Abstract
Objective
Cancer patients are at high risk of venous thromboembolism (VTE), a significant cause of cancer-related death. Historically, low molecular weight heparins (LMWH) were the gold standard therapy for cancer-associated VTE, but recent evidence supports the use of direct factor Xa inhibitors in cancer-associated VTE and this is now reflected in many guidelines. However, uptake of direct factor Xa inhibitors varies and guidance on the use of direct factor Xa inhibitors in specific cancer sub-populations and clinical situations is lacking. This review presents consensus expert opinion alongside evaluation of evidence to support healthcare professionals in the use of direct factor Xa inhibitors in cancer-associated VTE.
Methods
Recent guidelines, meta-analyses, reviews and clinical studies on anticoagulation therapy for cancer-associated VTE were used to direct clinically relevant topics and evidence to be systematically discussed using nominal group technique. The consensus manuscript and recommendations were developed based on these discussions.
Results
Considerations when prescribing anticoagulant therapy for cancer-associated VTE include cancer site and stage, systemic anti-cancer therapy (including vascular access), drug-drug interactions, length of anticoagulation, quality of life and needs during palliative care. Treatment of patients with kidney or liver impairment, gastrointestinal disorders, extremes of bodyweight, elevated bleeding or recurrence risk, VTE recurrence and COVID-19 is discussed.
Conclusion
Anticoagulant therapy for cancer-associated VTE patients should be carefully selected with consideration given to the relative benefits of specific drugs when individualizing care. Direct factor Xa inhibitors are typically the treatment of choice for preventing VTE recurrence in non-cancer patients and should also be considered as such for cancer-associated VTE in most situations.
Introduction
Venous thromboembolism (VTE) is associated with poor prognosis and considerable morbidityCitation1,Citation2. It is the most significant cause of thrombotic death amongst cancer patients, accounting for approximately 4,000 cancer-related deaths each year in England and WalesCitation3. Compared with the general population, patients with active cancer have a 4- to 7-fold increased risk of VTE, including deep vein thrombosis (DVT) and pulmonary embolism (PE)Citation4,Citation5. While arterial thromboembolism, disseminated intravascular coagulation and thrombotic microangiopathy may present in patients with cancerCitation6, the most common form of cancer-associated thrombosis (CAT) is VTE, which is the focus of this article.
The pathophysiology of cancer-associated VTE is complex, several factors are known to increase the risk of VTE, including the primary tumor site, stage of cancer, surgical intervention and systemic anti-cancer treatment (SACT)Citation6. A UK cohort study estimated that the incidence rates of first VTE and VTE recurrence in patients with active cancer was 5.8 (95% confidence interval [CI], 5.7–6.0) and 9.6 (95% CI, 8.8–10.4) per 100 person-years, respectivelyCitation7. Anticoagulant treatment of VTE with low-molecular-weight heparins (LMWHs), vitamin K antagonists (VKAs) or direct factor Xa inhibitors effectively reduces thrombus progression, recurrence and associated mortalityCitation8.
Historically, LMWHs were considered the gold standard of care for cancer-associated VTE management, but it requires subcutaneous injections once or twice daily - a significant burden for patients who require long-term anticoagulationCitation9,Citation10. VKAs have a high risk of drug-drug interactions (DDIs) and require frequent laboratory monitoring of international normalized ratio (INR). Direct oral anticoagulants (DOACs), specifically direct factor Xa inhibitors (apixaban, edoxaban and rivaroxaban), are an appealing alternative in cancer patients due to the oral route of administration, predictable pharmacokinetics, rapid onset of action, short half-life, minimal food and drug interactions, and the lack of need for INR monitoringCitation11.
Data from pivotal trials have demonstrated the efficacy and safety of direct factor Xa inhibitors in cancer-associated VTECitation10,Citation12–17, leading to the approval of direct factor Xa inhibitors for managing cancer-associated VTE in the EUCitation18. In light of the expanding evidence base, direct factor Xa inhibitors have been incorporated into several treatment guidelines, some of which recognize them as a first line optionCitation19–22. However, in our experience, prescribing of direct factor Xa inhibitors for treatment of cancer-associated VTE is variable across the UK, despite the guidelines and supporting trial data. Reasons for this include concerns around potentially increased incidence of major bleeding eventsCitation23, lack of awareness, inadequate experience in prescribing direct factor Xa inhibitors, limited data for specific clinical situations, and uncertainty over their positioning within the anticoagulation treatment pathway.
Guidance on the role of direct factor Xa inhibitors for managing cancer-associated VTE may be helpful to UK prescribers. Therefore, in this article we discuss our view on the positioning of direct factor Xa inhibitors in the cancer-associated VTE treatment pathway, and endeavor to provide clarity on the appropriate prescription of anticoagulants in several sub-populations with complex clinical considerations. Our guidance incorporates available evidence supplemented by our consensus opinion as experienced practitioners in this field. This correlates with recently published European Society of Cardiology guidance on cardio-oncologyCitation24.
Methods
Relevant guidelines and recent clinical studies, meta-analyses and literature reviews on anticoagulation treatment for cancer-associated VTE were identified by pragmatic, non-structured hand searching of available literature relating to direct factor Xa inhibitor use for cancer-associated VTE. Searches were conducted on PubMed, Google Scholar and Ovid online using key word terms, which included cancer-associated thrombosis, venous thromboembolism, cancer, DOAC, apixaban, rivaroxaban, edoxaban, LMWH; supplementary evidence was also provided by the lead authors. The authors attended a virtual roundtable meeting in which direct factor Xa inhibitor clinical trial data were examined and the risk-benefit profile of direct factor Xa inhibitor use in different cancer subpopulations was discussed. Using a nominal group technique approach, each topic was discussed systematically by all clinical expert authors, who provided their input in turn. Based on these discussions the manuscript outline was drafted and consensus viewpoints were formulated. The meeting was facilitated by HEOR Ltd and chaired by ATC and RA. Follow-up discussions and revisions were conducted via email correspondence facilitated by ARM and PDG. All authors participated in revisions and approved the final article. Review and incorporation of comments from the clinical authors were conducted by ARM and PDG independently of Bristol Myers Squibb (BMS) and Pfizer.
