ABSTRACT
The current study aims to clarify the temporal associations between maternal sensitivity and children’s sleep problems across early childhood. This study comprised 942 Dutch mother–child dyads from the Generation R Study, a population-based prospective cohort study. Throughout early childhood, maternal sensitivity was observed in mother–child interactions and coded using Ainsworth’s 9-point rating scales (1.5 years) and the revised Erickson 7-point rating scales (3 and 4 years). Caregivers reported children’s sleep problems on the Sleep Problems Scale of the Child Behaviour Checklist 1½−5 at child ages 1.5, 3, and 6 years. Cross-lagged panel modelling revealed that higher levels of maternal sensitivity (3 years) were associated with fewer sleep problems (6 years); all other temporal associations between maternal sensitivity and children’s sleep problems were nonsignificant. In conclusion, some indication of an association of parenting with children’s sleep across early childhood was found, but there was no evidence for bidirectional associations over time.
Sleep problems commonly occur in paediatric populations, with up to 25% of children experiencing sleep problems (Mindell, Sadeh, Wiegand, How, & Goh, Citation2010; Van Litsenburg, Waumans, Van den Berg, & Gemke, Citation2010). Sleep problems in early childhood are associated with poorer cognitive, emotional, and behavioural functioning (Chaput et al., Citation2017; Reynaud, Vecchierini, Heude, Charles, & Plancoulaine, Citation2018; Sadeh, Citation2007; Sivertsen et al., Citation2015) and child psychopathology (Gregory & Sadeh, Citation2016), such as depression and anxiety (e.g. Jansen et al., Citation2011). Two of the most prevalent reported sleep problems in early childhood are difficulties initiating sleep and nighttime awakenings (Sadeh, Mindell, Luedtke, & Wiegand, Citation2009). Potentially, separation from parents and darkness at bedtime may be distressing for children and could make sleep initiation and sleep maintenance challenging (Dahl & El-Sheikh, Citation2007; Tétreault, Bouvette-Turcot, Bernier, & Bailey, Citation2017). Theoretical frameworks emphasize ongoing dynamic associations between the child and the environment and suggest that children’s sleep may both predict parenting and be predicted by parenting. Therefore, so-called transactional sleep models suggest the possibility of bidirectional associations between parenting and children’s sleep (El-Sheikh & Kelly, Citation2017; Sadeh & Anders, Citation1993; Sadeh, Tikotzky, & Scher, Citation2010; Sameroff & Mackenzie, Citation2003; Tikotzky, Citation2017).
Parental sensitivity is the ability of parents to perceive and interpret children’s cues accurately and to react to them promptly and appropriately. Depending on the setting of the parent–child interaction (e.g. free play, teaching, or caregiving), sensitivity constitutes abilities such as cooperation, non-intrusiveness, supportiveness, respect for autonomy, and structuring (Ainsworth, Blehar, Waters, & Wall, Citation1978). Parental sensitivity is a known predictor of children’s emotional security (Ainsworth et al., Citation1978; De Wolff & Van Ijzendoorn, Citation1997). Experiencing emotional security may enable children to initiate and maintain sleep (Dahl & El-Sheikh, Citation2007; Sadeh et al., Citation2010; Tétreault et al., Citation2017; Tikotzky, Citation2017).
Cross-sectional studies examining maternal sensitivity and children’s sleep have shown mixed findings. In some studies, observed higher maternal sensitivity at bedtime (Teti, Kim, & Countermine, Citation2010) and during daytime (Priddis, Citation2009) were related to fewer infant sleep problems as measured with caregiver-reported children’s sleep diaries (Priddis, Citation2009; Teti et al., Citation2010). However, other studies found no significant association between observed maternal sensitivity and sleep as assessed using mother-reported sleep diaries (Bates, Viken, Alexander, Beyers, & Stockton, Citation2002) and actigraphy (Scher, Citation2001), nor any differences in observed maternal sensitivity between preschoolers with and without sleep problems (Millikovsky-Ayalon, Atzaba-Poria, & Meiri, Citation2015). Longitudinal studies have also shown mixed findings between maternal sensitivity and different sleep constructs. Observed higher maternal sensitivity in infancy was related to a higher percentage of nocturnal sleep as measured with sleep diaries at preschool age (Bordeleau, Bernier, & Carrier, Citation2012; Tétreault et al., Citation2017) and longer sleep duration as measured with actigraphy at child aged 7 years (Cimon-Paquet, Tétreault, & Bernier, Citation2019). However, maternal sensitivity was not related to the longest bout of uninterrupted sleep (Tétreault et al., Citation2017), sleep duration over a 24-hour period (Bordeleau et al., Citation2012) or ratio of sleep duration to time in bed (Cimon-Paquet et al., Citation2019). In contrast, in the longitudinal study of Weinraub and colleagues (Citation2012), higher observed maternal sensitivity was associated with more mother-reported nighttime awakenings throughout early childhood.
Although many studies have conceptualized parental sensitivity as a predictor of children’s sleep, few studies have examined the converse association (El-Sheikh & Kelly, Citation2017). Importantly, associations from children’s sleep to parenting are equally plausible as sensitive parenting may be impaired by children’s sleep problems. Aside from potential genetic effects (Gregory, Rijsdijk, & Eley, Citation2006), mothers of preschoolers with sleep problems indicated in a qualitative study that their child’s sleep problems have a negative impact on their emotional well-being (e.g. frustration) and daytime functioning (e.g. exhaustion), which could potentially undermine sensitive parenting (Smith, Galland, & Lawrence, Citation2019). In line with this, mothers of children with sleep problems (i.e. referred or according to clinical cut-offs) reported poor maternal sleep quality themselves, and higher levels of fatigue, which in turn were related to factors that potentially undermine sensitive parenting, such as greater levels of parenting stress and lower parenting warmth (Giallo, Rose, & Vittorino, Citation2011; Meltzer & Mindell, Citation2007). Furthermore, mothers experiencing more fatigue or insufficient sleep were less likely to use sensitive verbal control techniques in mildly stressful situations (White, Bradley, Neverve, Stirewalt, & Summers, Citation2015).
