Abstract
Objective
To investigate the effectiveness of pericapsular soft tissue and realignment (PSTR) exercises for patients with osteoarthritis (OA) of the hip and Harris Hip Score (HHS) below 60 points. Most previous studies of hip exercise have not been applied for patients with moderate to severe hip OA, especially those with an HHS below 60 points. Most studies of hip exercise in OA have involved muscle strength training, stretching, functional training and aerobic fitness programs, and have not included pelvic realignment exercise. We investigated the effect of pelvic realignment exercise for patients with hip OA and HHS below 60 points.
Methods
Design: multicenter, prospective, observational, single-arm study. Setting: clinical examination on an outpatient basis. Participants: 193 patients with hip OA and HHS below 60 points. Interventions: patient education and supervised PSTR exercises. Outcome measures: primary outcome: HHS; secondary outcomes: changes in numerical rating scale (NRS) scores, abduction of range of motion, Timed Up and Go (TUG) test within 30 min after PSTR exercises at baseline and other six items, full analysis set (FAS, all participants who performed PSTR exercises) and subgroup analysis (participants with minimal joint space (MJS) of 0 mm at baseline).
Results
FAS analysis (N = 193): significant differences in HHS were found between baseline and 3 month follow-up, and between baseline and 6 month follow-up in the Unilateral and Bilateral OA groups (p < .001). All mean differences were within the 95% confidence interval. Significant improvement in NRS scores, abduction of range of motion, and TUG test within 30 min after PSTR exercises were found at baseline (p < .001). Subgroup analysis (N = 130): the results revealed significant differences (p < .001) in HHS and NRS, abduction of range of motion and TUG test within 30 min after PSTR exercises at baseline, as in the FAS analysis.
Conclusion
Our findings suggested that PSTR exercises were effective for patients with HHS below 60 points, even those with MJS of 0 mm.
Clinical Trials Registry
20 July 2017 (UMIN000028277)
Introduction
Safiri et al.Citation1 reported that there were more than 300 million cases of hip and knee osteoarthritis (OA) worldwide in 2017, representing an increase in prevalence of approximately 10% since 1990. Early diagnosis and treatment of OA together with improvement of healthcare infrastructure are required to manage the increasing number of patients with OA. Although exercise therapy is reported to be beneficial for alleviating pain and improving function in lower limb OA, evidence for this notion has come primarily from studies of knee OACitation2,Citation3.
In hip OA, exercise interventions have shown promising results, but there is currently a need for high-quality clinical studiesCitation3. Most previous studies on the use of exercise to alleviate hip OA have included participants with mild to moderate hip OACitation3–8. However, exercise is not typically applied for patients with moderate to severe hip OA, especially those with a Harris Hip Score (HHS) below 60 pointsCitation9. The HHS was developed to assess the results of hip surgery, and is used to evaluate various hip disabilities and methods of treatment in adult populations. This physician-completed instrument comprises subscales for pain severity (one item, 0–44 points), function (seven items, 0–47 points), absence of deformity (one item, 0–4 points) and range of motion (two items, 0–5 points). Scores range from 0 (worse disability) to 100 (less disability).
Total hip arthroplasty is typically recommended for patients with an HHS below 60 pointsCitation4,Citation7. Most studies that have examined exercise as a non-surgical treatment for hip OA have involved muscle strength training, stretching, functional training and aerobic fitness programs, according to a Cochrane reviewCitation3. Previous studies reported that exercise produced no improvement of symptoms and function in patients with an HHS below 60 pointsCitation3–8. In addition, because long-term postponement of surgery or avoidance of surgery requires continuous treatment, and manual therapies that require frequent hospital visits are not suitable for long-term treatments, the development of self-care methods through home exercises that are feasible without leaving the workplace may have valuable implications.
