Population Registry (CPR), Danish National Patients Register (NPR), the Danish Cancer Registry (DCR), and the Danish Cause of Death Register (DAR). CPR contains information on gender, date of birth, and vital status linked to a unique civil registration number assigned to every individual in Denmark upon birth or immigration [Citation32]. NPR contains information on all registered hospital contacts in Denmark since 1946, including inpatient consultations, medical and surgical procedures, and diagnosis codes in accordance with the International Classification of Disease, which was registered using the 10th edition (ICD-10) [Citation33]. DAR contained information on the assumed causative cause of death among all citizens dying in Denmark, classified according to the ICD-10 codes, and was used in the analysis of DAOH30/365. The quality of the information entered in the DAR relies upon the accuracy of the physician’s notifications hence subject to uncertainty [Citation34]. Data on patients treated with curative intent was extracted from the databases after required approvals from the Danish Data Protection Agency (Approval number: 05228), the Danish Health Data Authority (Approval number: 04280), and the Ethical Committee (Approval number: H-1-2014-053). Based on this data, DAOH30/365 and Charlson Comorbidity Index scores (CCI) were calculated [Citation35,Citation36] for all patients. In Denmark, residents are treated at no personal cost in the public healthcare system financed through taxes, thus stressing the unique diversity in the national databases. Due to reimbursement and mandatory reporting, all hospital contacts are reported in NPR. By law, no cancer patients are treated within the private healthcare system.
The primary outcome was DAOH30/365, and secondary outcomes were LOS, mortality, and readmissions within the 30- and 365-days follow-up period.
In order to carry out comparative testing, patients were divided into groups based on patient and tumor-specific factors listed in . Patients were grouped based on gender, age, number of pack-years of smoking, daily units of alcohol, and CCI score at the time of index surgery. Patients were further grouped according to T-stage [Citation37], UICC-stage (8th edition) [Citation38], and according to treatment modality, i.e., surgery or surgery + adjuvant RT. Patients were also grouped according to their LOS following primary surgery (<3 days, 3–5 days, 6–8 days, or more than eight days), whether they were readmitted to the hospital within the first 30 days following surgery, had recurrence, and whether reoperation was performed. Finally, patients were categorized according to the occurrence of death within the study period.
Table 1. DAOH30 and DAOH365 of patient characteristics.
Statistical analysis
Categorical data are presented as numbers with relative percentages. Continuous data are presented as means with 95% confidence intervals (CI) or medians with 25th and 75th interquartile range (IQR). Differences between groups were assessed with Mann–Whitney U test. Quantile linear regression modeling was performed to test for differences between groups with non-parametric continuous data. Statistical analyses were performed in the statistical environment R statistics version 3.5.2 [Citation39]. p < 0.05 was considered statistically significant.
DAOH is a composite measure incorporating hospital length of stay following the index surgery (day 0), readmission to either the index or any other hospital, and deaths after surgery into a single outcome metric [Citation8]. DAOH was calculated using hospitalization and mortality data from the date of the primary surgery (day 0) [Citation29].
DAOH30 was calculated by subtracting Days Alive and In Hospital within 30 days after surgery (DAIH30) and Days Dead within 30 days after surgery (DD30) from the follow-up period of 30 days.
DAIH30 was defined as the aggregate of days with an overnight stay in hospital after the day of the primary surgery and in the follow-up period of 30 days. DD30 was defined as the number of days from death to the end of the 30-days follow-up period. DAOH365 was calculated similarly to DAOH30 as described above with 365 days instead of 30 days. Outpatient hospital visits, including adjuvant RT, were not included in the DAOH30/365 calculation.
Readmission causes and postoperative complications
Readmission to the hospital within 30 and 365 days after surgery was categorized according to the cause leading to hospital admission and the related diagnosis code(s) registered during hospitalization. Each in-hospital period for a patient included one or more registrations in LPR, and each registration was affiliated with a primary diagnosis code. Registered diagnosis codes include postoperative complications causes but could also be due to other concurrent diseases or already existing comorbidities. Diagnosis codes were grouped according to type and category into five major groups defined as (I) postoperative complications, (II) malignancy, (III) cardiopulmonary, (IV) digestive system disorders, and (V) other. In every major group, subgroups were included to further specify the cause of readmission. A weighting factor, expressing how much every single major group and subgroup contributed DAOH reduction, was calculated to determine the relative impact of every readmission cause in relation to the entire postoperative course [Citation23].
