Abstract
Objective: Acute graft-versus-host disease (aGVHD) is a common and life-threatening complication of allogeneic hematopoietic stem cell transplantation (allo-HSCT). The extent to which aGVHD increases inpatient costs associated with allo-HSCT has not been thoroughly evaluated. In this analysis, mortality, hospital length of stay (LOS) and costs associated with aGVHD during allo-HSCT admissions are evaluated.
Methods: This is a retrospective analysis of discharge records from the National Inpatient Sample database for patients receiving allo-HSCT between 1 January 2009 and 31 December 2013. Allo-HSCT discharges with an aGVHD diagnosis were included in the aGVHD group and those without any graft-versus-host disease (GVHD) diagnosis comprised the non-GVHD group. Mortality, LOS and costs were compared between the two groups, as well as within subgroups, including age (<18 vs. ≥18 years) and survival status (alive vs. deceased) at discharge.
Results: Overall, mortality (16.2% vs. 5.3%; p < .01), median hospital LOS (42.0 vs. 26.0 days; p < .01) and median total costs ($173,144 vs. $98,982; p < .01) were significantly increased in patients with aGVHD versus those without GVHD during hospitalizations for allo-HSCT, irrespective of age group. Patients with aGVHD who were <18 years of age had a lower mortality rate but greater hospital LOS and total costs versus patients aged ≥18 years. Patients who died during allo-HSCT hospitalization had longer LOS and incurred greater costs than those who survived in both the aGVHD and non-GVHD groups.
Conclusion: Occurrence of aGVHD during allo-HSCT admissions resulted in a tripling of the mortality rate and a near doubling of hospital LOS and total costs. In addition, death during allo-HSCT hospitalizations was associated with greater healthcare utilization and costs. Effectively mitigating aGVHD may improve survival and substantially reduce hospital LOS and costs for allo-HSCT.
Introduction
Hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment option for many patients with high-risk or relapsed hematologic malignanciesCitation1. The number of allogeneic HSCT (allo-HSCT) procedures performed has increased steadily since the 1980s, with more than 8000 allo-HSCT procedures performed annually in the United States since 2013Citation1. The success of allo-HSCTs during this time has also increased due to advances in conditioning regimens, immunosuppressive therapy and supportive care, along with human leukocyte antigen (HLA) typing and improved donor selectionCitation2. However, the outcomes of allo-HSCT still need improvement, with an estimated 1-year survival rate of approximately 60%Citation1,Citation3. The major barriers to successful outcomes following allo-HSCT include primary disease relapse and complications from transplant procedures (e.g. acute or chronic graft-versus-host disease [GVHD], infection, or other peri-HSCT toxicities). Risk of GVHD remains a major early and late non-relapse complication of allo-HSCT.
As a consequence of the complexity of the procedure and associated risks, allo-HSCTs involve a variety of costly interventions. In the United States, the aggregate cost from bone marrow transplant procedures was an estimated $1.3 billion in 2007Citation4, an 85% increase from the aggregate cost in 2004. During this time, the total number of allo-HSCT-related hospital stays increased by 51%. A claims database analysis of HSCT procedures conducted from 2007 to 2009 reported a median hospital stay of 19 days and median inpatient total costs of $99,899 for patients who underwent autologous HSCTCitation5. In comparison, patients who underwent allo-HSCT had notably longer median hospital stays (31 days) and greater median total costs ($203,026).
Limited data exist regarding the economic impact of specific HSCT complications. Many patients (40%–60%) who undergo allo-HSCT develop acute graft-versus-host disease (aGVHD), a potentially life-threatening complication in which alloreactive donor T cells attack healthy recipient tissuesCitation6–8. aGVHD manifests primarily in the skin, liver and gastrointestinal tractCitation6. Despite improvements in overall survival observed in patients with aGVHD over recent years, the 1-year survival rate for patients who develop grade III/IV aGVHD is only 40%Citation9.
Limited contemporary data have been reported on the healthcare resource utilization and costs directly attributed to aGVHD after allo-HSCT. A better understanding of the economic burdens of aGVHD may help direct needed attention towards reductions in healthcare resource allocation, which still compromises broader availability of allo-HSCT throughout the world. We conducted a contemporary, nationally representative estimate of the mortality rates, hospital length of stay (LOS) and total inpatient costs associated with aGVHD during allo-HSCT admissions in the United States.