Recently, Dahlberg et al.Citation10 reported the effects of a digital self-management program after 24 or 48 weeks of treatment, revealing an improvement in pain measured using a numerical rating scale (NRS) for patients with severe hip OA. The NRS is a segmented numeric version of the visual analog scale in which a respondent selects a whole number (0 to 10 integers) that best reflects the intensity of their painCitation11. The development of a self-management program using digital tools may have useful applications. In the field of orthopedics, surgeons typically pay attention to the relationship between cartilage loss and pain to identify accurate surgical indications. Investigations of this problem initially focused on joint space loss on radiography findingsCitation12,Citation13. Interestingly, recent studies have examined whether cartilage loss causes pain in osteoarthritisCitation14 and whether sprifermin (an agonist of fibroblast growth factor-18) has relevant effectsCitation15. These studies investigated the relationship between cartilage loss and worsening pain in a longitudinal study of knee OA. To the best of our knowledge, no previous studies have examined the relationship between cartilage loss and worsening pain in longitudinal studies of hip OA. The current study was conducted to investigate this issue. In addition, we propose that radiographic findings should be evaluated at each follow-up point to clarify the relationship between cartilage loss and worsening pain.
To conduct a clinical trial examining this issue in patients with severe hip OA, it is important for patients to experience an improvement from baseline at an early stage. In addition, we propose that improvement at baseline is important for encouraging patients with severe hip pain to avoid or postpone surgery. Between 1998 and 2006, we treated patients with hip OA by engaging them in stretching and open kinetic chain exercise to strengthen the hip abductor of the gluteus medius. However, in patients with an HHS below 60 points, performing these exercises did not improve symptoms or function. These findings were similar to the results reported by Bennell et al.Citation5. Therefore, we adopted an alternative exercise, which was developed in Shiatsu practice in Japan (Supplementary Appendix 1). We observed that some patients with severe hip OA exhibited improvement of symptoms at an early stage after performing this alternative exercise. We started using this exercise as a pericapsular soft tissue and realignment (PSTR) exercise (Supplementary Appendix 2) in 2007 and have performed this exercise between 2007 and 2010. We found that pelvic realignment exercises were not included in a previous Cochrane review of studiesCitation3. We confirmed the effects of this exercise for patients with hip OA in a retrospective study of 1077 cases from 2011 to 2014Citation16. The results revealed that many patients with severe hip OA experienced an improvement, such as pain at baseline, and pelvic realignment exercise was most effective for this improvement because it reduced walking instability most effectively. The pelvic realignment exercises were not included, even in a digital self-management program reported by Dahlberg et al.Citation10.
In the current study, we report the results of a multicenter, prospective, single-arm study involving PSTR exercises for patients with an HHS below 60 points. We measured changes in various outcome measures, such as HHS, NRS, Kellgren–Lawrence (K/L) grade, which is a common method for classifying the severity of osteoarthritis using five gradesCitation17, and minimal joint space (MJS), which is the joint space width at the narrowest point on plain radiographs for the assessment of severity of OA. The main objective of this study was to conduct prospective observation. The results revealed that the mean HHS change from baseline increased with PSTR exercise, even for patients with an HHS below 60 points. We collected basic data regarding the extent of improvement in HHS with PSTR exercise. As a secondary objective, we investigated the relationship between cartilage loss and worsening pain.
Methods
Study design
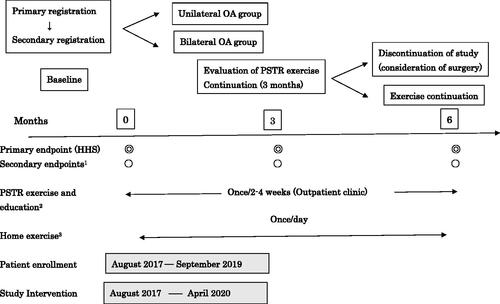
We designed a multicenter, prospective, single-arm study of PSTR exerciseCitation18. Patients who had radiographic hip OA (standing radiography) and provided written informed consent were selected at primary registration. Patients with an HHS below 60 points and without diseases other than OA on magnetic resonance imaging (MRI) scans were selected at secondary registration after primary registration. Outcomes were assessed at baseline, 3 months and 6 months because we observed no major changes in symptoms or function between 6 month and 1 year follow-up in our previous studiesCitation16,Citation19. At each follow-up, the assessments were scheduled within 1 month of the planned follow-up date because many patients visited hospitals from distant areas. Patients underwent instruction and supervision by physical therapists (PTs) once every 2 to 4 weeks and exercised at home as part of their daily routine from baseline to 6 month follow-up. Patient enrollment was conducted between August 2017 and September 2019, and the study intervention was conducted between August 2017 and April 2020 ().
