Introduction
Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL) [Citation1]. In early stages it presents with localized patches and/or plaques, primarily in sun protected areas. For some patients MF can progress to more advanced stages with tumors or erythroderma and increased risk of extracutaneous spread [Citation2], and a subset of patients develop transformed MF, characterized by an increased number of large cells and often CD30 positivity. MF with penile involvement is rare, with only 3 cases reported in the literature [Citation1–3], but an important differential diagnosis to consider in patients with genital dermatoses or erosions that are refractory to treatment. We present the first clinical case with transformed penile MF. It is also the first report of successful treatment of penile MF with radiation therapy.
Case
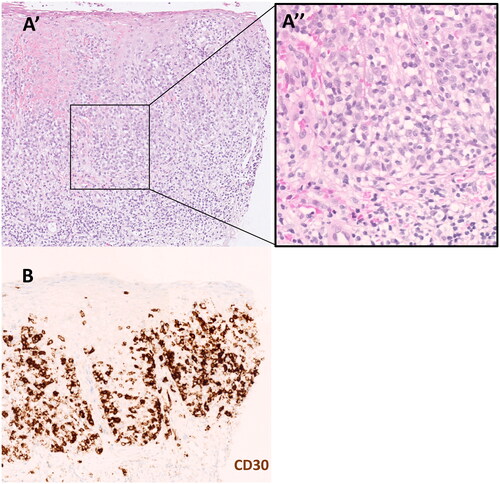
The patient is an 83-year old man followed at our dermatology clinic since 32 years ago due to MF stage IB. He had previously been treated with methotrexate, Interferon A, bath-PUVA, narrow band UVB, localized radiation therapy, Imiquimod and topical steroids. In the beginning of 2020, the patient developed erythematous plaques with a slight desquamation and erosions on the penis shaft, underneath the foreskin (). Treatment with topical steroids with an antifungal additive (triamcinolone acetonide with econazole) was used with some effect, but the rash came back as soon as the treatment was tapered. The patient was highly affected by both pain and secretion from the genital lesions. Because of the poor response to treatment and the fact that penile involvement of MF is very rare, a biopsy was taken from a plaque on the penis to confirm the diagnosis and to rule out other malignancies. PAD showed an atypical lymphocytic infiltrate dominated by CD3+CD4+ T-lymphocytes with a pronounced epidermotropism, and more than 25% large cells, consistent with MF with large cell transformation (). The large cells were diffusely positive for CD30 and mainly localized in the epidermis (), which is an unusual histological pattern [Citation5]. In line with the findings of large cell transformation, MF involvement of the genital area has been suggested to be a sign of aggressive or widespread disease [Citation2,Citation4]. However, there were no signs of systemic involvement in this patient. When the diagnosis was confirmed, stronger topical steroids (clobetasol propionate) was tried, and later systemic treatment with Acitretin, both without significant effect. The patient was therefore referred to radiation therapy of the penis shaft, 4 Gy × 2, which led to complete response in the genital area () and no side effects. The genital skin has remained healed during clinical follow-ups.
Figure 1. (A) Erythematous plaques with a slight desquamation and erosions on the penis shaft, underneath the foreskin. (B) Complete response following radiation therapy of the penis shaft, 4 Gy × 2.
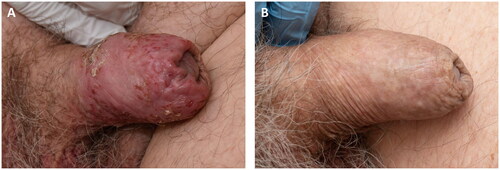
Figure 2. (A’) Hematoxylin eosin staining, magnification 19.6×, (A’’) Hematoxylin eosin staining, magnification 40×, (B) CD30 staining using standard clinical 3, 3'-diaminobenzidine (DAB) protocol at the department of pathology and cancer diagnostics, Karolinska university hospital, Stockholm, Sweden, magnification 19.2×.
Discussion
This clinical case emphasizes the importance of considering MF as a differential diagnosis in patients with genital dermatoses or erosions that are refractory to treatment or otherwise suspicious, especially in patients already diagnosed with MF. We furthermore present the first case of transformed penile MF, in support for previous speculations that genital MF might reflect a more aggressive clinical manifestation. Local radiation therapy is identified as an efficient and safe treatment option for MF also in the genital area.
Acknowledgements
The patient in this manuscript has given written informed consent to publication of his case details.
Disclosure statement
HB has received honoraria from participating in advisory boards of Kyowa Kirin in 2019 and 2022. The other authors report no conflicts of interest.
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article.
Additional information
Funding
References
- Chiam LYT, Chan YC. Solitary plaque mycosis fungoides on the penis responding to topical imiquimod therapy. Br J Dermatol. 2007;156(3):560–562.
- Schaufler C, Ferenczi K, Hegde U, et al. Complete response of penile mycosis fungoides with systemic brentuximab therapy. Urol Case Rep. 2021;34:101460.
- O’Brien JS, Manning T, Perera M, et al. Blueprint unknown: a case for multidiciplinary management of advanced penile mycosis fungoides. Can J Urol. 2017;24(6):9139–9144.
- Geller S, Pitter K, Moskowitz A, et al. Treatment of vulvar mycosis fungoides tumors with localized radiotherapy. Clin Lymphoma Myeloma Leuk. 2018;18(7):e279–e281.
- Salhany KE, Cousar JB, Greer JP, et al. Transformation of cutaneous T cell lymphoma to large cell lymphoma. Am J Pathol. 1988;132(2):265–277.
