Introduction
Before 1998, in the UK varicose veins were usually treated by open surgery under general anaesthetic. The principles of the open operation were to ligate the incompetent junction or junctions of where superficial veins connected with deep veins of the legs, and then to strip out the distal associated venous truncal vein and remove any surface varices. This process was commonly called “high tie”, “stripping” and “phlebectomies”.
This procedure removed the source of venous reflux from deep to superficial veins and removed the incumbent conduit and associated surface venous dilatations. However, since veins are part of the connective tissue of the body, they tend to grow back after damage, a process the venous surgeons call “neovascularisation”Citation1,Citation2 but other doctors observe elsewhere in the body and call normal “healing”.
When new veins grow to replace those that have been removed surgically, the new veins are avalvular. Therefore, as soon as they grow back again, they are incompetentCitation1,Citation2.
In March 1999 the first catheter based endovenous thermoablation was performed in the UK as an alternative to open ligation and strippingCitation3. This was a disruptive change, heralding the change from open to endovenous surgery.
The principle of the endovenous approach was to close an incompetent vein with heat, generated from within the lumen by an endovenous catheter. Initially it was thought that closure was obtained by collagen contraction and denaturation combined with endothelial damageCitation4–6, although subsequent research has suggested that it is also the transmural death of the cells in the vein wall that lead to permanent closure of the target vein by fibrosisCitation7,Citation8.
Although the first cases were performed with a high ligation and retrograde passage of the catheter down the vein to replace stripping, almost immediately this was replaced by percutaneous puncture of the truncal vein distally under ultrasound control, with the endovenous catheter being passed proximally. The first devices used radiofrequency electric currents to produce the heatCitation9, and subsequently laserCitation10, steamCitation11 and microwaveCitation12 have all been introduced.
As heat is used to close the vein, tumescent anaesthetic solution must be injected around the vein. After truncal incompetence is ablated, incompetent perforators can be closed using endovenous thermoablation using a technique called TransLuminal Occlusion of Perforators (TRLOP)Citation13 and varicosities can be treated by phlebectomy or foam sclerotherapy.
By 2013, the National Institute for Health and Care Excellence (NICE) produced Clinical Guidelines CG168 which recommended endovenous thermal ablation (or “endothermal ablation” as they called it) as the first line treatment for varicose veinsCitation14.
Over the last 20 years, venous surgeons and companies researching new devices have largely concentrated on non-thermal alternatives to endovenous thermal ablation to remove the requirement for the injection of tumescent anaesthesia. Such techniques include foam sclerotherapyCitation15, mechanochemical ablation (MOCA)Citation16 and cyanoacrylate gluesCitation17. However, probably because these all use the endovenous approach, none have proven to be disruptive to the dominance of endovenous thermoablation.
High Intensity Focused Ultrasound (HIFU)
High Intensity Focused Ultrasound (HIFU) may prove to be the next disruptive technology in the treatment of varicose veins and venous reflux disease. It is totally non-invasive, with ultrasound energy being beamed from a transducer applied to the skin above the vein. Gentle pressure of the device on the skin above the vein closes the vein, removing any blood that might thrombose or remove heat during treatment.
The therapeutic ultrasound is focused on the target vein, using a linear ultrasound array to obtain an image of the target vein in real time. The focused ultrasound generates heat at a precise point deep to the skin, guided by the real time ultrasound image. Each treatment cycle, a volume of tissue about the size of a grain of rice is ablated at about 85–90 °C. Due to the heat, some patients do require small amounts of local anaesthetic to be injected at the point of heating.
So why might HIFU disrupt the current standard treatment of varicose veins by endovenous thermoablation?
HIFU heats the target vein to temperatures proven to cause permanent closure of an incompetent vein by fibrosis. It does not require cannulation of the vein and indeed nothing is inserted into the target vein at all. There is no need for an operating theatre and, as nothing is introduced into the vein itself, this procedure can be performed in a clean clinical room.
