Abstract
Objective
To measure health state preferences and estimate utility values for tardive dyskinesia (TD) from the perspective of the US general population, accounting for factors affecting quality of life (QOL).
Methods
Participants from the general population were recruited and asked to watch and assess videos of professional actors simulating nine health states, including psychiatric disorders with/without TD and moderate-to-severe TD without any underlying disease. Time tradeoff (TTO) methods were used to elicit utility values, which ranged from −1 (worse than death) to +1 (perfect health) and represented individual preferences for avoiding specific health states associated with TD. Lower TTO utility values indicated individuals’ willingness to give up more years of life to avoid living in each health state.
Results
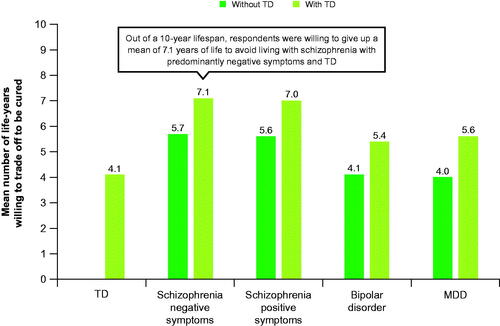
Based on TTO responses (n = 157), mean ± standard deviation utility for TD alone was 0.59 ± 0.38. Mean utilities for schizophrenia with negative symptoms (without TD: 0.43; with TD: 0.29) and positive symptoms (without TD: 0.44; with TD: 0.30) were generally lower than those for bipolar disorder (without TD: 0.59; with TD: 0.46) and major depressive disorder (without TD: 0.60; with TD: 0.44). According to utility decrements associated with TD (0.13–0.16), respondents were willing to give up 1.3 to 1.6 years during a 10-year lifespan to avoid living with TD.
Conclusions
Utility decrements for TD in this study were slightly larger than previously reported values, potentially due to incorporation of QOL and social consequences in TD health state descriptions. An important limitation of this analysis is that participants’ willingness to trade future years of healthy life may not indicate actual willingness to accept the life decrement. These findings can be leveraged to improve cost-effectiveness analyses used to assess the value of treatments for TD.
Introduction
Schizophrenia, bipolar disorder, and major depressive disorder (MDD) are psychiatric disorders associated with profound impairments in social and occupational functioningCitation1. According to the World Health Organization, these disorders are among the leading causes of global years lived with disabilityCitation2. Antipsychotic medications are the first-line treatment for schizophrenia, and they are often used as monotherapy or adjunctively to treat bipolar disorder or MDDCitation3–5. Despite their efficacy in treating symptoms and behaviors associated with these disorders, antipsychotic medications are associated with significant side effects, such as acute extrapyramidal symptoms (e.g. akathisia, dystonia, and parkinsonism) and persistent tardive dyskinesia (TD)Citation5,Citation6.
TD is characterized by involuntary movements that are typically stereotypic, choreiform, or dystonic and develops in association with dopamine-receptor antagonists used as typical or atypical antipsychotics, antidepressants, antiemetics, or for other indicationsCitation1,Citation7,Citation8. TD can occur in anyone receiving dopamine-receptor antagonists (e.g. for mood disorders as well as schizophrenia) and can significantly impair patients’ quality of life (QOL) by exposing them to social withdrawal, professional and social stigma, and disruption of treatment for underlying psychiatric disorders, which may negatively impact psychiatric stabilityCitation9–12. Vesicular monoamine transporter 2 (VMAT2) inhibitors are recommended as first-line therapy in patients with persistent TD if the use of dopamine-receptor antagonists cannot be limited or avoidedCitation13,Citation14.
Utility values represent individual preferences for avoiding specific disease states or conditions and are used to inform healthcare decision making. There are several methods for estimating utility values, including time tradeoff (TTO) and standard gamble (SG). To date, all TD utility studies have used SGCitation15,Citation16; however, SG has been shown to impose a high cognitive burden on respondents and to overestimate utilitiesCitation17,Citation18. In contrast, the TTO method, which is widely used to measure utilities for health states, has been shown to have less total bias than SGCitation18–21.
Although previous studies have measured the utility associated with TD, most do not capture QOL and social consequences when describing the TD health statesCitation15,Citation16. A few studies have provided respondents with a brief sense of how TD symptoms affect a patient’s life during the utility assessmentCitation17,Citation22; however, the health state descriptions still excluded key aspects of the disease, such as social stigma, which may lead to an underestimation of the disutility associated with TD as well as the value of TD treatment. This study provides an updated measure of the utility of TD using TTO, while considering important factors mediating QOL, including social stigma associated with TD.
