Abstract
Background
Schizophrenia is a heterogeneous disorder with a burden that can vary greatly depending on the severity and the duration. Previous research has suggested that patients in the earlier stages of schizophrenia (typically first-episode schizophrenia) benefit from effective early treatment, however, a comprehensive review of the burden specifically in this population has not been undertaken. A systematic literature review was therefore conducted to characterize the clinical, economic, and humanistic burden, as reported in naturalistic studies of schizophrenia populations specifically at an early stage of disease in comparison with healthy controls, patients with chronic schizophrenia, and patients with other psychiatric disorders.
Methods and materials
Searches were conducted in MEDLINE, MEDLINE In-Process, Embase, PsycINFO, and EconLit databases for records published between January 2005 and April 2019, and of relevant conference abstracts published between January 2014 and May 2019. Data were extracted from relevant publications and subjected to qualitative evaluation.
Results
Fifty-two publications were identified for inclusion and revealed a considerable burden for early schizophrenia with regards to mortality, psychiatric comorbidities such as substance abuse and depression, poor social functioning, and unemployment. Comparisons with chronic schizophrenia suggested a greater burden with longer disease duration, while comparisons with other psychiatric disorders were inconclusive. This review uncovered various gaps in the available literature, including limited or no data on incarcerations, caregiver burden, and costs associated with early schizophrenia.
Conclusions
Overall, the burden of schizophrenia is apparent even in the early stages of the disease, although further research is required to quantify the burden with chronic schizophrenia and other psychiatric disorders.
Introduction
Schizophrenia is a heterogeneous disease, which varies greatly in its manifestation across patient groups, disease course, and incidence in different parts of the worldCitation1,Citation2. Globally it was estimated that there were approximately 20 million people with schizophrenia in 2017, amounting to around 12,500 years lived with disabilityCitation2. It is a severe psychiatric disorder with patients experiencing disability throughout their illness, manifesting through alteration of thought, hallucinations, and delusions, amongst other negative and cognitive symptomsCitation3. The illness may have consequences on social interaction and functioning which can impact day-to-day activities such as gaining or maintaining employment and relationships with family and friendsCitation4. The economic burden of schizophrenia is large, with a recent study suggesting most of this burden arises from indirect costsCitation5.
Despite advances in the understanding of the disease and the introduction of novel therapies, only a minority of people with schizophrenia fully recoverCitation6. Research has suggested that treating patients during the earlier stages of schizophrenia, typically within the first psychotic episode, increases the chance of recovery, reduces the risk of relapse, and could provide patients with more favorable long-term outcomesCitation7–10. A meta-analysis of 10 randomized controlled trials (RCTs) concluded that early intervention in first-episode psychosis or early schizophrenia spectrum disorders was superior to usual care across all outcomes, including treatment discontinuation, psychiatric hospitalization, school or work involvement, and symptom severityCitation11.
While many sources of burden are known to impact patients with schizophrenia and their carersCitation4, few systematic literature reviews (SLRs) have considered the burden of disease specifically for patients early in the disease. To complement early intervention in schizophrenia, it is important to identify the aspects of disease burden that are particularly problematic for this group and guide management in a way that addresses those unmet needs.
This SLR aimed to characterize the disease burden for patients “early” in the course of schizophrenia and their caregivers, as observed in naturalistic studies, to better understand and highlight their unmet needs. The aspects of burden investigated in this review span clinical burden (including comorbidities and mortality), economic burden (such as hospitalization and unemployment), and humanistic burden (such as social functioning and quality of life [QoL]). The review set out to make comparisons with healthy controls to identify all sources of burden. Additionally, comparisons were made with chronic schizophrenia and other psychiatric disorders to identify areas that may play a greater role for the early schizophrenia population but could be overlooked if considering schizophrenia or early psychiatric disorders as a whole.
Methods
Search strategy and selection of studies
An SLR was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelinesCitation12. Searches were conducted in MEDLINE, MEDLINE In-Process, Embase, PsycINFO, and EconLit (last searched 12th April 2019; Supplementary Tables 1 and 2), as well as in the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effect, the National Health Service Economic Evaluations Database and the Health Technology Assessment Database (last searched on 11th April 2019; Supplementary Tables 3 and 4). Supplementary searches of major schizophrenia and pharmacoeconomics conferences held between 2014 and 2015 were conducted using the Northern Light Life Sciences Conference Abstracts and Embase databases (Supplementary Table 5). Proceedings of major schizophrenia and pharmacoeconomics congresses held within the last three years (January 2016 through April 2019) were searched by hand (Supplementary Table 6). Conference searches were restricted by date under the assumption that conference presentations not subsequently published as journal articles within the past five years are likely to be of low quality. Finally, hand searches of the bibliographies of all relevant SLRs, network meta-analyses, and all ultimately included, full-text journal articles were undertaken to identify any additional, relevant studies for inclusion in the review.
