Abstract
Objective: To estimate the rate of non-treatment among elderly women with osteoporosis (OP) and to examine the association between patient characteristics and receiving treatment.
Research design and methods: This cross-sectional, retrospective, observational study utilized patient information and claims from the Humana database to identify Medicare covered women aged ≥65 years old and continuously enrolled with evidence of either an OP diagnosis or an OP-related fracture during 2007–2011. The main outcome was receipt of pharmacological treatment of OP during 2012 (follow-up). The percentage of non-treatment was calculated and a stepwise selection logistic regression model was employed to estimate the association between baseline demographic and clinical characteristics and receiving treatment.
Results: A total of 109,829 patients were included. Mean age was 75.7 years and 79.4% were identified with OP through OP diagnosis codes and did not have evidence of a prior fracture. Approximately one-third (32%) of patients had used OP medications during the baseline period, and 39% had experienced at least one gastro-intestinal event during baseline. Among all patients, 71.4% did not receive OP therapy during follow-up. The strongest factor associated with receiving treatment was prior use of OP therapy (odds ratio [OR] = 31.3; p < .001). Among the subgroup of patients with baseline fractures, 75.9% did not receive OP therapy during follow-up and the strongest factor associated with receiving treatment remained prior use of OP therapy (OR = 20.4; p < .001). Those with high comorbidity burden were less likely to receive treatment in both the overall cohort and within the subgroup with baseline fractures.
Conclusions: Among Medicare-eligible women aged ≥65 identified with OP between 2007 and 2011, 71.4% did not receive OP treatment during 2012, including 75.9% of the subgroup of patients with a prior fracture. The use of diagnosis and procedures codes to identify patients with osteoporosis is subject to variation in coding.
Introduction
An estimated 15.4%, or 8.2 million, of women aged 50 years or older had osteoporosis (OP) at either the femoral neck or lumbar spine in 2010 in the USCitation1, and roughly one in two Caucasian women aged 50 years or older experience an OP-related fracture during their lifetimeCitation2. For women aged 65 years or older, the estimated mortality rate within one year after a hip fracture is 9.4%Citation3. Vertebral fractures, whether clinically apparent or silent, are major predictors of future fracture riskCitation4: there is an up to five-fold increase for subsequent vertebral fracture and two- to three-fold increase for fractures at other sitesCitation5. The cost of OP-related fracture in the US was an estimated $16.9 billion in 2005, and over three quarters of the total costs of incident fractures were among women ($12.8 billion)Citation6.
Multiple medications are currently available for the treatment of OP that can reduce risk of fracture. These include bisphosphonates (BPs): alendronate, risedronate, ibandronate, zoledronic acid, as well as non-BPs: raloxifene, calcitonin, teriparatide, denosumab in the US. All have been shown to be effective in reducing the fracture risk in patients with OPCitation7. Previous studies have demonstrated that non-treatment of osteoporosis is commonCitation8–20, whether assessed after clinical or self-reported OP diagnosisCitation10,Citation20, before OP-related fracturesCitation8,Citation11,Citation16, or after fracturesCitation9,Citation11–19. Common barriers to treatment initiation include: concerns over side effectsCitation21 including gastro-intestinal (GI) eventsCitation22–25, costCitation26, and patient frailtyCitation26.
While some previous studies have attempted to identify characteristics associated with the likelihood of OP treatmentCitation8–10,Citation19, most published studies have focused on treatment among patients newly indicated for treatment and did not include patients with prior use of therapy, even though prior osteoporosis therapy has been shown to be predictive of future treatmentCitation27. Additionally, few studies of OP non-treatment focus on a Medicare population. Therefore, this study sought to estimate the proportion of non-treatment among Medicare-covered individuals diagnosed with OP or having at least one OP-related fracture and to examine patient characteristics associated with receiving treatment. We also assessed outcomes among the subset of patients with a history of OP-related fracture, as previous research has reported substantially different treatment rates between those with and without a previous fractureCitation28.