Figure 1. Study design. 1SF-36v2, NRS, ROM, open angles of the hip, maximum hip abduction muscle strength, TUG test, one-leg standing time with eyes open, K/L grade, MJS. Proportion of participants who continued PSTR exercises for 3 months. Proportion of participants who continued PSTR exercises for 6 months. Proportion of participants who exhibited an improvement in HHS of more than 10 points. 2PSTR exercise performance was recorded on the medical chart at each visit in addition to baseline, 3 month follow-up and 6 month follow-up. 3Participants performed the PSTR exercises daily at home and visited outpatient clinics on the scheduled dates.
The study was carried out in accordance with the Declaration of Helsinki and was approved by the Fukuoka Wajiro Hospital and Asama General Hospital Ethics Committees. The trial was registered in the University hospital Medical Information Network (UMIN) Clinical Trials Registry on 20 July 2017 (UMIN000028277)Citation18. The authors were contacted once every 6 months by the UMIN Center until the study was completed. Written informed consent was obtained from participants before primary registration. The patients were observed by two hospitals and the inclusion screening was performed at the Arthritis Center of Fukuoka Wajiro Hospital in Fukuoka, Japan (Study Center 1) and the Department of Orthopaedic Surgery of Asama General Hospital (Study Center 2) in Nagano, Japan. One orthopedic surgeon examined all radiographs at each study center.
The patient’s symptoms were evaluated and rated by five PTs at Study Center 1 and by four PTs at Study Center 2. Information about patients’ characteristics was collected by three nurses and one medical clerk at Study Center 1, and by one nurse at Study Center 2. Data collection was performed using an electronic data capture system.
Participants
No special recruitment methods (e.g. newspaper advertising) were undertaken for this study. The rationale for participant selection is presented in Supplementary Appendix 3.
Inclusion criteria at primary registration
Patients meeting all of the following criteria were considered to be eligible:
Patients who wished to avoid surgery.
Patients aged 18–85 years at the time of granting consent.
Patients who experienced hip pain for more than 3 months.
Patients meeting at least two of the following items 1–3 (American College of Rheumatology criteriaCitation20) or item 4 on radiography:
1. ESR < 20 mm/ha.
2. Osteophytes (femoral or acetabular).
3. Joint space narrowing.
4. Hip pain due to acetabular dysplasia.
a. Patients who did not meet item 4 of criterion 4) and met only one of items 2 or 3 required further confirmation.
5. Patients for whom the difference in the height of the tip of the greater trochanter was below 2.0 cm on standing full-length radiographs of the lower extremities.
6. Patients who provided written consent for participation in this study.
Exclusion criteria at primary registration
Patients meeting any of the following criteria were excluded:
Patients who had undergone treatment for cardiovascular disease.
Patients who had undergone treatment for cancer.
Patients with severe osteoporosis/dysfunction in the lower extremities caused by an accident or disease besides OA of the hip (e.g. young adult mean bone mineral density below 50%), or OA in the knee above K/L grade 2.
Patients who were pregnant.
Patients who had undergone any kind of surgery of the lower extremities.
Patients who had undergone instruction regarding PSTR exercises by therapists within 1 year (patients who performed exercises by themselves according to instructions published elsewhere were not excluded).
Patients with dementia who appeared to be ineligible for exercise treatment (on the basis of a doctor’s judgment, e.g. patients who had difficulty keeping a diary or understanding the exercises).
Other patients that the attending physician considered to be ineligible.
Inclusion criteria at secondary registration
Participants meeting the following criterion were considered to be eligible:
Patients with an HHS below 60 points.
Exclusion criteria at secondary registration, in MRI findings
Participants meeting any of the following criteria were excluded:
Patients with osteonecrosis of the femoral head.
Patients with a subchondral insufficiency fracture of the femoral head.
Patients with Perthes disease.
Patients with rheumatoid arthritis.
Patients with infection.
Patients in whom malignant diseases were suspected at the hip joints or around the hip.
Treatments
The interventions were developed at two hospitals. The patient education and PSTR exercise methodologies were reported previouslyCitation16. A reference hyperlink for a video demonstration of PSTR exercises is provided in Supplementary Appendix 2.