Methods
Study design
This was a retrospective analysis of inpatient discharge records between 1 January 2009 and 31 December 2013, from the National Inpatient Sample (NIS) database. The NIS is the largest publicly available, all-payer inpatient healthcare database in the United States and comprises data from >7 million hospital inpatient stays per year. These data are derived from billing submissions from hospitals to statewide data organizations covering >95% of the United States population, thereby approximating a 20% stratified sample of all discharges from US hospitals included in the Healthcare Cost and Utilization Project (HCUP), which is sponsored by the Agency for Healthcare Research and Quality (AHRQ).
Patient record inclusion criteria
Included in the analysis were discharge records indicating allo-HSCT (International Classification of Diseases, Ninth Revision [ICD-9] procedure codes 41.02, 41.03, 41.05, 41.06, 41.08), with no indication of past or concurrent solid organ transplant. Discharges with aGVHD (ICD-9 279.50) as a primary or secondary discharge diagnosis were included in the aGVHD cohort; discharges without a diagnosis code for any type of GVHD were included in the non-GVHD comparison cohort. Discharges with chronic GVHD, overlap syndrome or unspecified GVHD were excluded from the analysis. Readmissions only for allo-HSCT complications after HSCT admission discharges were excluded because the corresponding allo-HSCT admission records were not available.
In compliance with the Health Insurance Portability and Accountability Act (HIPAA), patient data utilized in this analysis were de-identified. As a retrospective, cohort analysis of data that cannot be subsequently used to identify patients, this study is exempt from institutional review board reviewCitation10.
Assessments
Outcomes evaluated included the proportion of patients who died in the hospital (i.e. inpatient mortality), hospital LOS and total costs of hospital stay. Costs were calculated from hospital charges in the NIS database using a standard HCUP charge-to-cost ratio.
Patient demographic characteristics (age, sex, race), type of payers (Medicare [government-sponsored age and/or disability-based health insurance policy], Medicaid [government-sponsored financial need-based public assistance program for costs associated with medical care], private or other), disease diagnosis (leukemia, non-Hodgkin lymphoma, other), donor and source of stem cells (peripheral blood, cord blood or bone marrow), and US region of transplant hospital (Northeast, Midwest, South and West) are described. Comorbidities were assessed using AHRQ comorbidity software within HCUP, which employs ICD-9 codes and the Diagnosis Related Group in effect on the discharge date to identify coexisting medical conditions not directly related to the principal diagnosis for which allo-HSCT was indicated. Comorbidities may have originated prior to hospitalization for allo-HSCT. The burden of comorbid chronic conditions was described using the Chronic Condition Indicator (CCI) tool within HCUP, which categorizes ICD-9 Clinical Modification codes into chronic and non-chronic categoriesCitation11.
Statistical analyses
Univariate analysis of frequencies and percentages were conducted for categorical variables; mean, standard error and median values were calculated for continuous variables. Discharges for allo-HSCT admissions with aGVHD were compared with discharges among patients without GVHD. Subgroup comparisons between discharges with aGVHD versus without GVHD were evaluated among patients <18 years of age versus those ≥18 years of age, as well as among patients who were alive versus deceased at the time of discharge.
The Wilcoxon rank sum test or t test was used to compare continuous variables, and the chi-square test for categorical variables. The mortality rate at discharge was compared using the chi-square test. Hospital LOS and costs were compared using the Wilcoxon rank sum test. The correlation between hospital LOS and costs was calculated using the Pearson coefficient. The a priori level of significance for all analyses was .05. All statistical analyses were performed using SAS statistical software (SAS Institute Inc., Cary, NC, USA).
Results
Sample size, patient demographics and clinical characteristics
Overall, 7478 discharges for allo-HSCT were identified, including 729 discharges with aGVHD and 5949 discharges without any GVHD. Discharges with unspecified GVHD (759), chronic GVHD (22) and overlap syndrome (19) were excluded. There were also 8189 readmissions for allo-HSCT complications after HSCT admission discharges (7038 with GVHD and 1151 without GVHD) that were excluded from analysis.
Patient demographics and clinical characteristics are presented in . The median ages were 40 and 50 years for patients with aGVHD and without GVHD, respectively. Most patients were ≥18 years of age. In both groups, most patients were male, white and had private insurance. Patients were generally well distributed across the 5 years of study and across the regions of the United States. The stem cell source for most patients was peripheral blood (aGVHD, 68.7%; without GVHD, 76.6%); other sources included bone marrow (aGVHD, 16.3%; without GVHD, 16.4%) and cord blood (aGVHD, 14.4%; without GVHD, 6.1%). Common comorbidities during hospitalization for allo-HSCT (affecting ≥5% of the aGVHD and non-GVHD cohorts, respectively) were hypertension (36.8% and 36.7%), diabetes without chronic complications (14.0% and 10.1%), depression (8.9% and 11.0%) and anemias (8.2% and 11.6%).