Titles and abstracts were screened by a single reviewer, with all included articles and a random sample of 10% of excluded articles checked by a second reviewer. Full-texts of all potentially eligible studies identified in the title/abstract screening were reviewed by two independent reviewers. Discrepancies were resolved at all stages by a third independent reviewer when necessary. Studies were eligible for inclusion if they were written in the English language and reported relevant outcomes. Outcomes of interest were those related to clinical, economic, or humanistic burden in early schizophrenia. Studies were required to include patients formally diagnosed with schizophrenia (e.g. according to the International Classification of Diseases [ICD] or Diagnostic and Statistical Manual of Mental Disorders [DSM] criteria). Patients were also required to have early schizophrenia, which was defined as being within the first episode of schizophrenia, being within five years since schizophrenia diagnosis, or being described as early in the course of disease according to the publication itself. Studies of caregivers of patients with early schizophrenia were additionally eligible for inclusion. The SLR was not focused on early-onset schizophrenia, therefore age was not used to define early schizophrenia. A broader definition of early psychosis or undiagnosed schizophrenia was avoided to reduce confounding given the heterogeneous nature of schizophrenia and other psychoses.
Studies were required to include a relevant comparator population (healthy controls, chronic schizophrenia, or other psychiatric disorders). Studies that included patients with early schizophrenia as a subset of a larger population were included only if relevant outcomes were presented separately for these patients. To focus on data more likely to be representative of clinical practice, only observational studies, SLRs, or narrative reviews were included. The review was restricted to articles published in or after 2005 to focus on areas of burden that are relevant to current clinical practice.
Data extraction and analysis
Relevant data from full-text publications and conference proceedings (abstracts, posters, or oral presentations) were extracted into pre-defined extraction tables in Microsoft Excel. Data extraction was performed by a single individual for each included study. A second individual independently verified the extracted information, while a third individual arbitrated any discrepancies. A list of data variables that were extracted is provided in Supplementary Table 7. Quality assessment was performed using the Downs and Black checklist for non-randomized studiesCitation13.
Results
Included studies
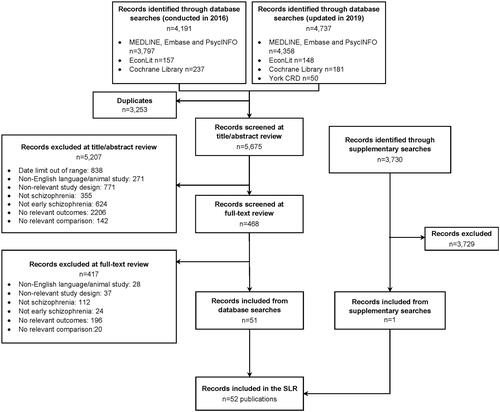
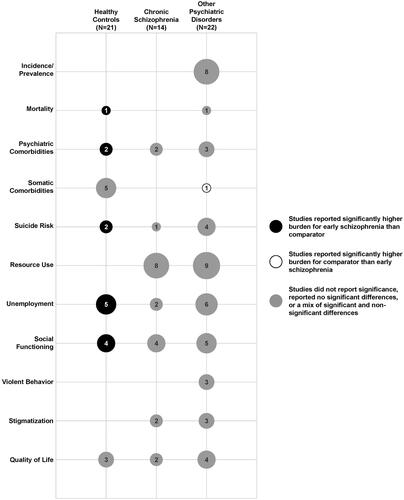
After removing duplicates, a total of 5675 citations were identified (). From these, 52 publications were included. Twenty publications reported outcomes for early schizophrenia compared with a healthy control population, 18 compared with other psychiatric disorders, 9 compared with chronic schizophrenia, 4 compared with both chronic schizophrenia and other psychiatric disorders, and 1 compared with chronic schizophrenia and a healthy control population (). Further characteristics of the included studies are provided in Supplementary Tables 8 and 9. Based on the Downs and Black checklistCitation13, studies were generally of good quality. Full results of the quality assessment are provided as in Supplementary Tables 10 and 11.
Clinical burden
Incidence and prevalence
Eight publications reported the incidence or prevalence of early schizophrenia compared with other psychiatric disorders, mostly for regions of EnglandCitation14–21. Studies on the incidence of schizophrenia were relatively old, with the most recent reporting data up to 2011Citation18. Reported incidence rates of schizophrenia ranged from 4.1 to 13.2 cases per 100,000 person-years, while rates for other non-affective psychoses or schizophrenia spectrum disorders ranged from 3.6 to 17.0 per 100,000 person-years, and rates for affective psychoses from 1.5 to 8.9 per 100,000 person-yearsCitation16,Citation18–20.
Four publications reported prevalence as the proportion of first-episode psychosis patients with a diagnosis of schizophreniaCitation14–16,Citation21. Variation in the psychiatric disorders reported in these papers, as well as differences in geographical location between studies makes it challenging to determine how the prevalence of schizophrenia compares with other disorders. Nevertheless, there was a general trend towards schizophrenia making up a smaller proportion of psychosis diagnoses in more recent studies (57% of all psychoses before 1980Citation16; 31‒34% before 2000Citation16; 13% up to 2005Citation14,Citation15 and 11% up to 2011Citation21). Kirkbride et al. conducted a longitudinal comparison of schizophrenia rates between 1978 and 1999 and hypothesized this trend may reflect increased reluctance to diagnose schizophrenia on initial presentation, or increased incidence of other non-affective psychosesCitation16. No data on the prevalence of early versus chronic schizophrenia were identified.