Orthopedic surgeons instructed the patients to perform PSTR exercises after secondary registration until 6 month follow-up. Patients were instructed by PTs once every 2 to 4 weeks at visiting hospitals, and performed the exercises at home once a day (). The following treatments were prohibited in combination with PSTR exercises during this study:
Change in the type or increase of the dosage of analgesics.
Chiropractic care or other hip joint exercise therapy.
Surgery.
Outcome measures
The primary outcome measure was change in HHS, and the secondary outcomes were NRS scores, range of motion (ROM), opening angle of the hip, maximum strength of hip abductors, Timed Up and Go (TUG) test (in which the patient is observed and timed while they rise from an arm chair, walk 3 meters, turn, walk back and sit down again)Citation21, the one-leg standing time with eyes open (OLSTEO; a common screening test of balance in which the ability to stand on one leg for as long as possible is measured), the Short-Form 36-Item Health Survey version 2 (SF-36v2; a set of generic, coherent and easily administered quality-of-life measures)Citation22–24, K/L grade, MJS, the proportion of participants who continued PSTR exercises for 3 months and 6 months, and the proportion of participants in whom HHS improved by more than 10 points. All outcomes were assessed at baseline (before PSTR exercises), 3 months, and 6 months. In addition to these time points, NRS, ROM (only abduction), and the TUG test were evaluated within 30 min after PSTR exercises at baseline to explore early predictive markers of the effects of PSTR exercise.
PT staff at Study Centers 1 and 2 established an evaluation method of HHS pain score using NRS as modified HHS (Supplementary Appendix 4) because the use of the previous HHS pain scoring system sometimes resulted in a 10 point difference between PT staff members for the same patients, which was caused by the ambiguous expression of pain characteristics. Four orthopedic surgeons and one radiologist (Study Center 1: two orthopedic surgeons and one radiologist; Study Center 2: two orthopedic surgeons) established a modified K/L grade of radiography (Supplementary Appendix 5), in which attempts were made to minimize variation in the evaluation methods. PTs at the two hospitals attended two group meetings and held several discussions via email to unify the exercise techniques and the method of measurement of ROM, the opening angle of the hip (according to a modified Patrick’s test)Citation16, maximum strength of hip abductors using a hand-held dynamometer, TUG test and OLSTEO before the initiation of this study.
Participants were classified into two groups: a Unilateral OA group (no pain [HHS pain score of 44 points] in the opposite hip) and a Bilateral OA group (pain in both hips, HHS pain score below 40 points, bilaterally). In the Bilateral OA group, the side of the hip targeted for analysis was selected as follows:
Decision criteria for the evaluation target side
The hip with the lowest HHS Pain Score.
When the HHS Pain Score was the same in both hips, the hip with the lowest HHS (Total Score) was selected.
When the HHS Pain Score and Total Score were the same, the hip with the smallest abduction angles was selected.
When the HHS Pain Score, Total Score and abduction angles were the same, the hip with the smallest open angle of the hip was selected.
Cases in which symptoms worsened. HHS decreased by more than 20 points compared with that at baseline.
Cases in which the patient requested surgery.
Cases in which the patient requested the discontinuation of PSTR exercises.
Cases in which the patient died during the study.
Others: cases in which the treatment was changed because the participant had become ineligible for the study for other reasons (e.g. breaking a rule of the protocol).
Statistical analyses
The main purpose of this study was basic data collection to determine the effects of PSTR exercises. This study was not conducted as a confirmatory study with a threshold. Therefore, the sample size of this study was set as the number of patients that was possible to recruit within the enrollment period. Differences in the background parameters between the Unilateral and Bilateral OA groups were analyzed using t-tests for continuous variables and chi-square tests for discrete variables. A paired t-test or a McNemar test was used to evaluate the change from baseline at 3 and 6 months in each endpoint. In addition to the main analysis for the full analysis set (FAS; all eligible patients who performed PSTR exercises), subgroup analysis was conducted for patients with MJS of 0 mm. Furthermore, an analysis of the per protocol set (PPS; patients who completed 6 months of PSTR exercises) was implemented. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). A value of p < .05 was considered to indicate statistical significance.
