ABSTRACT
Purpose
To examine the associations between muscular fitness (MF) and body composition.
Method
MF was assessed with three tests of FitnessGram test battery. Total body fat percentage (BF%), abdominal fat percentage (AF%) and fat-free mass (FFM) were measured by dual-energy X-ray absorptiometry (DXA). The IOTF body mass index (BMI) cut-offs were used to define healthy weight, overweight, and obesity.
Results
MF was inversely associated with BF% and AF%. The children in the moderate and high MF groups had significantly lower BF% and AF% compared with the children in the low MF group within the same BMI category. After adjusting for cardiorespiratory fitness (CRF), BMI and sex, the differences between the MF groups were significant for BF% but not for AF%.
Conclusion
There were significant inverse associations between MF and DXA -measured adiposity. Within the same BMI category, total and abdominal adiposity were lower in children with moderate or high MF than in children with low MF.
Introduction
Over the recent decades, obesity has increased among children and adolescents in most countries worldwide (Di Cesare et al., Citation2019; NCD, Citation2017; Ng et al., Citation2014). Furthermore, declines in physical activity (PA) and physical fitness have also been observed (Aubert et al., Citation2018; Fühner, Kliegl, Arntz, Kriemler, & Granacher, Citation2021; Tomkinson & Olds, Citation2007; Tremblay et al., Citation2010). This is a very worrying trend because both physical fitness and obesity are strongly related to health status in children and adolescents (Di Cesare et al., Citation2019; Ortega et al., Citation2018; Ortega, Ruiz, Castillo, & Sjöström, Citation2008). In addition, childhood obesity tends to track into adulthood, corresponding to an increased risk of cardiometabolic diseases and mortality later in life (Di Cesare et al., Citation2019; Reilly & Kelly, Citation2011; Singh, Mulder, Twisk, van Mechelen, & Chinapaw, Citation2008).
The treatment of obesity is relatively challenging, and thus the potential of physical fitness to attenuate the negative consequences of obesity has been of interest to researchers (Ortega et al., Citation2018). Certain components of physical fitness, such as cardiorespiratory fitness (CRF) and muscular fitness (MF), are considered to comprise health-related fitness (American College of Sports Medicine, Citation2018; Caspersen, Powell, & Christenson, Citation1985), and among these health-related fitness components, CRF has been studied the most. Prior studies have clearly shown that CRF is an indicator of health and is strongly associated with health outcomes, such as obesity and abdominal obesity in youth (Ortega et al., Citation2018; Raghuveer et al., Citation2020). In addition, there is evidence that increasing CRF in childhood, regardless of weight status, could reduce the risk of developing cardiometabolic health problems associated with obesity later in life (Schmidt, Magnussen, Rees, Dwyer, & Venn, Citation2016).
Less is still known about the associations between MF and obesity in childhood and in addition, most of the data available from previous studies, are based on body mass index (BMI) -defined obesity (Smith et al., Citation2014; Thivel, Ring-Dimitrioum, Weghuber, Frelut, & O'Malley, Citation2016). However, BMI is a proxy measure because it does not distinguish between fat mass and non-fat mass (Marra, Sammarco, & De Lorenzo, Citation2019), whereas dual-energy X-ray absorptiometry (DXA) is the current reference method for the assessment of body composition, providing accurate estimates of total body fat (BF), abdominal region fat (AF) and fat-free mass (FFM) (Marra et al., Citation2019). As direct measures of body composition are better indicators of adiposity and health risk (Zeng, Dong, Sun, Xie, & Cui, Citation2012) and also MF is increasingly thought to be important marker of health, understanding the associations between accurately measured adiposity and MF may contribute to the development of evidence-based interventions to prevent childhood obesity.
The aim of this population-based cross-sectional study of eight-year-old children was to examine the associations between MF and body composition assessed by DXA.
Methods
Participants
A random sample (n = 750) of eight-year-old children, born in the same year and living in Tampere, Finland, was drawn from the population register. The families of the children were mailed an invitation to participate in the study and informed of the purpose and nature of the study and its measurements. The families willing to participate in the study, responded to the invitation and booked a suitable research time for them. The voluntary children, accompanied by one of their parents, arrived at the UKK-institute research site and both gave their written informed consent upon arrival. The final sample of voluntary children, who provided complete data regarding their MF, CRF, body composition, and anthropometric measurements, consisted of 304, approximately eight years old children (151 girls and 153 boys; mean 8.6 years; range 8.2–9.2 years) The study was approved by the Ethics Committee of Pirkanmaa hospital district (the reference number: R05105).