Methods
Study design and population
This study elicited TD utility values from the US general population using computer-assisted telephone interviews (CATIs). Participants were shown videos as well as written vignettes depicting nine health states related to moderate-to-severe TD. Health states included mild-to-moderate schizophrenia with predominantly negative symptoms, schizophrenia with predominantly positive symptoms, bipolar disorder, and MDD, each with and without moderate-to-severe TD as well as TD without underlying disease. The scripted videos were recorded by professional actors, who simulated the health states with and without TD, to control for the underlying health states’ effects. The videos simulated dialogue between a patient and his/her psychiatrist to illustrate the most important symptoms and impairments of the health state, while the vignettes complemented the videos by summarizing the symptoms captured in the video and describing additional symptoms and the QOL associated with the health state. After watching each video and reading the vignette for a particular health state, participants rated the value of the health state on a visual analog scale (VAS) and responded to a series of TTO questions to assess their perceived utility of the health state. Each participant completed a training task and practice task prior to evaluating all nine health states to ensure they understood the concept of TTO. An example script and vignette are shown in the Supplemental Materials.
To ensure that video scripts and vignettes provided accurate and comprehensive descriptions of the health states, one-on-one interviews were conducted with eight external psychiatrists who were familiar with TD and the underlying psychiatric disorders as well as eight patients with TD and any of the underlying psychiatric disorders. Psychiatrists and patients did not necessarily have a relationship with one another. Interviews were conducted based on a structured interview guide, which was reviewed and approved by the New England Institutional Review Board. Eligible external psychiatrists were licensed psychiatrists in the United States who have treated patients with TD, schizophrenia, bipolar disorder, and/or MDD for the past ≥5 years and who have treated ≥5 patients with TD, schizophrenia, bipolar disorder, and/or MDD over the past 12 months. Patients were included if they were aged ≥18 years at the time of the interview; had a confirmed diagnosis of TD and a confirmed diagnosis of schizophrenia, bipolar disorder, or MDD; and were able to speak English. An expert with experience treating TD and the underlying psychiatric disorders reviewed the actors’ performances and provided feedback during filming to ensure the authenticity of the simulated symptoms and the appropriate severity levels of TD and underlying disorders for the purpose of this study.
Participants were recruited from the general US population through an online panel that was maintained by a well-established third-party global provider of data collection and market research, who also administered the survey. Individuals willing to participate responded to an initial online survey that verified eligibility according to the inclusion criteria. In order to ensure a margin of error <20% of the standard deviation (SD), 200 total participants were recruited. Information on the response rate was not available; only data from participants who completed the survey were available. Eligible participants were aged ≥18 years without a diagnosis of TD, schizophrenia, bipolar disorder, or MDD and were able to speak and read English. Participants were also required to be able to speak on the phone and have access to a computer screen (or tablet) to see the survey materials. If participants were deemed eligible, informed consent was collected before proceeding to the main survey questions and scheduling a CATI (approximately 50 min each without breaks). The survey terminated if informed consent was not provided. Participants who completed the full survey and the CATI were compensated for their participation in the study. The New England Institutional Review Board approved the study on 5 November 2019.
Outcomes and analyses
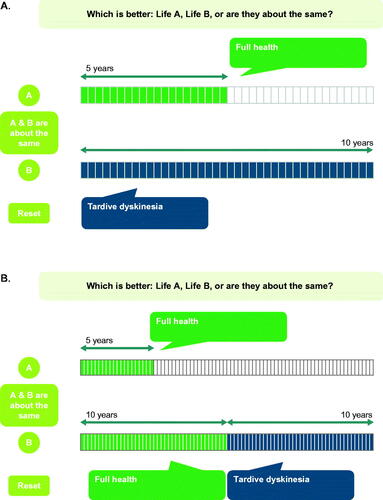
Participant demographics were collected to ensure that the study sample was representative of the US general population. The primary outcome was utility values estimated using TTO. TTO questions were illustrated using visual aids (). Utility values for TTO ranged from −1 (worse than death) to +1 (perfect health), with the smallest difference being 0.05. TTO utilities were validated using utility values obtained from the VAS, which ranged from 0 (worst imaginable health) to 100 (best imaginable health). VAS ratings were divided by 100 to obtain utility values for the health states. For the TD health states, participants watched the TD video, read the accompanying vignettes, and then evaluated the TD health state using VAS and TTO. For the health states with an underlying disorder, participants watched a video with uncontrolled symptoms and read the accompanying vignette before moving on to the video and vignette for the same disorder with controlled symptoms and evaluating the health state of the latter (with potential chance of relapse) using VAS and TTO. Finally, participants watched the video and read the vignette for the same disorder with controlled symptoms as well as TD and responded to VAS and TTO questions. Participants then completed the same sequence for the next underlying disorder. Health states of different underlying disorders were presented in a random order to reduce an ordering effect.
