Abstract
Objective
Guidelines developed by the American College of Cardiology/American Heart Association (ACC/AHA) recommend lipid-lowering therapies (LLTs) to reduce low-density lipoprotein cholesterol (LDL-C) and atherosclerotic cardiovascular disease (ASCVD) risk. This study described LLT utilization patterns and LDL-C goal achievement (to <70 mg/dL) among patients with ASCVD in the United States.
Methods
This retrospective study was conducted using Optum’s de-identified Clinformatics Data Mart Database (CDM). Patients with their first ASCVD diagnosis (index date) in the CDM database between July 1, 2015, and December 31, 2018, were followed for ≥12 months to assess LLT utilization patterns and change in LDL-C. LLTs included were statins and non-statin LLTs (ezetimibe, fibrates, and proprotein convertase subtilisin/kexin type 9 inhibitors). Adherence was measured as the proportion of days covered (PDC), defined as the number of days with drug on-hand (or number of days exposed to drug) divided by the 12-month follow-up period. Patients with PDC ≥0.8 were considered adherent.
Results
Among the patients with ASCVD (N = 1,424,893) included in this study, only 621,978 (43.7%) had at least one LDL-C measurement at baseline (6 months prior to and 3 months after the index date). The mean age was 71.5 years, and almost half of the patients were female. Patients were followed for a mean (standard deviation [SD]) duration of 30.6 (11.4) months (median of 29.9 months). During the follow-up, about one-quarter of the patients did not receive any LLT. Among treated patients, 89.5% received statins and 10.5% received non-statin LLT. Less than half (47.6%) of the patients were adherent to the index treatment during the 12-month follow-up. Even in patients receiving combination therapy (statin + non-statin LLT), a sizable proportion (35.8%) showed an increase in LDL-C over the follow-up period.
Conclusions
This retrospective study highlighted limited LDL-C monitoring in patients with ASCVD, and unmet need in terms of suboptimal utilization of non-stain LLTs, limited adherence to LLTs, and inadequate lipid control after treatment (among those with LDL-C measurements during the follow-up period) need to be addressed to improve outcomes in this patient cohort.
PLAIN LANGUAGE SUMMARY
International societies of cardiologists recommend use of medications to lower the “bad” cholesterol, and its risk of cardiovascular diseases like stroke. We aimed to describe how those medications are being used and to what extent patients with cardiovascular diseases in the United States have their “bad” cholesterol under control. Results of this study indicate that cholesterol check-up among the patients was limited. Among recommended medications, statins were mostly used, whereas use of other recently approved medications was minimal. One-quarter of patients were not prescribed medications to control their cholesterol. Moreover, patients were not taking the medications as frequently as prescribed.
Introduction
High levels of low-density lipoprotein cholesterol (LDL-C) are strongly associated with an increased risk of cardiovascular disease (CVD) and coronary heart diseaseCitation1. Elevated LDL-C levels accounted for 4.4 million deaths worldwide, as reported in the 2019 global burden studyCitation2. About one-third of the adult American population have elevated LDL-C levels (≥130 mg/dL). In the United States (US), hyperlipidemia accounted for an estimated healthcare spending of $26.4 billion in 2016Citation2. Approximately 80% of the patients with atherosclerotic cardiovascular disease (ASCVD) and treated with statins did not meet the LDL-C goal in the USCitation3. Reduction in LDL-C using lipid-lowering therapies (LLT) reduces ASCVD mortality and morbidity. A meta-analysis of 28 statin trials showed a 21% reduction in major coronary events, coronary revascularization, and stroke for every 1 mmol/L reduction in LDL-C levelsCitation4, whereas another meta-analysis of 49 trials including both statin and non-statin therapies demonstrated a 23% reduction in the risk of major vascular events with 1 mmol/L reduction in LDL-C levelsCitation5. A more recent meta-analysis of 19 trials including statins, ezetimibe, and proprotein subtilisin/kexin type 9 inhibitors (PCSK9i) demonstrated a 19% reduction in major vascular outcomes associated with 1 mmol/L reduction in LDL-C levelsCitation6. A strong association between lowering LDL-C and lower risk of ASCVD has also been reported by the European Atherosclerosis Society Consensus PanelCitation7.