The treatment is totally non-invasive, save for those patients who may need small volumes of local anaesthetic to be injected around the target vein. However, even if local anaesthetic is used, the volumes for this are substantially less than the amount of tumescence pumped around truncal veins during catheter based endovenous thermoablation. As the vein is not cannulated, infection and bleeding risk is minimal and so this can be used in patients who are fully anticoagulated.
Of course, as with any new technology, the current device is large, cumbersome, expensive and treatment is slow in long truncal veins. Being so new (the CE mark for the Sonovein, Theraclion, Paris, France was only given in April 2019) we have not yet fully identified which patients and which patterns of disease are optimally treated with HIFU and which are not suitable.
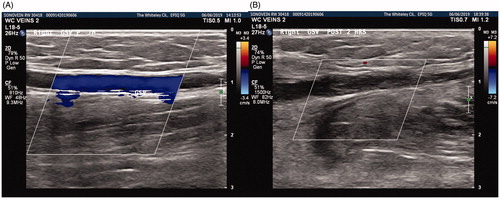
At the time of originally writing this, we had performed 5 cases in May 2019 using the Sonovein machine (). The maximum power used in each pulse varies depending on the depth of the vein. As the HIFU energy is focused, it can be considered as a “cone” of energy emerging from the treatment head and converging on the focal point 24 mm from the rim of the transducer. The energy density passing through the skin must be below that that might cause a skin burn. Hence the deeper the vein, the broader the base of the “cone” of ultrasound, and so the higher the energy available/implementable per pulse.
Figure 1. Sonovein (HIFU) machine being used to treat the right Great Saphenous Vein in a clinic room.

Sonovein automatically detects the depth of the vein from the skin surface, and adjusts the maximum energy that can be delivered, in order to protect the skin. This, combined with a skin cooling delay which is computed within the device, prevents any thermal skin damage. This appears to work as we have seen no skin burns or skin complications in any of these, nor subsequent, treatments.
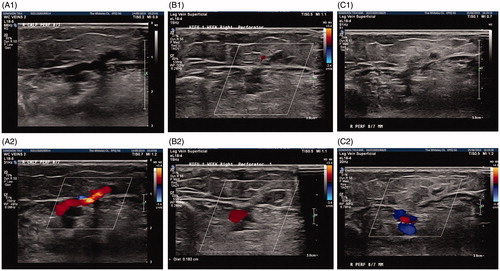
Each pulse of HIFU last for 8 s, and then there is a variable delay to ensure skin temperature is normal before a further pulse (). In the time, the robotic head can be moved in order for the next section of vein to be treated with the next pulse. Currently, this means that the treatment of long truncal veins is time-consuming, although the treatment of incompetent perforator veins, neovascular tissue and saphenous stumps in recurrent varicose veins is very fast. Patients are fully mobile immediately after the procedure and no thromboprophylaxis is needed.
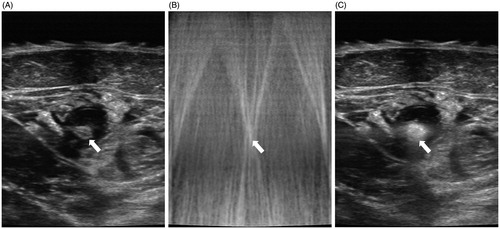
Figure 2. (A) Ultrasound image of Great Saphenous Vein (white arrow) surrounded by a little local anaesthetic. (B) The image during the HIFU pulse with the “white cross” of reflected ultrasound where gas is produced from the blood in the treated vein (white arrow). (C) The immediate post-treatment image of a successfully treated Great Saphenous Vein. Note the gas formation within the vein and vein wall, shown as a white reflection on ultrasound (white arrow).
Even though this is the beginning of the authors learning curve, it is clear to us that the technology works, and the patients found the experience acceptable. As this is an early report of a new technology and is also reporting work performed in our learning curve, we are not formally publishing our full results. These will be submitted for publication soon, when we can compare our learning curve outcomes with subsequent treatments. However, it is already clear that closure rates on duplex ultrasound follow-up appear to be at least as good as endovenous thermal ablation in the same short term ( and ).