Figure 1. Example visual aids for TTO questions in the surveya. (A) Valuation of states considered to be better than death. (B) Valuation of states considered to be worse than death. TTO, time tradeoff. aFor states considered better than death, the protocol presents Life A as x years in full health and Life B as 10 years in the target state. For states considered worse than death, Life A is presented as x years in full health and Life B as 10 years in full health followed by 10 years in the target state. The tasks terminate when indifference is stated, and the direction of the tasks can be reversed at any point.
Participant characteristics, including age, sex, race, region, education, employment, household income, comorbidities, and current health status measured by VAS, were summarized descriptively. Current health VAS was reported as mean, standard deviation (SD), and range; other continuous variables were reported as mean (SD), while categorical variables were reported as frequency and percentage.
The validity of VAS and TTO ratings was assessed by testing results for logical errors. Logical errors were defined as a participant rating a more severe health state (e.g. bipolar disorder with TD) as better than a less severe health state (e.g. bipolar disorder alone). All ratings by any participants with logical errors were censored from the analyses due to potential bias in their response. Sensitivity analyses were conducted to assess the impact of removing logical errors on utility values. Two scenarios were evaluated: (1) answers with logical errors were removed, while logical answers from those participants were retained and (2) all responses from all participants were retained.
Results
Participant characteristics
A total of 157 participants provided valid responses to all TTO questions (). The mean (SD) age was 47 (18) years, and 56.1% were female. Overall, 44.6% of participants reported no chronic conditions. Among participants with chronic illnesses, the most common conditions were hypertension (24.8%), asthma (14.6%), diabetes (12.7%), and depression (10.2%). Using VAS, participants rated their mean (SD) current health status as 80 (16), where a score of 100 represents best imaginable health.
Table 1. Participant characteristics.
Utility values
According to TTO responses, the mean (SD) utility for moderate-to-severe TD alone was 0.59 (0.38). The mean (SD) utilities for mild-to-moderate schizophrenia with dominance of negative symptoms (without TD: 0.43 [0.39]; with TD: 0.29 [0.48]) and those for mild-to-moderate schizophrenia with dominance of positive symptoms (without TD: 0.44 [0.48]; with TD: 0.30 [0.54]) were similar and were lower than the mean utilities for mild-to-moderate bipolar disorder (without TD: 0.59 [0.38]; with TD: 0.46 [0.43]) and mild-to-moderate MDD (without TD: 0.60 [0.36]; with TD: 0.44 [0.44]; ). Utility decrements associated with moderate-to-severe TD when it occurred with an underlying psychiatric disorder ranged from 0.13 to 0.16 (), depending on the type of coexisting underlying psychiatric disorder. The full distributions of TTO responses for each health state are shown in Supplemental Figure S1. According to TTO responses, participants were willing to give up 1.3 to 1.6 years of life during a 10-year lifespan to avoid living with TD.
Figure 2. TTO utility values for the main sample (n = 157)a. MDD, major depressive disorder; TD, tardive dyskinesia; TTO, time tradeoff. aParticipants who demonstrated a misunderstanding of the health states by answering that the health state plus TD was preferable to the health state alone in the TTO have been removed from the sample.
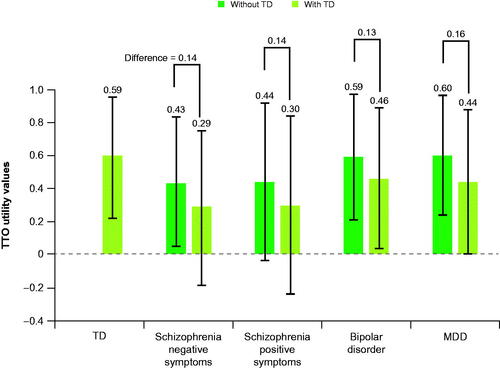
Figure 3. TTO results for the main sample (n = 157)a. MDD, major depressive disorder; TD, tardive dyskinesia; TTO, time tradeoff. aParticipants who demonstrated a misunderstanding of the health states by answering that the health state plus TD was preferable to the health state alone in the TTO have been removed from the sample.