Table 1. Demographics and clinical characteristics of allo-HSCT admissions in patients with and without aGVHD.
Mortality, hospital length of stay and costs during allogeneic hematopoietic stem cell transplantation hospitalizations
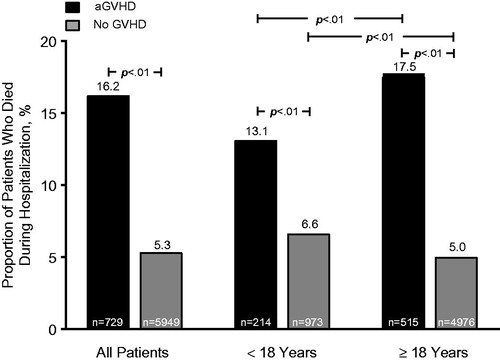
The in-hospital mortality rate was 16.2% for patients with aGVHD versus 5.3% for patients without GVHD (p < .01; ). Mortality rates were lower for patients with aGVHD who were <18 years of age compared with adults; however, aGVHD was associated with higher inpatient mortality rates in both age subgroups.
Figure 1. Death during hospitalization for allo-HSCT. Abbreviations. aGVHD, Acute graft-versus-host disease; allo-HSCT, Allogeneic hematopoietic stem cell transplantation; GVHD, Graft-versus-host disease.
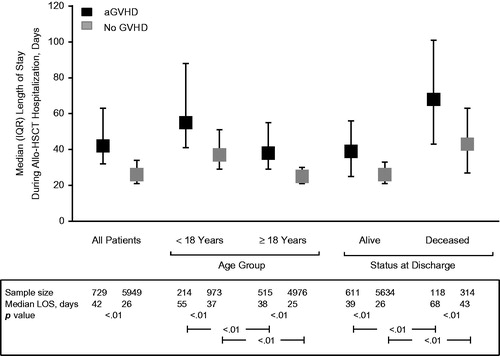
The median hospital LOS was significantly longer for patients with aGVHD compared with patients without GVHD (42.0 vs. 26.0 days, respectively; p < .01; ). Similar trends were observed among patients stratified by age group (<18 and ≥18 years of age) and survival status at discharge (alive and deceased). Patients who were <18 years of age had longer hospital stays than older patients, and patients who died in the hospital had longer stays than patients who survived the hospitalization.
Figure 2. Median LOS during hospitalization for allo-HSCT. Error bars represent the IQR. Data missing for 1 patient in the non-GVHD group. Abbreviations. aGVHD, Acute graft-versus-host disease; allo-HSCT, Allogeneic hematopoietic stem cell transplantation; GVHD, Graft-versus-host disease; IQR, Interquartile range; LOS, Length of stay.
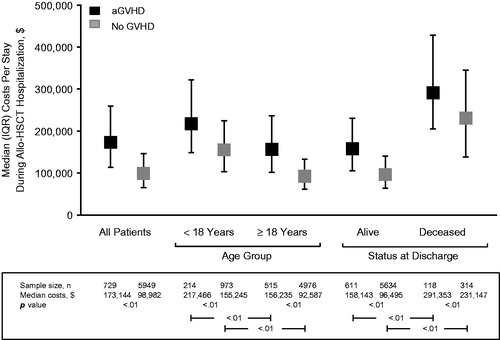
The median costs per stay were significantly greater for patients with aGVHD compared with those without GVHD ($173,144 vs. $98,982, respectively; p < .01; ). The higher costs among patients with aGVHD were observed among patients stratified by age group (<18 and ≥18 years of age; p < .01 for aGVHD vs. no GVHD for both) and also by survival status at discharge (alive and deceased; p < .01 for aGVHD vs. no GVHD for both). Within groups of patients with or without aGVHD, those <18 years of age had higher costs than those ≥18 years of age, and those who had died in the hospital had higher costs than those who survived the hospitalization. A correlation analysis indicated that total allo-HSCT hospitalization costs were directly proportional to hospital LOS (r = 0.711; p < .01).
Figure 3. Median costs per stay during hospitalization for allo-HSCT. Error bars represent the IQR. Data missing for 1 patient in the non-GVHD group. Abbreviations. aGVHD, Acute graft-versus-host disease; allo-HSCT, Allogeneic hematopoietic stem cell transplantation; GVHD, Graft-versus-host disease; IQR, Interquartile range.