Guidelines developed by professional societies, including the American College of Cardiology/American Heart Association (ACC/AHA), recommend lipid management to reduce the risk of ASCVD eventsCitation8,Citation9. Furthermore, a greater absolute reduction in LDL-C levels in patients with ASCVD may lead to greater CV risk reduction. The American guidelines suggest the use of maximally tolerated statins to lower LDL-C levels in patients with ASCVD, to which ezetimibe and, if needed, a proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) can be added to achieve lipid goalsCitation8. The focused update of the Expert Consensus Decision Pathway on the role of non-statin therapies for LDL-C lowering in the management of ASCVD risk recommends a threshold of 70 mg/dL for all patients with clinical ASCVD who are on statins and with baseline LDL-C of 70–189 mg/dLCitation9.
Study rationale
In the US, awareness of high cholesterol levels has increased from 51.5% to 67.7% in patients with a history of ASCVD over the period of 2005–2006 to 2015–2016Citation2. However, real-world studies have reported inadequate LDL-C control and poor adherence to clinical guidelines for the management of lipid levelsCitation10–12. Understanding the current trends in clinical practice, utilization patterns of LLT, and lipid target levels achieved with various LLT will facilitate and further clarify the need for therapy escalation in this patient population.
This real-world study aimed to describe the current patients’ characteristics, treatment patterns, and achievement of LDL-C targets in patients with ASCVD with hypercholesterolemia in the US. The study stratified the patient population by LDL-C levels and explored the adherence, persistence, treatment switching, and discontinuations associated with different LLT.
Methods
Study design
This was a retrospective, non-interventional study using Optum’s de-identified Clinformatics Data Mart (CDM) Database. Patients were identified during the identification period from July 1, 2015, to December 31, 2018, and the overall study period was from January 1, 2015, to December 31, 2019. At the time of study protocol development and database analysis, the most recent CDM data available was up to December 31, 2019. The index date was defined as the first ASCVD encounter during the identification period.
This study used de-identifiable, anonymous data from the CDM and was designed in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for PharmacoepidemiologyCitation13, Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelinesCitation14, and with the ethical principles laid down in the Declaration of Helsinki. As this study was based on de-identified administrative claims data, it was exempted from Institutional Review Board approval.
Data source
The CDM enables integration and linking of patient level data from a variety of real world sourcesCitation15. It contains de-identified administrative claims data (including inpatient and outpatient medical claims, pharmacy claims, and laboratory results) from enrollees of commercial insurance and Medicare Advantage (C and D) plan in the US and is geographically diverse across all 50 states, thus providing a sample representative of the populationCitation16. Medicare Advantage is offered by private health insurance companies, which is known as Part C and usually also includes Part DCitation17.
Study population
Patients who had at least one ASCVD encounter (defined by the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]/International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] diagnosis) and hypercholesterolemia (defined by ICD-9-CM/ICD-10-CM diagnosis), prescribed with at least one LLT, or with a test result of LDL-C ≥70 mg/dL (any time prior to or 3 months after the index date) were included. LLTs included were statins and non-statin LLTs (ezetimibe, fibrates, and PCSK9i). Patients were required to have continuous enrollment (no allowance of gaps) 6 months prior to the index date (pre-index) to capture LDL-C qualifying data and additional baseline variables. A 12-month continuous post-index period was also required for the patient profile and treatment patterns analysis. Patients with missing patient ID, missing year of birth, and missing gender in the database were excluded from the study.
Study measures
The key measures extracted from the CDM to describe the profile of patients with ASCVD with hypercholesterolemia were demographics and clinical characteristics (including the earliest reported CVD, comorbidities, and LDL-C values). These characteristics were assessed during the 6-month pre-index period, unless otherwise specified. Chronic comorbidities were assessed at any time prior to the index period (not limited to the pre-index period). Other key outcomes assessed were treatment patterns such as adherence, persistence, treatment switching, and LLT discontinuations during the follow-up period among patients who were prescribed LLTs. All outcome measures were stratified according to the LDL-C levels of patients measured 6 months pre-index to 3 months after the index date: patients with LDL-C ≥70 mg/dL and those with LDL-C <70 mg/dL.