Most readmissions had the diagnosis code of their primary disease co-assigned concurrently with the cause of readmission, e.g., postoperative bleeding. In the case of reoperation, the diagnosis code assigned to the readmission was also the primary disease, often not further specified. The process above was performed for both the 30 days and 365 days follow-up periods. Postoperative complications were defined as any diagnosis codes associated with the surgery within 30 days following surgery, e.g., postoperative bleeding, infection, etc.
Results
A total of 867 patients with OSCC treated with primary surgery were included in this study. The median age at surgery was 63 years (IQR 56–70 years). Only 108 (12.5%) patients were registered with no smoking history, while 266 (30.7%) patients had a history of smoking for more than 40 pack-years ( and ). A total of 198 (22.8%) patients had a history of drinking more than four units of alcohol per day. A total of 137 (15.8%) patients were readmitted with an overnight stay within 30 days after surgery. During the first 30 days following index surgery, 49 (5.7%) patients underwent reoperation for their OSCC.
Figure 1. Boxplot of Median DAOH30 for Patients- and Postoperative Characteristics. UICC: Union for international Cancer Control; CCI: Charlson Comorbidity Index; LOS: Length of (hospital) stay.
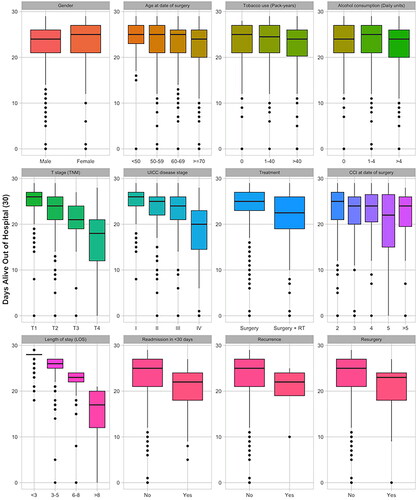
DAOH30
The median DAOH30 was 25 days (IQR 21–27 days) for the entire cohort. Patients aged above 60 years had a lower DAOH30 than patients aged under 50 years, p < 0.02. This was further confirmed through a quantile linear regression model, which found a lower DAOH30 with increasing age, p < 0.001, . No difference in DAOH30 was found according to the number of pack-years of smoking or daily alcohol intake. Lower DAOH30 was seen with increasing T-stage, and . Similarly, a lower DAOH30 was seen with increasing UICC stages, and . Patients who underwent surgery without adjuvant RT had a median DAOH30 of 25 days (IQR 23–27 days), while patients who received adjuvant RT had a median DAOH30 of 22.5 days (IQR 19–26 days), p < 0.001. Only patients with a CCI score >5 had a significantly lower DAOH30 than patients with CCI scores 2–5, p = 0.012. Concurrently, a quantile linear regression model found a significantly lower DAOH30 with increasing T- or N-stage, and CCI, . Quantile linear regression modeling found lower DAOH30 with increasing primary LOS, .
Table 2. Quantile linear regression of patient characteristics and DAOH30 and DAOH365.
We found no significant DAOH30 reduction in patients with residual malignant disease within 30 days after surgery. Patients who underwent reoperation (not further specified) for their OSCC had significantly lower DAOH30 than patients who did not undergo reoperation, p < 0.001. Reduced DAOH30 was significantly associated with six-month mortality, p < 0.001, and .
DAOH365
The median DAOH365 was 356 days (IQR 336–360 days) for the entire cohort. The fraction of patients with specified intervals of DAOH365 is seen in . Patients aged ≥ 70 years had a lower DAOH365 than patients aged under 50 years, with median DAOH365 of 354.5 days (IQR 318–360 days) and 358 days (IQR 344–361 days), respectively, p = 0.045. No difference in DAOH365 was found between groups according to the number of pack-years of smoking. A significant reduction of 1.6 days in DAOH365 was found between patients with and without alcohol consumption, and quantile linear regression modeling found a significantly lower DAOH365 with increasing alcohol consumption, p < 0.01. A significant association was seen between advanced T-stages and lower DAOH365 throughout all increasing T-stages, , and ; this was further confirmed with quantile linear regression, p < 0.001. In line with advancing T-stages, a significant association between advanced UICC stages and lower DAOH365 was seen throughout all increasing UICC stages, and . Patients who solely underwent surgery had a median DAOH365 of 358 days (IQR 349–361 days), while patients who underwent surgery with adjuvant RT had a median DAOH365 of 347 days (IQR 310–357 days), p < 0.001. Patients with a CCI score > 2 had a significantly lower DAOH365 than patients with a CCI score ≤ 2. A quantile linear regression model found a consistently lower DAOH365 with increasing CCI scores, .