Muscular fitness (MF) assessments
The assessment of MF was accomplished with three test items from the FitnessGram health-related fitness test battery for children and adolescents, in accordance with the instructions outlined in the test manual (Meredith & Welk, Citation2010). The chosen test items included a curl-up test, a trunk lift test, and a modified pull-up test. The curl-up test was used to assess abdominal muscle strength and endurance. This test required each participant to perform as many curl-ups as possible following a given cadence. One trial was allowed and the resulting score was the number of curl-ups correctly performed. The trunk lift test was used to assess the strength of the back extensor muscles. This test required each participant to lie prone, lift their upper body off the floor using the extensor muscles of the back, and hold that position while the distance from floor to the child’s chin was measured. The resulting score was the distance measured in centimetres. Two trials were allowed and the highest score was recorded. The modified pull-up test was used to assess upper body strength and endurance. This test required each participant to lie in a supine position with their body horizontally straight, grasp a bar placed just out of reach, and pull up toward the bar. One trial was allowed and the resulting score was the number of successfully completed modified pull-ups performed. The children arrived for MF tests in pairs and before the actual test, the children were given time to practice in pairs but performed the actual test one at a time. Attention was given by the researcher to performance technique during all the tests. Each child was assessed individually by the same experienced researcher (SS). The standardized total MF score was computed from the three test item scores. The three MF test item scores were standardized separately for both sexes, after which the different MF -variables were combined into one variable, and finally divided into the thirds of the obtained variable: low MF (the lowest third), moderate MF (the middle third) or high MF (the highest third).
Cardiorespiratory fitness (CRF) assessment
The assessment of CRF was accomplished with the 20-m shuttle run test (20-mSRT), which involves continuously running between two lines placed 20 m apart, keeping time with a recorded sound signal at a specific pace that grows faster with each minute (Leger, Mercier, Gadoury, & Lambert, Citation1988; Nevill et al., Citation2021). We have described the test procedure in detail previously (Stigman et al., Citation2009). The result of this test was a CRF score, expressed as the number of 20-m-distance laps completed by each participant.
Body composition and anthropometric measurements
The total body fat percentage (BF%), abdominal region fat percentage (AF%), and fat-free mass (FFM) of each participant were measured with DXA (GE Lunar Prodigy Advance, GE Lunar Radiation Corp., Madison, WI). Abdominal region fat, which includes intra-abdominal fat and subcutaneous fat, was evaluated at a manually delineated region of interest that included the soft tissue area of the body between the lowest ribs and the superior border of the iliac crest. Waist circumference (WC) was measured with a measuring tape, midway between the lowest rib and the superior border of the iliac crest. Height was measured to the nearest 0.1 cm and weight was determined using a high-precision electronic scale (F 150S-D2, Sartorius AG, Goettingen, Germany) to the nearest 0.1 kg, and the measurements were used to calculate BMI (kg/m2). The participants were classified as healthy weight, overweight or obese, according to the BMI cut-offs of the International Obesity Task Force (IOTF) for age and sex (Rolland-Cachera, Citation2011), as recommended by the European Childhood Obesity Group (Jin et al., Citation2020).
Statistical analysis
Means and standard deviations were calculated for all variables. Pearson’s correlation coefficient was used to assess the correlations between the variables. A one-way analysis of variance (ANOVA) was used to examine differences in participant characteristics across the MF groups. When an ANOVA result was statistically significant (p < 0.05), a Tukey’s or Tamhane’s post hoc comparison tests was used to identify specific between-group differences. The influence of MF on BF% and AF% was determined using an analysis of covariance (ANCOVA). The dependent variables (BF% and AF%) were included in the models in their original continuous scales of measurement, and MF group (low, moderate or high) was entered as a factor variable. All models included BMI, sex, and CRF as covariates, and all models were run separately for BF% and AF%. All statistical analyses were carried out using SPSS version 26.0 (IBM Corp, Armonk, NY, USA), and the level of significance was set at p = .05.
Results
According to the BMI cut-offs of the IOTF, 80.9% of the participants were of healthy weight (girls: 81.4%, boys: 80.4%), 17.1% were overweight (girls: 17.9%, boys: 16.3%) and 2,0% were obese (girls: 0.7%, boys: 3.3%).
The participant characteristics are shown in . DXA-measured body composition differed significantly by sex; specifically, girls had significantly higher BF% and AF% than boys, and boys had significantly higher FFM than girls. There were also statistically significant between-sex differences in the MF test results, in that girls were more proficient than boys in the curl-up and trunk lift tests.