Methods
Study design and data source
A cross-sectional, retrospective, observational analysis was conducted using an administrative claims dataset spanning 1 January 2007 to 31 December 2013. The data source was the Humana database, which includes over 4 million Medicare members and covers all regions of the US. The database contains patient enrollment information and demographic information, as well as medical claims, lab claims, and pharmacy data. Medical claims contain International Clinical Diagnosis, 9th revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, Current Procedural Terminology (CPT) codes, Healthcare Common Procedure Coding System (HCPCS) codes, site of service codes, provider specialty codes, and health plan and patient costs. Pharmacy claims include National Drug Code (NDC) for dispensed medications, quantity dispensed, drug strength, days supply, and health plan and patient costs. Unique identifiers allow for longitudinal tracking of patients and any changes in medication. All data were accessed using techniques compliant with the Health Insurance Portability and Accountability Act.
Study sample
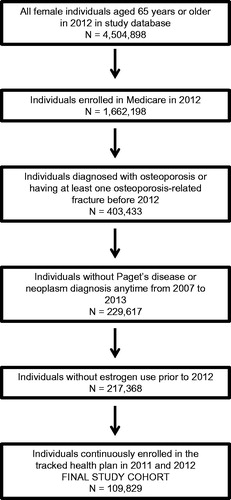
Female patients aged 65 years and older as of 2012 who were identified as enrolled in Medicare were eligible for inclusion. Subjects were required to either have a medical claim with an OP diagnosis (ICD-9-CM 733.0x) or an OP-related fracture as evidenced by both an ICD-9-CM diagnosis code and CPT codeCitation29–31 (see the supplementary Appendix for codes) between 1 January 2007 and 31 December 2011. Additionally, subjects were required to be continuously enrolled in any tracked health plan for all of 2011 and 2012. Those with a medical claim with a diagnosis for Paget’s disease of the bone (ICD-9-CM code 731.0) or malignant neoplasms (ICD-9-CM codes 140–171, 174–208, 230–239) at any point in the study and those with evidence of estrogen use prior to 2012 were excluded, since estrogen is approved for prevention (rather than treatment) of OP5. The subset of patients with a fracture prior to 2012 was also analyzed separately.
Measures
The baseline period used for the identification of comorbidities, baseline fractures, and baseline medication use was 2011, while OP treatment was determined during 2012 (follow-up) and defined as the presence of at least one pharmacy claim for an OP medication or a medical claim with an injectable OP medication in 2012. The percentage of non-treatment was calculated as the number without OP treatment in 2012 divided by the number of patients in the entire sample. Demographic information and baseline clinical characteristics were identified for all patients included in the analysis. Disease burden was established through the Charlson Comorbidity Index (CCI)Citation32, the prevalence of OP-related comorbidities (from ICD-9-CM diagnosis codes: osteopenia; arthritis; musculoskeletal pain; menopause and menopausal symptoms; respiratory disease; hypothyroidism; hyperthyroidism; diabetes; Alzheimer’s disease, dementia, depression, anxiety, sleep disorders; cardiovascular diseases; cerebrovascular diseases; kidney diseases; nutritional disorders; obesity; indication of decreased mobility; hypertension; hyperparathyroidism; vitamin D deficiency; Parkinson’s disease; alcohol disorder; anorexia or bulimia; inflammatory bowel disease; or celiac disease), and evidence of GI events. The use of medications, including OP medications, gastro-protective agents (proton pump inhibitors [PPIs], H2-receptor antagonists, cytoprotectants), non-steroidal anti-inflammatory drugs (NSAIDs), and glucocorticoids was also identified. Baseline fractures were categorized into vertebral, hip, and other fractures. All-cause utilization was assessed through medical claims and separated into inpatient visits, outpatient visits, emergency department (ED) visits, and other visits.
Statistical analysis
Descriptive analyses were performed on all relevant study variables. Counts and proportions were calculated for categorical variables, and means and standard deviations (SDs) were calculated for continuous variables. Univariate comparisons between treated and untreated patients utilized Student’s t-test for continuous measures and chi-square test for categorical variables.
Logistic regression was used to identify factors associated with the likelihood of receiving OP treatment (the independent response variable) among all patients. Initially, all demographic and clinical variables thought to be relevant were included as adjustment variables, including age category (65–74, 75–84, 85+), history of medication use, CCI category (0, 1, 2, 3+), all-cause healthcare utilization, and the occurrence or presence of OP-related comorbidities and events. A stepwise selection procedure was employed to identify the best model, using a p-value cut-off of 0.05 for both the removal and addition of covariates. In addition, the same logistic regression analysis was applied to the subset of patients with a baseline fracture.
