Abstract
Objective
Blood supply shortages may create unnecessary burden, including treatment delay, worsened quality of life, or increased healthcare resource utilization in patients with myelodysplastic syndromes (MDS). This study examined physicians’ experience with blood supply shortages in the MDS population. Additionally, physicians’ perspectives on the factors that impact clinical, economic, and humanistic outcomes of patients with MDS were investigated.
Methods
A total of 378 physicians primarily specializing in hematology/oncology across the UK, France, Germany, Italy, and Spain completed the survey (n ≈ 75 in each country). Physicians answered questions regarding adequacy of blood supply for patients with MDS who require red blood cell (RBC) transfusions and identified factors impacting the clinical, economic, and humanistic outcomes in the MDS population.
Results
Over 65% of physicians reported that their patients with MDS requiring RBC transfusions encountered RBC transfusion delays due to blood supply shortage. Among physicians who reported delays, 13.8% of patients were impacted, ranging from 11.0% in Spain to 19.4% in Italy. On average, patients experienced a 4.2-day delay in receiving RBC transfusions due to blood supply shortages, and 16.7% of patients required additional healthcare provider visits. Eastern Cooperative Oncology Group performance status, threshold hemoglobin levels, and age were the top factors reported by more than two-thirds of physicians that impact outcomes of patients with MDS.
Conclusion
Our findings support the need for new treatments in MDS that reduce transfusions and thus blood supply needs, and that would have a beneficial effect on clinical, humanistic, and economic outcomes.
Introduction
Myelodysplastic syndromes (MDS) are a group of malignant hematologic diseases characterized by ineffective bone marrow hematopoiesis, peripheral blood cytopenias, and a risk of progression to acute myeloid leukemia (AML)Citation1,Citation2. The incidence of MDS increases markedly with age, with an estimated 20–50 cases per 100,000 per year in those aged ≥60 yearsCitation1. In countries with aging populations, the number of patients with MDS is expected to increase in the coming decades.
The majority of patients with MDS have anemia and require red blood cell (RBC) transfusions. Due to the chronic nature of MDS-associated anemia, many patients develop long-term dependence on RBC transfusions and may incur complications such as iron overloadCitation3. Transfusion dependence (TD) is associated with substantial clinical, health-related quality of life (HRQoL), and economic consequences. TD patients have significantly more hospitalizations and infectious complications and a shorter overall survival than transfusion independent (TI) patientsCitation4,Citation5. The cost of repeated transfusions and more frequent hospitalizations contribute to a higher economic burden, with TD patients incurring double the medical costs of TI patientsCitation6. Moreover, chronic transfusions negatively affect HRQoL to the extent that patients with MDS would consider a treatment that temporarily made them feel worse if it stopped or reduced the need for transfusions or would be willing to trade length of life, in order to achieve TICitation7–9.
One critical factor in MDS treatment is sufficient blood supply, which is essential for the administration of RBC transfusions to patients with MDS. Blood is a limited resource and as donations have a short shelf life, regular donors are essential to secure a constant supply. Most countries struggle to maintain a sufficient blood supply to meet patient needsCitation10, and a shortage of blood supply may create additional burden for patients with MDS by causing treatment delays.
Physicians’ perspectives on the factors that impact outcomes of patients with MDS are not well understood and, to our knowledge, no studies have examined physicians’ experience associated with blood supply shortages and RBC transfusion delays in the MDS population. The current study investigated physicians’ experience associated with shortage of blood supply and RBC transfusion delays in patients with MDS and the physicians’ perspectives on the factors that impact clinical, economic, and humanistic outcomes of patients with MDS.
Methods
Participants
Participating physicians were located in the UK, France, Germany, Italy, and Spain. Physicians were considered eligible for the survey if they had been in practice for 2–35 years, had managed ≥15 patients with MDS in the past 3 months, spent at least 75% of their time in direct patient care, and if their primary medical specialty was in oncology and/or hematology. Participants were required to provide informed consent.