Figure 2. Boxplot of Median DAOH365 for Patients- and Postoperative Characteristics. UICC: Union for international Cancer Control; CCI: Charlson Comorbidity Index; LOS: Length of (hospital) stay.
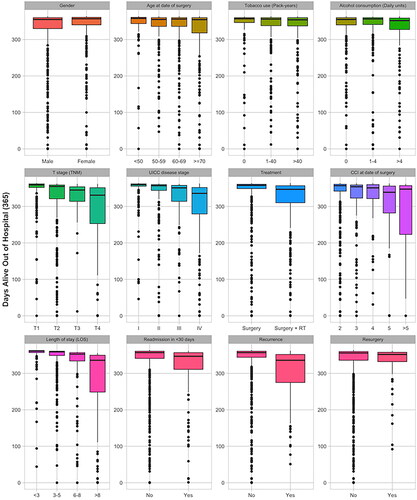
DAOH365 was significantly lower in patients with a primary LOS > 3 days compared to patients discharged within three days of hospitalization after surgery, p < 0.001. Although non-significant, patients discharged on the same day of surgery had a lower DAOH365 than patients discharged after 1 to 5 days after surgery, median DAOH365 356 days (IQR 342–365 days) and 361 days (IQR 357–363 days), p = 0.394. Quantile linear regression modeling found lower DAOH30 with increasing primary LOS, after adjusting for the primary LOS (). Patients who had a recurrence within 365 days had a significantly lower DAOH365 than patients with no recurrence, respectively 336 days (IQR 278–352 days) and 357 days (IQR 344–361 days), p < 0.001. Patients who underwent reoperation (not further specified) for their OSCC had significantly lower DAOH than patients who did not undergo reoperation, p = 0.016. Reduced DAOH365 was significantly associated with one-year mortality, p < 0.001 ( and ). Overall, 111 (12.8%) patients died within one year after surgery. Of these, 6 (0.7%) patients died within 30 days, 32 patients (3.7%) died within 180 days following surgery, while the remaining 73 patients (8.4%) died in the period 180–365 days after surgery.
Postoperative follow-up
The number of patients readmitted within 30 days following surgery was n = 137 (15.8%). Some patients had more than one readmission in the period, resulting in a total of n = 277 readmissions. The majority of readmissions, n = 179 (64.6%), within 30 days following surgery were due to a concurrent reason related to malignancy, with 172 (62.4%) readmissions due to head and neck malignancy. Forty-one readmissions (14.8%) to the hospital within 30 days following surgery were registered as diagnoses that were likely to be postoperative complications. Among these postoperative complications, postoperative infection (n = 18, 6.5%) had the highest impact, followed by postoperative bleeding (n = 12, 4.3%) on DAOH30 reduction. Other causes for readmission are listed in . The number of patients readmitted within 365 days following surgery was n = 162 (18.7%), resulting in a total of n = 919 readmissions. The majority of readmissions, n = 368 (40%) within 365 days after surgery were due to a concurrent reason related to malignancy, with head and neck malignancies being the most frequent, n = 301 (32.8%). The remaining readmission causes are seen in .
Table 3. Readmission causes within 30- and 365 days following surgery.
Discussion
This study found that the median DAOH30 and DAOH365 after OSCC surgery were 25 days (IQR 21–27 days) and 356 days (IQR 336–360 days), respectively.
While most studies have explored DAOH for a period of 30 to 90 days, several postoperative complications and poor survival manifest several months after surgery [Citation18,Citation40,Citation41]. This study suggests that a combinatory exploration of 30- and 365-days follow-up periods after surgery offers important insight into patients’ overall postoperative course and rehabilitation, including postoperative complications, recurrences, reoperation, and deaths. Where the period of 30 days provides an understanding of surgery-related factors affecting the postoperative course, the extended period of observation to 365 days captures the long-term complications after surgery that can impair quality of life [Citation42]. Previous studies have argued that, given the potential for missing data and the weight of additional work, DAOH-assessment for more than 30 days has no significant additional benefit over DAOH for 30 days [Citation9]. While other studies have argued that DAOH beyond 30 days is important in detecting time-cause differences in specific complications [Citation21,Citation40]. Databases and registries used in this study are established and maintained regional and nationwide, no additional work is required for follow-ups and the potential missing data is minimal. Therefore, we believe that a combined analysis of DAOH30 and DAOH365 yields a superior evaluation of the postoperative outcome in a well-defined timely manner. The risk of variations in overall hospital stay, from admission to discharge, can impact DAOH and can potentially constitute a bias, why standardized criteria for admission and discharge is of importance for overall trackability of the entire postoperative course.