Index treatment was defined as the first LLT after the earliest ASCVD diagnosis. About 60% of the patients included in the study cohort received LLT at baseline prior to the first ASCVD diagnosis, where predominantly statins were used. Adherence to index treatment(s) was measured as the proportion of days covered (PDC). PDC is calculated for oral treatments as the number of days with drug on-hand (or number of days exposed to drug) divided by the number of days in the specified time interval (12-month follow-up period for this study), regardless of index treatment discontinuation. And, for injectables, PDC was measured as the number of distinct days with treatment in the follow-up period divided by the number of days in the follow-up period. Patients with PDC ≥0.8 were considered adherent. Treatment switching was defined as initiation of new LLT after the index treatment(s) with an overlap of <60 days after the last day of supply of index treatment(s). Combination or add-on therapy occurred when an additional LLT was initiated within 60 days after the previous LLT. Persistence was defined as the duration from the initiation to discontinuation of the initial LLT allowing a maximum of 60-day gapCitation18. Time to discontinuation was defined as a gap of therapy of 60 days with the index treatment, initiation of a new treatment, or the end of the study period, selected based on the earliest occurrence. To assess patients achieving the LDL-C goal of <70 mg/dL over the 12-month follow-up, LDL-C measurements at any time from 3 months after the index date up to the 12-month post-index period were considered. LDL-C measurements closest to the initial treatment within 6 months before and at least 3 months after the index treatment were used to assess change in LDL-C over treatment and the proportion of patients achieving the LDL-C goal <70 mg/dL after starting index treatment.
Treatment utilization pattern endpoints (adherence, persistence, and therapy modification) were assessed by LDL-C level subgroups (LDL-C <70 mg/dL or ≥70 mg/dL). Change in LDL-C and time to treatment discontinuation endpoints were further evaluated by therapeutic class subgroups.
Statistical analysis
All planned analyses were descriptive, with no adjusted analyses performed to compare patient groups. Continuous variables were summarized using mean and standard deviation (SD), and categorical variables were presented as frequency counts and percentages. Missing data were considered a separate category in all analyses and described using frequency counts and percentages. The analyses were conducted using Statistical Analysis Software (SAS studio 3.81 [SAS Institute, Cary, NC] and R studio 2021.09.1 [PBC, Boston, MA]).
Results
A total of 1,424,893 patients with ASCVD and hypercholesterolemia who were continuously enrolled in the insurance plans during the 6-month pre-index and over 12-month follow-up period were eligible and included in the study ().
Table 1. Patient flow with inclusion criteria.
Patient characteristics
The mean (SD) age of the patients at the index date was 71.5 (10.7) years; 49.9% of patients were female, and the majority had Medicare Advantage insurance (80.7%) (). About one-third of the patients were from the South-East region of the US. The most common index ASCVD diagnosis was coronary artery disease (51.5%), followed by peripheral arterial disease (42.7%) and cerebrovascular disease (11.3%). Only 43.7% of patients had LDL-C measurement at baseline, with a mean (SD) of 95.9 (35.5) mg/dL. The most common comorbidity in the cohort was hypertension (76.9%), followed by diabetes mellitus (38.4%) and depression/mental disorder (34.0%).
Table 2. Baseline demographic and clinical characteristics in the overall cohort and subgroups stratified by baseline LDL-C level.
The study cohort was stratified by LDL-C levels (LDL-C ≥70 mg/dL or <70 mg/dL) measured at baseline (nearest measure to the index date). Among patients with LDL-C ≥70 mg/dL, 54.5% were female, whereas among those with LDL-C <70 mg/dL, about 41.6% were female. Hypertension, diabetes mellitus, depression/mental disorder, and mixed dyslipidemia were the most common comorbidities in the patient subgroups stratified by LDL-C levels.
Subgroup: payer type
Similar outcomes were observed in the cohorts stratified by payer subtype. A direct comparison between the same LDL-C cohorts across payers was not suitable as the age of the population varied considerably. Also, the distribution by sex was different, 54% in the Medicare Advantage group and 39.8% in the commercial insured group were female. Coronary artery disease (58.2%) was the most common index ASCVD event in commercially insured patients, whereas peripheral arterial disease (51.8%) was the most common in the Medicare Advantage group. Patients with Medicare Advantage insurance had higher occurrence of comorbidities, such as atrial fibrillation, chronic kidney disease, and diabetes mellitus ().