Mortality
Only one study reported all-cause mortality for early schizophrenia compared with the general populationCitation22. It found mortality rates to be significantly higher for the schizophrenia group, regardless of the level of antipsychotic exposure (range in hazard ratios: 2.31–9.90)Citation22. In contrast, a study of patients with early psychosis found that neither diagnosis of schizophrenia nor diagnosis of brief psychosis at first hospitalization were significant risk factors for non-suicide deathsCitation21.
Psychiatric comorbidities
Comorbid diagnosed depression was not reported in the studies identified in this review, however, two publications assessed depressive symptoms in first-episode schizophrenia using the Hamilton Rating Scale for Depression and Beck’s Depression Inventory, respectivelyCitation23,Citation24. They found that patients with first-episode schizophrenia had significantly higher levels of depression than healthy controls (p < .01)Citation23,Citation24. Compared with chronic schizophrenia, patients with early schizophrenia had higher levels of depression, reaching significance in one studyCitation25, but not in a second studyCitation24.
Findings from comparisons with other psychiatric disorders were mixed. One study found substance use disorder was the most common comorbid disorder in both patients with first-episode schizophrenia (62.9% [178/283]) and first-episode schizoaffective disorder (68.8% [44/64])Citation26. Conversely, no significant differences in the rates of comorbid substance use disorder, psychiatric disorder or major depressive disorder were seen between the two groupsCitation26. A further study using the Calgary Depression Scale reported no significant differences in scores between patients with first-episode psychosis diagnosed with schizophrenia compared with those diagnosed with delusional disorderCitation27. On the other hand, a second study reported a higher frequency of psychiatric comorbidities, particularly affective disorder, in patients with first-episode delusional disorder compared with first-episode schizophrenia (p = .009)Citation28.
Somatic comorbidities
Six studies reported somatic comorbidities in early schizophreniaCitation15,Citation25,Citation29–32, mostly comparing metabolic or cardiovascular comorbidities in first-episode schizophrenia with healthy controls. Some studies concluded there was a higher risk of comorbidities in patients with early schizophrenia than in healthy controls (impaired glucose tolerance [p = .002] and suspected Brugada syndrome [p < .001])Citation29,Citation31. Conversely, others reported no significant difference (impaired fasting glucose, metabolic syndrome, and cardiovascular risk)Citation29,Citation30,Citation32, or did not report significance (metabolic syndrome)Citation32,Citation33. No studies compared somatic comorbidities between early and chronic schizophrenia, and there was only one study comparing early schizophrenia with another psychiatric disorderCitation15. This study found that patients with psychotic depression had a significantly higher prevalence of physical health problems both at presentation and after one year of follow-up compared with those with schizophrenia (p < .05)Citation15.
Risk of suicide
The rates of suicide attempts by patients with early schizophrenia ranged from 8.8% to 20.0%Citation26,Citation34–36. Two studies investigated the risk of suicide in early schizophrenia compared with healthy controls, finding the risk of both suicide and suicide attempts to be significantly higher in early schizophrenia (p < .05)Citation36,Citation37. On the other hand, the only study comparing early and chronic schizophrenia populations found no significant differences in the rate of suicide attempts between the two groupsCitation35. Amongst the four studies reporting suicide rates in comparison with other psychiatric disorders, two reported no significant differences in suicide attempt rates compared with first-episode schizoaffective disorder or mania with psychotic featuresCitation26,Citation34. The remaining two considered rates of suicide deaths but did not conduct statistical testingCitation21,Citation37.
Economic burden
Hospitalization and resource use
No studies reported costs associated specifically with early phases of schizophrenia. Nonetheless, hospitalization-related outcomes were reported in several studies comparing early schizophrenia with chronic schizophrenia and other psychiatric disorders (). Studies comparing early versus chronic schizophrenia showed a trend towards higher mean numbers of hospitalizations for patients with chronic schizophrenia, which reached significance in 3 of 6 studies (p < .05)Citation24,Citation38,Citation39. The remaining studies did not report statistical analyses or found no significant differencesCitation35,Citation40,Citation41. One study showed patients with chronic schizophrenia had a significantly longer duration of hospital stay compared with early schizophreniaCitation42.
Table 1. Inpatient hospitalization resource use data in early schizophrenia patient cohorts.
The results were mixed when patients with first-episode schizophrenia were compared with those with other psychiatric disorders. Hospitalization-related resource use was reported to be significantly higher for early schizophrenia compared with bipolar disorder (p < .001)Citation43, but lower compared with schizoaffective disorder (p < .05)Citation26. A further study reported that patients with first-episode psychotic mania had a significantly higher mean number of hospital admissions over three years than patients with first-episode schizophrenia, but significantly fewer readmissionsCitation34,Citation44. The remaining studies either found no statistically significant differences or did not report statistical significanceCitation14,Citation15,Citation28,Citation45.