Altogether, previous studies and theory suggest the possibility of bidirectional effects between maternal sensitivity and sleep problems. However, studies examining bidirectional links between maternal sensitivity and sleep problems are scarce and do not examine these associations across different developmental periods in early childhood. Studies that have examined bidirectionality between maternal sensitivity and children’s sleep problems have found associations of maternal sensitivity affecting children’s sleep problems in early infancy (Bilgin & Wolke, Citation2017; Philbrook & Teti, Citation2016) and bidirectional associations in school-aged children (Bell & Belsky, Citation2008). In early infancy, higher maternal sensitivity was related to fewer regulatory problems, including sleep problems (Bilgin & Wolke, Citation2017), and promoted more infant sleep (Philbrook & Teti, Citation2016). However, in these studies, regulatory problems and infant sleep did not predict maternal sensitivity (Bilgin & Wolke, Citation2017; Philbrook & Teti, Citation2016). In school-aged children (i.e. 8- to 11-year-old children), lower maternal sensitivity and more conflicted mother–child relationships were associated with more sleep problems over time. Children’s sleep problems in turn predicted decreases in maternal sensitivity and less closeness in mother–child relationships (Bell & Belsky, Citation2008).
Aim and hypotheses
Due to the lack of bidirectional studies across different developmental periods in early childhood, there is an incomplete picture of the associations between maternal sensitivity and sleep problems. The aim of the current study is to examine the associations between maternal sensitivity and children’s sleep problems across early childhood by examining these associations repeatedly in children aged between 1.5 and 6 years using data from a large longitudinal birth cohort.
Although studies examining links between maternal sensitivity and sleep problems have revealed inconsistent findings (Bell & Belsky, Citation2008; Bilgin & Wolke, Citation2017; Philbrook & Teti, Citation2016), due to the few bidirectional studies across early childhood and the plausibility of bidirectional associations between maternal sensitivity and sleep according to theoretical frameworks of the transactional sleep model (El-Sheikh & Kelly, Citation2017; Sadeh et al., Citation2010; Sadeh & Anders, Citation1993; Sameroff & Mackenzie, Citation2003; Tikotzky, Citation2017), we hypothesize that bidirectional associations exist between maternal sensitivity and sleep problems across early childhood. More specifically, over time, we expect (H1) higher levels of maternal sensitivity to be associated with fewer sleep problems in children and (H2) fewer sleep problems of children to be associated with higher levels of maternal sensitivity (see ).
Method
Setting and study population
We report how we determined our sample size, all data exclusions, and all measures in the study. This study was embedded in the Generation R Study, a prospective population-based cohort study investigating the growth and development from foetal life onwards in Rotterdam, the Netherlands. All pregnant women with an expected delivery date between April 2002 and January 2006 were invited to participate by their midwife or obstetrician during routine visits. Participating children and their families received questionnaires and were invited to the research centre (see Kooijman et al., Citation2016, for a detailed description of the study). A subsample of 1247 children was recruited for the Generation R Focus cohort, a cohort consisting of children of Dutch origin (i.e. the children, their parents, and their grandparents were all born in the Netherlands) selected for additional in-depth investigation. This subsample consists of a homogenous group of white mother–child dyads. Written informed consent was obtained from all caregivers. The Medical Ethical Committee of the Erasmus Medical Center Rotterdam approved the study (MEC 217.595/2002/202).
In this study, mother–child dyads from the Generation R Focus cohort were included when at least one assessment of children’s sleep problems and at least one assessment of maternal sensitivity were available (n = 942). Within this sample, information on maternal sensitivity was available for 607 mothers (64.4%) of children aged 1.5 years, for 692 mothers (73.5%) of children aged 3 years and for 623 mothers (66.1%) of children aged 4 years. Data on children’s sleep problems were available for 847 children (89.9%) at 1.5 years, 839 children (89.1%) at 3 years, and 853 children (90.6%) at 6 years of age.
Non-response analyses were performed, comparing included mother–child dyads (i.e. at least one assessment of children’s sleep problems and at least one assessment of maternal sensitivity were available) and excluded mother–child dyads. Mothers included in the analyses (n = 942) were older than mothers who were not included (n = 305), t (431.99) = −5.45, p < .001, and had a higher educational level, χ2 (1) = 28.35, p < .001. Moreover, children included in the analyses were more often girls, χ2 (1) = 4.64, p < .05.
Measures
Maternal sensitivity
Maternal sensitivity was observed when mother and child visited the research centre with children aged 1.5 and 3 years, and during a home visit with children aged 4 years. The sensitivity measures at the different time points were all developed from the perspective of the attachment theory (Ainsworth et al., Citation1978; Kok et al., Citation2013). Coders were extensively trained and regularly supervised (Kok et al., Citation2013).
Maternal Sensitivity at 1.5 Years. During a visit at the research centre, maternal sensitivity was observed in a 5-minute free play session and a 5-minute psychophysiological assessment. Recordings were coded using Ainsworth’s 9-point rating scales for Sensitivity and Cooperation (Ainsworth, Bell, & Stayton, Citation1974). An overall maternal sensitivity score was generated by standardizing the scores and creating an average across both subscales and situations, with higher scores indicating more maternal sensitivity. The intercoder reliability (intraclass correlation coefficient [ICC], single measure, absolute agreement) ranged from .65 to .71 (Kok et al., Citation2013).