Table 1. Characteristics of all the participants by sex. Means (SD).
The Pearson’s correlations coefficients between body composition (BF%, AF%, and FFM) and MF test item results and total MF scores, are shown in . When the MF test items were examined separately, the strongest correlations were found (among both sexes) between modified pull-up performance and BF% and between modified pull-up performance and AF%. Furthermore, BF% and AF% were significantly correlated with total MF scores (among both sexes). Statistically significant correlation was found between FFM and modified pull-up performance among boys.
Table 2. The Pearson’s correlation coefficient between body composition and MF test items and MF total score by sex.
shows the body composition characteristics in the low, moderate, and high MF groups by sex. Statistically significant differences in weight, BMI, and WC were found between MF groups among both sexes. Furthermore, BF% and AF% were significantly higher among both sexes in the low MF group compared with the moderate and high MF groups.
Table 3. Body composition of the girls and boys by thirds of muscular fitness (low, moderate and high MF). Means (SD).
The participants’ body composition characteristics were examined within the BMI categories (healthy weight, overweight and obese) and compared between the low, moderate, and high MF groups (). Among the healthy weight children, BF% was significantly higher in the low MF group than in the moderate and high MF groups, and AF% was significantly higher in the low MF group than in the high MF group. Among the overweight and obese children, BF% was significantly higher in the low MF group than in the moderate and high MF groups, and the AF% was significantly higher in the low MF group than in the moderate MF group. Furthermore, weight and BMI differed between the low and moderate MF groups among the overweight and obese children.
Table 4. The body composition characteristics within the BMI categories (healthy weight, overweight and obese) by the MF groups. Means (SD).
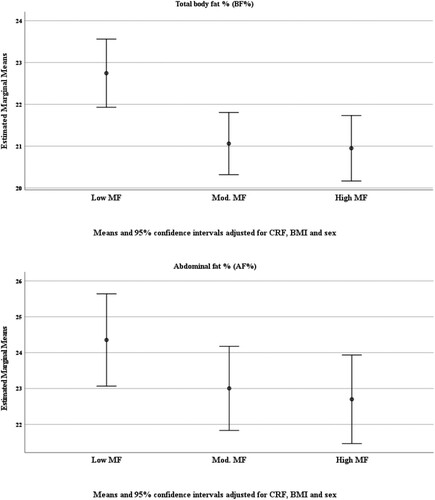
When the associations between MF and BF% and AF% were examined, adjusting for CRF, BMI, and sex, the differences between MF groups were statistically significant for BF% (p = 0.005) but not for AF% (p = 0.192). Specifically, the statistically significant differences in BF% were found between the high and low MF groups (p = 0.011) and between the moderate and low MF groups (p = 0.010). (a and b).
Discussion
The aim of the present study was to examine the associations between MF and accurately assessed body composition in a population-based sample of eight-year-old children. The main finding was that there were strong inverse associations between MF and total body fatness and between MF and abdominal fatness. The children with lower MF had higher total body adiposity and abdominal adiposity compared to the children with higher MF. These associations were observed among both sexes. The present results are consistent with and expand upon previous findings of associations between MF and obesity as a health outcome, for which obesity has mainly been defined based on BMI or abdominal obesity indicated by WC (Ortega et al., Citation2008; Smith et al., Citation2014; Thivel et al., Citation2016). However, making comparisons between the studies of these associations is challenging because there are no standard procedures for the assessment of MF in children. Assessments of MF with lower body weight bearing tests have consistently been shown to be inversely associated with adiposity, which is commonly measured by BMI or WC (Ortega et al., Citation2008; Smith et al., Citation2014; Thivel et al., Citation2016). Contrary to these findings, positive associations have been found between muscle strength and adiposity, when muscle strength has been assessed with the handgrip test (Ortega et al., Citation2008; Smith et al., Citation2014; Thivel et al., Citation2016).
Adiposity and especially increased abdominal adiposity (measured by DXA) have been shown to be independently associated with increased cardiometabolic health risk in obese children and adolescents (Jin et al., Citation2020). Conversely, there is accumulating evidence that health-related fitness, especially CRF, is associated with adiposity and may counteract the negative consequences of obesity in childhood (Ortega et al., Citation2018; Schmidt et al., Citation2016). Less is still known about the effect of MF in children and adolescents (Ortega et al., Citation2018). In longitudinal studies (García-Hermoso, Ramírez-Campillo, & Izquierdo, Citation2019) MF has been found to be inversely associated with adiposity and cardiometabolic risk. However, none of these studies assessed body composition with sophisticated methods. It is not possible to estimate whether MF attenuates the obesity-related future health risks of the children in the present cross-sectional research. However, the overweight and obese children with higher MF had significantly lower total and abdominal adiposity than the children with lower MF at the same BMI category. The similar association was observed among the healthy-weight children. Regardless of BMI category, higher MF was associated with lower total and abdominal adiposity.