Forty-nine patients underwent reoperation during the 30 days follow-up period. A substantial part of these are thought to be due to sentinel node biopsy (SNB), which is routinely performed at our institution and is positive in 20–30% of the patients [Citation43] and when found to be positive leads to a subsequent neck dissection. However, the data derived from national registries do not allow for detailed information regarding the indication for reoperation.
Several studies have proven a relationship between alcohol and tobacco use and the risk of OSCC development as well as increased cancer-related mortality [Citation44,Citation45]. Although approximately one-third of the patients in this study were considered heavy smokers and categorized with heavy alcohol consumption, this study found no association between the use of alcohol and tobacco, including their respective quantity and DAOH30. However, we found that alcohol consumption of more than four units per day was significantly associated with a lower DAOH365. Advanced tumor stage was, as expected, found to be significantly associated with a lower DAOH30 and DAOH365, which may suggest differences in surgical approach and hence the risk of postoperative complications as well as diverse treatment plans with adjuvant treatment offered advanced tumor stages. Patients who underwent adjuvant RT had a significant reduction in both DAOH30 and DAOH365, reflecting a higher tumor stage or deviating surgery-related factors such as positive margins and/or extracapsular spread in cervical lymph nodes. Treatment with adjuvant RT was counted as outpatient visit since the treatment is not given under hospitalization. Hence, RT treatment did not impact DAOH itself, as no DAIH was added to the calculation of DAOH, but the multimodal therapy treatment was significantly associated with lower DAOH30/365. Postoperative RT has also been shown to significantly reduce the quality of life of OSCC patients [Citation46], i.e., an indirect parameter in the measure of DAOH [Citation8].
Primary LOS was found to be significantly associated with both DAOH30 and DAOH365. Although the definition of DAOH does not allow adjustment for primary LOS, we found an association between the length of primary LOS and lower DAOH30/365, most prominent for DAOH365. Furthermore, we found that patients discharged on the same day of surgery had a slightly lower DAOH than patients discharged after 1–5 days which might suggest that too early discharge after surgery fails to capture potential postoperative complications.
Quantile linear regression found that tumor specific factors (such as TNM- and UICC-stage) affect both DAOH30 and DAOH365. Comorbidities, as measured by CCI, impacted both DAOH30&365. Comorbidity has consistently been found to have an adverse impact on treatment effectiveness and cancer survival, where studies have reported higher rates of complications in cancer patients with comorbidity [Citation47,Citation48].
We found that patients with OSCC recurrence had a significantly reduced DAOH365. Patients readmitted within 30 days after surgery had an average of approximately two readmissions per patient during the first month after surgery, while the average number of readmissions within one year was 5.7 readmissions per patient. Of all patients readmitted within one year, approximately 85% were also readmitted within the first month after surgery, suggesting readmission within the first month could be a predictor for further readmissions within one year, hence resulting in a further DAOH reduction.
Postoperative infections (other than respiratory or systemic infection) and postoperative hemorrhage had the highest impact among postoperative complications on DAOH30 reduction and hence increased morbidity. This mandates closer attention to preventing these complications in future perioperative enhancement studies since prevention of these causes will lead to the most significant improvement in DAOH30 and thereby improve treatment quality and efficiency, both from a patient-cohort and healthcare perspective. In addition, clinical attention should focus on patients with a CCI >2 (since median DAOH365 is reduced with a median of 11.6 days with each increasing CCI score), patients with heavy alcohol consumption, and patients receiving adjuvant RT since these patients are at risk of increased morbidity according to DAOH365. Future studies should strive to improve the long-term postoperative course for these patients.
The study has limitations. Since population databases and registries capture postoperative morbidity with varying accuracy and severity during the prospective registration process, the true incidence of complications might be higher. The diagnosis codes and data from the national registries might not reflect all specific complications developing under readmission, e.g., a patient readmitted with postoperative infection which develops irregular heart rhythm that prolongs the LOS will often only be registered as a postoperative infection if the patient is not transferred to another department, e.g., the cardiologic department. In cases where patients, during a continuous admission, were transferred between departments we used the diagnosis codes associated with each department to calculate the relative impact of a readmission diagnosis. Another limitation is the inability to filter out SNB followed by complete neck dissection. However, the strengths of this study include a well-described cohort of patients undergoing primary surgical treatment for primary OSCC with prospective registration of comorbidity and with a complete mandatory follow-up of hospital contacts through the regional and national databases.