Maternal Sensitivity at 3 and 4 Years. During the research centre visit at 3 years of age and the home visit at 4 years of age, mothers and children were asked to perform two 3- to 4-minute tasks which challenged the child. At 3 years of age, in the ‘building a tower’ task, mothers and children had to place blocks on a rod in a particular order, so that the blocks fitted together like puzzle pieces. In the ‘Etch-a-Sketch’ task, mothers and children were asked to complete a maze using a drawing toy with two knobs, with the parent controlling one knob and the child controlling the other. At 4 years of age, in the ‘building a tower’ task, parents and children had to build a tower as high as possible. In the ‘Etch-a-Sketch’ task, mothers and children had to draw complicated figures with the parent controlling one knob and the child controlling the other knob of the drawing toy. Recordings of these tasks were coded using the revised Erickson 7-point rating scales for Supportive presence and Intrusiveness to measure maternal sensitivity (Egeland, Erickson, Clemenhagen-Moon, Hiester, & Korfmacher, Citation1990). Maternal supportive presence scores and reversed intrusiveness scores were used as indicators of maternal sensitivity at 3 and 4 years of age, with higher scores indicating more maternal sensitivity. The ICC ranged from .75 to .79 for the 3-year measurement and from .79 to .85 for the 4-year measurement (Kok et al., Citation2013).
Sleep problems
Children’s sleep problems were assessed with the Sleep Problems Scale of the Child Behaviour Checklist 1½−5 (CBCL/1½−5; Achenbach & Rescorla, Citation2000) at child ages 1.5, 3, and 6 years, which were completed by the caregivers (between 84% and 100% were completed by the mother). The Sleep Problems Scale contains seven questions about sleep problems (i.e. ‘doesn’t want to sleep alone’; ‘resists going to bed at night’; ‘has trouble getting to sleep’; ‘sleeps less than most kids during the day and/or night’; ‘wakes up often at night’; ‘nightmares’; ‘talks or cries out in sleep’). Caregivers rated the sleep problems on a 3-point rating scale: 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true). Items were summed to weighted scores according to the manual (Achenbach & Rescorla, Citation2000), with higher scores indicating more sleep problems. The psychometric properties of the CBCL/1½−5 are well established, with adequate test-retest reliability (α = .92 over 8 days) and internal consistency (α = .78; Achenbach & Rescorla, Citation2000). Moreover, the CBCL/1½−5 Sleep Problem Scale has been used as a measure of children’s sleep problems in previous studies (e.g. Gregory & O’Connor, Citation2002; Koopman-Verhoeff et al., Citation2019).
Statistical analyses
Longitudinal measurement invariance was assessed for maternal sensitivity at child aged 3 and 4 years. Maternal sensitivity at 1.5 years was examined with a slightly different coding scheme and could therefore not be included in the assessment of measurement invariance. Measurement invariance for maternal sensitivity for children aged 3 and 4 years was assessed by comparing increasingly stringent models, reflecting (A) configural (i.e. equivalent basic factor structure over time, no cross-time constraints); (B) metric (i.e. equal factor loadings); and (C) scalar invariance (i.e. equal factor loadings and item intercepts) (Van de Schoot, Lugtig, & Hox, Citation2012). If imposing invariance constraints resulted in a significant increase in the Chi-square and, additionally, in ΔCFI (comparative fit index) ≥ −.01, supplemented by ΔRMSEA (root mean square error of approximation) ≥ .015 or ΔSRMR (standardized root mean square residual) ≥ .03 (item loadings) or ΔSRMR ≥ .010 (item intercepts, residual variances), the respective constraint was not tenable (Chen, Citation2007). If measurement invariance could not be established at a certain level, the less stringent model (i.e. configural model for metric non-invariance and metric model for scalar non-invariance) was inspected to determine the items with the strongest non-variance by examining which items’ factor loadings (for metric non-invariance) or intercepts (for scalar non-invariance) were likely to differ the most across time. Thereafter, the fit of the less constrained and more constrained model was compared once again while releasing items with the strongest non-invariance one by one, providing that at least two item loadings and intercepts were constrained across the two measurement occasions. If the more constrained model did not fit worse than the less constrained model, partial invariance was established (Van de Schoot et al., Citation2012). The final latent factor scores for maternal sensitivity at child aged 3 and 4 years, including all tenable constraints, were saved and used as observed variables in the following step of the analyses.
The directionality of associations between maternal sensitivity and children’s sleep problems over time was assessed using cross-lagged panel modelling (CLPM). Analyses were conducted in Mplus (Version 8.4). Stability of maternal sensitivity and children’s sleep problems was taken into account by regressing later scores of each construct on earlier scores. Concurrent associations between maternal sensitivity and children’s sleep problems were taken into account by estimating within-time point correlations. To examine the direction of associations between maternal sensitivity and children’s sleep problems, cross-lagged paths from maternal sensitivity to children’s sleep problems at the subsequent time point were estimated. Conversely, paths from children’s sleep problems to maternal sensitivity were estimated at the subsequent time point. Child age was included as a covariate. Missing data were dealt with using Full Information Maximum Likelihood, which produces unbiased parameter estimates (Muthen & Muthen, Citation1998–2017).