Results
Patient identification
There were 4,504,898 women 65 years or older in the database and 1,662,198 were continuously enrolled in Medicare during 2012 (). Of these, 403,433 had a diagnosis of OP or had evidence of at least one OP-related fracture. After the inclusion and exclusion criteria were applied, a total of 109,829 patients were identified for analysis. In the overall cohort, the mean (SD) age was 75.7 (6.0) (). Most patients identified with OP for this study were identified through the use of OP diagnosis codes (79.4%) and did not have evidence of a prior fracture. However, 9.1% of the study cohort was identified through evidence of an OP-related fracture, and the remaining 11.5% had evidence of both (data not shown).
Table 1. Baseline characteristics by treatment status.
Baseline characteristics
Thirty-two percent of patients had used OP medications during the baseline period, and 39% had experienced at least one GI event during baseline (). The most common comorbidities used in calculating the CCI included diabetes without complications (11.2%), chronic pulmonary disease (4.2%), and CHF (4.0%), while the most common OP-related comorbidities included hypertension (75.5%), arthritis (52.1%), musculoskeletal pain (34.3%), respiratory diseases (33.6%). A total of 9141 (8.3%) of patients had evidence of a baseline fracture.
OP treatment
Among all patients included in the sample, 31,366 (28.6%) received OP treatment in 2012; in the subset of patients with a baseline fracture, 2203 (24.1%) received OP treatment in 2012 (). Among all treated patients, the prescribed therapy was more often BP (86.4%) than non-BP (13.6%); the most commonly prescribed BP was alendronate (71.5% of treated patients), with ibandronate, risedronate, and zoledronic acid each accounting for fewer than 6% of treated patients. Similar results were observed within the subset of patients with baseline fractures: 81.5% received BPs, including 64.5% treated with alendronate, and 18.5% treated with non-BPs (). Within the entire cohort, treated and non-treated patients were observed to have similar age (mean [SD] age = 75.7 [6.0] for treated patients and 75.7 [6.1] for untreated patients). Treated patients were observed to be more likely to have received OP-related medications (81.5% vs. 12.1%, p < .001) and to have a lower disease burden in general, as demonstrated by a lower mean CCI (0.40 vs. 0.53, p < .001) (). There were several other relatively modest differences between treated and untreated patients that were significantly different but the magnitude of the difference may not be clinically meaningful. For example, NSAID (27.0% vs. 22.8%, p < .001), and glucocorticoid (23.0% vs. 21.1%, p < .001) use was observed to be higher among treated patients (). Treated patients were also observed to be slightly less likely to have baseline GI events (37.4% vs. 39.1%, p < .001), diabetes (8.8% vs. 12.2%, p < .001), chronic pulmonary disease (3.4% vs. 4.6%, p < .001), congestive heart failure (3.0% vs. 4.4%, p < .001), and hypertension (74.7% vs. 75.9%, p < .001). Further, treated patients were observed to have fewer OP-related fractures of any type (7.0% vs. 8.8% p < .001), including fewer hip and other fractures, but had more vertebral fractures (3.3% vs. 2.7%, p < .001). When compared with untreated patients, patients with OP treatment in 2012 were observed to be less likely to have baseline inpatient and ED visits, but more likely to have outpatient and other visits (). Finally, treated patients were observed to be more likely to have their OP identified from OP diagnosis codes than untreated patients. Similar results were seen when comparing treated and untreated patients within the subset of patients with baseline fractures ().
Table 2. Type of osteoporosis treatment in 2012.
Factors associated with OP treatment
Results of the stepwise logistic regression for the likelihood of receiving OP treatment for the entire cohort are presented in . The strongest factor associated with receiving OP treatment in 2012 was baseline OP medication use (odds ratio [OR] = 31.27; 95% confidence interval [CI] = 30.17–32.41). Other factors associated with an increased odds of OP treatment during follow-up included: baseline use of PPIs (OR = 1.12) or NSAIDs (OR = 1.08), the occurrence of baseline GI events (OR = 1.05), the presence of respiratory diseases (OR = 1.07) and hyperparathyroidism (OR = 1.25), a baseline vertebral fracture (OR = 1.27), and having at least one outpatient (OR = 1.75) or other (OR = 1.08) visit. Characteristics associated with a lower odds of receiving treatment included older age (OR age 85+ vs. age 65–74 = 0.94), higher comorbid condition burden (OR for CCI score of 3+ vs. 0 = 0.83) and the presence of diabetes (OR = 0.90), cardiovascular (OR = 0.94) and cerebrovascular diseases (OR = 0.91), obesity (OR = 0.90), and hypertension (OR = 0.95). Those with at least one baseline ED visit also had lower odds of receiving treatment (OR = 0.87).