Table 3. Baseline demographic and clinical characteristics by payer subtype.*
Treatment patterns
Over the 12-month follow-up, the most commonly prescribed index treatment was statin monotherapy (). Statin intensity was calculated for statin prescription claims with non-missing strength and dose information. About 59.7% of the patients were prescribed high-intensity statins (59.6% in the LDL-C <70 mg/dL group and 62.2% in the LDL-C ≥70 mg/dL group). About 66.5% of patients in the LDL-C ≥70 mg/dL group and almost 75% in the LDL-C <70 mg/dL group were prescribed atorvastatin or simvastatin. The use of LLT monotherapy other than statins was minimal, with fibrates being the second most prescribed class, followed by ezetimibe. Almost one-quarter of the patients in the overall cohort were not treated with any LLT (10.3% in the LDL-C <70 mg/dL and 38.5% in the LDL-C ≥70 mg/dL group).
Table 4. Treatment patterns of index therapies during the 12-month follow-up in the overall cohort, stratified by baseline LDL-C levels.
Treatment compliance
Less than half (47.6%) of the patients were adherent to the index treatment in the overall cohort and the mean (SD) time to discontinuation was 289 (115) days, measured until the end of the study period (median = 29.9 months ()). Among all drug classes, index statin monotherapy was associated with the highest adherence, at 63.7%. During the 12-month follow-up, 20.8% of the 667 patients treated with PCSK9i drug class were adherent. Relatively low mean adherence of 0.50 (0.29) during the 12-month follow-up and mean persistence of 184 (119) days were observed among patients treated with PCSK9i ().
Table 5. Adherence and persistence measures for the overall cohort, stratified by baseline LDL-C levels.
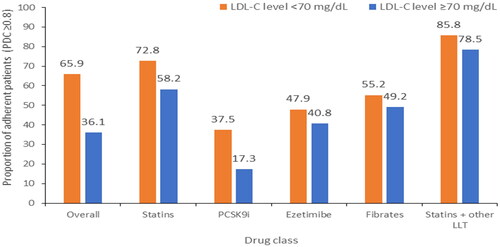
Two-thirds of patients with baseline LDL-C <70 mg/dL were adherent to treatment (65.9%) compared with around one-third of those with baseline LDL-C ≥70 mg/dL (36.1%) (). About 40% of patients in the baseline LDL-C ≥70 mg/dL group and 30.4% in the baseline LDL-C <70 mg/dL group discontinued the index treatment during the 12-month follow-up period. Similar to the overall cohort, the majority of patients (72.8%) on statin-based index treatments (either monotherapy or combination therapy) in the baseline LDL-C <70 mg/dL group were adherent, whereas 58% in the baseline LDL-C ≥70 mg/dL group were adherent (). Among the patients prescribed statin-based index treatments, 40% in the baseline LDL-C ≥70 mg/dL group and 31% in the baseline LDL-C <70 mg/dL group discontinued index treatment. For those prescribed PCSK9i as index treatments, about 49.8% in the baseline LDL-C ≥70 mg/dL group and 45% in the baseline LDL-C <70 mg/dL group discontinued index treatment during the 12-month follow-up period.
Treatment modification
Patients with available LDL-C measurements and index treatment within 1 year after the index date were included in the analysis (patients with LDL-C ≥70 mg/dL [n = 293,894]; patients with LDL-C <70 mg/dL [n = 129,505]) for treatment modification. In the cohorts stratified by LDL-C levels, about 90% of patients were initiated on statins as first-line treatment (). Statins are the most widely prescribed drugs across all the three lines of treatment. Of patients who initiated first-line treatment, 13.4% in the baseline LDL-C <70 mg/dL group and 17.4% in the baseline LDL-C ≥70 mg/dL group progressed to second-line treatment. A very low proportion of patients were initiated on drug classes (PCSK9i, ezetimibe, fibrates) other than statins as second-line treatment in the LDL-C ≥70 mg/dL (1.0%) and <70 mg/dL (0.5%) groups, respectively. Similarly, for third-line treatment, the proportions were 0.3% and 0.1%, respectively. Supplementary Figure S1 presents data on the switch of patients from the first line to the third line.