Current treatment options for patients with cancer-associated VTE
Direct factor Xa inhibitors vs LMWH in initial treatment (up to 6 months)
summarizes the key phase III randomized controlled trials evaluating the safety and efficacy of direct factor Xa inhibitors for managing patients with cancer-associated VTE versus LMWH (dalteparin). The Caravaggio and ADAM VTE trials demonstrated non-inferior VTE recurrence rates with comparable bleeding risk for apixaban vs. dalteparin, a LMWHCitation10,Citation12. For edoxaban, the Hokusai VTE Cancer study found that most cancer patients could expect the same outcomes as with dalteparin, as shown by non-inferiority for edoxaban in the composite primary outcome of VTE recurrence and major bleedingCitation13. Edoxaban was considered by the investigators to have an acceptable risk-benefit profile in most cancer types, according to subgroup analysis of the Hokusai VTE Cancer trialCitation14. However, gastrointestinal (GI) cancers had a greater risk of bleeding, and special consideration is required before prescribing edoxaban in this groupCitation14. SELECT-D and CASTA DIVA (a non-inferiority trial) evaluated rivaroxaban versus dalteparinCitation15,Citation17. The SELECT-D trial demonstrated a significant reduction in VTE recurrences with rivaroxaban compared with dalteparin, while the CASTA DIVA trial had insufficient patient data to reach the non-inferiority criteria. Both found increases in clinically relevant non-major bleeding (CRNMB) versus LMWH that were comparable to other direct factor Xa inhibitors. Following review from the data and safety monitoring committee, the SELECT-D protocol was amended to exclude patients with GI cancers due to a safety signal of bleeding events with rivaroxaban in this subgroupCitation15.
Table 1. Trials evaluating direct factor Xa inhibitors versus LMWH in cancer-associated VTE populations.
A meta-analysis of five major trials (ADAM VTECitation10, CaravaggioCitation12, Hokusai VTE CancerCitation13, SELECT-DCitation15, and CASTA DIVACitation17) found direct factor Xa inhibitors were associated with significantly lower risk of VTE recurrence compared with LMWH (hazard ratio, HR: 0.63; 95% CI, 0.47–0.86) but also a non-significantly higher risk of major bleeding (HR: 1.26; 95% CI, 0.84−1.90) and a significantly higher risk of CRNMB (HR: 1.48; 95% CI, 1.18−1.85)Citation17. Other meta-analyses, which did not incorporate CASTA DIVA, had broadly similar findings but variations in confidence intervals led to differing conclusions on statistical significanceCitation25–27. Nevertheless, the outcomes from these analyses indicate that treatment with direct factor Xa inhibitors confer a similar improvement in risk of VTE recurrence to the improvement conferred by LMWH in comparison to VKAs (relative risk, RR = 0.60, 95% CI: 0.45−0.79)Citation28.
Direct factor Xa inhibitors vs LMWH for secondary prevention of VTE (beyond 6 months)
The SELECT-D extension study of rivaroxaban vs placebo evaluated patients after six months of trial anticoagulation, but the study was insufficiently powered to detect statistically significant differences in the primary endpointsCitation16. While there was an indication of long-term reduction of VTE recurrence, along with increased risk of bleeding, the population was at low risk of recurrence. A post hoc analysis of the Hokusai VTE Cancer trial, which examined extended therapy with edoxaban, demonstrated that it was as effective and had a similar rate of VTE recurrence and bleeding risk as seen with dalteparinCitation29. The results of the API-CAT (NCT03692065) and EVE (NCT03080883) trials are eagerly awaited: they examine reduced dose vs standard dose apixaban after six months of anticoagulation and will provide evidence on the incremental value of dose reduction to reduce the risk of bleeding versus the risk of VTE recurrenceCitation30,Citation31.
A systematic literature review of clinical studies assessing long-term anticoagulation reinforced current treatment guidelines, demonstrating that VTE recurrence is still a significant risk in those discontinuing anticoagulation after 6 monthsCitation1. Furthermore, a US retrospective database study found that although adherence (the extent to which a patient complies with their prescribed anticoagulant regimen) was similar between LMWH and DOACs, treatment persistence was greater for DOACs; i.e. patients remained on DOACs for longer on average than on LMWHCitation32. This suggests that, while LMWH is a reliable choice of anticoagulation therapy, it is perhaps less favourable than DOACs for longer-term treatment, as DOACs are more convenient for patients and LMWH may involve increased overall cost and treatment administration burdenCitation9,Citation32,Citation33.
The role of direct factor Xa inhibitors in managing cancer-associated VTE
Current treatment guidelines for the management of cancer-associated VTE
Current treatment guidelines for the management of cancer-associated VTE are summarized in , in order of publication date. Due to the protracted writing process and the ever-evolving landscape, they do not necessarily incorporate the most up-to-date evidence. All guidelines recommend a minimum of 3 months of anticoagulation, with most recommending at least 6 months. Extended phases of therapy beyond 6 months may be considered on an individual basis, dependent on an appropriate risk to benefit assessment. Direct factor Xa inhibitors and LMWH are consistently recommended over unfractionated heparin (UFH), fondaparinux and VKAs, such as warfarin, in most patient subgroups. VKAs are not recommended as the primary choice but as an option if direct factor Xa inhibitors or LMWH are contraindicated, inappropriate or unavailable.
Table 2. Summary of cancer-associated VTE clinical guidelines.
In the acute period of treatment for cancer-associated VTE, typically defined as the first 1–3 weeks, guidelines are split between recommending direct factor Xa inhibitorsCitation19,Citation20,Citation22 or LMWHCitation34–36. It should be noted that, for patients treated with edoxaban, LMWH is required for the initial 5 days following the incident cancer-associated VTE, unlike apixaban or rivaroxaban which can be initiated immediatelyCitation38. Over the standard treatment period, typically up to 6 months, guidelines state a preference for direct factor Xa inhibitors over LMWHCitation19,Citation20,Citation22, or recommend bothCitation35,Citation36, with the exception of the National Comprehensive Cancer Network (NCCN) guidelines, which recommends LMWHCitation34.
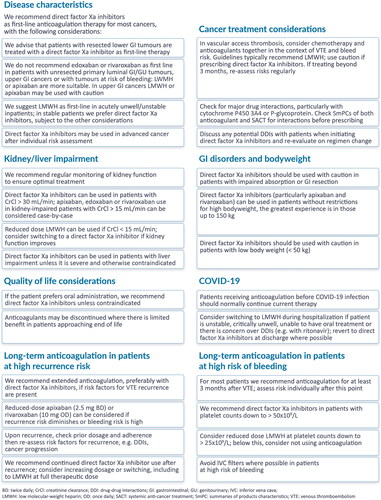
Despite the availability of treatment guidelines, there remains variation in how cancer-associated VTE is managed in the UK, with direct factor Xa inhibitors having not been fully embraced as a viable alternative to LMWH yet. This is in part due to a lack of experience of when and how to use direct factor Xa inhibitors, but also the result of insufficient guidance for specific and complex clinical situations that are often encountered during cancer-associated VTE management. We discuss some of these topics below and a synopsis is provided in .
Considering cancer site when prescribing anticoagulation therapy
The site of the primary cancer is a risk factor for VTE, VTE recurrence and bleeding. Hence, the site of origin is an important consideration when prescribing anticoagulants for cancer-associated VTE. In patients with cancer-associated VTE treated with a direct factor Xa inhibitor, a higher rate of overall bleeding events has been observed in those with pancreatic, colorectal, gastroesophageal, and genitourinary (GU) cancersCitation13–15,Citation39. Increased bleeding with direct factor Xa inhibitors may be due to mucosal bleeding which is influenced by malignancy type and the prescribed direct factor Xa inhibitor, with higher risk of bleeding in upper gastrointestinal (GI) malignancies versus LMWH, particularly with edoxaban or rivaroxabanCitation40,Citation41.