Physicians were recruited through M3, an internal database of >1,000,000 healthcare professionals worldwide, with physician demographics generally representative of the physician population in each of the participating countries. Physicians were paid for their participation. Physician incentive amounts were determined by the M3 panel according to the fair market value in each country for a research interview, considering the length of the interview/survey, the physician specialty/expertise, and the complexity of the interview/survey subject matter. The study protocol was approved with exemption status by Pearl Institutional Review Board (Indianapolis, IN, USA).
Survey design
A multi-phase approach was performed. In phase 1, cognitive interviews were conducted with physicians (n = 3 in each country) in January–February 2020 to pre-test and revise the questionnaire to ensure relevance, understanding, and appropriateness of language and survey content.
Phase 2 consisted of a web-based survey to generate quantitative data, which was conducted in April–May 2020. The survey assessed physician demographics and their experience of blood supply shortages for their patients with MDS requiring RBC transfusions. The survey also assessed physicians’ opinions on the top 10 factors (from a list of 32) that impact the clinical, economic, and humanistic outcomes of all patients with MDS. To quantify the relative importance of each factor, participants were further requested to distribute 100 points across the 10 factors that they had selected to weigh the impact of these factors.
Also, an exploratory analysis examined whether the location of a practice (urban, suburban, or rural) or size of a practice impacted 2 key outcomes: length of transfusion delay and percentage of patients experiencing transfusion delay.
In both phases, physicians took the survey in their native language. The survey was designed in English and was translated into the local language (French, German, Italian, and Spanish) at Global Lexicon (ISO 9001-accredited) by trained native-speaker linguists familiar with health outcomes research and medical terminology, and the translations were checked by Language Insight (ISO 9001-accredited). Once qualified for either phase 1 or 2, participants were provided a unique survey link via email (which included an appropriate introduction to the research and a request for informed consent). The consent statement informed potential respondents that participation was voluntary and that responses would remain confidential. It also included information about the goals of the study, the approximate length of the survey, and incentives for participation. Lastly, the statement of informed consent provided potential respondents with the resources to address any concerns they may have. After reading the statement of informed consent, the respondents had to select the option “I agree to participate” to enter the survey. For those who selected “I do not agree to participate”, study participation was terminated.
Physicians were not aware of the study sponsor and the sponsor was not given any identifying information on the participating physicians. In France, due to French legislation (Loi Bertrand and Loi Anti-Cadeaux) requirements, physicians were informed that Bristol Myers Squibb was the sponsor at the end of the survey; physicians were not able to modify their responses upon seeing this information, so that the data were not biased by the physicians receiving this information.
Statistical analysis
Results were described descriptively in proportions for categorical/ordinal data and mean (with standard error [SE] or 95% confidence interval [CI]) for continuous data. Overall ANOVA (analysis of variance) tests to compare data across countries were conducted. Scheffé’s multiple comparison adjustments were also conducted for outcomes found significant with the overall ANOVA test (alpha level = 0.05).
Results
Physician study population
In total, 378 physicians completed the survey across the included countries (n ≈ 75 in each country); a total of 10 oncologists, 124 hematologists, and 244 hematologist/oncologists participated (). Physician characteristics are presented in (data also under review in another manuscript). On average, physicians were in clinical practice for 14.7 years and reported that they spent 88.7% of their professional time in patient care. Physicians estimated that they had seen an average of 54.5 patients with MDS in the past 3 months and that approximately 47.4% of their patients were TD. Overall, more physicians use the revised International Prognostic Scoring System (IPSS-R) (58.2%) than the IPSS (41.8%).
Figure 1. Survey respondents’ medical specialties. Figure adapted from Gupta et al.Citation11.
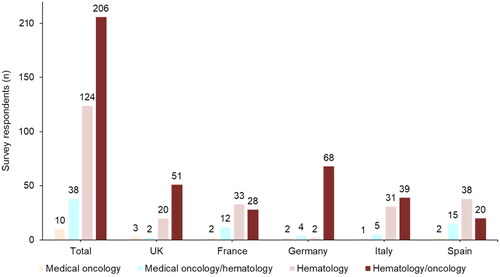
Table 1. Physician characteristics by country.