Table 6. Treatment modification from the index (first-line) to the third-line treatment within 12-month after the index date.*
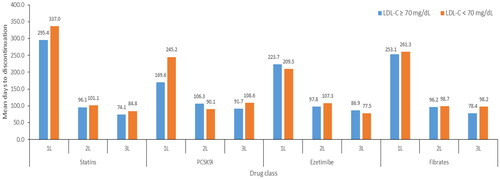
Treatment discontinuation
The mean number of days to treatment discontinuation across various lines is shown in . Regardless of the LDL-C levels of patients, persistence to treatment was similar. For all treatments initiated as first-line, the mean (SD) days to discontinuation was 295.6 (137.2) in the LDL-C ≥70 mg/dL group and 338.2 (115.0) in the LDL-C <70 mg/dL group. The mean (SD) number of days to discontinuation for second-line treatment was 100.0 (69.3) and 78.2 (64.0) and that for third-line treatment was 105.7 (70.5) and 86.5 (65.9) in the baseline LDL-C ≥70 mg/dL and <70 mg/dL groups, respectively. For patients with baseline LDL-C ≥70 mg/dL, 40% receiving first-line, 35.5% receiving second-line, and 30.1% receiving third-line treatment discontinued treatment, whereas among patients with baseline LDL-C <70 mg/dL, 30.4% receiving first-line, 29.5% receiving second-line, and 27.2% receiving third-line treatment discontinued treatment during the 12-month follow-up.
Goal attainment
The majority of the patients treated with LLT remained above the LDL-C target (<70 mg/dL) during the 12-month follow-up period; thus, more intense therapies are warranted for attaining LDL-C target in this patient population. Only 20.4% of the patients with baseline LDL-C ≥70 mg/dL, with 1 year of continuous enrollment and at least two LDL-C measurements before and after the index treatment (N = 159,630, including patients who received second-line therapy, no further lines of therapy, or those who discontinued treatment after index therapy), were at the target LDL-C level (<70 mg/dL) after the index treatment. The proportion of patients in the overall group who achieved the target LDL-C level (<70 mg/dL) increased from 20.4% after the index date, to 28.3% over the 12-month of follow-up. Among patients those were prescribed statins (N = 140,534), statins + other LLTs (N = 10,107), PCSK9i (N = 199), fibrates (N = 4,540), and ezetimibe (N = 2,331) as index therapies, 28.5%, 34.6%, 47.2%, 18.5%, and 11.9% achieved the target LDL-C level (<70 mg/dL) over the 12-month of follow-up, respectively. About one-third of the patients who continued the index first-line treatment over the 12-month follow-up were at the target LDL-C level compared with only 19.7% of those who discontinued the first-line treatment and received no further treatment.
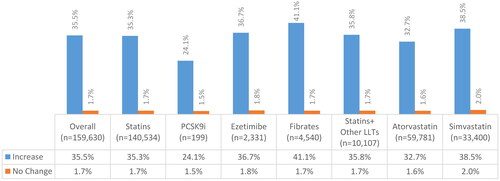
The percentage change in LDL-C levels was calculated for patients with baseline LDL-C ≥70 mg/dL. Despite being prescribed treatment, 35.5% of patients showed an increase in LDL-C levels (). Even in patients using combination therapy (statin + any non-statin LLT), a sizable proportion (35.8%) had increased LDL-C levels over the follow-up period.
Figure 3. Proportion of patients with increase or no change in LDL-C levels over the 12-month follow-up across drug classes.
Abbreviations: LDL-C, low-density lipoprotein cholesterol; LLT, lipid-lowering therapy; PCSK9i, proprotein convertase subtilisin/kexin type 9 inhibitors.
* LDL-C measurements closest to the index treatment (1) within 6 months before and (2) at least 3 months after the index treatment were used to calculate the change in LDL-C levels.