Results
Characteristics of the patients
In total, 657 patients with hip pain visited Fukuoka Wajiro Hospital and Asama General Hospital from August 2017 to September 2019, of whom 414 patients were enrolled in the primary registration and 196 patients with an HHS <60 points were eligible at the secondary registration. Three patients were excluded (two patients: withdrawal of consent, one patient: unfitness), and a final sample of 193 patients was analyzed; 47 patients discontinued the study, and at least 31 of these patients requested surgery ( and ). The proportion of participants who received a recommendation for surgery at another hospital before the first visit was 98.9% in the Unilateral OA group and 96.1% in the Bilateral OA group ().
Figure 2. Study flow diagram. Abbreviation. FAS, Full analysis set. Numbers in parentheses indicate the numbers of participants included in the statistical analysis (number of participants evaluated within 1 month on the planned date). (A) Cases in which the patient requested surgery. (B) Cases in which the patient requested the discontinuation of PSTR exercises. (C) Cases in which the treatment was changed because the patient was not eligible for the study (e.g. breaking the protocol). (D) Cases in which symptoms worsened. HHS decreased by more than 20 points compared with that at baseline. Study Center 1: Fukuoka Wajiro Hospital; Study Center 2: Asama General Hospital.
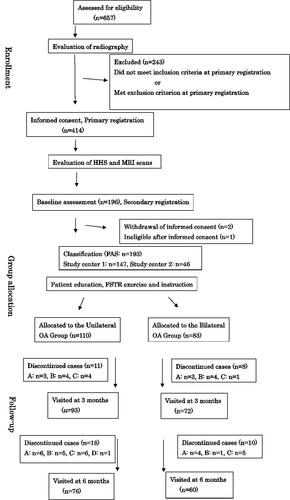
Table 1. Baseline characteristics.
FAS analysis (all participants, 193 patients)
Primary outcome
Significant differences in HHS were noted both between baseline and 3 month follow-up, and between baseline and 6 month follow-up in the Unilateral and Bilateral OA groups (p < .001 for all items; baseline–3 months: the Unilateral OA group, mean difference 16.4, 95% CI 13.3–19.5; the Bilateral OA group, mean difference 13.3, 95% CI 10.1–16.5; baseline–6 months: the Unilateral OA group, mean difference 19.6, 95% CI 15.8–23.4; the Bilateral OA group, mean difference 19.5, 95% CI 15.8–23.2) ().
Table 2. Difference in the HHS as primary outcome and other secondary outcomes at baseline, and follow-up at 3 months and 6 months.
Secondary outcomes
SF-36v2, NRS, abduction of ROM, opening angle of the hip, maximum strength of the hip abductor, TUG test and OLSTEO showed significant improvement at one or both time points (between baseline and 3 months and/or baseline and 6 months; ). MJS in the Unilateral OA group showed significant impairment, whereas HHS and other secondary outcomes significantly improved ().
Table 3. Difference in ROM at baseline and follow-up at 3 months and 6 months.
Table 4. Difference in SF-36 scores at baseline and follow-up at 3 months and 6 months (NBS [norm-based scoring]).
The proportions of participants who continued PSTR exercises for 3 months were 77.3% in the Unilateral OA group and 85.5% in the Bilateral OA group. The proportions of participants who performed PSTR exercises for 6 months were 73.6% in the Unilateral OA group and 78.3% in the Bilateral OA group. The proportions of participants exhibiting an improvement in HHS of more than 10 points were 54.5% at 3 month follow-up and 53.6% at 6 month follow-up in the Unilateral OA group; and 54.2% at 3 month follow-up and 54.2% at 6 month follow-up in the Bilateral OA group.
Subgroup analysis (participants with MJS of 0 mm, 130 patients)
Primary outcome
Significant differences in HHS were found, as in the FAS analysis (p < .001 in all items; baseline–3 months: the Unilateral OA group, mean difference 13.0, 95% CI 9.2–16.8; the Bilateral OA group, mean difference 10.3, 95% CI 6.7–14.0; baseline–6 months: the Unilateral OA group, mean difference 16.3, 95% CI 11.6–21.1; the Bilateral OA group, mean difference 13.4, 95% CI 9.9–16.8) ().