The present study examined the associations between MF and DXA -measured adiposity after adjusting for CRF, BMI and sex, it was found that children with higher MF had lower total adiposity compared to children with lower MF, but no statistically significant differences were found in abdominal adiposity between MF groups. Further studies of children, using sophisticated methods of body composition measurement are needed to determine whether higher MF contributes to lower total and abdominal adiposity or whether higher MF counteracts the negative health consequences of obesity.
The main strength of this study was the use of an accurate method (DXA) to assess body composition. Another strength was that all the participating children were born in the same year and recruited from the sample, which was randomly drawn from a population register. The sample of participating children was representative of their age group, considering the distribution of healthy-weight, overweight, and obese children (Vuorela, Citation2011). This study also had limitations. One limitation was that causal inferences could not be made due to the cross-sectional design of the study. In addition, the use of field tests to determine MF may not be ideal. Excessive body fat is an extra load that may adversely affect MF performance, especially when MF performance is measured with weight-bearing tests. However, field tests seem to provide results comparable to laboratory-based data in the assessment of overall MF in children, including those with obesity (Thivel et al., Citation2016). In the present study, MF was assessed with three test items of the FitnessGram, which is a valid and reliable, practical field test battery that has been widely used test to assess health-related fitness in children and youth (Kolimechkov, Citation2017; Plowman, Citation2013). These three test items mainly assess middle and upper body strength and endurance; thus, these items may be more suitable for children with excessive weight compared to test items that measure weight-bearing lower body strength.
The prevention of childhood obesity and the improvement of health-related fitness both have great impacts on public health (Chaput et al., Citation2020). Thus, the results of the present study of significant inverse associations between MF and DXA-measured total and abdominal adiposity in eight-year-old children, are important. Longitudinal studies have shown that childhood obesity often tracks into adulthood, and obesity is often difficult to treat (Di Cesare et al., Citation2019). In addition, studies have shown that youth with low MF are at an increased risk of maintaining low MF level into adulthood (Fraser et al., Citation2017). The persistence of weight status, the known health risks of obesity, and the low efficacy of obesity management, highlight the importance of health-related fitness. In particular, it would be important to inform kindergarten and lower grade school teachers about the importance of MF for health and for regularly include age-appropriate motivational MF enhancing activities.
Conclusion
The results of this population-based cross-sectional study revealed significant inverse associations between MF and DXA-measured total and abdominal adiposity in eight-year-old children. Within the same BMI category, total and abdominal adiposity were lower in children with moderate or high MF than in children with low MF. After adjusting for CRF, children with moderate or high MF had lower total adiposity compared to children with low MF. More studies utilizing accurate measures of body composition are needed to determine whether higher MF could attenuate the negative health consequences of obesity in children.
Acknowledgements
The authors would like to thank all the children and their families who participated. Sincere appreciation is extended to the laboratory personnel of UKK Institute and statistical analyst Jukka-Pekka Kesonen, M.Sc. from University of Jyväskylä, for their contribution to this study. This study was supported by the Ministry of Education and Culture and the Juho Vainio foundation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Sari Slotte
Sari Slotte, M.S.c (Sport and Health Sciences) is PhD student at Faculty of Sport and Health Sciences, University of Jyväskylä and university teacher in didactics of physical education at Faculty of Educational Sciences, University of Helsinki. Her research interests are on childhood obesity, fundamental movement skills and health related fitness.
Katriina Kukkonen-Harjula
Katriina Kukkonen-Harjula, MD, Ph.D., is an associate professor in exercise and sports medicine in Faculty of Medicine and Health Technology in Tampere University, Finland. Her research interests are health-related physical activity, evidence-based clinical guidelines, and rehabilitation of elderly population. She has published over 70 international peer-reviewed publications.
Marjo Rinne
Marjo Rinne is an emerita senior researcher at UKK Institute – Centre for Health Promotion Research. Her research interests have been on promoting health-enhancing physical activities. She has presented in 10 international conferences, published over 20 international peer-reviewed publications, and co-authored four textbooks in the field of physical activity which enhances health and prevents diseases, and Health-Related Fitness Testing.