Table 3. Results of stepwise logistic regression on the likelihood of receiving treatment for osteoporosis, all patients.
Similar to the analysis of the entire cohort, within the subset of patients with baseline fractures, the strongest factor associated with OP treatment in 2012 was prior OP medication use (OR = 20.37; 95% CI = 18.03–23.02) (). Baseline use of PPIs (OR = 1.32) or glucocorticoids (OR = 1.21) were also observed to increase the odds of OP treatment during follow-up, as did vitamin D deficiency (OR = 1.32) and vertebral fractures (OR = 1.33). Obesity (OR = 0.76), evidence of Alzheimer’s disease, dementia, depression, anxiety, or sleep disorders (OR = 0.86), and a CCI score of 3 or more (OR = 0.78) were associated with a lower odds of receiving treatment.
Table 4. Results of stepwise logistic regression on the likelihood of receiving treatment for osteoporosis, patients with a history of fracture.
Discussion
In this study, we observed that 71.4% of patients identified with OP between 2007 and 2011 did not receive OP treatment in 2012. Patients who did receive treatment had more baseline medication use, including OP medication, greater incidence of baseline vertebral fractures, and were less likely to have several comorbid conditions, including diabetes and cardiopulmonary diseases. Treated patients were more likely to have OP identified from an OP diagnosis code, as opposed to from OP-related fractures. Prior receipt of OP treatment was the strongest predictor of receiving OP treatment during follow-up, conveying 31-fold higher odds of receiving treatment. The next strongest predictor was a baseline outpatient visit, which was associated with 75% higher odds of OP treatment, followed by a baseline vertebral fracture (27% higher odds of receiving treatment). Many of the same associations were also observed within the subset of patients with baseline fractures.
Several previous studies using various methods to ascertain an OP diagnosis have reported under-treatment of OP. A study of Medicare-covered women during 2007–2008 reported OP treatment during the first year after OP diagnosis as 27.9%Citation25, which is very similar to the level reported in the current study of Medicare-covered women (28.6%). A study that identified patients from a commercial managed care population reported a slightly higher rate of treatment (35.7%)Citation20, but the study population was slightly younger (mean age 65.7 years) than that of the current study, and the authors found that older patients were less likely to receive OP treatment. Results from multiple studies suggest that the methods used to identify OP and treatment for OP may influence the level of treatment penetration observed. In a study of self-reported OP patients, 54.9% reported receiving treatmentCitation33, while a study that compared treatment rates by the method of OP identification observed that 9.4% of patients identified through the occurrence of a fracture received treatment within 90 days, while among patients identified via ICD-9-CM diagnosis or the presence of a bone-mineral density test, the percentage treated within 90 days was 41.6%Citation28. In the current study, 24.1% of patients with a baseline fracture received OP treatment during follow-up. This is very similar to the level reported by a study that utilized administrative data, where 24% were observed to have received OP treatment during the 1 year period after an OP-related fracture that occurred during 1994–1996Citation16. Although the study occurred some years prior to the current study (which requires caution in making direct comparisons), the authors also reported a significantly higher rate of treatment among those with vertebral fractures, as was observed in the current study. Another study reported that 27.6% of postmenopausal women who presented to a single facility with a low-trauma fracture in 2006–2007 were receiving OP treatmentCitation17. In the current study, we observed that the percentage of those with a baseline fracture who received OP treatment (24.1%) was lower than that of the entire cohort (28.6%). The finding that those whose OP was identified from diagnosis codes (instead of a fracture) had higher levels of OP treatment parallels results from a previous study that observed that the presence of an OP diagnosis was associated with a greater likelihood of receiving OP pharmacotherapyCitation9.