Conclusion
As with endovenous thermoablation in 1999, this technology will continue to develop. Both the device and the way it is used will, no doubt, improve rapidly as lessons are learnt with clinical experience. However, as a totally non-invasive treatment option for varicose veins, venous leg ulcers and other manifestations of venous reflux disease, HIFU must be considered as the next potential disruptive technology in this field.
Transparency
Declaration of funding
No funding to disclose.
Declaration of financial/other relationships
No conflicts of interests to disclose. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
MS conceptualized and designed the manuscript, analysed and interpreted the data, and wrote and critically revised the manuscript.
Acknowledgements
None reported.
References
- Munasinghe A, Smith C, Kianifard B, et al. Strip-track revascularization after stripping of the great saphenous vein. Br J Surg. 2007;94(7):840–843.
- Ostler AE, Holdstock JM, Harrison CC, et al. Strip-tract revascularization as a source of recurrent venous reflux following high saphenous tie and stripping: results at 5–8 years after surgery. Phlebology. 2015;30(8):569–572.
- Fraser L. New Varicose Vein Surgery Speeds Recovery [Internet]. The Telegraph. 2000 [cited 2019 May 20]. Available from: https://www.telegraph.co.uk/news/uknews/1374873/New-varicose-vein-surgery-speeds-recovery.html
- Rautio T, Ohinmaa A, Perälä J, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35(5):958–965.
- Min RJ, Khilnani NM. Endovenous laser treatment of saphenous vein reflux. Tech Vasc Interv Radiol. 2003;6(3):125–131.
- Zikorus AW, Mirizzi MS. Evaluation of setpoint temperature and pullback speed on vein adventitial temperature during endovenous radiofrequency energy delivery in an in-vitro model. Vasc Endovascular Surg. 2004;38(2):167–174.
- Whiteley MS. Holdstock. Percutaneous radiofrequency ablations of Varicose Veins (VNUS Closure). In: Greenhalgh RM, editor. Vascular and endovascular challenges. London; BibaPublishing; 2004. p. 361–381.
- Fan CM, Rox-Anderson R. Endovenous laser ablation: mechanism of action. Phlebology. 2008;23(5):206–213.
- Goldman MP. Closure of the greater saphenous vein with endoluminal radiofrequency thermal heating of the vein wall in combination with ambulatory phlebectomy: preliminary 6-month follow-up. Dermatol Surg. 2000;26(5):452–456.
- Navarro L, Min RJ, Boné C. Endovenous laser: a new minimally invasive method of treatment for varicose veins–preliminary observations using an 810 nm diode laser. Dermatol Surg. 2001;27(2):117–122.
- van den Bos RR, Milleret R, Neumann M, et al. Proof-of-principle study of steam ablation as novel thermal therapy for saphenous varicose veins. J Vasc Surg. 2011;53(1):181–186.
- Subwongcharoen S, Praditphol N, Chitwiset S. Endovenous microwave ablation of varicose veins: in vitro, live swine model, and clinical study. Surg Laparosc Endosc Percutan Tech. 2009;19(2):170–174.
- Bacon JL, Dinneen AJ, Marsh P, et al. Five-year results of incompetent perforator vein closure using TRans-Luminal Occlusion of Perforator. Phlebology. 2009;24(2):74–78.
- NICE Clinical Guidelines CG168 [Internet], 2013 [cited 2019 May 20). Available from: https://www.nice.org.uk/guidance/cg168.
- Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg. 2001;27(1):58–60.
- Elias S, Raines JK. Mechanochemical tumescentless endovenous ablation: final results of the initial clinical trial. Phlebology. 2012;27(2):67–72.
- Chan YC, Ting AC, Yiu WK, et al. Cyanoacrylate superglue to treat varicose veins: truly office based and minimally invasive? Eur J Vasc Endovasc Surg. 2013;45(2):176–177.