Our consensus viewpoint is that patients with luminal GI/GU cancer with an unresected primary tumor and tumors at risk of bleeding should not be prescribed edoxaban or rivaroxaban as first-line therapy; LMWH or apixaban are more suitable treatment strategies, provided no contraindications existCitation42,Citation43. We advise that patients with resected lower GI tumors are treated with a direct factor Xa inhibitor as first-line therapy; apixaban may be preferred since no increased risk of bleeding is apparent in patients with GI cancer receiving apixaban versus dalteparinCitation10,Citation12. We do not generally recommend direct factor Xa inhibitors in patients with upper GI cancer. However, apixaban or LMWH may be used with caution in this group, based on the limited trial data availableCitation44; risks (bleeding vs recurrence) and treatment preference should be discussed with the patient.
Data in certain cancer subtypes are insufficient, including brain metastases and hematological malignancies, often due to the exclusion criteria of clinical trials. As such, the transition to direct factor Xa inhibitors in these groups has been challenging. Nevertheless, real-world evidence suggests similar safety of direct factor Xa inhibitors and LMWH in patients with primary brain tumors and brain metastases, though further robust data are required to warrant a recommendation for direct factor Xa inhibitors in these populationsCitation45. We consider observational data to be useful for informing clinical practice where randomized trial data in sub-populations are scarce or non-existent, but such data should be used with caution.
Considering cancer stage when prescribing anticoagulant therapy
The risk of VTE recurrence and major bleeding increases with advancing cancer stageCitation6. Accordingly, our consensus view is to consider whether the cancer is localized, locally spread or metastatic when prescribing anticoagulation therapy. Cancer patients may also exhibit highly dynamic characteristics, including fluctuating platelet count and organ function, requiring regular modifications to treatment regimens. It is therefore necessary to individualize patient assessment and review therapy in response to patients’ evolving needs along their cancer pathwayCitation46.
Direct factor Xa inhibitors can be prescribed to patients at any stage of cancer, though locally spread and metastatic cancers are at a greater risk of recurrent VTE and of major bleeding events with anticoagulation treatmentCitation47. We suggest advanced stage cancer patients may be treated with direct factor Xa inhibitors according to an individualized risk-benefit profile of recurrence and bleeding risk. We also consider LMWH to be the preferred first-line option in acutely unwell and/or unstable hospitalized patients, as LMWH have fewer DDIs than direct factor Xa inhibitorsCitation43. They also have a shorter half-life and can be administered in patients with organ dysfunction, thrombocytopenia, or in need of an invasive procedure, with easier dose management if necessary. For more stable outpatients, we consider direct factor Xa inhibitors to be a more suitable long-term option.
Anticoagulation therapy in patients with vascular access thrombosis
Upper limb and catheter-associated VTE is prevalent in cancer patientsCitation48, but there is insufficient guidance on how to manage it. In addition, patients often have vascular access devices for delivery of SACT, which are an additional potential risk factor for bleeding and thrombosis. For these reasons, SACT and anticoagulant regimens should be considered together in the context of the associated risk. Guidelines typically recommend LMWH for the treatment of cancer-associated VTE in patients with line-associated thrombosisCitation49,Citation50, though direct factor Xa inhibitors are used in clinical practice at some centres. More trials are required to verify observational findings that direct factor Xa inhibitors preserved line function and reduced recurrence after catheter-associated thrombosisCitation51, and there was no observed difference in VTE recurrence and bleeding risk versus LMWHCitation52. Nevertheless, we suggest both LMWH and direct factor Xa inhibitors are appropriate treatment options for line-associated thrombosis and advise a treatment duration of three months. Should the line remain in place beyond a 3-month treatment period, we suggest the benefit of continuing anticoagulation, in relation to risk of bleeding or VTE recurrence, should be regularly re-assessed.
Drug-drug interactions
It should be noted that many DDIs are based on theoretical knowledge, and there is a paucity of data to establish their clinical relevance. This can lead to a reluctance to prescribe direct factor Xa inhibitors. A significant proportion of clinical trials assessing novel SACT exclude patients who are prescribed direct factor Xa inhibitors because of the lack of understanding of DDIs, which in turn restricts the availability of high-quality data on DDIs. In general, we advise to check for major drug interactions for acute VTE treatment, particularly those interacting with cytochrome P450 (CYP) 3A4 enzymes or P-glycoprotein (P-gp), to ensure there is a clear understanding of the risk of DDIs. Edoxaban has minimal CYP3A4 enzyme interaction and hence may be suitable in patients receiving concomitant therapy with drugs metabolized via this pathwayCitation53.
A published analysis of DDI databases and summaries of product characteristics (SmPCs) concluded that warfarin has greater DDI potential than other anticoagulants, while LMWH had the lowest potentialCitation53. It also reported that there was no difference in DDI potential between DOACs as a whole, although each DOAC may have different degrees or types of interactions. More specifically, a post hoc analysis of Caravaggio trial data considered interactions with cytotoxic agents, demonstrating that patients on apixaban or dalteparin showed no increased risk of VTE recurrence or major bleeding when receiving concomitant anti-cancer therapyCitation54. Before prescribing any anticoagulant, the SmPCs of the anticoagulant and SACTs should be reviewed to ensure safe use.
The anticoagulant of choice is a shared decision with the patient and they should be made aware of the likelihood of any potential DDIs, preferably with assistance from pharmacists to optimize treatment to reduce DDIsCitation55. Some patients with moderate risk of DDI may be willing to have assessment of anti-factor Xa levels to avoid regular injectable therapies; therefore, personalized care should always be provided. However, regular monitoring is of no value in ensuring therapeutic anti-factor Xa levels since target ranges have not been established and there is no evidence to guide changes in management based on anti-factor Xa levels. Nevertheless, where DDIs are of concern, measuring anti-factor Xa plasma levels, on an individual basis, may be considered. In addition to SACT, we suggest supportive care and concomitant medication such as anticonvulsants or antifungal therapy should be reviewed for potential DDIs. Caution should also be given to concomitant prescription of antiplatelet agents, specifically thienopyridines (clopidogrel) and/or aspirin, as evidence suggests elevated bleed risk in those receiving oral anticoagulantsCitation56. As a consensus group, we recommend that the decision to extend treatment with anticoagulants should be regularly evaluated to consider the dynamic risk of VTE and bleeding related to the cancer (response or progression), cancer treatment, which can include sudden wholesale change of “line of treatment” and individual patient factors.