Discussion
In the overall ASCVD cohort in our study, the mean age of the population was 71.5 years, and the gender distribution was almost equal. Utilization of LLT including statins, ezetimibe, PCSK9i, and/or their combinations has also been evaluated in the elderly population in real world studies with a mean age ≥65 years in the study cohortsCitation19,Citation20. Median (interquartile range) reported for LDL-C levels in patients with ASCVD in the study by Cannon et al.Citation19 (91 mg/dL [78, 113]) are similar to our results (91 mg/dL [71, 116]). One US-based studyCitation21, using the Truven MarketScan Research Database, estimated that 74.2% of the patients with ASCVD had LDL-C ≥70 mg/dL, which is similar to our cohort’s findings (76.8%). We found that a higher proportion of females had LDL-C ≥70 mg/dL (about 1.3–1.6-times) across the cohorts. In contemporary studies evaluating LLT use in patients with ASCVDCitation12,Citation19,Citation21,Citation22, the mean age of the population was lower (63–68 years) than that of our study population, which had a higher number of patients in the Medicare Advantage plan; gender distribution was similar between the two studies (43–49%).
This large retrospective cohort study of patients with ASCVD in the US highlighted that less than half of the patients had LDL-C measurements. About one-quarter of the patients were not prescribed LLT, whereas less than half of the treated patients were adherent (PDC ≥0.8) during the 12-month follow-up period. As highlighted in the recently published 2018 ACC/AHA guidelines, initiation or continuation of statin therapy to achieve LDL-C reduction ≥50% is recommended for subsequent risk reduction in patientsCitation8. Increased LDL-C measurement will encourage assessment of the risk profile of the patients and, thus, may result in optimal management of the disease according to recent guidelines.
In our study, about one-quarter of the patients with ASCVD were not prescribed any LLT. Similar results were reported in a UK-based studyCitation23, where, among patients with a high risk of ASCVD followed up for 2 years in intervals of 6 months, 36–37% were not prescribed any LLT at all time pointsCitation23. Another study based on US MarketScan dataCitation24 reported that 40% of patients with ASCVD were not on LLT over a 2-year follow-up. In line with the 2018 ACC/AHA guidelines, the most prescribed drug class in our overall ASCVD cohort was statins. A study by Yao et al.Citation12 on the temporal trends of statin use by analysis of OptumLab Data Warehouse reported an increase in statin use (within 30 days from discharge) for the overall ASCVD cohort from 2007 to 2016. Compared with our study, statin use (66.4%) was similar in the overall ASCVD cohort (59.9% in 2016) in their study.
In our study, patients were stratified by LDL-C levels considering the cutoff level of 70 mg/dL. As 76.8% of the patients had LDL-C levels higher than the recommended target of 70 mg/dL, it highlights the need for treatments to control LDL-C levels in patients with ASCVD. Of these patients, about 40% were not on any LLT compared with only 10% of those in the LDL-C <70 mg/dL group. Similarly in a study by De Backer et al.Citation25 about 71.0% of the patients had elevated LDL-C levels (≥70 mg/dL) in a European survey of patients with coronary heart disease across 27 countries over a median follow-up of 1.12 years. In a US-based study using MarketScan data to analyze patients with ASCVD with LDL-C ≥70 mg/dL, 50.3% were not on LLTCitation24. This indicates a gap in the treatment of patients with ASCVD who have LDL-C levels above the recommended threshold.
Treatment distribution of the patient groups stratified by LDL-C levels was similar to that of the overall cohort. A higher proportion of patients were on statins in both subgroups, where the LDL-C <70 mg/dL group had more patients on statins (1.5-times) than the LDL-C ≥70 mg/dL group over the 12-month follow-up. Similar results were observed in a US-based studyCitation21 analyzing statin use (either monotherapy or with ezetimibe) in an ASCVD population stratified by LDL-C levels with a cutoff of 70 mg/dL. Guidelines recommend the addition of non-statin therapy for patients with ASCVD with LDL-C ≥70 mg/dL when the maximum tolerated dose for statin is dispensedCitation8. However, in our study, patients in groups stratified by LDL-C levels had similar proportions of LLT use other than statins (approximately 8%), demonstrating a lack of escalation of therapy.