To evaluate the model fit, Chi-square statistics, CFI, Tucker–Lewis index (TLI), SRMR, and RMSEA values were examined. A nonsignificant Chi-square statistic, CFI and TLI values larger than .95, SRMR values smaller than .08 and RMSEA values smaller than .05 were used as an indication for a good fit (Hu & Bentler, Citation1999; Van de Schoot et al., Citation2012).
Results
Descriptive statistics and measurement invariance
Characteristics of the mothers and children are displayed in . Mothers’ age at intake of the Generation R study ranged between 16 and 44 years (M = 31.93 years, SD = 3.81) and most mothers had a high educational level with 74.6% having obtained at least a bachelor’s degree. Approximately half (49.7%) of the children in the sample were girls. Bivariate correlations between maternal sensitivity and children’s sleep problems are displayed in . Tests for measurement invariance indicated that partial metric invariance was obtained. Some adjustments were necessary; in the metric model, the factor loading of one item (i.e. intrusiveness during the building a tower task) had to be freely estimated across time. Because fewer than two item intercepts could be constrained across time (), partial scalar invariance could not be established. Partial metric invariance was obtained, which enables examination of associations between constructs (using CLPM).
Table 1. Child and maternal characteristics of study population (n = 942).
Table 2. Bivariate correlations between maternal sensitivity and children’s sleep problems.
Table 3. Comparing nested models: Testing measurement invariance for maternal sensitivity at child ages 3 and 4 years.
Direction of associations: maternal sensitivity and children’s sleep
Fit estimates indicated a good fit for the CLPM in which associations between maternal sensitivity and children’s sleep problems were modelled, χ2 (30) = 52.12, p = .007; CFI = 0.97; TLI = 0.95; SRMR = .03; RMSEA = .03. Model results are presented in and , and indicate that higher levels of maternal sensitivity at 3 years were associated with fewer children’s sleep problems at 6 years. The association between maternal sensitivity at child aged 1.5 years and children’s sleep problems at child aged 3 years was, however, not significant. Furthermore, no associations of children’s sleep problems with later maternal sensitivity were significant. Moreover, concurrent associations between maternal sensitivity and children’s sleep problems were not significant.
Figure 2. Cross-lagged panel model for maternal sensitivity and children’s sleep problems.
Note: Coefficients presented are standardized coefficient estimates. Significant coefficients are indicated in bold. **p < .01.
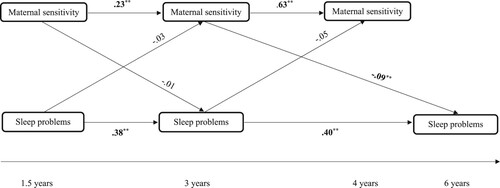
Table 4. Parameter estimates of the cross-lagged panel model for maternal sensitivity and children’s sleep problems.
Discussion
The current study examined the direction of associations between maternal sensitivity and children’s sleep problems across early childhood in a large prospective population-based cohort study with observations of maternal sensitivity. Only maternal sensitivity at child aged 3 years was associated with fewer children’s sleep problems at child aged 6 years. However, maternal sensitivity at child aged 1.5 years was not associated with children’s sleep problems at child aged 3 years, children’s sleep problems were not associated with later maternal sensitivity at any time point, and no concurrent associations between maternal sensitivity and children’s sleep problems were significant. Therefore, findings of the current study do not support our earlier formulated hypotheses, in which we expected bidirectional associations between maternal sensitivity and sleep problems across early childhood.
Associations between maternal sensitivity and child sleep have been reported in previous studies with higher levels of maternal sensitivity diminishing children’s sleep problems in infancy (Bilgin & Wolke, Citation2017; Philbrook & Teti, Citation2016), but findings from cross-sectional and longitudinal studies are unequivocal: some studies report no associations (e.g. Cimon-Paquet et al., Citation2019), and some report more awakenings when mothers are more sensitive to the needs of their infant (Weinraub et al., Citation2012). In the current study, no associations between maternal sensitivity and sleep were found at the age of 1.5 years. The current study did show that higher levels of maternal sensitivity in toddlerhood (3 years) were related to better child sleep at school age (6 years). Maternal sensitivity promotes development of self-regulation in children (Bowlby, Citation1969; Sadeh et al., Citation2010; Tikotzky, Citation2017), which may facilitate sleep initiation and enable children to soothe themselves back to sleep during night wakings (Dahl & El-Sheikh, Citation2007; Tikotzky, Citation2017). Interestingly, the age period around the transition to school is one of the least studied developmental periods in the field of parenting and child sleep. At the same time, it marks a period of rapid development of the child’s self-regulatory abilities, and simultaneous parenting challenges (e.g. boundary setting, sensitive discipline; Kok et al., Citation2022). This underlines the importance for future studies to establish the developmental challenges of parenting and child sleep in pre-school and school-aged children.
In the current study, children’s sleep problems did not predict maternal sensitivity. These findings are not in line with theoretical frameworks of transactional sleep models (Sadeh et al., Citation2010), in which parenting influences child sleep and vice versa. Potentially, the sleep behaviours as measured with the CBCL/1½−5 (e.g. has trouble getting to sleep) are not considered to be problematic by caregivers. Whether mothers perceive sleep behaviours as problematic is dependent on their own sleep-related attitudes and beliefs (Dai & Liu, Citation2021). Children’s sleep behaviours are more likely to be considered problematic when inconsistent with parents’ expectations, and perceived as uncontrollable, troublesome, and stressful. Possibly, mothers did observe the listed child sleep behaviours but did not perceive these sleep behaviours as problematic, resulting in nonsignificant associations. Since assessing the prevalence of sleep behaviours may not provide a complete picture of the bidirectional associations between parenting and children’s sleep, future studies should include assessments of parents’ perceptions and expectations of child sleep.