Overall, 41.3% of participants reported an age between 45 and 54 years, and 64.3% were male. Italy had a greater percentage of physicians aged <35 years (23.7%), while Germany had the highest percentage of physicians aged 55–64 years (21.1%). Italy was the only country to have a majority of female physicians (53.9%) completing the survey ().
In France, Germany, Italy, and Spain, the vast majority of practices were urban (≥89.5%), while in the UK, over a quarter of practices were suburban (26.3%). Germany (3.9%) and Spain (2.7%) were the only countries to report practices in rural areas. While 60.5% of participating physicians in Germany were working in practices with 2–4 oncologists/hematologists, the majority of physicians from other countries were working in relatively larger practices, with >5 oncologists/hematologists ().
Blood supply shortages and the consequences
A total of 65.6% of physicians reported that they had patients with MDS requiring RBC transfusions who encountered RBC transfusion delays due to blood supply shortages. A total of 17.2% reported that these blood shortages affected ≥25% of their patients with MDS, ranging from 9.3% in Spain to 31.6% in Italy (p < .10) (). On average, blood supply shortages impacted 9.0% (95% CI, 7.6–10.4) of all patients with MDS requiring transfusions, with the greatest differences again observed between Spain and Italy (6.6% vs. 14.1%, respectively; p = .025). Among physicians who reported delays (n = 248), 13.8% (95% CI, 11.9–15.7) of patients were impacted, ranging from 11.0% in Spain to 19.4% in Italy. Among the 248 physicians who reported that they had patients with MDS who encountered RBC transfusion delays due to blood supply shortage, the average length of RBC transfusion delay was 4.2 days (95% CI, 3.6–4.8) (), and 16.7% (95% CI, 14.3–19.1) of patients required additional healthcare provider visits (). The average length of RBC transfusion delays was similar between most countries; with the exception of Germany, which had the shortest treatment delays (3.1 days; ). There was notable variation between countries in the percentage of patients needing additional healthcare provider visits, which ranged from 12% in Spain to 19.9% in Italy. No significant difference was found across countries for either outcome ().
Figure 2. Consequences of blood supply shortages, (A) length of treatment delay; (B) percent of patients requiring additional visits to healthcare providers. Numbers to the right of the data bars indicate the mean, and error bars show the upper limit of the 95% CI. Abbreviations. CI, confidence interval; n, number of physicians with observations.
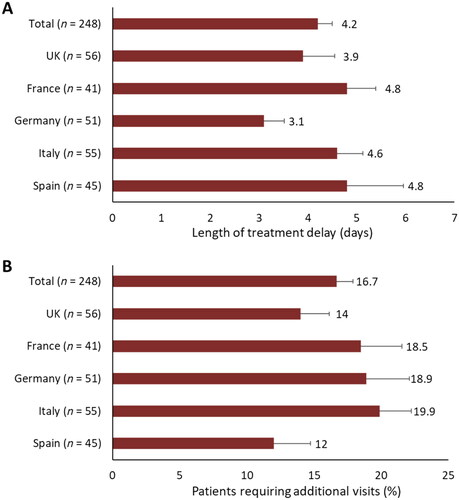
Table 2. Blood supply shortage metrics for patients with MDS requiring RBC transfusions.
Top factors that impact the clinical, economic, and humanistic outcomes of patients with MDS
The top 10 factors selected by physicians based on the number of selections and average weighted scores are presented in (the remaining factors are presented in Table S1, Supplemental File). Overall, Eastern Cooperative Oncology Group performance status (ECOG PS) was most frequently selected as an important factor (74.6%) and given the greatest mean impact score (8.93). After ECOG PS, the most frequently selected factors overall were hemoglobin level (66.7%), patient age (66.7%), infection (61.1%), and the percentage of blasts in bone marrow at diagnosis (60.1%). For each country, one of these factors was identified as the second most frequently selected factor. Further factors which were similarly highly ranked based on mean impact scores included: bone marrow % blasts at diagnosis (8.25), patient age (7.24), and hemoglobin level (6.75), while infection was ranked at 6.08. Other highly ranked factors were the presence of comorbidities/comorbidity index (6.59) and genetic abnormalities (6.40).