No significant differences were reported for the proportions of patients with early schizophrenia using antipsychotics compared with chronic schizophrenia or first-episode delusional disorderCitation27,Citation28,Citation46, although one study reported some significant differences in the antipsychotics used between early and chronic schizophrenia groupsCitation35. Regarding outpatient resource use, one study found that 63% of illicit substance users with first-episode schizophrenia and 37% of patients with drug-induced psychosis were in contact with secondary care services in the UK within the first year (statistical significance not reported)Citation14. A second study reported a significantly lower rate of outpatient contacts by patients with incident bipolar disorder compared with schizophrenia (p < .001)Citation43.
Unemployment
Unemployment rates for early schizophrenia ranged from 10% to 88% across the 13 studies included in this review. Employment rates were consistently lower for patients with early schizophrenia compared with healthy controls (p < .01)Citation47–51. Compared with chronic schizophrenia, one study found that unemployment was significantly lower in the early schizophrenia cohort (p < .001)Citation52, whereas a second showed a numerical decrease in unemployment in the early schizophrenia group, although no statistical analysis was performedCitation40. Between early schizophrenia and other psychiatric disorders (first-episode major depressive disorder, schizoaffective disorder, and delusional disorder) unemployment rates were relatively consistentCitation26,Citation27,Citation45, although it was also reported that in comparison with first-episode psychotic mania and schizoaffective disorder, patients with early schizophrenia had a significantly higher rate of unemployment (p < .05)Citation34,Citation44,Citation53.
Humanistic burden
Social functioning
Twelve publications reported social functioning outcomes in early schizophrenia versus healthy controls, chronic schizophrenia, and other psychiatric disorders ()Citation28,Citation34,Citation39,Citation42,Citation44,Citation54–60. Patients with early schizophrenia showed significantly poorer social functioning compared with healthy controls (p < .05)Citation54–56,Citation59. On the other hand, studies comparing with chronic schizophrenia did not conduct statistical comparisons or found no significant differencesCitation35,Citation39,Citation57,Citation58. Two studies found that patients with first-episode schizophrenia experienced significantly poorer social functioning when compared with psychotic mania and brief psychotic disorder (p < .05)Citation34,Citation44,Citation60 while further studies found no significant difference versus delusional disorderCitation28, or other psychiatric disorders with psychosisCitation58.
Table 2. Social functioning data in early schizophrenia patient cohorts.
Violent behavior
No studies reported on the occurrence of violent behavior in early schizophrenia versus chronic schizophrenia or healthy controls. Two studies found no significant differences for first-episode schizophrenia with current illicit drug use compared with patients with drug-induced psychosisCitation14, or for first-episode schizophrenia compared with psychotic maniaCitation34, respectively. A third study reported those with early schizophrenia being significantly more likely to have harmed others or property by the time they presented to secondary care compared with patients with psychotic depression (p < .05)Citation15.
Stigmatization
Two publications reported on studies of public opinion in Australia regarding stigmatization of people with early schizophrenia compared with chronic schizophrenia, depression, depression with suicidal thoughts, social phobia, and post-traumatic stress disorderCitation61,Citation62. The majority of participants (73.9% [95% CI: 70.7–76.9]) thought patients with early schizophrenia were likely to be discriminated against. The rate was lower compared with those with chronic schizophrenia (73.9% vs 84.1%; p < .05), but higher compared with the other psychiatric disordersCitation61,Citation62. A third publication reported on interviews with patients with first-episode schizophrenia (N = 150) from several European countries including Austria, Croatia, Czech Republic, Poland, Romania, Sweden, and TurkeyCitation45. Compared with patients with first-episode major depressive disorder, patients with schizophrenia reported a lower total Discrimination and Stigma Scale (DISC-12) score for experienced discrimination (p = .03)Citation45. More patients with schizophrenia reported negative discrimination from police, however in all other life areas discrimination was more frequent in the group with depression, reaching statistical significance for marriageCitation45.
Quality of life
Nine studies assessed QoL and happiness in patients with first-episode schizophrenia relative to healthy controls, chronic schizophrenia, or other psychiatric disorders ()Citation19,Citation27,Citation39,Citation52–54,Citation63–Citation65. Two of the three studies comparing QoL or happiness with healthy controls reported no significant differencesCitation54,Citation63, with the remaining study reporting significantly poorer scores on the SF-36 scale for patients with early schizophrenia (p < .01)Citation65. In comparison with chronic schizophrenia, one study reported no significant differenceCitation39, while the other reported significantly poorer QoL for patients with chronic schizophrenia (p = .02)Citation52. Findings from studies that compared early schizophrenia with other psychiatric disorders were similarly mixed. One study reported significantly poorer scores for early schizophrenia compared with schizophreniform and schizoaffective disorders (p < .05)Citation64. A second study using a different QoL measure found no significant differences between early schizophrenia and schizoaffective disorderCitation53. A further study reported significantly poorer QoL for early schizophrenia compared with bipolar disorder (p < .001), but no significant difference compared with major depressive disorderCitation19. The remaining study found no significant differences between first-episode schizophrenia and delusional disorderCitation27.
Table 3. Quality of life data in early schizophrenia patient cohorts.