Discussion
This retrospective analysis of a large, nationally representative population demonstrated that patients who developed aGVHD during hospitalization for allo-HSCT had an inpatient mortality rate approximately three times higher and hospital LOS and total costs approximately two times higher than those who did not develop GVHD. Hospital LOS was directly related to the total costs. Mortality rates were lower, and hospital LOS and total costs were higher for patients with aGVHD who were <18 years of age and for patients who died during the hospitalization. Overall, hospital LOS and total costs were consistently higher for patients who developed aGVHD, regardless of their age or survival status during the allo-HSCT hospitalization.
These findings extend earlier data concerning inpatient mortality, hospital LOS and costs associated with HSCTCitation5,Citation12–15 by evaluating the specific association of aGVHD with these resource use measures in recipients of allo-HSCT. GVHD is an established leading cause of death post-allo-HSCT. A retrospective analysis reported 1-, 2- and 3-year mortality probabilities of 12%, 17% and 20%, respectively, among 875 patients who developed aGVHD grade II or III/IV post-allo-HSCT in 2006–2012Citation9. Similarly, a Center for International Blood and Marrow Transplant Research report showed that GVHD was a contributor in 17% to 20% of deaths post-allo-HSCT among patients who received HLA-matched sibling or unrelated donor transplants in 2012–2013Citation16.
Additionally, a relationship between aGVHD diagnosis, longer hospital LOS and greater costs have been reported. A recent preliminary report of a US claims analysis covering 2009–2013 indicated that any diagnosis of aGVHD during the year following allo-HSCT increased hospital LOS by 17 days and total healthcare costs by >$100,000 compared with patients without aGVHDCitation17. Similar increases in hospital LOS and costs as a result of aGVHD post-allo-HSCT were reported by two older single-center studies in the United States and Sweden, covering 1994–1997 and 1975–2004Citation13,Citation18. In addition to aGVHD, the US study identified infection, veno-occlusive disease and death as key contributing factors to the high costs of allo-HSCTCitation13.
A key finding in the current study was that patients who died during the allo-HSCT hospitalization had significantly longer hospital LOS and higher costs, independent of aGVHD occurrence. In agreement with this finding, the Swedish analysis reported that death within 1 year of allo-HSCT was associated with significantly higher costsCitation18. The increased costs observed in patients who died may have included the use of the intensive care unit and other critical care. Further studies investigating inpatient healthcare resource utilization are needed to determine the direct drivers of these higher costs.
We observed that young patients had longer hospital LOS and higher costs during allo-HSCT hospitalizations compared with adults. Similar findings were reported in a large claims database analysis of the first 100 days after allogeneic transplantation in 2007–2009, in which median hospital LOS for patients aged ≤20 years (42 days) was notably higher than in the three older age groups (28–29 days)Citation5. Median total costs for patients ≤20 years old ($303,709) were also notably higher than the median costs observed across the three older age groups ($155,548–$202,962). Although children generally tolerate high-dose conditioning regimens and immunosuppressive therapy better than adultsCitation19, they often have a longer hospital LOS and accompanying costsCitation5. Very young children must be more stable and independent of nutritional and hydration support prior to discharge and often require longer inpatient observation for potential complications (infection, GVHD) post-allo-HSCT. Alternative and hopefully more effective aGVHD prophylaxis and treatment must be delivered without resulting in longer periods of hospitalization.
Given the limitations of the NIS database, this study was restricted to allo-HSCT hospitalizations with aGVHD or no GVHD, precluding longer-term patient follow-up for hospital readmission and survival. Therefore, these data are limited to evaluations of aGVHD that occurred during allo-HSCT hospitalization and, as such, likely underestimate both the rate of aGVHD and the costs/resource utilization in patients with aGVHD. Furthermore, data regarding aGVHD grade were not available within the database, so the impact of disease severity on costs and hospital LOS could not be assessed. Data on transplant specifics (e.g. donor type, conditioning regimen, GVHD prophylaxis and treatment, supportive measures) and survival beyond the allo-HSCT discharge date were not available in this data set; thus, the impact of GVHD risk factors or specific GVHD manifestations could not be directly assessed in our study, but would be important to consider in further studies.
Conclusions
The cost and mortality data reported in this study underscore the importance of advancing aGVHD prevention and treatment, both to improve patient survival and to reduce the healthcare costs associated with allo-HSCT. Effectively mitigating aGVHD may improve the survival of transplant patients while reducing inpatient resource use and costs.
Transparency
Declaration of funding
This work was funded by Incyte Corporation (Wilmington, DE, USA).
Author contributions: J.Y. was involved in study conceptualization, study design, analysis and interpretation of the results. S.P. was involved in study design, providing analysis direction and interpretation of the results. A.S. and D.W. were involved in study design, data analysis and data interpretation. All authors contributed to the development of the manuscript and approved the final draft.