Table 3. Top 10 factors and mean impact scores by country.
Within the selected top 10 factors, significant differences in preferences were observed between countries. Physicians in the UK considered the percentage of blasts in peripheral blood at diagnosis more important than physicians in Germany, based on both the number of selections (60.5% vs. 34.2%; p = .030) and mean contribution points (7.63 vs. 3.08; p = .002). In the UK, physicians also gave a significantly higher mean contribution score to genetic abnormalities in comparison to Germany (8.53 vs. 3.84; p = .010). In France, physicians ranked hemoglobin level as a top 10 factor more frequently than in Italy (77.3% vs. 52.6%; p = .034).
Effect of practice location and size on blood supply
The location (urban, suburban, or rural) and size of the practice or setting was found to impact the length of transfusion delay and the percentage of patients experiencing transfusion delay. The average length of delay was higher for physicians practicing in suburban areas versus those who practice in urban areas (5.59 days vs. 4.06 days). The group of physicians practicing in rural areas had the shortest average length of time, but only 3 physicians were in this group, meaning the sample size was too small to make any inferences. Similarly, those practicing in medium-sized practices (5–10 physicians) experienced greater delays than those in larger practices or centers (more than 10 physicians). Here, the average length of delay was 5.78 days and 3.56 days, respectively (Table S2, Supplemental File). The delay times were similar for physicians in smaller practices (2–4 physicians) and those in the larger practices. Regarding the percentage of patients experiencing transfusion delay, there was no discernable pattern.
Discussion
RBC transfusion remains a central component of symptom management and supportive care for most patients with MDS. The dependence of patients with MDS on frequent RBC transfusions can result in substantial clinical and economic consequences, diminished HRQoL, and poorer outcomesCitation4–6. The burden of MDS may be exacerbated by blood supply shortages, which can cause treatment delays and, as a result, increased healthcare resource utilization and worsened HRQoL. The current study examined and quantified physicians’ experience with blood supply shortages and RBC transfusion delays in the MDS patient population. Furthermore, we aimed to understand physicians’ perspectives on the factors that impact clinical, economic, and humanistic outcomes of patients with MDS.
Blood components are a vital commodity in healthcare systems and remain a scarce and precious resource. With the exception of Spain, all countries surveyed in this study were listed among the top 10 countries that accounted for >65% of the global blood supply in a 2011 World Health Organization reportCitation12. Nevertheless, in the present survey study, nearly two-thirds of physicians reported that they had patients with MDS who encountered RBC transfusion delays due to blood supply shortages. Moreover, although Italy has reportedly been self-sufficient in blood supplies since 2010Citation13, nearly a third of physicians in Italy in the present study reported that ≥25% of their patients with MDS experienced transfusion delays due to blood supply shortages. Overall, physicians estimated that blood shortages resulted in an average transfusion delay of 4.2 days and additional healthcare provider visits for up to a sixth of affected patients. Patients also experience significant symptoms prior to receiving a transfusionCitation14–16. Transfusion delays mean that patients must endure symptoms of anemia such as fatigue, weakness, and shortness of breath for longer periods, inevitably leading to a substantial negative impact on disease burdenCitation17,Citation18. Moreover, with the trend toward restrictive transfusion thresholds and longer intervals between transfusions, any additional delays likely compound the adverse effects on quality of life (QoL). In a multinational study about experiences with transfusion care, a majority of patients with MDS endorsed higher hemoglobin transfusion thresholds to improve their QoL (62% preferred a threshold of ≥8.5 g/dL, and 20% preferred a threshold of ≥10 g/dL)Citation14. Thus, making patients, who experience low hemoglobin status due to more restrictive transfusion policies, wait even longer for a transfusion because of delays due to blood shortages increases their disease burden further and, therefore, the added delay has clinical meaning.