Secondary outcomes
SF-36v2, NRS, abduction of ROM, opening angle of the hip, maximum strength of hip abductor, TUG test and OLSTEO showed significant improvements at one or both time points (between baseline and 3 months and/or baseline and 6 months) as in the FAS analysis (). K/L grade showed no significant changes ().
The proportions of participants who continued PSTR exercises for 3 months and 6 months were 72.2% and 68.1% in the Unilateral OA group, and 84.5% and 72.4% in the Bilateral OA group, respectively. The proportions of participants in whom HHS improved by 10 points or more were 45.8% at 3 months and 45.8% at 6 months follow-up in the Unilateral OA group, and 48.3% at 3 months and 44.8% at 6 months follow-up in the Bilateral OA group.
Changes in NRS, abduction of ROM, TUG test within 30 min after PSTR exercises at baseline
FAS and subgroup analysis revealed significant improvement in NRS, abduction of ROM and TUG test within 30 min after PSTR exercises in the Unilateral and Bilateral OA groups at baseline (p < .001 in all items) ().
Table 5. Changes of NRS, abduction of ROM, TUG test within 30 min after PSTR exercises at baseline.
Exploratory analysis
A significant difference was found between Study Centers 1 and 2 in HHS change at 6 months from baseline. However, significant improvements were observed at 3 and 6 months from baseline, respectively, at each study center ().
Table 6. Differences in baseline characteristics between Study Center 1 and Study Center 2.
Discussion
The results of the current study suggested that the PSTR exercises were effective for patients with hip OA and an HHS below 60 points, even those with MJS of 0 mm.
In previous studiesCitation16,Citation19, almost all cases with improved activities of daily living showed an HHS change from baseline of more than 10 points and an HHS Pain Score change of more than 10 points. In contrast, almost all cases with poor results showed no change in HHS Pain Score. Therefore, we evaluated the proportion of participants in whom HHS improved by more than 10 points according to HHS Pain Score grading, because the main symptom associated with OA is painCitation9. A mean HHS change of 10–20 points from baseline was found at 3 months and 6 months in an analysis of FAS (all participants, N = 193 patients) and subgroup analysis (participants with MJS of 0 mm, N = 130 patients). In addition, an analysis of PPS (N = 132) produced similar results. A significant change in HHS of more than 10 points was found at all time points. The proportion of participants in whom HHS improved by more than 10 points was approximately 50% at 3 month and 6 month follow-up in the FAS and subgroup analyses. The proportions of participants who received a recommendation of surgery at another hospital before their first visit to our clinic were 98.9% in the Unilateral OA group and 96.1% in the Bilateral OA group at baseline. This finding suggests that hospitals other than Study Centers 1 and 2 typically perform surgery for almost all patients with severe hip OA. All patients with severe hip OA were told by doctors at the hospitals they visited before their first visit to our clinic that the exposed subchondral bone secondary to loss of cartilage from the joint surface was contacted, causing hip pain that can be relieved only by surgery. The finding that 50% of patients who planned to undergo surgery exhibited an HHS change of more than 10 points provides valuable clinical information. In addition, some patients exhibited an improvement of HHS of more than 20–30 points compared with HHS at baseline, despite being recommended surgery. These findings may be useful for informing future studies investigating this issue.
Among the patients, 47 discontinued the study. Of these, 31 patients requested surgery (dropout rate: 24.6%). In this study, we investigated all cases with an HHS below 60 points, including cases of dropout because of surgery. All patients who took part in this study were considered to have an indication for surgery at another hospital, and wished to prevent or postpone surgery. We considered that most patients who underwent surgery later were not indicated for PSTR exercise at their first visit. In addition, patients that we considered to have an indication for surgery were also included in the group of patients with poor results. In a future study, we plan to investigate the distinctions between the cases indicated for surgery and the cases in which PSTR exercises are effective at baseline. In addition, it will be necessary to investigate the true effect of PSTR exercise for cases with appropriate indications.
It is unclear why a significant difference in HHS change was observed between Study Centers 1 and 2. However, PSTR exercises showed a significant effect at both study centers. This difference should be investigated in future studies. Study Center 1 is located in an urban area and Study Center 2 is located in a rural area. Results from urban and rural study centers should be analyzed separately in the future.