Since daytime parenting challenges may differ from nighttime parenting challenges (e.g. bedtime routines; Camerota, Propper, & Teti, Citation2019; Mindell & Williamson, Citation2018), maternal sensitivity assessed at daytime may be less strongly associated with children’s sleep than maternal sensitivity assessed at nighttime. To our knowledge, no studies have examined the difference between nighttime maternal sensitivity and daytime maternal sensitivity. However, some studies have reported that higher nighttime maternal sensitivity was associated with fewer children’s sleep problems in infancy (Philbrook & Teti, Citation2016; Teti et al., Citation2010) and sensitive nighttime interactions were related to secure attachment quality (Higley & Dozier, Citation2009). In these studies (Higley & Dozier, Citation2009; Philbrook & Teti, Citation2016; Teti et al., Citation2010), nighttime sensitivity was observed and coded using existing sensitivity concepts (e.g. structuring and non-intrusiveness). Future studies could apply existing sensitivity concepts to parent–child interactions around nap time, bedtime, and night wakings to determine whether parental daytime and nighttime sensitivity differ and how both sets of parenting behaviours are related to children’s sleep problems.
Specific parental behaviours might be required in the context of child sleep. Sensitivity, as assessed in the current study, includes both supportive presence (i.e. positive regard and emotional support) and non-intrusiveness (i.e. respecting the child’s autonomy). Although this assessment is considered the gold standard for observing maternal sensitivity, in the context of child sleep, parents may be focused on disengagement (as opposed to engagement) from the child to prepare the child for sleep and separation from the parent (Teti et al., Citation2010). The used observations of maternal sensitivity mainly encourage parent–child engagement (e.g. mothers are asked to interact with their child). For future studies, assessing maternal sensitivity might include additional measures of sensitive disengagement to assess maternal sensitivity more accurately and appropriately within a sleep context.
The results of the current study may be of particular interest for the treatment of children’s sleep problems. Existing behavioural interventions often involve ignoring the child after bedtime (e.g. cry it out approach; Ball, Douglas, Kulasinghe, Whittingham, & Hill, Citation2018, Citation2020; Mindell, Kuhn, Lewin, Meltzer, & Sadeh, Citation2006), which do not align with the notion of sensitive parenting (Ball et al., Citation2018, Citation2020). The few interventions that promote parental sensitivity around bedtime have been evaluated as promising by parents and practitioners, but empirical evidence remains limited (Ball et al., Citation2018, Citation2020). Future interventions may benefit from including assessments of sleep-related parental perceptions and parental sensitivity.
Limitations and directions for future research
Several limitations warrant caution in the interpretation of our findings. Firstly, measurement invariance for maternal sensitivity could only be assessed for the measures at child ages 3 and 4 years. However, assessments of maternal sensitivity were consistent with Ainsworth’s seminal theory (Ainsworth et al., Citation1978) and the current research is a response to the calls of research to examine measurement invariance as a prerequisite for meaningful comparisons in research (Putnick & Bornstein, Citation2016). Moreover, because the assessments were partially invariant at the metric level, associations between the factors scores could be meaningfully interpreted, allowing for an examination of the direction of associations between maternal sensitivity and children’s sleep problems over time.
Secondly, only maternal parenting was included in the current study. As children’s sleep takes places within a broader system of caregivers, children’s sleep problems can be explored within the family context and other caregivers’ parenting behaviours should be taken into account (Sadeh et al., Citation2010; Tikotzky, Citation2017). Indeed, both higher paternal involvement and sensitivity of both parents have been demonstrated to be related to better children’s sleep in early childhood (Bernier, Tétreault, Bélanger, & Carrier, Citation2017; Bordeleau et al., Citation2012). Moreover, fathers possibly act as a buffer to reduce maternal stress in families of children with sleep disturbances (Millikovsky-Ayalon et al., Citation2015). Future studies should adopt a multi-informant approach to capture children’s sleep within a broader system of caregivers.
Thirdly, in the current study, mother-reported questionnaires were used to assess children’s sleep problems. The CBCL/1½−5 Sleep Problem Scale has been reliably used as a measure of children’s sleep problems (e.g. Gregory & O’Connor, Citation2002; Koopman-Verhoeff et al., Citation2019), mothers give fairly reliable reports of younger children’s sleep (Carskadon, Citation2011) and observations of sensitivity were used, thus eliminating the risk of single rater bias. However, questionnaire data is likely (in part) subjective, and affected by informants’ characteristics (e.g. symptoms of psychopathology; Camerota et al., Citation2019). Future studies should therefore investigate parenting and children’s sleep using a multimethod approach (i.e. objective and subjective measures), to aid the interpretation of future findings and ultimately supporting healthy sleep in families.
Fourthly, the current sample consisted of a homogeneous, population-based group of Dutch mother–child dyads and most mothers had a relatively high educational level. Therefore, it is unknown whether the current findings are generalizable to populations with different ethnic and cultural backgrounds.
Lastly, due to a relatively low level of sleep problems in the current sample, effect sizes in the current study could be restricted. However, although only modest effect sizes were found, these small effects may still have significant implications when used for (preventive) interventions and specific subgroups of children (Kok et al., Citation2013; McCartney & Rosenthal, Citation2000).
Conclusion
The current study examined the directionality of associations between maternal sensitivity and children’s sleep problems across early childhood in a large longitudinal population-based sample with observations of maternal sensitivity. No evidence for bidirectionality between maternal sensitivity and children’s sleep problems was found. Findings from this large nationally representative cohort study indicate that maternal sensitivity at child aged 3 years is associated with fewer children’s sleep problems at child aged 6 years. Future studies could focus on sleep-related parenting behaviours, such as sensitive disengagement around bedtime.