Declaration of financial/other relationships
J.Y. and S.P. have disclosed that they are employees and stockholders of Incyte Corporation. A.S. has disclosed that at the time of analysis he was an employee of Market Access Solutions, Health Economics and Outcomes Research (Raritan, NJ, USA). D.W. has disclosed that he has received support as a consultant from Kadmon and Enlivex, and research funding from Alexion and Incyte Corporation.
CMRO peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
Writing assistance was provided by Jane Kovalevich, PhD (Complete Healthcare Communications, LLC [North Wales, PA], a CHC Group company), whose work was funded by Incyte Corporation (Wilmington, DE).
Previous presentation: This study was previously presented at the 2017 meeting of the American Society of Health-System Pharmacists Midyear Clinical Meeting.
References
- D’Souza A, Fretham C. Current uses and outcomes of hematopoietic cell transplantation (HCT): CIBMTR summary slides [Internet] 2017. Center for International Blood and Marrow Transplant Research, 2017 [cited 2018 Jul 18]. Available from: http://www.cibmtr.org.
- Singh AK, McGuirk JP. Allogeneic stem cell transplantation: a historical and scientific overview. Cancer Res. 2016;76:6445–6451.
- Holtan SG, DeFor TE, Lazaryan A, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–1338.
- Stranges E, Russo CA, Friedman B. HCUP Statistical Brief #82. Procedures with the most rapidly increasing hospital costs, 2004–2007 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality, 2009 [cited 2017 Oct 12]. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb82.pdf.
- Majhail NS, Mau LW, Denzen EM, Arneson TJ. Costs of autologous and allogeneic hematopoietic cell transplantation in the United States: a study using a large national private claims database. Bone Marrow Transplant. 2013;48:294–300.
- Ferrara JL, Levine JE, Reddy P, Holler E. Graft-versus-host disease. Lancet. 2009;373:1550–1561.
- Gratwohl A, Brand R, Frassoni F, et al. Cause of death after allogeneic haematopoietic stem cell transplantation (HSCT) in early leukaemias: an EBMT analysis of lethal infectious complications and changes over calendar time. Bone Marrow Transplant. 2005;36:757–769.
- Jagasia M, Arora M, Flowers ME, et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood. 2012;119:296–307.
- Khoury HJ, Wang T, Hemmer MT, et al. Improved survival after acute graft-versus-host disease diagnosis in the modern era. Haematologica. 2017;102:958–966.
- United States Department of Health and Human Services. Code of Federal Regulations: Title 45 Part 46- Protection of Human Subjects [Internet]. 2009 [cited 2018 Jun 28]. Available from: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cf r-46/index.html.
- Healthcare Cost and Utilization Project. Chronic condition indicator [Internet]. Rockville, MD: Agency for Healthcare Research and Quality, 2016 [cited 2017 Sep 20]. Available from: www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp.
- Sundaramurthi T, Wehrlen L, Friedman E, et al. Hematopoietic stem cell transplantation recipient and caregiver factors affecting length of stay and readmission. Oncol Nurs Forum. 2017;44:571–579.
- Lee SJ, Klar N, Weeks JC, Antin JH. Predicting costs of stem-cell transplantation. J Clin Oncol. 2000;18:64–71.
- Majhail NS, Mothukuri JM, Brunstein CG, Weisdorf DJ. Costs of hematopoietic cell transplantation: comparison of umbilical cord blood and matched related donor transplantation and the impact of posttransplant complications. Biol Blood Marrow Transplant. 2009;15:564–573.
- Bennett C, Waters T, Stinson T, et al. Valuing clinical strategies early in development: a cost analysis of allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant. 1999;24:555–560.
- Center for International Blood & Marrow Transplant Research (CIBMTR). HCT trends and survival data [Internet]. 2015 [cited 2017 Oct 6]. Available from: https://www.cibmtr.org/referencecenter/slidesreports/summaryslides/Pages/index.aspx.
- Grubb WW, Huse S, Alam N, et al. Economic burden of acute graft-versus-host disease (GvHD) following allogeneic hematopoietic cell transplant (HCT) for hematologic malignancies. Blood. 2016;128:1187.
- Svahn BM, Remberger M, Alvin O, et al. Increased costs after allogeneic haematopoietic SCT are associated with major complications and re-transplantation. Bone Marrow Transplant. 2012;47:706–715.
- Gamper CJ, Takemoto CM, Chen AR, et al. High-dose cyclophosphamide is effective therapy for pediatric severe aplastic anemia. J Pediatr Hematol Oncol. 2016;38:627–635.