NRS, abduction of ROM and TUG test performance showed significant improvement within 30 min after PSTR exercises in the Unilateral and Bilateral OA groups at baseline, even in patients with loss of cartilage. This evaluation may be useful for examining the effects of early predictive markers of PSTR exercises. In addition, these results indicate that patients with severe hip OA may obtain an improvement of symptoms from baseline at the early stage. PSTR exercises appear to be suitable for investigating the relationship between cartilage loss and worsening pain in patients with severe hip OA, and may encourage patients with severe hip OA to avoid or postpone surgery.
MJS in the Unilateral OA group revealed significant impairment, but HHS and other secondary outcomes significantly improved with PSTR exercises. These results suggest that cartilage loss might not affect pain directly. We have observed cases in which joint space is preserved at baseline, then cartilage disappears completely over time, but symptoms are improved with PSTR exercise (Supplementary Appendix 6).
The current study suggested that pelvic realignment exercises were effective for patients with an HHS below 60 points, even among those with MJS of 0 mm. Therefore, realignment of the pelvis and lower extremities might be more effective than muscle strength training for patients with severe hip OA. In addition, this finding appears to explain why many patients with severe hip OA complain of pain in areas other than the affected hip, such as the foot, ankle, calf, knee, thigh, and low back. We plan to investigate the complex pain-related mechanisms of hip OA by analyzing the alignment of the pelvis and lower extremities in future studies.
Strength and limitations
To the best of our knowledge, this study is the first to report that exercise is effective for patients with hip OA and an HHS below 60 points who wish to postpone or avoid surgery for a prolonged period. Exercises such as muscle strength training, stretching, functional training and aerobic fitness programs have not previously been found to have significant effects for patients with moderate to severe hip OA, particularly those with an HHS below 60 pointsCitation3–8. Pelvic realignment exercises of PSTR exercise provide a new strategy. However, the current study was a single arm observational study conducted at only two study centers. To confirm the current findings, there is a need for further studies, such as randomized controlled trials.
We plan to investigate the effects of functional orthoticsCitation25 for patients with hip OA, and to evaluate the improvement of walking instability. Functional orthotics have a structure that is designed to correct the malalignment of the lower extremities and low back in hip OA. Other orthotics and insoles do not have such a structural design. We plan to investigate effective combinations of PSTR exercises and functional orthotics in future. In addition, we plan to investigate the most effective factors in the improvement of pain and function in patients with severe hip OA, and to compare realignment treatment with muscle strength training.
Conclusions
This study suggested that PSTR exercises were effective in patients with an HHS below 60 points, even those with MJS of 0 mm.
Pelvic realignment exercise may improve pain and function in severe hip OA.
Comparison with other studies
According to the most recent Cochrane reviewCitation3, previous studies of hip OA patients have generally involved land-based exercise programs consisting of traditional muscle strength training, functional training or aerobic fitness programs, except for one study in which participants were enrolled in a tai chi programCitation26. To the best of our knowledge, the current study is the first to investigate the effectiveness of a pelvic realignment exercise for anterior pelvic tilt to improve function in patients with hip OACitation27.
Transparency
Declaration of funding
This study did not receive funding.
Declaration of financial/other relationships
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. CMRO peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Some of the results of this study were presented as an abstract and poster at the 2021 OARSI World Congress; 28 April–1 May 2021.
Author contributions
K.H. and T.T. contributed to study design, collection, analysis and interpretation of data, and drafting and revising of the manuscript. T.S. contributed to analysis and interpretation of data, use of statistics and critical revision of the manuscript. Y.T. and F.I. contributed to the explanations of PSTR exercises, writing the Discussion and analysis of patient characteristics at baseline (). All authors approved the final version of the manuscript.
Ethics statement
The study was carried out in accordance with the Declaration of Helsinki and was approved by the Fukuoka Wajiro Hospital and Asama General Hospital medical research ethics committees.