In conclusion, the median DAOH30 and DAOH365 after OSCC surgery were 25 days (IQR 21–27 days) and 356 days (IQR 336–360 days), respectively. This was significantly reduced in patients with advanced tumor stages and in patients with a higher comorbidity score. Furthermore, the study found that alcohol consumption reduced DAOH365 but not DAOH30, suggesting a long-term impact on recovery but less of an impact on short-term recovery. The most common postoperative complication causes of readmission within 30 days following surgery were postoperative bleeding and infection, with the latter having the highest relative impact on the reduction of DAOH30.
Discloure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Additional information
Funding
References
- Ettinger KS, Ganry L, Fernandes RP. Oral cavity cancer. Oral Maxillofac Surg Clin North Am. 2019;31(1):13–29.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
- Montero PH, Patel SG. Cancer of the oral cavity. Surg Oncol Clin N Am. 2015;24(3):491–508.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
- Pare A, Joly A. Oral cancer: risk factors and management. Presse Med. 2017;46(3):320–330.
- Engholm G, Ferlay J, Christensen N, et al. NORDCAN—a nordic tool for cancer information, planning, quality control and research. Acta Oncol. 2010;49(5):725–736.
- Karnov KKS, Grønhøj C, Jensen DH, et al. Increasing incidence and survival in oral cancer: a nationwide danish study from 1980 to 2014. Acta Oncol (Madr). 2017;56(9):1204–1209.
- Myles PS, Shulman MA, Heritier S, et al. Validation of days at home as an outcome measure after surgery: a prospective cohort study in Australia. BMJ Open. 2017;7(8):e015828.
- Bell M, Eriksson LI, Svensson T, et al. Days at home after surgery: an integrated and efficient outcome measure for clinical trials and quality assurance. E Clin Med. 2019;11:18–26.
- Zhang C, Xi MY, Zeng J, et al. Prognostic impact of postoperative complications on overall survival in 287 patients With oral cancer: a retrospective Single-Institution study. J Oral Maxillofac Surg. 2019;77(7):1471–1479.
- Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213.
- Moonesinghe SR, Grocott MPW, Bennett-Guerrero E, Perioperative Quality Initiative (POQI) I Workgroup, et al. American society for enhanced recovery (ASER) and perioperative quality initiative (POQI) joint consensus statement on measurement to maintain and improve quality of enhanced recovery pathways for elective colorectal surgery. Perioper Med (Lond). 2017;6:6.
- Austin JM, McGlynn EA, Pronovost PJ. Fostering transparency in outcomes, quality, safety, and costs. JAMA. 2016;316(16):1661–1662.
- Lynn J, McKethan A, Jha AK. Value-Based payments require valuing what matters to patients. JAMA. 2015;314(14):1445–1446.
- Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481.
- Buggy DJ, Freeman J, Johnson MZ, StEP-COMPAC Group, et al. Systematic review and consensus definitions for standardised endpoints in perioperative medicine: postoperative cancer outcomes. Br J Anaesth. 2018;121(1):38–44.
- Hinami K, Bilimoria KY, Kallas PG, et al. Patient experiences after hospitalizations for elective surgery. Am J Surg. 2014;207(6):855–862.
- Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242(3):323–326.
- Moonesinghe SR, Harris S, Mythen MG, et al. Survival after postoperative morbidity: a longitudinal observational cohort study. Br J Anaesth. 2014;113(6):977–984.
- Pinto A, Faiz O, Davis R, et al. Surgical complications and their impact on patients’ psychosocial well-being: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e007224.
- Jørgensen CC, Petersen PB, Kehlet H, Lundbeck Foundation Center for Fast-track Hip and Knee Replacement Collaborative Group Days alive and out of hospital after fast-track total hip and knee arthroplasty: an observational cohort study in 16 137 patients. Br J Anaesth. 2019;123(5):671–678.
- Scott SI, Madsen AKØ, Rubek N, et al. Days alive and out of hospital after treatment for oropharyngeal squamous cell carcinoma with primary transoral robotic surgery or radiotherapy - a prospective cohort study. Acta Otolaryngol. 2021;141(2):193–196.