Juha Valtonen
Juha Valtonen, PhD (education) and MA (physical education) is a senior university lecturer in the didactics of physical education at the University of Helsinki, Finland. His research interests are on teacher development and children's physical activity. He has presented in eight conferences and published 13 peer-reviewed publications. He has worked as a university lecturer in teacher education almost for four decades.
Pauli Rintala
Pauli Rintala is a professor in Adapted Physical Activity at the University of Jyväskylä. His research interests are on individuals with special needs, their motor skills and fitness issues and physical activity. He has presented in more than 50 international conferences, published over 80 international peer-reviewed publications, and co-authored five textbooks in the field of Adapted Physical Activity.
References
- American College of Sports Medicine. (2018). ACSM's guidelines for exercise testing and prescription (10th ed.). Philadelphia, PA: Lippincott Williams &Wilkins.
- Aubert, S., Barnes, J. D, Abdeta, C., Nader, P. A., Adeniyi, A. F., Aguilar-Farias, N, Tenesaca, D. S. A., Bhawra, J., Brazo-Sayavera, J., Cardon, G., Chang, C. K., Delisle Nyström, C., Demetriou, Y., Draper, C. E., Edwards, L., Emeljanovas, A., Gába, A., Galaviz, K.I., González, S.A., … Tremblay, M. S. (2018). Global matrix 3.0 physical activity report card grades for children and youth: Results and analysis from 49 countries. Journal of Physical Activity and Health, 15(Suppl. 2), S251–S273.
- Caspersen, C. J., Powell, K. E., & Christenson, G. M. (1985). Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports, 100(2), 126–131.
- Chaput, J-P., Willumsen, J., Bull, F., Chou, R., Ekelund, U., Firth, J., Jago, R., Ortega, F. B., & Katzmarzyk, P. T. (2020). 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: Summary of the evidence. International Journal of Behavioral Nutrition and Physical Activity, 17(1):141.
- Di Cesare, M., Sorić, M., Bovet, P., Miranda, J. J., Bhutta, Z., Stevens, G. A., Laxmaiah, A., Kengne, A-P., & Bentham, J. (2019). The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Medicine, 17(1), 212.
- Fraser, B. J., Schmidt, M. D., Huynh, Q. L., Dwyer, T., Venn, A. J., & Magnussen, C. G. (2017). Tracking of muscular strength and power from youth to young adulthood: Longitudinal findings from the childhood determinants of adult health study. Journal of Science and Medicine in Sport, 20(10), 927–931.
- Fühner, T., Kliegl, R., Arntz, F., Kriemler, S., & Granacher, U. (2021). An update on secular trends in physical fitness of children and adolescents from 1972 to 2015: A systematic review. Sports Medicine, 51, 303–320.
- García-Hermoso, A., Ramírez-Campillo, R., & Izquierdo, M. (2019). Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and meta-analysis of longitudinal studies. Sports Medicine, 49(7), 1079–1094.
- Jin, B., Lin, H., Yuan, J., Dong, G., Huang, K., Wu, W., Chen, X., Zhang, L., Wang, J., Liang, X., Dai, Y., Xu, X., Zhou, X., Zhu, M., Li, G., Cutfield, W. S., Hofman, P. L., Derraik, J. G. B., & Fu, J. (2020). Abdominal adiposity and total body fat as predictors of cardiometabolic health in children and adolescents with obesity. Frontiers in Endocrinology, 11, 579.
- Kolimechkov, S. (2017). Physical fitness assessment in children and adolescents: A systematic review. European Journal of Physical Education and Sport Science, 3(4), 65–79.
- Leger, L. A., Mercier, D., Gadoury, C., & Lambert, J. (1988). The multistage 20 m shuttle run test for aerobic fitness. Journal of Sports Science, 6(2), 93–101.
- Marra, M., Sammarco, R., & De Lorenzo, A. (2019). Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-ray absorptiometry (DXA): a critical overview. Contrast Media & Molecular Imaging, 3548284, eCollection.
- Meredith, M. D., & Welk, G. J. (2010). Fitnessgram/activitygram test administration manual (4th ed.). Champaign, IL: Human Kinetics.
- Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., Margono, C., Mullany, E. C., Biryukov, S., Abbafati, C., Ferede Abera, S., Abraham, J. P., Abu-Rmeileh, N. M. E., Achoki, T., AlBuhairan, F. S., Alemu, Z. A., Alfonso, R., Ali, M. K., Ali, R., Guzman, N. A., … Gakidou, E. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global burden of disease study 2013. Lancet, 384(9945):766–781.