Moreover, additional visits to healthcare providers leads to increased economic burden to both the patient and healthcare resources and possibly negatively impacts the patient’s HRQoL. To date, little research has been performed to understand the consequences of blood supply shortages on patients with MDS and further studies are needed to investigate the additional burden of disease created by delayed RBC transfusions in this population. Although there are numerous Europe-wide incentives to increase blood donation and programs to improve blood supply management, ultimately, other supportive care and treatment options will continue to play a role to reduce TD in patients with MDS. Supportive care that aims to ameliorate the symptoms of the disease includes growth factors that improve blood count (e.g. erythropoietin and granulocyte colony-stimulating factor) and iron chelation drugs, such as deferoxamine, to manage buildup of excess iron due to blood transfusionsCitation17–19. Treatments that focus on improving the underlying bone marrow disease and slow the progression to leukemia include hypomethylating agents such as azacitidine, and immunomodulating therapy such as lenalidomideCitation18,Citation19. For high-risk patients with MDS, chemotherapy is recommended. Allogeneic stem cell transplantation is the only curative therapy available, but it has many side effectsCitation18,Citation19. Thus, even though numerous treatment options exist, many are not well tolerated; therefore, there is still a need for novel therapies that can reduce the dependence on blood transfusions and reduce the disease burden for patients with MDS.
In this study, physicians regarded patients’ ECOG PS, hemoglobin levels, and age as the top factors that impact the clinical, economic, and humanistic outcomes of patients with MDS. These perspectives align with studies of prognostic factors in the MDS population. ECOG PS was most frequently selected as an important factor and given the greatest mean impact score. This scale provides an overall impression of a patient’s level of function in self-care, daily activity, and physical activityCitation20, and is often used to help make treatment-related decisions. Several recent large-scale studies of azacitidine treatment in patients with high-risk MDS have shown ECOG PS to be a predictive factor for progression/leukemia-free survivalCitation21,Citation22 and overall survivalCitation22,Citation23. Such data may underlie the selection of ECOG PS as an important factor in the present study. Similarly, patient age and hemoglobin levels at disease onset influence treatment decisions and have been shown to correlate with QoL in patients with MDSCitation7,Citation24 and to provide information on survival and risk of progression to AMLCitation25.
Our results should be interpreted within the context of relevant study limitations. The self-reported nature of the survey is associated with potential corresponding biases such as inaccurate recall and false reporting (whether intentional or unintentional). Also, given the cross-sectional nature of the data, statements of causality cannot be made from the study results, and some types of variables (e.g. while on prescription treatment vs. not on prescription treatment) cannot be assessed. In addition, physician sample sizes in this study are small and might be too small to make certain inferences or assume certain patterns within different subgroups of interest. Furthermore, this survey was conducted online at the beginning of the COVID-19 pandemic (Q2 2020) and hence, there could be potential biases in terms of physician selection and the cohort recruited, which may influence the generalizability of results across all 5 countries in which physicians treating patients with MDS were surveyed.
There are a number of limitations that arise as a result of the survey design that should be considered in future work. The questionnaire does not include questions related to each physician’s transfusion threshold, and therefore, we cannot comment to what extent this factor may have impacted our findings. For example, in Europe, there is wide variability in the hemoglobin thresholds for transfusion. In Germany, transfusion policies are more liberal, with thresholds as high as 8–10 g/dL, whereas in other countries, such as Greece, a more restrictive transfusion threshold of 7 g/dL is recommended for patients with no cardiac comorbidityCitation26–28. These differences in threshold levels may reflect each country’s respective blood availability and blood safetyCitation29,Citation30. Restrictive transfusion thresholds have helped to counter blood supply shortages by reducing the number of transfusions and, in countries where blood safety is still not assured, having a lower threshold has helped to reduce the risk of infection from potentially contaminated bloodCitation30. However, despite these guidelines, adherence by practitioners to the restrictive thresholds is often poorCitation31 and any data analyses that rely on threshold levels that are published in guidelines may be misleading. Furthermore, the survey questionnaire asked physicians specifically regarding blood supply shortages. However, the delay in RBC transfusions could also have been due to the patient developing antibodiesCitation32 and/or availability of storage space in facilities.