- Larsen MHH, Scott SI, Kehlet H, et al. Days alive and out of hospital a validated patient-centred outcome to be used for patients undergoing transoral robotic surgery: protocol and perspectives. Acta Otolaryngol. 2021;141(1):95–98.
- Fanaroff AC, Cyr D, Neely ML, et al. Days alive and Out of hospital: exploring a Patient-Centered, pragmatic outcome in a clinical trial of patients With acute coronary syndromes. Circ Cardiovasc Qual Outcomes. 2018;11(12):e004755.
- Yu A, Rogers E, Wang M, et al. Population-based study of home-time by stroke type and correlation with modified rankin score. Neurology. 2017;89(19):1970–1976.
- Ariti CA, Cleland JGF, Pocock SJ, et al. Days alive and out of hospital and the patient journey in patients with heart failure: insights from the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) program. Am Heart J. 2011;162(5):900–906.
- Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
- Maibom SL, Røder MA, Poulsen AM, et al. Morbidity and days alive and Out of hospital Within 90 days Following radical cystectomy for bladder cancer. Eur Urol Open Sci. 2021;28:1–8.
- Jerath A, Austin PC, Wijeysundera DN. Days alive and Out of hospital: validation of a patient-centered outcome for perioperative medicine. Anesthesiology. 2019;131(1):84–93.
- Weiser TG, Semel ME, Simon AE, et al. In-hospital death following inpatient surgical procedures in the United States, 1996-2006. World J Surg. 2011;35(9):1950–1956.
- Jensen JS, Jakobsen KK, Mirian C, et al. The copenhagen oral cavity squamous cell carcinoma database: protocol and report on establishing a comprehensive oral cavity cancer database. Clin Epidemiol. 2019;11:733–741.
- Thygesen LC, Daasnes C, Thaulow I, et al. Introduction to danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7 Suppl):12–16.
- Lynge E, Sandegaard JL, Rebolj M. The danish national patient register. Scand J Public Health. 2011;39(7 Suppl):30–33.
- Helweg-Larsen K. The danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–29.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- Sundararajan V, Henderson T, Perry C, et al. New ICD-10 version of the charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294.
- Edge SB, Compton CC. The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Vol. 17, annals of surgical oncology. Ann Surg Oncol. 2010;17(6):1471–1474.
- Kano S, Sakashita T, Tsushima N, et al. Validation of the 8th edition of the AJCC/UICC TNM staging system for tongue squamous cell carcinoma. Int J Clin Oncol. 2018;23(5):844–850.
- R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018.
- Shulman MA, Myles PS, Chan MV, et al. Measurement of disability-free survival after surgery. Anesthesiology. 2015;122(3):524–536.
- Myles PS, Peyton P, Silbert B, ANZCA Trials Group Investigators, et al. Perioperative epidural analgesia for major abdominal surgery for cancer and recurrence-free survival: randomised trial. BMJ. 2011;342:d1491.
- Linsen SS, Gellrich N-C, Kruskemper G. Age- and localization-dependent functional and psychosocial impairments and health related quality of life six months after OSCC therapy. Oral Oncol. 2018;81:61–68.
- Schilling C, Stoeckli SJ, Vigili MG, et al. Surgical consensus guidelines on sentinel node biopsy (SNB) in patients with oral cancer. Head Neck. 2019;41(8):2655–2664.
- Mayne ST, Cartmel B, Kirsh V, et al. Alcohol and tobacco use prediagnosis and postdiagnosis, and survival in a cohort of patients with early stage cancers of the oral cavity, pharynx, and larynx. Cancer Epidemiol Biomarkers Prev. 2009;18(12):3368–3374.
- Radoi L, Paget-Bailly S, Cyr D, et al. Tobacco smoking, alcohol drinking and risk of oral cavity cancer by subsite: results of a french population-based case-control study, the ICARE study. Eur J Cancer Prev. 2013;22(3):268–276.
- Rabbels J, Wyzisk M, Siessegger M, et al. Quality of life of patients with squamous cell carcinoma of the oral cavity. Mund Kiefer Gesichtschir. 2005;9(5):300–305.
- Sarfati D, Koczwara B, Jackson C. The impact of comorbidity on cancer and its treatment. CA Cancer J Clin. 2016;66(4):337–350.
- Sogaard M, Thomsen RW, Bossen KS, et al. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013;5(Suppl 1):3–29.