Based on VAS responses, the mean (SD) utility for moderate-to-severe TD alone was 0.50 (0.21). VAS utility values for all health states were found to be in the same range as TTO utility values (Supplemental Figure S2). VAS utility decrements for TD ranged from 0.09 to 0.15, depending on underlying psychiatric disorder. Sensitivity analyses, which evaluated the inclusion of logical answers from participants who had any logical errors (Supplemental Figure S3) and the inclusion of all answers from all participants (Supplemental Figure S4), were not found to change the utility values significantly (i.e. changes in each utility value were ≤0.05).
Discussion
Although previous studies estimated the utility associated with TD, many did not capture QOL and social consequences when describing the TD health states, which may lead to an underestimation of the disutility associated with TD as well as the value of TD treatmentCitation15,Citation16. This study assessed utility values for health states associated with TD and found TD utility decrements to be slightly larger than those previously reported, potentially because of the incorporation of QOL and social consequences in TD health state descriptions.
Participants in the current study estimated the utility value for TD with no underlying psychiatric disorder to be 0.59. The mean utilities for schizophrenia, regardless of symptom dominance, were lower than the mean utility values for bipolar disorder and MDD. Based on TTO responses, the utility decrement associated with TD when it occurred with an underlying psychiatric disorder ranged from 0.13 to 0.16, suggesting that participants were willing to give up 1.3 to 1.6 years of life during a 10-year lifespan to avoid living with TD. Notably, the utility values for TD alone (0.59), bipolar disorder alone (0.59), and MDD alone (0.60) were all very similar, suggesting that the study population views these conditions as equivalently detrimental to their lives.
Findings from the current study differed from those previously reported, potentially because of the inclusion of QOL and social consequences in the health state descriptions. For example, in one study that elicited utility values from the general population using photographs, the utility value for TD with no underlying psychiatric disorder was estimated to be higher than the utility value reported in the current studyCitation15. The previous study reported the utility value for TD alone as 0.7, compared with 0.59 in the current studyCitation15. In another study, participants from the general population were shown videos describing health states and asked to estimate the utility decrement of TD associated with schizophreniaCitation17. In that study, the utility decrement of TD associated with schizophrenia was estimated to be smaller (0.095) than that in the current study (0.14)Citation17.
To date, all studies have examined the utility decrement of TD in addition to only one type of psychiatric disorder, despite TD presenting as a side effect of antipsychotic medications and commonly occurring with different underlying psychiatric disorders. This study expands upon the current literature by capturing several types of underlying psychiatric disorders (i.e. schizophrenia, bipolar disorder, and MDD) in addition to TD when estimating utility decrements. Additionally, this study used TTO methods to elicit utility values, as opposed to the SG method. SG is grounded in expected utility theory; however, it has been shown to be associated with significant cognitive burden and lead to greater total biasCitation18.
This study has some limitations. First, there may have been discrepancies between participants’ understanding of the health states and patients’ real-life experiences, despite obtaining clinicians’ and TD patients’ feedback on the videos and written vignettes. Additionally, utility values estimated in this study only captured the impact of moderate-to-severe TD, which is not representative of the full range of possible patient experiences. We decided to focus on moderate-to-severe TD in this study because abnormal movements in individuals with minimal or milder symptoms of TD may be more variable and less reliable in affecting patient awareness, which could hinder detection of a signal in our analysis. However, future follow-up studies could extend our observations regarding the impact of various levels of TD severity on utility values. Similarly, only the common symptoms of mild-to-moderate schizophrenia, bipolar disorder, and MDD were included in the videos and vignettes and may not represent the full spectrum of symptoms experienced by patients with these conditions. Therefore, utility values could vary if specific disease symptoms and severity were evaluated. Finally, as with all TTO analyses, participants’ assessment of the value of future years of healthy life does not always match the value of current years of healthy life, which impacts individuals’ willingness to accept the life decrement.
Conclusions
In this survey-based study of participants representative of the general population, TD utility decrements were slightly larger than those previously reported, potentially due to the incorporation of QOL and social consequences in TD health state descriptions. These findings underscore the value of incorporating factors that affect QOL into utility assessments. Moreover, the utility values reported in this study can be leveraged to improve cost-effectiveness analyses used by decision makers to assess the value of treatments for patients with TD.
Transparency
Declaration of funding
This study was funded by Teva Pharmaceutical Industries Ltd., Tel Aviv, Israel.