Conclusion
Two-thirds of physicians reported that shortage of blood supply resulted in a delay in RBC transfusions for patients with MDS requiring transfusions. A total of 17.2% of physicians reported that ≥25% of their patients with MDS requiring transfusions experienced a transfusion delay due to blood supply issues. Patients’ ECOG PS, hemoglobin level, and age were the top factors reported by more than two-thirds of physicians to impact outcomes of patients with MDS. New treatment options should be explored to help patients with MDS to become TI, which may also help improve clinical, economic, and humanistic outcomes of patients with MDS.
Transparency
Declaration of funding
The study was sponsored by Bristol Myers Squibb.
Declaration of financial/other relationships
SG, HC, and JG are employees of Cerner Enviza (formerly known as Kantar Health), which has provided consultancy for Bristol Myers Squibb. AGK and JT have provided consultancy to Bristol Myers Squibb. SJ and DT are employees of, and have equity ownership in, Bristol Myers Squibb. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Ethics approval
The study protocol was approved with exemption status by Pearl Institutional Review Board (Indianapolis, IN, USA). Participants gave informed consent before participation.
Gupta__CMRO__Physican_survey_MS_Supp_Material_Nov_17_clean.docx
Download MS Word (54.9 KB)Supp_Table.docx
Download MS Word (47.4 KB)Acknowledgements
Authors would like to thank Dr. Ann-Marie Waldron (Cerner Enviza GmbH, Munich) for medical writing assistance. The authors received editorial assistance in the preparation of this manuscript from Eilish McBurnie, PhD, of Excerpta Medica, supported by Bristol Myers Squibb. The authors are fully responsible for all content and editorial decisions for this manuscript.
Data availability statement
Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
- Malcovati L, Hellström-Lindberg E, Bowen D, et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults: recommendations from the European LeukemiaNet. Blood. 2013;122(17):2943–2964.
- Germing U, Lauseker M, Hildebrandt B, et al. Survival, prognostic factors and rates of leukemic transformation in 381 untreated patients with MDS and del(5q): a multicenter study. Leukemia. 2012;26(6):1286–1292.
- Harnan S, Ren S, Gomersall T, et al. Association between transfusion status and overall survival in patients with myelodysplastic syndromes: a systematic literature review and meta-analysis. Acta Haematol. 2016;136(1):23–42.
- Germing U, Oliva EN, Hiwase D, et al. Treatment of anemia in transfusion-dependent and non-transfusion-dependent lower-risk MDS: current and emerging strategies. HemaSphere. 2019;3(6):e314.
- Smith BD, Mahmoud D, Dacosta-Byfield S, et al. Health care utilization and risk of infection and bleeding among patients with myelodysplastic syndromes with/without transfusions, and with/without active therapy. Leuk Lymphoma. 2014;55(5):1119–1125.
- Lucioni C, Finelli C, Mazzi S, et al. Costs and quality of life in patients with myelodysplastic syndromes. Am J Blood Res. 2013;3(3):246–259.
- Oliva EN, Finelli C, Santini V, et al. Quality of life and physicians’ perception in myelodysplastic syndromes. Am J Blood Res. 2012;2(2):136–147.
- Szende A, Schaefer C, Goss TF, et al. Valuation of transfusion-free living in MDS: results of health utility interviews with patients. Health Qual Life Outcomes. 2009;7:81.
- Sekeres MA, Maciejewski JP, List AF, et al. Perceptions of disease state, treatment outcomes, and prognosis among patients with myelodysplastic syndromes: results from an internet-based survey. Oncologist. 2011;16(6):904–911.
- European Commission. Summary of the Conference on the Evaluation of the EU Legislation on Blood, Tissues and Cells. 2019; [cited 2022 March 2]. Available from: https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/btc_evaluationconference_sr_en.pdf.
- Gupta S, Kulasekararaj AG, Costantino H, et al. Association between transfusion status and clinical and economic outcomes in patients with myelodysplastic syndromes from the physicians’ perspective. Cancer Rep. 2022;2022:e1680.
- World Health Organization. Global Database on Blood Safety: Summary Report 2011. 2011; [cited 2022 March 2]. Available from: https://www.who.int/bloodsafety/global_database/GDBS_Summary_Report_2011.pdf.