Logistic regression analysis revealed that, in the overall cohort, prior use of OP medications was the strongest predictor of OP treatment which is consistent with a previous study of Medicare patients that observed that patients with prior OP treatment had over a nine-fold increase in the odds of appropriate OP management (pharmacological treatment or diagnostic testing) following a fracture, versus those without prior OP treatmentCitation27. Use of gastro-protective agents and NSAIDs at baseline were also associated with an increased odds of receiving OP treatment during follow-up; these characteristics have also been noted as factors associated with OP initiation among treatment-naïve womenCitation25,Citation34. In addition, a baseline vertebral fracture was predictive of OP treatment. Vertebral fractures have previously been shown to be associated with higher treatment ratesCitation15,Citation16. Andrade et al.Citation16, in particular, noted that compared with those experiencing a hip or wrist fracture, patients with a vertebral fracture received subsequent OP treatment approximately twice as often. Older patients, and those with diabetes, cardiovascular or cerebrovascular diseases, obesity, hypertension, or a higher CCI score were less likely to be treated.
Many of these findings mirror results of previous research. In some studies, older patients were less likely to receive OP treatmentCitation16,Citation20, although BP treatment appears to be more likely as age increasesCitation20,Citation28. Other factors that have been reported to have a positive association with receiving OP treatment include lower body mass indexCitation28,Citation33 and lower disease burdenCitation33, including lower incidence of chronic inflammatory joint disease, hypertension, and diabetesCitation20. These studies parallel our results which suggest that patients with higher disease burden, comorbid hypertension and diabetes, and patients who were obese were less likely to receive OP treatment. In the subset of patients with a baseline fracture within the current study, many of the same factors were identified as significant predictors of receiving treatment. Prior OP medication use remained the strongest predictor; gastro-protective agent use and vertebral fractures had similar, higher odds of receiving treatment. However, fewer comorbid conditions were found to be predictive: only the presence of vitamin D deficiency was associated with receiving treatment, while mental or cognitive disorders in the form of Alzheimer’s disease, dementia, depression, anxiety, and sleep disorders decreased the odds of receiving treatment. This is not without precedent: a Swedish study using data from 2001–2004 found that those with dementia were less likely to receive OP medications than those without dementia, after adjusting for other factorsCitation35.
The potential for side-effects has been cited as a barrier to OP treatmentCitation26, and the occurrence of GI events, specifically, has been shown to reduce the likelihood of receiving any OP treatmentCitation20,Citation36, as well as the likelihood of being treated with a BP versus a non-BPCitation25. In the current study, baseline GI events were associated with increased odds of OP treatment during follow-up. GI events are common in the elderlyCitation37 and among patients taking OP treatmentCitation38; whether the GI event is a result of prior treatment or a pre-existing GI condition is unknown.
This study adds to the literature that demonstrates that OP treatment levels are suboptimal even though treatment is known to reduce the likelihood of future fractures. Further, we observed that OP treatment rates appear to differ by the method of OP identification: treatment rates were higher among patients with an OP diagnosis code versus only an OP-related fracture, and higher for patients with vertebral fractures versus other fractures. The strongest predictor of receiving OP treatment during follow-up was receipt of OP therapy during baseline. For the Medicare-covered population studied, the factors associated with non-treatment identified in this study represent risk factors for providers to consider in the clinical management of elderly women with OP.
As with all claims-based analyses, this study has certain limitations which should be considered when interpreting the results. First, claims are primarily intended for billing purposes, and the presence of a diagnosis code does not necessarily imply the presence of disease. Pharmacy claims represent prescription fills, and do not guarantee that medication was taken as prescribed or at all. Use of over-the-counter medications or prescription medications provided as samples is not captured in pharmacy claims. Additionally, information on bone mineral density was not available from these data. Given that adherence to and persistence with OP medication is known to be suboptimalCitation31,Citation39–41, it is possible that at least some patients in our study who did not receive treatment in 2012 may have previously received treatment, especially those diagnosed earlier in the study period (i.e. 2008). Additionally, the Food and Drug Administration published a review in June of 2012 that suggested that patients at low risk of fracture should consider discontinuing BP therapy after 3–5 yearsCitation42, which could have influenced patient behavior or provider prescribing patterns during our follow-up period of 2012. However, the overall treatment penetration we observed is similar to levels reported by other studies, and many of the factors found to be associated with receiving treatment agree with previous research. We applied exclusion criteria to avoid confounding by indications for BP use other than osteoporosis and also required a minimum of 2 years of continuous enrollment; as a result our analytic sample represented 27% of patients identified with OP or an OP-related fracture prior to 2012 which may limit generalizability of our findings. Our results are also based on a sample of Medicare patients with managed care and may not be generalizable to patients with Medicare fee-for-service or other form of insurance.