Acknowledgements
The general design of the Generation R Study is made possible by financial support from the Erasmus Medical Center, Rotterdam; the Netherlands Organization for Health Research and Development (ZonMw); the Netherlands Organisation for Scientific Research (NWO); and the Ministry of Health, Welfare and Sport. Rianne Kok is supported by an EUR Fellowship Grant from the Erasmus University Rotterdam. The authors thank all participants and parents, students, practitioners, hospitals, midwives, and pharmacies. The Generation R Study is conducted by the Erasmus Medical Center in close collaboration with the School of Law and Erasmus School of Social and Behavioral Sciences of the Erasmus University Rotterdam, the Municipal Health Service Rotterdam area, the Rotterdam Homecare Foundation, and Stichting Trombosedienst and Artsenlaboratorium Rijnmond (STAR), Rotterdam.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
H. Ying Chuck
H. Ying Chuck is a PhD candidate at the Erasmus Movez Lab at Erasmus University Rotterdam. Her research focuses on how youth can be empowered to perform media literate behaviors online.
M. Elisabeth Koopman-Verhoeff
M. Elisabeth Koopman-Verhoeff is a child psychologist and postdoc at the Institute of Education and Child Studies of Leiden University and the Department of Child and Adolescent Psychiatry/Psychology of the Erasmus University Medical Center–Sophia Children's Hospital. Her research interests are (treatment of) psychopathology and sleep in children and adolescents.
Amaranta D. de Haan
Amaranta D. de Haan is an assistant professor at Erasmus University Rotterdam. Her research focuses on the explanation of parental behaviors and well-being.
Joran Jongerling
Joran Jongerling is an assistant professor at the Department of Methodology & Statistics of the Tilburg School of Social & Behavioral Sciences at Tilburg University. His research focuses on measurement and analysis techniques for intensive longitudinal data.
Annemarie I. Luik
Annemarie I. Luik is an assistant professor at the Department of Epidemiology at the Erasmus MC University Medical Center. Her research focuses on sleep and mental health in population-based samples.
Rianne Kok
Rianne Kok is an associate professor at the Department of Psychology, Education and Child Studies at Erasmus University Rotterdam. She studies how early social relationships and interactions shape self-regulation and moral development in children.
Nicole Lucassen
Nicole Lucassen is an endowed professor at Erasmus University Rotterdam. Her research focuses on effectivity of family support and interventions, specifically within the context of poverty.
Maartje P. C. M. Luijk
Maartje P. C. M. Luijk is a professor at Erasmus University Rotterdam. Her research focuses on parenting and its influence on the development of children.
References
- Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA preschool forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families.
- Ainsworth, M. D. S., Bell, S. M., & Stayton, D. J. (1974). Infant-mother attachment and social development: Socialization as a product of reciprocal responsiveness to signals. In M. P. M. Richards (Ed.), The integration of a child into a social world (pp. 99–135). London: Cambridge University Press.
- Ainsworth, M. D. S., Blehar, M. C., Waters, E., & Wall, S. (1978). Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum.
- Ball, H. L., Douglas, P. S., Kulasinghe, K., Whittingham, K., & Hill, P. (2018). The Possums Infant Sleep Program: Parents’ perspectives on a novel parent-infant sleep intervention in Australia. Sleep Health, 4(6), 519–526. doi:10.1016/j.sleh.2018.08.007
- Ball, H. L., Taylor, C. E., Thomas, V., Douglas, P. S., & The SBY Working Group. (2020). Development and evaluation of ‘Sleep, Baby & You’ – An approach to supporting parental well-being and responsive infant caregiving. PLOS ONE, 15(8), e0237240. doi:10.1371/journal.pone.0237240
- Bates, J. E., Viken, R. J., Alexander, D. B., Beyers, J., & Stockton, L. (2002). Sleep and adjustment in preschool children: Sleep diary reports by mothers relate to behavior reports by teachers. Child Development, 73(1), 62–75. doi:10.1111/1467-8624.00392
- Bell, B. G., & Belsky, J. (2008). Parents, parenting, and children’s sleep problems: Exploring reciprocal effects. British Journal of Developmental Psychology, 26(4), 579–593. doi:10.1348/026151008X285651
- Bernier, A., Tétreault, É, Bélanger, M-È, & Carrier, J. (2017). Paternal involvement and child sleep: A look beyond infancy. International Journal of Behavioral Development, 41(6), 714–722. doi:10.1177/0165025416667851
- Bilgin, A., & Wolke, D. (2017). Development of comorbid crying, sleeping, feeding problems across infancy: Neurodevelopmental vulnerability and parenting. Early Human Development, 109, 37–43. doi:10.1016/j.earlhumdev.2017.04.002
- Bordeleau, S., Bernier, A., & Carrier, J. (2012). Longitudinal associations between the quality of parent−child interactions and children's sleep at preschool age. Journal of Family Psychology, 26(2), 254–262. doi:10.1037/a0027366
- Bowlby, J. (1969). Attachment and loss: Attachment (Vol. 1). New York: Basic Books.