- NCD Risk Factor Collaboration (NCD-RisC). (2017). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet, 390(10113), 2627–2642.
- Nevill, A. M., Ramsbottom, R., Sandercock, G., Bocachica-González, C. E, Ramírez-Vélez, R., & Tomkinson, G. (2021). Developing a new curvilinear allometric model to improve the fit and validity of the 20-m shuttle run test as a predictor of cardiorespiratory fitness in adults and youth. Sports Medicine, 51(7), 1581–1589.
- Ortega, F. B., Cadenas-Sanchez, C., Lee, D. C., Ruiz, J. R, Blair, S. N., & Sui, X. (2018). Fitness and fatness as health markers through the lifespan: An overview of current knowledge. Progress in Preventive Medicine, 3(2), e0013.
- Ortega, F.B., Ruiz, J.R., Castillo, M.J., & Sjöström, M. (2008). Physical fitness in childhood and adolescence: A powerful marker of health. International Journal of Obesity, 32(1), 1–11.
- Plowman, S. (2013). Muscular strength, endurance, and flexibility assessments [internet]. In S. Plowman & M. D. Meredith (Eds.), Fitnessgram/Activitygram Reference Guide (4th ed.). (pp. 8-1–8-55). Dallas, TX: The Cooper Institute. https://www.cooperinstitute.org/vault/2440/web/files/662.pdf
- Raghuveer, G., Hartz, J., Lubans, D. R., Takken, T., Wiltz, J. L., Mietus-Snyder, M., Perak, A. M., Baker-Smith, C., Pietris, N., Edwards, N. E., & American Heart Association Young Hearts Athero, Hypertension and Obesity in the Young Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young. (2020). Cardiorespiratory fitness in youth: An important marker of health: A scientific statement from the American Heart association. Circulation, 142(7), e101–e118.
- Reilly, J. J., & Kelly, J. (2011). Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. International Journal of Obesity, 35(7), 891–898.
- Rolland-Cachera, M. F. (2011). Childhood obesity: Current definitions and recommendations for their use. International Journal of Pediatric Obesity, 6(5-6), 325–331.
- Schmidt, M. D., Magnussen, C. G., Rees, E., Dwyer, T., & Venn, A. J. (2016). Childhood fitness reduces the long-term cardiometabolic risks associated with childhood obesity. International Journal of Obesity, 40,1134–1140.
- Singh, A. S., Mulder, C., Twisk, J. W., van Mechelen, W., & Chinapaw, M. J. (2008). Tracking of childhood overweight into adulthood: A systematic review of the literature. Obesity Reviews, 9, 474–488.
- Smith, J. J., Eather, N., Morgan, P. J., Plotnikoff, R. C., Faigenbaum, A. D., & Lubans, D. R. (2014). The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sports Medicine, 44(9), 1209–1223.
- Stigman, S., Rintala, P., Kukkonen-Harjula, K., Kujala, U., Rinne, M., & Fogelholm, M. (2009). Eight-year-old children with high cardiorespiratory fitness have lower overall and abdominal fatness. International Journal of Pediatric Obesity, 4(2), 98–105.
- Thivel, D., Ring-Dimitrioum S., Weghuber, D., Frelut, M. L., & O'Malley, G. (2016). Muscle strength and fitness in pediatric obesity: A systematic review from the European Childhood Obesity Group. Obesity Facts, 9(1), 52–63.
- Tomkinson, G. R., & Olds, T. (2007). Secular changes in pediatric aerobic fitness test performance: The global picture. Berlin, Germany: Karger Publishers.
- Tremblay, M.S., Shields, M., Laviolette, M., Craig, C. L., Janssen, I., & Connor Gorber, S. (2010). Fitness of Canadian children and youth: Results from the 2007–2009 Canadian health measures survey. Health Reports, 21(1), 7–20.
- Vuorela, N. (2011). Body mass index, overweight and obesity among children in Finland - A retrospective epidemiological study in Pirkanmaa district spanning over four decades [Doctoral dissertation, Tampere University, Finland]. Tampere University Dissertations Archive. http://urn.fi/urn:isbn:978-951-44-8446-9
- Zeng, Q., Dong, S. Y., Sun, X. N., Xie, J., & Cui, Y. (2012). Percent body fat is a better predictor of cardiovascular risk factors than body mass index. Brazilian Journal of Medical and Biological Research, 45(7), 591–600.