Quality of life considerations
Patients generally prefer orally administrable options over injectable treatments, assuming it causes minimal disruption to current SACTCitation57. Patients have shown improved treatment satisfaction for DOACs compared to VKAsCitation58, and LMWHCitation59–61. In the SELECT-D trial, there was no difference in measurable health-related quality of life or coping with LMWH vs rivaroxabanCitation15, but the COSIMO study found that patients with cancer-associated VTE who switched from LMWH to rivaroxaban had improved treatment satisfactionCitation59. A similar outcome was seen in the ADAM-VTE trial, whereby patient satisfaction scores favored apixaban over dalteparinCitation10. Furthermore, greater treatment satisfaction is associated with better adherence, compliance and persistenceCitation62, thereby improving treatment outcomes. With this in mind, our consensus view is that DOACs should be used where there is patient preference for oral administration over parenteral, unless DOAC use disrupts anti-cancer regimens or is contraindicated.
Appropriate use of anticoagulation therapy in palliative care
Existing guidelines for cancer-associated VTE do not consider optimal anticoagulation treatment in palliative care, and recommend indefinite anticoagulation for patients with active cancerCitation63. However, for terminally ill cancer patients, we suggest to balance priorities when prescribing anticoagulants, with particular regard to the inconvenience and discomfort of parenteral agents. We therefore suggest that anticoagulants may be discontinued altogether in circumstances where there is limited benefit and patients are at the end of life.
Role of direct factor Xa inhibitors in cancer patients with complex clinical needs
Cancer patients often have complex needs that require careful consideration when prescribing anticoagulants, including those with kidney or liver impairment, gastrointestinal disorders, nausea/vomiting, extremes of body weight, increased risk of bleeding, increased risk of VTE recurrence and patients hospitalized with COVID-19.
Kidney impairment
Kidney function must be taken into account when considering an anticoagulation regimen. In line with the phase III direct factor Xa inhibitor registration studies, we suggest calculating creatinine clearance (CrCl) instead of estimated glomerular filtration rate (eGFR) in patients receiving a direct factor Xa inhibitor to avoid overestimating kidney function. Due to the exclusion criteria of many trials, there are limited clinical data surrounding the use of anticoagulants in patients with cancer-associated VTE and moderate to severely impaired kidney function. However, a post hoc analysis of Caravaggio showed that moderate kidney impairment (CrCl 30–59 mL/min) was not associated with an increased risk of major bleeding or recurrent VTE in cancer patients treated with apixaban or dalteparin, supporting the use of direct factor Xa inhibitors in patients with moderate kidney impairmentCitation64. We suggest initiating apixaban in patients with kidney impairment owing to the reduced dependence on renal clearance versus other direct factor Xa inhibitorsCitation65. Based on our consensus, we recommend that patients with cancer can be offered apixaban if CrCl is greater than 30 mL/min. The SmPC allows patients for CrCl as low as 15 mL/min to be prescribed apixabanCitation66, but this should be considered carefully on a case by case basis, similarly to comparable patients without cancer.
For patients with CrCl < 15 mL/min or on kidney replacement therapy we recommend LMWH at a reduced dose and, should kidney function improve, we support switching to a direct factor Xa inhibitor. It is important to note that therapeutic doses of LMWH may also accumulate in patients with severe kidney impairment and subsequent measurement of anti-Xa levels may be indicated.
Elevated risk of VTE recurrence is an important factor to consider in patients with kidney impairment. Additionally, prescribing anticoagulants in these patients may be further complicated by the presence of comorbidities and/or end-stage kidney disease, where anticoagulation may be affected by dialysis. Kidney function may also fluctuate significantly over relatively short periods. We therefore recommend regular monitoring of kidney function to ensure treatment remains optimized.
Liver impairment
A reduction in liver function is likely to affect the safety and effectiveness of anticoagulant treatment, as well as the detoxification of chemotherapy. We consider direct factor Xa inhibitors to be the preferred anticoagulant option unless liver impairment is sufficiently severe for them to be contraindicated (as defined in the individual SmPCs). Patients with hepatocellular or pancreatic cancer may be at an increased risk of liver impairment. For this reason, we recommend liver function tests and assessment of patients according to the Child-Pugh score; low serum albumin may also be a sign of significant liver impairment in this patient groupCitation67. We recommend special consideration should be given to potential DDIs in liver-impaired patients prescribed anticoagulants, and we suggest individualized treatment decisions should be made according to patient condition.
Gastrointestinal disorders and nausea/vomiting
In general, we suggest patients with GI conditions can be given direct factor Xa inhibitors for cancer-associated VTE management. However, patients with acute nausea, persistent vomiting or dysphagia who are unable to take oral medication and do not receive nasogastric intubation, may be managed temporarily with LMWHCitation68. Should GI complications subside, we suggest that treatment should be reverted to direct factor Xa inhibitors. We consider that there is a need for caution when prescribing DOACs to patients with possible impaired GI absorption such as those with bowel disease or substantial resection. Limited evidence suggests that DOAC absorption varies depending on the resection siteCitation69; however, further research is required to confirm such associations. Many patients are able to absorb DOACs despite resection, but we recommend measuring a drug-specific anti-factor Xa level or to assess plasma concentration and confirm absorption. However, it is important to note that measuring DOAC levels is of limited use as therapeutic ranges are yet to be clearly definedCitation70. The dynamic nature of GI complications in cancer patients should be considered and we recommend that anticoagulation regimens should be adapted accordingly.
Extremes of body weight
The International Society on Thrombosis and Haemostasis (ISTH) guidelines (2021) state that standard doses of rivaroxaban and apixaban are appropriate treatment strategies for VTE regardless of high bodyweight (>120 kg) and BMI (>40 kg/m2), and regular peak or trough measurements are not considered necessaryCitation71. However, the NICE guidelines are yet to be updated and only recommend direct factor Xa inhibitors in patients with a body weight lower than 50 kg or greater than 120 kg if therapeutic levels are monitoredCitation22. As a consensus group, we support direct factor Xa inhibitor use, particularly apixaban and rivaroxaban, in patients with upper extremes of body weight up to 150 kg, given that pharmacokinetic data and real-world evidence suggest that direct factor Xa inhibitors are unlikely to require dose alterations. For example, an observational study of 100 patients weighing over 120 kg reported reassuring pharmacokinetic data for DOACs in patients up to 230 kgCitation72. However, the number of patients with weights exceeding 150 kg included in previous studies have been limited, thus we suggest caution may be warranted in this subgroup and checking a trough level may be considered in these patients.
Conversely, for patients with very low body weight (<50 kg), we recommend particular care should be given to the prescription of anticoagulants, in part due to the paucity of data in underweight patients. The Hokusai VTE trial was the only trial assessing a direct factor Xa inhibitor that stratified dosing by body weight, demonstrating efficacy and safety in underweight patients (<60 kg) at a reduced dose (30 mg)Citation73, a recommendation which can be found in the SmPCCitation38. Additionally, a cross-sectional study found that underweight (<60 kg) cancer patients treated with half-dose (2.5 mg, twice daily) apixaban had comparable plasma trough levels to patients with bodyweight greater than 60 kg at full doseCitation74. It should be noted that reduced doses of apixaban and rivaroxaban are not specifically licensed in this setting. Nevertheless, we urge caution for prescribing direct factor Xa inhibitors, including edoxaban, in patients with very low body weight as there is insufficient data to confirm their safety. We consider LMWH to be a viable alternative in patients with extreme low body weight, although minimal subcutaneous fat in some patients will complicate administration.