- Camerota, M., Propper, C. B., & Teti, D. M. (2019). Intrinsic and extrinsic factors predicting infant sleep: Moving beyond main effects. Developmental Review, 53, 100871. doi:10.1016/j.dr.2019.100871
- Carskadon, M. A. (2011). Sleep’s effects on cognition and learning in adolescence. In H. P. A. Van Dongen & G. A. Kerkhof (Eds.), Progress in brain research (Vol. 190, pp. 137–143). Elsevier. doi:10.1016/B978-0-444-53817-8.00008-6
- Chaput, J. P., Gray, C. E., Poitras, V. J., Carson, V., Gruber, R., Birken, C. S., … Tremblay, M. S. (2017). Systematic review of the relationships between sleep duration and health indicators in the early years (0-4 years). BMC Public Health, 17, 91–107. https://doi.org/10.1186/s12889-017-4850-2
- Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. doi:10.1080/10705510701301834
- Cimon-Paquet, C., Tétreault, É, & Bernier, A. (2019). Early parent–child relationships and child sleep at school age. Journal of Applied Developmental Psychology, 64, 101057. doi:10.1016/j.appdev.2019.101057
- Dahl, R. E., & El-Sheikh, M. (2007). Considering sleep in a family context: Introduction to the special issue. Journal of Family Psychology, 21(1), 1–3. doi:10.1037/0893-3200.21.1.1
- Dai, Y., & Liu, J. (2021). Parental perceived child sleep problems: A concept analysis. Journal for Specialists in Pediatric Nursing, 26(2), e12327. doi:10.1111/jspn.12327
- De Wolff, M. S., & Van Ijzendoorn, M. H. (1997). Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development, 68(4), 571–591. doi:10.1111/j.1467-8624.1997.tb04218.x
- Egeland, B., Erickson, M. F., Clemenhagen-Moon, J., Hiester, M. K., & Korfmacher, J. (1990). 24 months tools coding manual. Project STEEP-revised 1990 from mother-child project scales. Minneapolis, MN: University of Minnesota.
- El-Sheikh, M., & Kelly, R. J. (2017). Family functioning and children’s sleep. Child Development Perspectives, 11(4), 264–269. doi:10.1111/cdep.12243
- Giallo, R., Rose, N., & Vittorino, R. (2011). Fatigue, wellbeing and parenting in mothers of infants and toddlers with sleep problems. Journal of Reproductive and Infant Psychology, 29(3), 236–249. doi:10.1080/02646838.2011.593030
- Gregory, A. M., & O’Connor, T. G. (2002). Sleep problems in childhood: A longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child & Adolescent Psychiatry, 41(8), 964–971. doi:10.1097/00004583-200208000-00015
- Gregory, A. M., Rijsdijk, F. V., & Eley, T. C. (2006). A twin-study of sleep difficulties in school-aged children. Child Development, 77(6), 1668–1679. doi:10.1111/j.1467-8624.2006.00966.x
- Gregory, A. M., & Sadeh, A. (2016). Annual research review: Sleep problems in childhood psychiatric disorders – a review of the latest science. Journal of Child Psychology and Psychiatry, 57(3), 296–317. doi:10.1111/jcpp.12469
- Higley, E., & Dozier, M. (2009). Nighttime maternal responsiveness and infant attachment at one year. Attachment & Human Development, 11(4), 347–363. doi:10.1080/14616730903016979
- Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi:10.1080/10705519909540118
- Jansen, P. W., Saridjan, N. S., Hofman, A., Jaddoe, V. W. V, Verhulst, F. C., & Tiemeier, H. (2011). Does disturbed sleeping precede symptoms of anxiety or depression in toddlers? The generation R study. Psychosomatic Medicine, 73(3), 242–249. doi:10.1097/PSY.0b013e31820a4abb
- Kok, R., Linting, M., Bakermans-Kranenburg, M. J., van IJzendoorn, M. H., Jaddoe, V. W. V., Hofman, A., … Tiemeier, H. (2013). Maternal sensitivity and internalizing problems: Evidence from two longitudinal studies in early childhood. Child Psychiatry & Human Development, 44, 751–765. doi:10.1007/s10578-013-0369-7
- Kok, R., Luijk, M. P. C. M., Lucassen, N., Prinzie, P., Jongerling, J., Van IJzendoorn, M. H., … Bakermans-Kranenburg, M. J. (2022). The role of supportive parenting and stress reactivity in the development of self-regulation in early childhood. Journal of Child and Family Studies, 31, 2424–2435. doi:10.1007/s10826-022-02360-8
- Kooijman, M. N., Kruithof, C. J., van Duijn, C. M., Duijts, L., Franco, O. H., van IJzendoorn, M. H., de Jongste, J. C., Klaver, C. C. W., van der Lugt, A., Mackenbach, J. P., Moll, H. A., Peeters, R. P., Raat, H., Rings, E. H. H. M., Rivadeneira, F., van der Schroeff, M. P., Steegers, E. A. P., Tiemeier, H., Uitterlinden, A. G., … Jaddoe, V. W. V. (2016). The Generation R Study: Design and cohort update 2017. European Journal of Epidemiology, 31, 1243–1264. doi:10.1007/s10654-016-0224-9
- Koopman-Verhoeff, M. E., Serdarevic, F., Kocevska, D., Bodrij, F. F., Mileva-Seitz, V. R., Reiss, I., … Luijk, M. P. C. M. (2019). Preschool family irregularity and the development of sleep problems in childhood: A longitudinal study. Journal of Child Psychology and Psychiatry, 60(8), 857–865. doi:10.1111/jcpp.13060
- McCartney, K., & Rosenthal, R. (2000). Effect size, practical importance, and social policy for children. Child Development, 71(1), 173–180. doi:10.1111/1467-8624.00131
- Meltzer, L. J., & Mindell, J. A. (2007). Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: A pilot study. Journal of Family Psychology, 21(1), 67–73. doi:10.1037/0893-3200.21.1.67
- Millikovsky-Ayalon, M., Atzaba-Poria, N., & Meiri, G. (2015). The role of the father in child sleep disturbance: Child, parent, and parent–child relationship. Infant Mental Health Journal, 36(1), 114–127. doi:10.1002/imhj.21491
- Mindell, J. A., Kuhn, B., Lewin, D. S., Meltzer, L. J., & Sadeh, A. (2006). Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep, 29, 1263–1276. doi:10.1093/sleep/29.10.1263
- Mindell, J. A., Sadeh, A., Wiegand, B., How, T. H., & Goh, D. Y. T. (2010). Cross-cultural differences in infant and toddler sleep. Sleep Medicine, 11(3), 274–280. doi:10.1016/j.sleep.2009.04.012
- Mindell, J. A., & Williamson, A. A. (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews, 40, 93–108. doi:10.1016/j.smrv.2017.10.007
- Muthén, L. K., & Muthén, B. O. (1998–2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén.