Discussion
Disease burden in early schizophrenia
The literature identified by this review illustrates there are multiple sources of burden for patients with schizophrenia compared with healthy controls, even at the early stages of the disease. All-cause mortality, risk of suicide, and psychiatric comorbidities were significantly higher in patients with early schizophrenia compared with the general population, and it has been suggested previously that patients with schizophrenia are at a particularly high risk of suicide in the first few years after diagnosisCitation66,Citation67. A thorough assessment of suicide risk is therefore crucial during the early management of schizophrenia. Social functioning outcomes were consistently poorer for patients with early schizophrenia and correspondingly unemployment rates were higher compared with healthy controls. Together, this highlights the disruption that symptoms of schizophrenia can cause even at the onset of disease and the importance of multidisciplinary care involving psychosocial intervention at an early stage.
Comparisons with chronic schizophrenia and other psychiatric disorders were less conclusive, with a high proportion of studies finding no significant differences. Nevertheless, there was a general trend to worsening burden with more chronic disease and poorer social functioning outcomes for patients with early schizophrenia compared with patients with other psychiatric disorders.
Data gaps
Some notable data gaps were identified. No studies assessed the prevalence of early versus chronic schizophrenia, while studies comparing early schizophrenia with other psychiatric disorders were limited to European cohorts only and dominated by historic data with potentially limited relevance today. Additional literature gaps include the lack of data on caregiver burden or comprehensive description of comorbidities, including cardiac and hepatic comorbidities that are important risk factors for early mortality in patients with schizophreniaCitation68–70. Furthermore, although QoL was widely reported across the studies, a surprising finding was the large variation in QoL measurements, with only one study utilizing the Schizophrenia Quality of Life Scale, a commonly used scale to assess QoL and functioning in schizophreniaCitation39.
Further noteworthy data gaps were identified regarding economic burden, as no studies measuring direct or indirect costs attributed to early schizophrenia were found. Some data relating to resource use were identified, however, these were mostly outcomes reported as baseline characteristics, such as inpatient hospital stays and outpatient contacts. Considering literature beyond the scope of this review, a study of USA claims data for schizophrenia spectrum disorder patients found that more patients in their first year of disease were hospitalized compared with chronic patients and that they had significantly higher treatment costsCitation71. Costs related to inpatient hospitalization were a major component of overall treatment costs, particularly for those with disease duration of less than one yearCitation71. A further known aspect of the economic and humanistic burden of schizophrenia is criminal offending, with higher risks of convictions for violent crimes reported for people with schizophrenia than the general populationCitation72, but related data specifically for early schizophrenia were not identified in this review.
Limitations
Some limitations of this research should be noted. Studies were often small and were not always primarily intended to collect data on the disease burden or to make formal comparisons between early schizophrenia and the groups of interest in this review. In addition, a small proportion of the included studies were conference abstracts that may not have been peer reviewed as rigorously as full journal publications.
Metrics used to measure various aspects of burden varied across studies and as a result, few studies reported on any given outcome. Confounding factors such as age and duration of medication exposure could have affected comparisons between the groups of interest, in particular when considering comparisons between early and chronic schizophrenia. Nonetheless, due to the small number of studies identified it was not possible to conduct a quantitative assessment of the impact of these factors. Further variation between studies could be due to differences in diagnostic criteria used, although most studies reported using DSM-IV or ICD-10 (Supplementary Table 8). Furthermore, not all studies reported diagnostic codes to confirm only a “pure schizophrenia” population was included, therefore some studies with mixed schizophrenia disorder populations may have been included in this review inadvertently. Finally, there was wide variation between studies in terms of how early and chronic schizophrenia were defined.
Since this review focused on the burden associated with early schizophrenia, search terms related to “early” were used to refine the searches. These terms were based on a prior review of the literature conducted by our group to identify definitions of early schizophreniaCitation73. It is possible, however, that some studies on the incidence of schizophrenia, or studies following patients from the first diagnosis but not specifically concerned with the early stages of schizophrenia, would not have been identified if they did not use terminology related to “early”. Certain aspects of disease burden were not considered in this review. Notably, general functioning scores, including the global assessment of function (GAF) were not extracted. Finally, and particularly when considering the literature gaps, it should be kept in mind that this review only included articles published in or after 2005 and written in the English language.
Conclusions
This review has highlighted several areas of burden for patients with early schizophrenia, including increased mortality, psychiatric comorbidities such as substance abuse and depression, poorer social functioning, and increased levels of unemployment. While the burden of early schizophrenia relative to healthy controls is evident, comparisons with chronic schizophrenia and other psychiatric disorders are less conclusive. Various gaps in available data were uncovered, for example for incarcerations, caregiver burden, and outpatient costs, and even for the more widely reported outcomes there were still few studies identified on each aspect of burden in early schizophrenia overall.
Transparency
Declaration of funding
This work was supported by H. Lundbeck A/S and Otsuka Pharmaceutical Europe Ltd.
Declaration of financial/other relationships
This study was initiated and sponsored by H. Lundbeck A/S and Otsuka Pharmaceutical Europe Ltd. PS and A-GN are employees of H. Lundbeck A/S. JM is an employee of Otsuka Pharmaceutical Europe Ltd. SS, HKR, EW, MO and ED were employees of Costello Medical Consulting at the time of this research and were supported by a grant from H. Lundbeck A/S for this study. BC-F and RN received an honorarium from H. Lundbeck A/S for their participation in the study but did not receive remuneration for their contribution to the development of this manuscript.