Long-term direct factor Xa inhibitor therapy in patients with cancer-associated VTE at high risk of bleeding
When prescribing anticoagulants, we recommend that the clot type (DVT or PE) and site (distal or proximal DVT; peripheral PE or central PE) should be taken into consideration, as well as the length of time since the VTE event. Additionally, consideration should be given to the reversibility of anticoagulant therapies when prescribing in patients at elevated risk of bleedingCitation75.
In most patients, anticoagulation therapy should be prescribed for a minimum of 3 months following a VTE event, according to most guidelines (). After this treatment period, it should be ensured that those with a comparatively low VTE recurrence risk and high bleed risk are not treated with anticoagulants beyond the period where risk outweighs benefit. In those with moderate to low bleeding risks, we suggest that anticoagulation may continue for longer than six months if a patient has an active underlying disease or risk factors for VTE recurrence are still present.
Thrombocytopenia a reduction in the number of circulating platelets that is common in cancer patients, can result in bleeding and bruising, and retard blood clotting after injury. It often presents as a “dynamic risk” to patients during anticancer therapy, as platelet counts can fluctuate significantlyCitation76. Currently, there is limited data on the use of direct factor Xa inhibitors in patients with significant thrombocytopenia due to exclusion criteria in many trials. Nevertheless, our consensus is that direct factor Xa inhibitors should be prescribed in patients with platelet counts as low as 50 × 109/L. If counts are lower than this, we advise considering platelet support and reduced dose LMWH down to a minimum platelet count of 20–25 × 109/L, with careful consideration given to the timing of acute or non-acute VTE recurrence. For those with platelet counts below 20 × 109/L, we advise considering withholding anticoagulation.
Dose reduction is preferable to discontinuing therapy entirely, and platelet transfusions should also be considered for patients with acute VTE to enable therapeutic dose anticoagulation to be administered, particularly in the first month after VTE when VTE-related death and recurrence are particularly highCitation77.
Where it is possible, we recommend that inferior vena cava (IVC) filters should be avoided, though, they may be necessary in patients with a very recent VTE who are actively bleeding or who have an absolute contraindication to anticoagulation therapy. If required, retrievable IVC filters should be used and should be removed when bleeding risk has subsided and anticoagulants can be used.
Long-term direct factor Xa inhibitor therapy in patients with cancer-associated VTE at high risk of recurrence
All patients should be assessed for their risk of recurrences at 3–6 months, in consultation with their oncologists, evaluating cancer progression and anticoagulation strategies, according to clinical guidelines. Many cancer-associated VTE patients will have long-term risk factors that will maintain the risk of recurrence over longer periods, such as active cancer, metastatic disease, concurrent SACT, a previous history of venous thrombosis, and the ongoing presence of central lines. In these instances, we recommend extended anticoagulation, preferably using direct factor Xa inhibitors, for as long as the risk factors remain present. Should the patient also be deemed to have a high risk of bleeding, we suggest that a reduced dose of apixaban (2.5 mg BD, instead of 5 mg BD) or rivaroxaban (10 mg OD, instead of 20 mg OD) can be considered. Further evidence on the long-term efficacy of reduced dose apixaban is expected from the API-CAT and EVE trialsCitation30,Citation31. We suggest that factors such as the presence or absence of residual DVT at 6 months, but not an elevated D-dimer in cancer patients, may be taken into consideration when determining whether to continue anticoagulation.
Recurrent VTE may still occur in patients receiving anticoagulation treatment. Therefore, when managing a suspected recurrence while on treatment, we recommend that it should first be established whether there is a true recurrence. Extensions of existing clots are difficult to diagnose without definitive diagnostic imaging. Next, it should be established whether the patient is on appropriate anticoagulation treatment at the correct dose and is sufficiently adherent. Once these factors are ascertained, other risk factors for recurrence should be considered, including DDIs and progression of the cancer. Evidence is supportive of continuing direct factor Xa inhibitors, which are associated with the lowest rates of VTE recurrence in patients with cancer-associated VTE when compared to LMWH and VKAsCitation8,Citation78. Patients on a direct factor Xa inhibitor who have had a recurrence should preferably receive increased dosing, up to the maximum licensed dose if necessary, or switch to alternative direct factor Xa inhibitors. However, we suggest switching to a full therapeutic dose of LMWH may also be considered, and if recurrence arises while already on therapeutic LMWH we advise increasing the dose of LMWH by 20–25% and considering conducting an anti-Xa assay.
The effect of COVID-19 on medical care for patients with cancer-associated VTE
Cancer patients with coronavirus infections are more likely to be hospitalized and develop VTE versus those without cancerCitation79. However, there are no specific treatment guidelines regarding extended thromboprophylaxis or VTE treatment in cancer patients with COVID-19 infectionCitation80.
If patients are already receiving anticoagulation therapy before infection we recommend that they should remain on the same therapy. If necessary (for example, if patients are unstable, critically unwell, or unable to ingest oral therapies), we advise that clinicians should consider switching to LMWH for the duration of the inpatient stay, in line with published guidance for VTE prophylaxis in patients with COVID-19Citation81,Citation82. Additionally, consideration should be given to potential DDIs when treating with direct factor Xa inhibitors. DOACs may also interact with certain antiviral medication such as ritonavir (a component of Paxlovid), resulting in increased exposure to the DOAC and increased risk of bleedingCitation83. Hence, where there is particular concern surrounding DDIs, we suggest LMWHs may be considered as an alternative. Before patients are discharged from hospital, they should generally be re-commenced on the medication they were admitted on where possible.
Conclusion
This article provides guidance on the management of cancer-associated VTE in diverse circumstances based on the consensus opinion of clinicians from a range of specialisms with expertise in treating these patients. Although a systematic approach was used, a limitation of the article is that it does not constitute a formal treatment guideline, as a comprehensive guideline-writing methodology was not applied.
DOACs are typically the standard of care for preventing VTE recurrence in non-cancer patients and should also be considered as the standard of care for first-line treatment for VTE in patients with cancer. Anticoagulation through the use of LMWH reduces VTE recurrences by 40% compared to VKAsCitation28, and recurrence may be further reduced by 40% when managed with direct factor Xa inhibitors compared to LMWHCitation27, demonstrating the fundamental benefit of appropriate use of direct factor Xa inhibitors for patients with cancer-associated VTE. The challenges associated with managing cancer patients mean that they should be carefully selected for the most appropriate class of anticoagulant therapy, and consideration should be given to the relative benefits of specific drugs when tailoring individualized care. LMWH may be preferred in some clinical settings, particularly in acutely unwell and/or unstable patients and patients with upper GI cancer, since there is more experience in prescribing LMWH, fewer DDIs and lower bleeding risk. Individualized care personalized to patient requirements and preferences is always required. However, increased use of direct factor Xa inhibitors to manage cancer-associated VTE has the potential to reduce the incidence of VTE recurrence and the associated morbidity and mortality.