- Philbrook, L. E., & Teti, D. M. (2016). Bidirectional associations between bedtime parenting and infant sleep: Parenting quality, parenting practices, and their interaction. Journal of Family Psychology, 30(4), 431–441. doi:10.1037/fam0000198
- Priddis, L. E. (2009). Tuned in parenting and infant sleep patterns. Early Child Development and Care, 179(3), 259–269. doi:10.1080/03004430600912132
- Putnick, D. L., & Bornstein, M. H. (2016). Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Developmental Review, 41, 71–90. doi:10.1016/j.dr.2016.06.004
- Reynaud, E., Vecchierini, M. F., Heude, B., Charles, M. A., & Plancoulaine, S. (2018). Sleep and its relation to cognition and behaviour in preschool-aged children of the general population: A systematic review. Journal of Sleep Research, 27(3), e12636. doi:10.1111/jsr.12636
- Sadeh, A. (2007). Consequences of sleep loss or sleep disruption in children. Sleep Medicine Clinics, 2(3), 513–520. doi:10.1016/j.jsmc.2007.05.012
- Sadeh, A., & Anders, T. F. (1993). Infant sleep problems: Origins, assessment, interventions. Infant Mental Health Journal, 14(1), 17–34. doi:10.1002/1097-0355(199321)14:1<17::AID-IMHJ2280140103>3.0.CO;2-Q
- Sadeh, A., Mindell, J. A., Luedtke, K., & Wiegand, B. (2009). Sleep and sleep ecology in the first 3 years: A web-based study. Journal of Sleep Research, 18(1), 60–73. doi:10.1111/j.1365-2869.2008.00699.x
- Sadeh, A., Tikotzky, L., & Scher, A. (2010). Parenting and infant sleep. Sleep Medicine Reviews, 14(2), 89–96. doi:10.1016/j.smrv.2009.05.003
- Sameroff, A. J., & Mackenzie, M. J. (2003). Research strategies for capturing transactional models of development: The limits of the possible. Development and Psychopathology, 15(3), 613–640. doi:10.1017/S0954579403000312
- Scher, A. (2001). Mother–child interaction and sleep regulation in one-year-olds. Infant Mental Health Journal, 22(5), 515–528. doi:10.1002/imhj.1015
- Sivertsen, B., Harvey, A. G., Reichborn-Kjennerud, T., Torgersen, L., Ystrom, E., & Hysing, M. (2015). Later emotional and behavioral problems associated with sleep problems in toddlers: A longitudinal study. JAMA Pediatrics, 169(6), 575–582. doi:10.1001/jamapediatrics.2015.0187
- Smith, L., Galland, B., & Lawrence, J. (2019). A qualitative study of how preschoolers’ problematic sleep impacts mothers. Behavioral Sleep Medicine, 17(3), 314–326. doi:10.1080/15402002.2017.1357118
- Teti, D. M., Kim, B. R., & Countermine, M. (2010). Maternal emotional availability at bedtime predicts infant sleep quality. Journal of Family Psychology, 24(3), 307–315. doi:10.1037/a0019306
- Tétreault, É, Bouvette-Turcot, A. A., Bernier, A., & Bailey, H. (2017). Associations between early maternal sensitivity and children’s sleep throughout early childhood. Infant and Child Development, 26(4), e2004. doi:10.1002/icd.2004
- Tikotzky, L. (2017). Parenting and sleep in early childhood. Current Opinion in Psychology, 15, 118–124. doi:10.1016/j.copsyc.2017.02.016
- Van de Schoot, R., Lugtig, P., & Hox, J. (2012). A checklist for testing measurement invariance. European Journal of Developmental Psychology, 9(4), 486–492. doi:10.1080/17405629.2012.686740
- Van Litsenburg, R. R. L., Waumans, R. C., Van den Berg, G., & Gemke, R. J. B. J. (2010). Sleep habits and sleep disturbances in Dutch children: A population-based study. European Journal of Pediatrics, 169, 1009–1015. doi:10.1007/s00431-010-1169-8
- Weinraub, M., Bender, R. H., Friedman, S. L., Susman, E. J., Knoke, B., Bradley, R., … Williams, J. (2012). Patterns of developmental change in infants’ nighttime sleep awakenings from 6 through 36 months of age. Developmental Psychology, 48(6), 1511–1528. doi:10.1037/a0027680
- White, C. P., Bradley, S. L., Neverve, L., Stirewalt, L., & Summers, X. (2015). Does maternal fatigue influence maternal verbal control in a stressful parenting task with toddlers? Journal of Child and Family Studies, 24, 351–362. doi:10.1007/s10826-013-9843-x