Author contributions
Study concept and design: PS, A-GN, JM, SS; acquisition, analysis or interpretation of data: all authors; drafting of the manuscript: all authors; critical revision of the manuscript for important intellectual content: all authors; obtained funding: A-GN, JM; study supervision: PS, A-GN, JM, SS; administrative, technical or material support: PS, A-GN, JM, HKR, EW, MO, ED, SS.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Supplemental Material
Download MS Word (161.4 KB)Acknowledgements
No assistance in the preparation of this article is to be declared.
References
- Ayesa-Arriola R, de la Foz VO-G, Martínez-García O, et al. Dissecting the functional outcomes of first episode schizophrenia spectrum disorders: a 10-year follow-up study in the PAFIP cohort. Psychol Med. 2019;18:1–14.
- James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858.
- World Health Organization (WHO). Schizophrenia; [cited 2020 Jun 15]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/schizophrenia.
- Millier A, Schmidt U, Angermeyer MC, et al. Humanistic burden in schizophrenia: a literature review. J Psychiatr Res. 2014;54:85–93.
- Mayoral‐van Son J, Juncal‐Ruiz M, Ortiz‐García de la Foz V, et al. Understanding the direct and indirect costs of a first episode of psychosis program: insights from PAFIP of Cantabria, Spain, during the first year of intervention. Early Intervent Psychiatry. 2019;13(5):1182–1190.
- Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–1306.
- Karson C, Duffy RA, Eramo A, et al. Long-term outcomes of antipsychotic treatment in patients with first-episode schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:57–67.
- Murru A, Carpiniello B. Duration of untreated illness as a key to early intervention in schizophrenia: a review. Neurosci Lett. 2018;669:59–67.
- Penttilä M, Jääskeläinen E, Hirvonen N, et al. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205(2):88–94.
- Penttilä M, Miettunen J, Koponen H, et al. Association between the duration of untreated psychosis and short-and long-term outcome in schizophrenia within the Northern Finland 1966 Birth Cohort. Schizophr Res. 2013;143(1):3–10.
- Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75(6):555–565.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- Crebbin K, Mitford E, Paxton R, et al. First-episode drug-induced psychosis: a medium term follow up study reveals a high-risk group. Soc Psychiatry Psychiatr Epidemiol. 2009;44(9):710–715.
- Crebbin K, Mitford E, Paxton R, et al. First-episode psychosis: An epidemiological survey comparing psychotic depression with schizophrenia. J Affect Disorders. 2008;105(1–3):117–124.
- Kirkbride JB, Croudace T, Brewin J, et al. Is the incidence of psychotic disorder in decline? Epidemiological evidence from two decades of research. Int J Epidemiol. 2009;38(5):1255–1264.
- Louhija U-M, Saarela T, Juva K, et al. Brain atrophy is a frequent finding in elderly patients with first episode psychosis. Int Psychogeriatr. 2017;29(11):1925–1929.
- Mule A, Sideli L, Capuccio V, et al. Low incidence of psychosis in Italy: confirmation from the first epidemiological study in Sicily. Soc Psychiatry Psychiatr Epidemiol. 2017;52(2):155–162.
- Owoeye O, Kingston T, Scully PJ, et al. Epidemiological and clinical characterization following a first psychotic episode in major depressive disorder: comparisons with schizophrenia and bipolar I disorder in the Cavan-Monaghan First Episode Psychosis Study (CAMFEPS). Schizophr Bull. 2013;39(4):756–765.
- Reay R, Mitford E, McCabe K, et al. Incidence and diagnostic diversity in first-episode psychosis. Acta Psychiatr Scand. 2010;121(4):315–319.
- Stralin P, Hetta J. Medication, hospitalizations and mortality in 5 years after first-episode psychosis in a Swedish nation-wide cohort. Early Interv Psychiatry. 2019;13(4):902–907.
- Torniainen M, Mittendorfer-Rutz E, Tanskanen A, et al. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2015;41(3):656–663.
- Jhung K, Park JY, Song YY, et al. Experiential pleasure deficits in the prodrome: a study of emotional experiences in individuals at ultra-high risk for psychosis and recent-onset schizophrenia. Compr Psychiatry. 2016;68:209–216.
- Leung JS, Lee TM, Lee CC. Facial emotion recognition in Chinese with schizophrenia at early and chronic stages of illness. Psychiatry Res. 2011;190(2–3):172–176.
- Shrivastava A, Shah N, Johnston M, et al. Predictors of long-term outcome of first-episode schizophrenia: a ten-year follow-up study. Indian J Psychiatry. 2010;52(4):320–326.
- Cotton SM, Lambert M, Schimmelmann BG, et al. Differences between first episode schizophrenia and schizoaffective disorder. Schizophr Res. 2013;147(1):169–174.
- Rowland T, Birchwood M, Singh S, et al. Short-term outcome of first episode delusional disorder in an early intervention population. Schizophr Res. 2019;204:272–303.
- Hui CL, Lee EH, Chang WC, et al. Delusional disorder and schizophrenia: a comparison of the neurocognitive and clinical characteristics in first-episode patients. Psychol Med. 2015;45(14):3085–3095.