- Grecuccio C, Ferraro M, Colafelice M, et al. Blood transfusion practice: state of the art on promoting blood donation in Italy. Biomed Prev. 2017;1:89.
- Vijenthira A, Starkman R, Lin Y, et al. Multi-national survey of transfusion experiences and preferences of patients with myelodysplastic syndrome. Transfusion. 2022;62(7):1355–1364.
- Koutsavlis I. Transfusion thresholds, quality of life, and current approaches in myelodysplastic syndromes. Anemia. 2016;2016:8494738.
- Wood EM, McQuilten ZK. Outpatient transfusions for myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2020;2020(1):167–174.
- Bowen DT. Treatment strategies and issues in low/intermediate-1-risk myelodysplastic syndrome (MDS) patients. Semin Oncol. 2005;32(4 Suppl 5):S16–S23.
- Platzbecker U. Treatment of MDS. Blood. 2019;133(10):1096–1107.
- Palacios-Berraquero ML, Alfonso-Piérola A. Current therapy of the patients with MDS: walking towards personalized therapy. J Clin Med. 2021;10(10):2107.
- Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655.
- Wehmeyer J, Zaiss M, Losem C, et al. Impact of performance status and transfusion dependency on outcome of patients with myelodysplastic syndrome, acute myeloid leukemia and chronic myelomonocytic leukemia treated with azacitidine (PIAZA study). Eur J Haematol. 2018;101(6):766–773.
- Papageorgiou SG, Kotsianidis I, Bouchla A, et al. Serum ferritin and ECOG performance status predict the response and improve the prognostic value of IPSS or IPSS-R in patients with high-risk myelodysplastic syndromes and oligoblastic acute myeloid leukemia treated with 5-azacytidine: a retrospective analysis of the Hellenic national registry of myelodysplastic and hypoplastic syndromes. Ther Adv Hematol. 2020;11:2040620720966121.
- Itzykson R, Thépot S, Quesnel B, et al. Prognostic factors for response and overall survival in 282 patients with higher-risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117(2):403–411.
- Stauder R, Yu G, Koinig KA, et al. Health-related quality of life in lower-risk MDS patients compared with age- and sex-matched reference populations: a European LeukemiaNet study. Leukemia. 2018;32(6):1380–1392.
- Falantes JF, Calderón C, Márquez Malaver FJ, et al. Clinical prognostic factors for survival and risk of progression to acute myeloid leukemia in patients with myelodysplastic syndromes with <10% marrow blasts and non-unfavorable cytogenetic categories. Clin Lymphoma Myeloma Leuk. 2013;13(2):144–152.
- Müller MM, Geisen C, Zacharowski K, et al. Transfusion of packed red cells: indications, triggers and adverse events. Dtsch Arztebl Int. 2015;112(29–30):507–517; quiz 518.
- Viprakasit V, Gattermann N, Lee JW, et al. Geographical variations in current clinical practice on transfusions and iron chelation therapy across various transfusion-dependent anaemias. Blood Transfus. 2013;11(1):108–122.
- Tsante A, Papandreadi A, Tsantes AG, et al. Seeking strategies to optimize blood utilization: the preliminary experience with implementing a patient blood management program in a Greek tertiary hospital. J Clin Med. 2021;10(10):2141.
- World Health Organization (WHO). Global Status Report on Blood Safety and Availability 2016. Geneva: WHO; 2017. Licence No. CC BY-NC-SA 3.0 IGO.
- Fong IW. Current trends and concerns in infectious diseases: emerging infectious diseases of the 21st century. New York: Springer; 2020. Chapter 8, Blood transfusion-associated infections in the twenty-first century: new challenges; p. 191–215.
- Mahecic TT, Dünser M, Meier J. RBC transfusion triggers: is there anything new? Transfus Med Hemother. 2020;47(5):361–368.
- Hendrickson JE, Tormey CA, Shaz BH. Red blood cell alloimmunization mitigation strategies. Transfus Med Rev. 2014;28(3):137–144.