Transparency
Declaration of funding
This work was supported by Pfizer and Bristol Myers Squibb, who financed the medical writing and publication costs during the development and publication of this manuscript. Bristol Myers Squibb actively participated in the development of this manuscript.
Declaration of financial/other relationships
ATC has received fees for serving on an adjudication committee from Boehringer Ingelheim and AbbVie; grant support and fees for serving on committees from Bristol Myers Squibb, Daiichi Sankyo and Pfizer; consulting fees from Janssen, Portola Pharmaceuticals and Ono Pharmaceuticals; fees for serving on a steering committee and consulting fees from Bayer. CAB has received consultant fees/honoraria from Ablynx, Bayer, BMS/Pfizer Alliance, Lilly, Novartis, and Portola Pharmaceuticals; in addition to fees from Amgen, Bayer, BMS/Pfizer Alliance, Eli Lilly, Janssen, and Novartis. AY has received consultant fees/honoraria from BMS/Pfizer Alliance, Chugai and LEO Pharma and an unrestricted educational grant from Bayer. AM has received financial support from Bayer, Boehringer Ingelheim, BMS and LEO Pharma, in addition to consultant fees/honoraria from Bayer, BMS, LEO Pharma and Pfizer. He has also received speaker fees from Bayer, LEO Pharma, Pfizer and Sanofi, and served on advisory boards for Bayer, BMS, LEO Pharma and Pfizer. BV has received consulting fees from Eisai, EUSA Pharma and Ipsen, speaker fees for BMS, Eisai, EUSA Pharma, Ipsen, Merck Sharp & Dohme Oncology, Pfizer/EMD Serono, travel support from BMS, EUSA Pharma and Ipsen, and participation on Data Safety Monitoring boards and//or advisory boards for Merch Sharp & Dohme Oncology, Esai, Janssen. NHJ has received speaker fees from Bayer, BMS, Pfizer, Daiichi Sankyo and Leo Pharma. GB has received speakers and served on advisory boards for BMS, Bayer and Daiichi Sankyo. SC has served on advisory boards with Pfizer, BMS, Jazz and Sanofi. KGP, DB, CC and SM are employees of BMS. ARM and PDG are/were employees of Health Economics and Outcomes Research Ltd., Cardiff, UK. Health Economics and Outcomes Research Ltd. received fees from BMS in relation to this study. RA has received financial support and consultant fees/honoraria from BMS, Bayer, Daiichi Sankyo, Pfizer and Portola Pharmaceuticals.
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
All authors contributed to the conception, writing and review of this article. All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Acknowledgements
Medical writing and editorial support was provided by Chloe Salter and Jo Whelan of Health Economics and Outcomes Research Ltd., Cardiff, UK. Health Economics and Outcomes Research Ltd. received fees from BMS in relation to this study.
Data availability statement
None
References
- Moik F, Colling M, Mahé I, et al. Extended anticoagulation treatment for cancer-associated thrombosis-rates of recurrence and bleeding beyond 6 months: a systematic review. J Thromb Haemost. 2022;20(3):619–634.
- Khorana AA. Venous thromboembolism and prognosis in cancer. Thromb Res. 2010;125(6):490–493.
- All-Party Parliamentary Thrombosis Group. Venous thromboembolism (VTE) in cancer patients: cancer, chemotherapy and clots; 2015. Available from: http://apptg.org.uk/wp-content/uploads/2016/12/VTE-in-Cancer-Patients-2015.pdf#:∼:text=Of%20the%20patients%20who%20died%20of%20cancer%20in,underestimate%20of%20the%20true%20scale.%20High%20Risk%20Cancers.
- Fuentes HE, Tafur AJ, Caprini JA. Cancer-associated thrombosis. Dis Mon. 2016;62(5):121–158.
- Nicholson M, Chan N, Bhagirath V, et al. Prevention of venous thromboembolism in 2020 and beyond. J Clin Med. 2020;9(8):2467.
- Abdol Razak NB, Jones G, Bhandari M, et al. Cancer-associated thrombosis: an overview of mechanisms, risk factors, and treatment. Cancers. 2018;10(10):380.
- Cohen AT, Katholing A, Rietbrock S, et al. Epidemiology of first and recurrent venous thromboembolism in patients with active cancer. A population-based cohort study. Thromb Haemost. 2017;117(1):57–65.
- Sobieraj DM, Baker WL, Smith E, et al. Anticoagulation for the treatment of cancer-associated thrombosis: a systematic review and network meta-analysis of randomized trials. Clin Appl Thromb Hemost. 2018;24(9_suppl):182s–187s.
- van der Wall SJ, Klok FA, den Exter PL, et al. Continuation of low-molecular-weight heparin treatment for cancer-related venous thromboembolism: a prospective cohort study in daily clinical practice. J Thromb Haemost. 2017;15(1):74–79.
- McBane IR, Wysokinski WE, Le-Rademacher JG, et al. Apixaban and dalteparin in active malignancy-associated venous thromboembolism: the ADAM VTE trial. J Thromb Haemost. 2020;18(2):411–421.
- Elyamany G, Alzahrani AM, Bukhary E. Cancer-associated thrombosis: an overview. Clin Med Insights Oncol. 2014;8:CMO.S18991.
- Agnelli G, Becattini C, Meyer G, Caravaggio Investigators, et al. Apixaban for the treatment of venous thromboembolism associated with cancer. N Engl J Med. 2020;382(17):1599–1607.
- Raskob GE, van Es N, Verhamme P, Hokusai VTE Cancer Investigators, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018;378(7):615–624.
- Mulder FI, van Es N, Kraaijpoel N, et al. Edoxaban for treatment of venous thromboembolism in patient groups with different types of cancer: results from the Hokusai VTE cancer study. Thromb Res. 2020;185:13–19.
- Young AM, Marshall A, Thirlwall J, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 2018;36(20):2017–2023.
- Marshall A, Levine M, Hill C, et al. Treatment of cancer‐associated venous thromboembolism: 12‐month outcomes of the placebo versus rivaroxaban randomization of the SELECT‐D trial (SELECT‐D: 12m). J Thromb Haemost. 2020;18(4):905–915.
- Planquette B, Bertoletti L, Charles-Nelson A, CASTA DIVA Trial Investigators, et al. Rivaroxaban vs. dalteparin in cancer-associated thromboembolism: a randomized trial. CHEST. 2022;161(3):781–790.