Supplemental Material
Download MS Word (52.7 KB)Supplemental Material
Download MS Word (53.2 KB)Acknowledgements
K.H. and T.T. acknowledge the support of K. Toyota, S. Tokunaga, S. Soda, S. Aritake and S. Sakamoto (staff at the Clinical Research Support Center Kyushu). We wish to thank the staff at the Department of Rehabilitation of Fukuoka Wajiro Hospital and Asama General Hospital for their contributions to instruction for PSTR exercises. We are grateful for the support provided by the nurses and medical clerks of Fukuoka Wajiro Hospital and Asama General Hospital. The authors wish to thank all of the patients who participated in this study. We thank Benjamin Knight MSc from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
References
- Safiri S, Kolahi A-A, Smith E, et al. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the Global Burden of Disease Study 2017. Ann Rheum Dis. 2020;79(6):819–828.
- Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1:CD004376.
- Fransen M, McConnell S, Hernandez-Molina G, et al. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;22:CD007912.
- Fernandes L, Storheim K, Sandvik L, et al. Efficacy of patient education and supervised exercise vs patient education alone in patients with hip osteoarthritis: a single blind randomized clinical trial. Osteoarthritis Cartilage. 2010;18(10):1237–1243.
- Bennell KL, Egerton T, Martin J, et al. Effect of physical therapy on pain and function in patients with hip osteoarthritis: a randomized clinical trial. JAMA. 2014;311(19):1987–1997.
- White DM, Cibulka MT, Woehrle J. Physical therapy and hip osteoarthritis. JAMA. 2014;312(12):1257–1258.
- Svege I, Nordsletten L, Fernandes L, et al. Exercise therapy may postpone total hip replacement surgery in patients with hip osteoarthritis: a long-term follow-up of a randomised trial. Ann Rheum Dis. 2015;74(1):164–169.
- Thompson AR, Christopherson Z, Marshall LM, et al. A pilot randomized controlled trial for aerobic and strengthening exercises on physical function and pain for hip osteoarthritis. PM R. 2020;12(3):229–237.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755.
- Dahlberg LE, Dell’Isola A, Lohmander LS, et al. Improving osteoarthritis care by digital means – effects of a digital self-management program after 24- or 48-weeks of treatment. PLoS One. 2020;15(3):e0229783.
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804.
- Kim C, Nevitt MC, Niu J, et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ. 2015;351:h5983–8 h5983.
- Iidaka T, Muraki S, Akune T, et al. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthritis Cartilage. 2016;24(1):117–123.
- Bacon K, Lavalley MP, Jafarzadeh SR, et al. Does cartilage loss cause pain in osteoarthritis and if so, how much? Ann Rheum Dis. 2020;79(8):1105–1110.
- Hochberg MC, Guermazi A, Guehring H, et al. Effect of intra-articular sprifermin vs placebo on femorotibial joint cartilage thickness in patients with osteoarthritis: the FORWARD randomized clinical trial. JAMA. 2019;322(14):1360–1370.
- Hayashi K, Tokunaga S, Haruguchi K, et al. Dramatic effects of new home exercises for patients with osteoarthritis of the hip: pericapsular soft tissue and realignment exercises. J Physiother Phys Rehabil. 2018;3:162–173. Supplementary Information.
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502.
- Hayashi K. Investigation regarding effects of PSTR (pericapsular soft tissue and realignment) exercises to improve function in patients with osteoarthritis of the hip and a Harris Hip Score (HHS) below 60 points. Tokyo: University hospital Medical information Network; 2017.
- Hayashi K. Dramatic effects of a new home exercise to improve hip function for patients with osteoarthritis. Osteoarthr Cartilage. 2015;23:A165–A166.
- Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514.
- Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148.
- Brazier JE, Fukuhara S, Roberts J, et al. Estimating a preference-based index from the Japanese SF-36. J Clin Epidemiol. 2009;62(12):1323–1331.
- Suzukamo Y, Fukuhara S, Green J, et al. Validation testing of a three-component model of short FORM-36 scores. J Clin Epidemiol. 2011;64(3):301–308.
- Fukuhara S, Akizawa T, Morita S, et al. Understanding measurements of vitality in patients with chronic kidney disease: connecting a quality-of-life scale to daily activities. PLoS One. 2012;7(7):e40455.
- Brown DN. Orthotic insert having heel post with contoured lower surface. United States Patent US6,782,643 B2. 2004; Aug 31.
- Bennell KL, Dobson F, Hinman RS. Exercise in osteoarthritis: moving from prescription to adherence. Best Pract Res Clin Rheumatol. 2014;28(1):93–117.
- Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589.