- Chen DC, Du XD, Yin GZ, et al. Impaired glucose tolerance in first-episode drug-naive patients with schizophrenia: relationships with clinical phenotypes and cognitive deficits. Psychol Med. 2016;46(15):3219–3230.
- Nyboe L, Vestergaard CH, Moeller MK, et al. Metabolic syndrome and aerobic fitness in patients with first-episode schizophrenia, including a 1-year follow-up. Schizophr Res. 2015;168(1–2):381–387.
- Sutterland A, Blom M, De Haan L, et al. Studying heart arrhythmias in relation to psychosis (SHARP). Increased prevalence of suspect Brugada ECG in recent onset schizophrenia. Early Intervent Psychiatry. 2014;8(Suppl 1):59.
- Uz Y, Gulec H. Cardiometabolic risk in Turkish patients with first episode schizophrenia. Klinik Psikofarmakoloji Bulteni. 2014;24(suppl 1):S316.
- Srivastava S, Bhatia MS, Sharma A. Comparative study of quality of life and metabolic syndrome in schizophrenia patients who are receiving treatment versus antipsychotic naive, first episode patients from a tertiary care hospital. Asian J Psychiatr. 2018;31:121–123.
- Chang WC, Lau ESK, Chiu SS, et al. Three-year clinical and functional outcome comparison between first-episode mania with psychotic features and first-episode schizophrenia. J Affect Disord. 2016;200:1–5
- García-Álvarez L, Garcia-Portilla MP, Caso JR, et al. Early versus late stage schizophrenia. What markers make the difference? World J Biol Psychiatry. 2019;20(2):159–165.
- Zhang XY, Du X, Yin G, et al. Prevalence and clinical correlates of and cognitive function at the time of suicide attempts in first-episode and drug-naive patients with schizophrenia. Austral NZ J Psychiatry. 2018;52(9):864–875.
- Randall JR, Walld R, Finlayson G, et al. Acute risk of suicide and suicide attempts associated with recent diagnosis of mental disorders: a population-based, propensity score-matched analysis. Can J Psychiatry. 2014;59(10):531–538.
- Pawelczyk T, Szymanska B, Grancow-Grabka M, et al. Telomere length in blood cells is related to the chronicity, severity, and recurrence rate of schizophrenia. Neuropsychiatr Dis Treat. 2015;11:1493–1503.
- Kim SJ, Shim JC, Kong BG, et al. Differences in cognitive function and daily living skills between early- and late-stage schizophrenia. Int J Psychiatry Clin Pract. 2015;19(4):245–251.
- Dubois V, Peuskens J, Geerts P, et al. Clinical outcomes of long-acting risperidone in recent versus long-term diagnosed Belgian schizophrenic patients: results from electronic Schizophrenia Treatment Adherence Registry (e-STAR) and Trial for the Initiation and Maintenance Of REmission in Schizophrenia with risperidone (TIMORES). Early Intervent Psychiatry. 2014;8(1):39–49.
- Matsuda Y, Sato S, Hatsuse N, et al. Neurocognitive functioning in patients with first-episode schizophrenia 1 year from onset in comparison with patients 5 years from onset. Int J Psychiatry Clin Pract. 2014;18(1):63–69.
- Mwansisya TE, Yi W, Wang Z, et al. Comparison of psychosocial determinants in inpatients with first-episode and chronic schizophrenia in China. Arch Psychiatr Nurs. 2013;27(1):32–41.
- Laursen MF, Licht R, Valentin JB, et al. Prognosis of early-onset bipolar disorder compared to early-onset schizophrenia and healthy controls in a nationwide register based study. Early Intervent Psychiatry. 2018;12(Supplement 1):152.
- Chang CW, Lau ES, Hui LM, et al. Three-year outcome comparison between patients presenting with first-episode psychotic mania and schizophrenia to easy program in Hong Kong. Schizophr Res. 2014;153:S304-S305.
- Corker EA, Beldie A, Brain C, et al. Experience of stigma and discrimination reported by people experiencing the first episode of schizophrenia and those with a first episode of depression: the FEDORA project. Int J Soc Psychiatry. 2015;61(5):438–445.
- Softic R, Becirovic E, Mirkovic Hajdukov M. Rehospitalization rate of first episode and chronic schizophrenia patients one year after discharge. Eur Psychiatr. 2016;33(S1):S587–S587.
- Bliksted V, Fagerlund B, Weed E, et al. Social cognition and neurocognitive deficits in first-episode schizophrenia. JAMA Psychiatry. 2014;71(10):1121–1128.
- Bliksted V, Frith C, Videbech P, et al. Hyper- and hypomentalizing in patients with first-episode schizophrenia: FMRI and behavioral studies. Psychoneuroendocrinology. 2019;104(2):269–275.
- Bliksted V, Videbech P, Fagerlund B, et al. The effect of positive symptoms on social cognition in first-episode schizophrenia is modified by the presence of negative symptoms. Neuropsychology. 2017;31(2):209–219.
- Fervaha G, Agid O, McDonald K, et al. Daily activity patterns in remitted first-episode schizophrenia. Compr Psychiatry. 2014;55(5):1182–1187.