Conclusions
This study examined OP treatment rates among women with Medicare coverage. Only 28.6% of patients identified with OP between 2007 and 2011 received treatment for OP in 2012, including 24.1% of those with a baseline fracture. The high rate of non-treatment among this elderly, Medicare-covered cohort implies that a large proportion of women with OP in this population may be at a higher risk for fracture than would be if they were receiving appropriate therapy. Additional research is warranted to further explore the reasons for non-treatment of OP within this population.
Transparency
Declaration of funding
This study was supported by Merck & Co. Inc.
Declaration of financial/other relationships
X.Y. and A.M. have disclosed that they are employees of Merck & Co. Inc. S.S. has disclosed that he was an employee of Merck & Co. Inc. at the time this study was conducted.
CMRO peer reviewer 1 has disclosed that she has received grants from Amgen; peer reviewer 2 has no relevant financial or other relationships to disclose.
Supplemental_Table.docx
Download MS Word (32.6 KB)Acknowledgments
Craig Solid PhD (Solid Research Group LLC, St Paul, MN, USA) and Sarah Peirce-Sandner MS (Optum, Eden Prairie, MN, USA) provided medical writing support with funding by Merck & Co. Inc.
Previous presentation: Portions of these results were presented at the 2015 Interdisciplinary Symposium on Osteoporosis in Washington, DC, USA, 21 May 2015.
References
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 2014;29:2520-6
- U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004
- Endo Y, Aharonoff GB, Zuckerman JD, et al. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma 2005;19:29-35
- Schousboe JT. Epidemiology of vertebral fractures. J Clin Densitom 2016;19:8-22
- Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 2014;25:2359-81
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 2007;22:465-75
- Watts NB, Bilezikian JP, Camacho PM, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract 2010;16(Suppl 3):1-37
- Gleason LJ, Menzies IB, Mendelson DA, et al. Diagnosis and treatment of osteoporosis in high-risk patients prior to hip fracture. Geriatr Orthop Surg Rehabil 2012;3:79-83
- Greenspan SL, Wyman A, Hooven FH, et al. Predictors of treatment with osteoporosis medications after recent fragility fractures in a multinational cohort of postmenopausal women. J Am Geriatr Soc 2012;60:455-61
- Guggina P, Flahive J, Hooven FH, et al. Characteristics associated with anti-osteoporosis medication use: data from the Global Longitudinal Study of Osteoporosis in Women (GLOW) USA cohort. Bone 2012;51:975-80
- Petrella RJ, Jones TJ. Do patients receive recommended treatment of osteoporosis following hip fracture in primary care? BMC Fam Pract 2006;7:31
- Simonelli C, Chen YT, Morancey J, et al. Evaluation and management of osteoporosis following hospitalization for low-impact fracture. J Gen Intern Med 2003;18:17-22
- Singh S, Foster R, Khan KM. Accident or osteoporosis?: Survey of community follow-up after low-trauma fracture. Can Fam Physician 2011;57:e128-33
- Teede HJ, Jayasuriya IA, Gilfillan CP. Fracture prevention strategies in patients presenting to Australian hospitals with minimal-trauma fractures: a major treatment gap. Intern Med J 2007;37:674-9
- Kroth PJ, Murray MD, McDonald CJ. Undertreatment of osteoporosis in women, based on detection of vertebral compression fractures on chest radiography. Am J Geriatr Pharmacother 2004;2:112-18
- Andrade SE, Majumdar SR, Chan KA, et al. Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med 2003;163:2052-7
- Premaor MO, Pilbrow L, Tonkin C, et al. Low rates of treatment in postmenopausal women with a history of low trauma fractures: results of audit in a Fracture Liaison Service. QJM 2010;103:33-40
- Luthje P, Nurmi-Luthje I, Kaukonen JP, et al. Undertreatment of osteoporosis following hip fracture in the elderly. Arch Gerontol Geriatr 2009;49:153-7
- Panneman MJ, Lips P, Sen SS, Herings RM. Undertreatment with anti-osteoporotic drugs after hospitalization for fracture. Osteoporos Int 2004;15:120-4