Declaration of financial/other relationships
RA, DG, and MZ are employees of Analysis Group, Inc. RR and SL are employees of Teva Pharmaceuticals. SNC has been a consultant for Teva, Neurocrine, Osmotica Pharmaceuticals, and DisperSol Technologies, and has received research grants from Neurocrine, Osmotica Pharmaceuticals, and Eagle Pharmaceuticals. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
RA, DG, and MZ contributed to the conception and design of the analysis, the analysis and interpretation of the data, and the drafting of the manuscript. RR and SL contributed to the conception and design of the analysis, the interpretation of the data, and the drafting of the manuscript. SNC contributed to the interpretation of the data and the drafting of the manuscript. All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Previous presentations
These data were previously presented, in part, at the 20th World Psychiatric Association (WPA) World Congress of Psychiatry Virtual Congress, which was held from 10–13 March 2021, and at the Academy of Managed Care Pharmacy (AMCP) Virtual National Meeting, which was held from 12–16 April 2021.
Ayyagari_supplemental_material.docx
Download MS Word (1.1 MB)Acknowledgements
We thank Caryn Gordon, PharmD (Cello Health Communications/MedErgy with funding from Teva Pharmaceuticals) for editorial assistance in the preparation of this manuscript.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Diagnostic and statistical manual of mental disorders (DSM-5®). Washington (DC): American Psychiatric Association; 2013 [cited 8 October 2021]. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm.
- Global Burden of Disease Study Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800.
- Buchanan RW, Kreyenbuhl J, Kelly DL, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. FOC. 2012;10(2):194–216.
- Vieta E. The role of long acting antipsychotics in bipolar disorder. Eur Psychiatr. 2017;41(S1):S15.
- Wang P, Si T. Use of antipsychotics in the treatment of depressive disorders. Shanghai Arch Psychiatry. 2013;25(3):134–140.
- Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334–1349.
- Cornett EM, Novitch M, Kaye AD, et al. Medication-induced tardive dyskinesia: a review and update. Ochsner J. 2017;17(2):162–174.
- Savitt D, Jankovic J. Tardive syndromes. J Neurol Sci. 2018;389:35–42.
- McEvoy J, Gandhi SK, Rizio AA, et al. Effect of tardive dyskinesia on quality of life in patients with bipolar disorder, major depressive disorder, and schizophrenia. Qual Life Res. 2019;28(12):3303–3312.
- Caroff SN, Yeomans K, Lenderking WR, et al. RE-KINECT: a prospective study of the presence and healthcare burden of tardive dyskinesia in clinical practice settings. J Clin Psychopharmacol. 2020;40(3):259–268.
- Strassnig M, Rosenfeld A, Harvey PD. Tardive dyskinesia: motor system impairments, cognition and everyday functioning. CNS Spectr. 2018;23(6):370–377.
- Wu JQ, Chen DC, Xiu MH, et al. Tardive dyskinesia is associated with greater cognitive impairment in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;46:71–77.
- Keepers GA, Fochtmann LJ, Anzia JM, et al. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. Washington (DC): American Psychiatric Association; 2021.
- Factor SA. Management of tardive syndrome: medications and surgical treatments. Neurotherapeutics. 2020;17(4):1694–1712.
- Lenert L, Morss S, Goldstein MK, et al. Measurement of the validity of utility elicitations performed by computerized interview. Med Care. 1997;35(9):915–920.
- Revicki DA, Hanlon J, Martin S, et al. Patient-based utilities for bipolar disorder-related health states. J Affect Disord. 2005;87(2–3):203–210.
- Lenert LA, Sturley AP, Rapaport MH, et al. Public preferences for health states with schizophrenia and a mapping function to estimate utilities from positive and negative symptom scale scores. Schizophr Res. 2004;71(1):155–165.
- Bleichrodt H. A new explanation for the difference between time trade-off utilities and standard gamble utilities. Health Econ. 2002;11(5):447–456.
- van Osch SM, Wakker PP, van den Hout WB, et al. Correcting biases in standard gamble and time tradeoff utilities. Med Decis Making. 2004;24(5):511–517.
- Wright DR, Wittenberg E, Swan JS, et al. Methods for measuring temporary health states for cost-utility analyses. Pharmacoeconomics. 2009;27(9):713–723.
- Bleichrodt H, Johannesson M. Standard gamble, time trade-off and rating scale: experimental results on the ranking properties of QALYs. J Health Econ. 1997;16(2):155–175.
- Morss SE, Lenert LA, Faustman WO. The side effects of antipsychotic drugs and patients’ quality of life: patient education and preference assessment with computers and multimedia. Proc Annu Symp Comput Appl Med Care. 1993;17–21.