- Huang ZH, Hou CL, Huang YH, et al. Individuals at high risk for psychosis experience more childhood trauma, life events and social support deficit in comparison to healthy controls. Psychiatry Res. 2019;273:296–302.
- Bamiso Makanjuola A, Ademola Adeponle B, Ayodele Obembe O. A comparison of quality-of-life in schizophrenia and affective disorder patients in a Nigerian tertiary hospital. Transcult Psychiatry. 2007;44(1):65–78.
- Sim K, Chan YH, Chong SA, et al. A 24-month prospective outcome study of first-episode schizophrenia and schizoaffective disorder within an early psychosis intervention program. J Clin Psychiatry. 2007;68(9):1368–1376.
- Agid O, McDonald K, Siu C, et al. Happiness in first-episode schizophrenia. Schizophr Res. 2012;141(1):98–103.
- Agid O, Siu C, Harvey PD, et al. Treatment outcomes, insight and recovery in first-episode schizophrenia. Schizophr Res. 2014;153:S165–S166.
- Ballon JS, Kaur T, Marks II, et al. Social functioning in young people at risk for schizophrenia. Psychiatry Res. 2007;151(1–2):29–35.
- Bougie JK, Malla A, Miguelez M, et al. Real life assessment of abilify maintena (reliam): interim analysis from a Canadian naturalistic study of aripiprazole long-acting injectable in patients with schizophrenia. Value Health. 2017;20(5):A293.
- Higuchi Y, Sumiyoshi T, Seo T, et al. Associations between daily living skills, cognition, and real-world functioning across stages of schizophrenia; a study with the Schizophrenia Cognition Rating Scale Japanese version. Schizophr Res Cogn. 2017;7:13–18.
- Jaracz K, Górna K, Rybakowski F. Social functioning in first-episode schizophrenia. A prospective follow-up study. Arch Psychiatry Psychotherapy. 2007;4:19–27.
- Lee EH, Hui CL, Chang WC, et al. Letter to the editor: comparison of cognitive functions, pre-morbid conditions and clinical characteristics between brief psychotic disorder and schizophrenia. Psychol Med. 2016;46(9):2011–2013.
- Reavley NJ, Jorm AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian National Survey of Mental Health Literacy and Stigma. Aust NZ J Psychiatry. 2011;45(12):1086–1093.
- Reavley NJ, Jorm AF. Stigmatising attitudes towards people with mental disorders: changes in Australia over 8 years. Psychiatry Res. 2012;197(3):302–306.
- Agid O, McDonald K, Fervaha G, et al. Values in first-episode schizophrenia. Can J Psychiatry. 2015;60(11):507–514.
- Al-Bataineh R, Crasan A, Purnichi T, et al. Is diagnosis indeed prognosis? 12 months outcome for schizophrenia, schizophreniform and schizoaffective disorder. Eur Neuropsychopharmacol. 2016;26(Suppl. 1):S49–S50.
- Law CW, Chen EY, Cheung EF, et al. Impact of untreated psychosis on quality of life in patients with first-episode schizophrenia. Qual Life Res. 2005;14(8):1803–1811.
- Fleischhacker WW, Kane JM, Geier J, et al. Completed and attempted suicides among 18,154 subjects with schizophrenia included in a large simple trial. J Clin Psychiatry. 2014;75(3):e184.
- Ventriglio A, Gentile A, Bonfitto I, et al. Suicide in the early stage of schizophrenia. Front Psychiatry. 2016;7:116.
- Hoang U, Stewart R, Goldacre MJ. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999–2006. BMJ. 2011;343(1):d5422–d5422.
- Nordentoft M, Wahlbeck K, Hällgren J, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLOS One. 2013;8(1):e55176.
- Tsai KY, Lee CC, Chou YM, et al. The incidence and relative risk of stroke in patients with schizophrenia: a five-year follow-up study. Schizophr Res. 2012;138(1):41–47.
- Nicholl D, Akhras KS, Diels J, et al. Burden of schizophrenia in recently diagnosed patients: healthcare utilisation and cost perspective. Curr Med Res Opin. 2010;26(4):943–955.
- Hodgins S, Piatosa MJ, Schiffer B. Violence among people with schizophrenia: phenotypes and neurobiology. In: Neuroscience of Aggression. Springer; 2013. p. 329–368.
- Newton RR, Nylander AG, Loze JY, et al. Diverse definitions of the early course of schizophrenia—a targeted literature review. NPJ Schizophr. 2018;4(1):21.
- Ivarsson T, Broberg AG, Arvidsson T, et al. Bullying in adolescence: psychiatric problems in victims and bullies as measured by the Youth Self Report (YSR) and the Depression Self-Rating Scale (DSRS). Nord J Psychiatry. 2005;59(5):365–373.
- Birchwood M, Smith J, Cochrane R, et al. The social functioning scale the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157(6):853–859.
- Diener E, Emmons RA, Larsen RJ, et al. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75.
- Lyubomirsky S, Lepper HS. A measure of subjective happiness: preliminary reliability and construct validation. Social Indicators Res. 1999;46(2):137–155.
- Burckhardt CS, Anderson KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1(1):60.