- Siris ES, Modi A, Tang J, et al. Substantial under-treatment among women diagnosed with osteoporosis in a US managed-care population: a retrospective analysis. Curr Med Res Opin 2014;30:123-30
- National Osteoporosis Foundation. Types of osteoporosis medications. Washington, DC, USA: National Osteoporosis Foundation, 2014. Available at: http://nof.org/articles/22 [Last accessed 26 July 2015]
- Hamilton B, McCoy K, Taggart H. Tolerability and compliance with risedronate in clinical practice. Osteoporos Int 2003;14:259-62
- Turbi C, Herrero-Beaumont G, Acebes JC, et al. Compliance and satisfaction with raloxifene versus alendronate for the treatment of postmenopausal osteoporosis in clinical practice: an open-label, prospective, nonrandomized, observational study. Clin Ther 2004;26:245-56
- Ettinger B, Pressman A, Schein J. Clinic visits and hospital admissions for care of acid-related upper gastrointestinal disorders in women using alendronate for osteoporosis. Am J Manag Care 1998;4:1377-82
- Siris ES, Yu J, Bognar K, et al. Undertreatment of osteoporosis and the role of gastrointestinal events among elderly osteoporotic women with Medicare Part D drug coverage. Clin Interv Aging 2015;10:1813-24
- Simonelli C, Killeen K, Mehle S, Swanson L. Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clin Proc 2002;77:334-8
- Block AE, Solomon DH, Cadarette SM, et al. Patient and physician predictors of post-fracture osteoporosis management. J Gen Intern Med 2008;23:1447-51
- Asche C, Nelson R, McAdam-Marx C, et al. Predictors of oral bisphosphonate prescriptions in post-menopausal women with osteoporosis in a real-world setting in the USA. Osteoporos Int 2010;21:1427-36
- Martin KE, Yu J, Campbell HE, et al. Analysis of the comparative effectiveness of 3 oral bisphosphonates in a large managed care organization: adherence, fracture rates, and all-cause cost. J Manag Care Pharm 2011;17:596-609
- Viswanathan HN, Curtis JR, Yu J, et al. Direct healthcare costs of osteoporosis-related fractures in managed care patients receiving pharmacological osteoporosis therapy. Appl Health Econ Health Policy 2012;10:163-73
- Wade SW, Curtis JR, Yu J, et al. Medication adherence and fracture risk among patients on bisphosphonate therapy in a large United States health plan. Bone 2012;50:870-5
- Quan H, Li B, Couris CM, et al. Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676-82
- Meadows ES, Mitchell BD, Bolge SC, et al. Factors associated with treatment of women with osteoporosis or osteopenia from a national survey. BMC Womens Health 2012;12:1
- Modi A, Siris ES, Tang J, et al. Gastrointestinal events and association with initiation of treatment for osteoporosis. ClinicoEconomics Outcomes Res 2015;7:603-13
- Haasum Y, Fastbom J, Fratiglioni L, Johnell K. Undertreatment of osteoporosis in persons with dementia? A population-based study. Osteoporos Int 2012;23:1061-8
- Yu J, Goldshtein I, Shalev V, et al. Association of gastrointestinal events and osteoporosis treatment initiation in newly diagnosed osteoporotic Israeli women. Int J Clin Pract 2015;69:1007-14
- Hall KE, Proctor DD, Fisher L, Rose S. American gastroenterological association future trends committee report: effects of aging of the population on gastroenterology practice, education, and research. Gastroenterology 2005;129:1305-38
- Modi A, Siris S, Yang X, et al. Association between gastrointestinal events and persistence with osteoporosis therapy: analysis of administrative claims of a U.S. managed care population. J Manag Care Specialty Pharm 2015;21:499-506
- Cramer JA, Amonkar MM, Hebborn A, Altman R. Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Curr Med Res Opin 2005;21:1453-60
- Huybrechts KF, Ishak KJ, Caro JJ. Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 2006;38:922-8
- Reynolds K, Muntner P, Cheetham TC, et al. Primary non-adherence to bisphosphonates in an integrated healthcare setting. Osteoporos Int 2013;24:2509-17
- Whitaker M, Guo J, Kehoe T, Benson G. Bisphosphonates for osteoporosis – where do we go from here? N Engl J Med 2012;366:2048-51