- Musgrave KM, Power K, Laffan M, et al. Practical treatment guidance for cancer-associated thrombosis – managing the challenging patient: a consensus statement. Crit Rev Oncol Hematol. 2022;171:103599.
- Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021;5(4):927–974.
- Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021;160(6):e545–e608.
- Streiff MB, Holmstrom B, Angelini D, et al. NCCN guidelines insights: cancer-associated venous thromboembolic disease, version 2.2018. J Natl Compr Canc Netw. 2018;16(11):1289–1303.
- National Institute for Health and Care Excellence. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing [NG158]; 2020. Available from: https://www.nice.org.uk/guidance/ng158.
- Li A, Garcia DA, Lyman GH, et al. Direct oral anticoagulant (DOAC) versus low-molecular-weight heparin (LMWH) for treatment of cancer associated thrombosis (CAT): a systematic review and meta-analysis. Thromb Res. 2019;173:158–163.
- European Society of Cardiology. ESC guidelines on cardio-oncology; 2022. Available from: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Cardio-oncology-guidelines.
- Giustozzi M, Agnelli G, Del Toro-Cervera J, et al. Direct oral anticoagulants for the treatment of acute venous thromboembolism associated with cancer: a systematic review and meta-analysis. Thromb Haemost. 2020;120(7):1128–1136.
- Mulder FI, Bosch FTM, Young AM, et al. Direct oral anticoagulants for cancer-associated venous thromboembolism: a systematic review and meta-analysis. Blood. 2020;136(12):1433–1441.
- Riaz IB, Fuentes HE, Naqvi SAA, et al. Direct oral anticoagulants compared with dalteparin for treatment of cancer-associated thrombosis: a living, interactive systematic review and network meta-analysis. Mayo Clin Proc. 2022;97(2):308–324.
- Posch F, Königsbrügge O, Zielinski C, et al. Treatment of venous thromboembolism in patients with cancer: a network meta-analysis comparing efficacy and safety of anticoagulants. Thromb Res. 2015;136(3):582–589.
- Di Nisio M, van Es N, Carrier M, et al. Extended treatment with edoxaban in cancer patients with venous thromboembolism: a post-hoc analysis of the Hokusai-VTE cancer study. J Thromb Haemost. 2019;17(11):1866–1874.
- Mahé I, Agnelli G, Ay C, et al. Extended anticoagulant treatment with full- or reduced-dose apixaban in patients with cancer-associated venous thromboembolism: rationale and design of the API-CAT study. Thromb Haemost. 2022;122(4):646–656.
- McBane RD, 2nd, Loprinzi CL, Ashrani A, et al. Extending venous thromboembolism secondary prevention with apixaban in cancer patients: the EVE trial. Eur J Haematol. 2020;104(2):88–96.
- Schaefer JK, Li M, Wu Z, et al. Anticoagulant medication adherence for cancer-associated thrombosis: a comparison of LMWH to DOACs. J Thromb Haemost. 2021;19(1):212–220.
- Li A, Manohar PM, Garcia DA, et al. Cost effectiveness analysis of direct oral anticoagulant (DOAC) versus dalteparin for the treatment of cancer associated thrombosis (CAT) in the United States. Thromb Res. 2019;180:37–42.
- National Comprehensive Cancer Network. Cancer-associated venous thromboembolic disease; 2022. Available from: https://www.nccn.org/professionals/physician_gls/pdf/vte.pdf.
- Key NS, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2020;38(5):496–520.
- Farge D, Frere C, Connors JM, International Initiative on Thrombosis and Cancer (ITAC) Advisory Panel, et al. International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. Lancet Oncol. 2019;20(10):e566–e581.
- Khorana AA, Noble S, Lee AYY, et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost. 2018;16(9):1891–1894.
- European Medicines Agency (EMA). Lixiana 60mg film-coated tablets – summary of product characteristics (SmPC); 2022. Availbale from: https://www.ema.europa.eu/en/documents/product-information/lixiana-epar-product-information_en.pdf.
- Kim JH, Yoo C, Seo S, et al. A phase II study to compare the safety and efficacy of direct oral anticoagulants versus subcutaneous dalteparin for cancer-associated venous thromboembolism in patients with advanced upper gastrointestinal, hepatobiliary and pancreatic cancer: PRIORITY. Cancers. 2022;14(3):559.
- Kraaijpoel N, Di Nisio M, Mulder FI, et al. Clinical impact of bleeding in cancer-associated venous thromboembolism: results from the Hokusai VTE cancer study. Thromb Haemost. 2018;118(8):1439–1449.
- Ingason AB, Hreinsson JP, Ágústsson AS, et al. Rivaroxaban is associated with higher rates of gastrointestinal bleeding than other direct oral anticoagulants: a nationwide propensity score-weighted study. Ann Intern Med. 2021;174(11):1493–1502.
- Ageno W, Vedovati MC, Cohen A, et al. Bleeding with apixaban and dalteparin in patients with cancer-associated venous thromboembolism: results from the Caravaggio study. Thromb Haemost. 2021;121(5):616–624.
- Wojtukiewicz MZ, Skalij P, Tokajuk P, et al. Direct oral anticoagulants in cancer patients. Time for a change in paradigm. Cancers. 2020;12(5):1144.
- Agnelli G, Muñoz A, Franco L, et al. Apixaban and dalteparin for the treatment of venous thromboembolism in patients with different sites of cancer. Thromb Haemost. 2022;122(5):796–807.
- Leader A, Hamulyák EN, Carney BJ, et al. Intracranial hemorrhage with direct oral anticoagulants in patients with brain metastases. Blood Adv. 2020;4(24):6291–6297.
- Picker N, Lee AY, Cohen AT, et al. Anticoagulation treatment in cancer-associated venous thromboembolism: assessment of patient preferences using a discrete choice experiment (COSIMO study). Thromb Haemost. 2021;121(2):206–215.
- Verso M, Agnelli G, Munoz A, et al. Recurrent venous thromboembolism and major bleeding in patients with localised, locally advanced or metastatic cancer: an analysis of the Caravaggio study. Eur J Cancer. 2022;165:136–145.
- Marin A, Bull L, Kinzie M, et al. Central catheter-associated deep vein thrombosis in cancer: clinical course, prophylaxis, treatment. BMJ Support Palliat Care. 2021;11(4):371–380.
- Sousa B, Furlanetto J, Hutka M, et al. Central venous access in oncology: ESMO clinical practice guidelines. Ann Oncol. 2015;26:v152–v168.
- Zwicker JI, Connolly G, Carrier M, et al. Catheter-associated deep vein thrombosis of the upper extremity in cancer patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2014;12(5):796–800.
- Davies GA, Lazo-Langner A, Gandara E, et al. A prospective study of rivaroxaban for central venous catheter associated upper extremity deep vein thrombosis in cancer patients (catheter 2). Thromb Res. 2018;162:88–92.
- Ross JA, Miller MM, Rojas Hernandez CM. Comparative effectiveness and safety of direct oral anticoagulants (DOACs) versus conventional anticoagulation for the treatment of cancer-related venous thromboembolism: a retrospective analysis. Thromb Res. 2017;150:86–89.
- Peixoto de Miranda ÉJF, Takahashi T, Iwamoto F, et al. Drug–drug interactions of 257 antineoplastic and supportive care agents with 7 anticoagulants: a comprehensive review of interactions and mechanisms. Clin Appl Thromb Hemost. 2020;26:1076029620936325.
- Verso M, Munoz A, Bauersachs R, et al. Effects of concomitant administration of anticancer agents and apixaban or dalteparin on recurrence and bleeding in patients with cancer-associated venous thromboembolism. Eur J Cancer. 2021;148:371–381.
- Beavers CJ, Rodgers JE, Bagnola AJ, American Heart Association Clinical Pharmacology Committee and Cardio-Oncology Committee of the Council on Clinical Cardiology and Council on Genomic and Precision Medicine; and the Council on Peripheral Vascular Disease, et al. Cardio-Oncology drug interactions: a scientific statement from the American heart association. Circulation. 2022;145(15):e811–e838.
- Valeriani E, Porreca E, Weitz JI, et al. Impact of concomitant antiplatelet therapy on the efficacy and safety of direct oral anticoagulants for acute venous thromboembolism: systematic review and meta-analysis. J Thromb Haemost. 2020;18(7):1661–1671.
- Hutchinson A, Rees S, Young A, et al. Oral anticoagulation is preferable to injected, but only if it is safe and effective: an interview study of patient and carer experience of oral and injected anticoagulant therapy for cancer-associated thrombosis in the select-d trial. Palliat Med. 2019;33(5):510–517.
- Toorop MMA, van Rein N, Nierman MC, et al. Switching from vitamin K antagonists to direct oral anticoagulants: treatment satisfaction and patient concerns. J Thromb Haemost. 2020;18(6):1390–1397.
- Cohen AT, Maraveyas A, Beyer-Westendorf J, COSIMO Investigators, et al. Patient-reported outcomes associated with changing to rivaroxaban for the treatment of cancer-associated venous thromboembolism – the COSIMO study. Thromb Res. 2021;206:1–4.
- Cohen AT, Keshishian A, Lee T, et al. Effectiveness and safety of apixaban, LMWH, and warfarin among high-risk subgroups of VTE patients with active cancer. Curr Med Res Opin. 2021;:1–16. DOI:10.1080/03007995.2021.1932448
- Desai R, Koipallil GK, Thomas N, et al. Efficacy and safety of direct oral anticoagulants for secondary prevention of cancer associated thrombosis: a meta-analysis of randomized controlled trials. Sci Rep. 2020;10(1):18945.
- Barbosa CD, Balp MM, Kulich K, et al. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
- Noble S. Venous thromboembolism and palliative care. Clin Med. 2019;19(4):315–318.
- Becattini C, Bauersachs R, Maraziti G, et al. Renal function and clinical outcome of patients with cancer-associated venous thromboembolism randomized to receive apixaban or dalteparin. Results from the Caravaggio trial. haematol. 2021;107(7):1567–1576.
- Weber J, Olyaei A, Shatzel J. The efficacy and safety of direct oral anticoagulants in patients with chronic renal insufficiency: a review of the literature. Eur J Haematol. 2019;102(4):312–318.
- European Medicines Agency (EMA). Eliquis 2.5mg film-coated tablets - summary of product characteristics (SmPC); 2022. Available from: https://www.ema.europa.eu/en/documents/product-information/eliquis-epar-product-information_en.pdf.
- Sun L, Yin H, Liu M, et al. Impaired albumin function: a novel potential indicator for liver function damage? Ann Med. 2019;51(7–8):333–344.
- Riess H, Ay C, Bauersachs R, et al. Use of direct oral anticoagulants in patients with cancer: practical considerations for the management of patients with nausea or vomiting. Oncologist. 2018;23(7):822–839.
- Puhr HC, Ilhan-Mutlu A, Preusser M, et al. Absorption of direct oral anticoagulants in cancer patients after gastrectomy. Pharmaceutics. 2022;14(3):662.
- Dunois C. Laboratory monitoring of direct oral anticoagulants (DOACs). Biomedicines. 2021;9(5):445.
- Martin KA, Beyer-Westendorf J, Davidson BL, et al. Use of direct oral anticoagulants in patients with obesity for treatment and prevention of venous thromboembolism: updated communication from the ISTH SSC subcommittee on control of anticoagulation. J Thromb Haemost. 2021;19(8):1874–1882.
- Martin AC, Thomas W, Mahir Z, et al. Direct oral anticoagulant concentrations in obese and high body weight patients: a cohort study. Thromb Haemost. 2021;121(2):224–233.
- Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. New Eng J Med. 2013;369(15):1406–1415.
- Bravo Villa V, Romero J, Rojas-Zaldivar E, et al. Apixaban in low-weight patients with cancer-associated thrombosis: a cross sectional study of drug levels. Res Pract Thromb Haemost. 2021;5(3):421–425.
- Thomas S, Makris M. The reversal of anticoagulation in clinical practice. Clin Med. 2018;18(4):314–319.
- Samuelson Bannow BT, Lee A, Khorana AA, et al. Management of cancer-associated thrombosis in patients with thrombocytopenia: guidance from the SSC of the ISTH. J Thromb Haemost. 2018;16(6):1246–1249.
- Makris M, Van Veen JJ, Tait CR, British Committee for Standards in Haematology, et al. Guideline on the management of bleeding in patients on antithrombotic agents. Br J Haematol. 2013;160(1):35–46.
- Moik F, Posch F, Zielinski C, et al. Direct oral anticoagulants compared to low-molecular-weight heparin for the treatment of cancer-associated thrombosis: updated systematic review and meta-analysis of randomized controlled trials. Res Pract Thromb Haemost. 2020;4(4):550–561.
- Alpert N, Rapp JL, Marcellino B, et al. Clinical course of cancer patients with COVID-19: a retrospective cohort study. JNCI Cancer Spectr. 2021;5(1):Pkaa085.
- Brenner B, Ay C, Gal GL, et al. Venous thromboembolism risk, prophylaxis and management in cancer patients with COVID-19: an unmet medical need. Thrombosis Update. 2022;6:100098.
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing COVID-19 [NG191]; 2022. Available from: https://www.nice.org.uk/guidance/ng191.
- Schulman S, Sholzberg M, Spyropoulos AC, International Society on Thrombosis and Haemostasis, et al. ISTH guidelines for antithrombotic treatment in COVID-19. J Thromb Haemost. 2022;20(10):2214–2225.
- Radboud UMC and University of Liverpool. Liverpool COVID-19 drug interactions; 2022. Available from: https://covid19-druginteractions.org/about.