Overall, <50% of patients were adherent (PDC ≥0.8) to the index treatment over the 12-month follow-up period. Measures for adherence and persistence were the highest for statins across all classes of drugs in all cohorts studied. Adherence measures were the lowest for PCSK9i, and discontinuation (%) was the most for ezetimibe, fibrates, and PCSK9i classes of drugs. Similar findings were noted in the study by Yao et al.Citation12, in which 70.5% of patients were adherent to statins. Discontinuation rates observed for PCSK9i in our cohort were similar to those reported in other US based studies (42.6–63.0%)Citation20,Citation26,Citation27 over a follow-up of 6–12 months. For statins only- and ezetimibe only-users, the discontinuation rates were 35.0% and 30.2%, respectively, in a claims-based study in the US over a follow-up period of 6 monthsCitation20. Contrary to our findings, about half of the patients using PCSK9i in a US based claims study were reported to be adherent. However, this study followed patients only until 6 monthsCitation20. In our study the populations using ezetimibe, fibrates, and PCSK9i were small which may limit the generalizability of the adherence and discontinuation results among the elderly US population. Of note is the considerably higher adherence (PDC ≥0.8) in patients with LDL-C <70 mg/dL than in those with LDL-C ≥70 mg/dL (0.84 vs 0.75), implying that patients adherent to treatment are able to achieve the target LDL-C levelCitation19.
The mean time to discontinuation of the index treatments was similar across the LDL-C groups analyzed. Patients had a longer treatment duration while using first-line treatment compared with other treatments. Patients with LDL-C ≥70 mg/dL discontinued first-line treatment in less time (mean = 295.6 days) than those with LDL-C <70 mg/dL (mean = 338.2 days). About 40% of patients in the baseline LDL-C ≥70 mg/dL group and 30.4% in the baseline LDL-C <70 mg/dL group discontinued their first-line index treatments.
About two-third of the patients with ASCVD with LDL-C ≥70 mg/dL did not achieve the LDL-C goal even after continuing index treatment over the 12-month of follow-up across all drug classes. These results were also reported in a real-world analysis of patients with ASCVD in the US using the GOULD registryCitation19, in which, over a 2-year follow-up, 21% of the patients with LDL-C ≥100 mg/dL and 33.9% of those with LDL-C = 70–99 mg/dL achieved a goal of LDL-C <70 mg/dLCitation19. In a study by Cannon et al.Citation19, 52.4% of patients on PCSK9i achieved the target LDL-C goal over 2 yearsCitation19, whereas, in our study, 47.2% achieved the same goal. However, only 0.1% of the total patients with LDL-C ≥70 mg/dL were prescribed PCSK9i. Our study results contrast with the European study (EUROASPIRE V) by De Backer et al.Citation25 where over half of the patients achieved target LDL-C goal. The EUROASPIRE V survey study was based on primary data collection, via web-based questionnaire and interview, whereas our study was based on secondary administrative claims data; thus may have contributed to differences in the study findings. Moreover, the study by De Backer et al. also highlighted that the baseline LDL-C levels were unknown in the large majority of the study cohort, therefore limiting the possibility of assessment of change in LDL-C levels after treatment.
In our study, 35.5% of patients who were prescribed LLT had an increase in the LDL-C level over follow-up, highlighting the lack of adequate lipid control with the existing treatments. Even in patients using combination therapy (statin + any drugs), a sizable proportion (35.8%) had an increase in LDL-C level over follow-up.
Few limitations that can be identified for the study come from the administrative nature of the data source and their use in observational research. The possibility of encountering incomplete follow-up data is acknowledged as patients who did not use facilities covered under the integrated data network captured using CDM would not be recorded in the database. Possible coding errors, coding for the purpose of rule-out rather than actual disease, and under-coding, without the possibility of verifying reported diagnoses, may affect the analysis. The diagnoses and data recorded may be inaccurate or subject to human or technical error. Medication use may be overestimated as the prescription of a drug was used as a proxy for use. In our study, the population using ezetimibe, fibrates, and PCSK9 inhibitors were small and may limit generalizability of the adherence and discontinuation results among the elderly US population.
Conclusion
The study highlights the low LDL-C testing rate in the ASCVD population, with about 56.4% of patients with ASCVD without LDL-C testing in a period of 9 months. Treatment options that might reduce LDL-C levels and associated CV risk are essential to improve outcomes in this population. However, the use of LLTs other than statins (e.g. ezetimibe, PCSK9i) was minimal in the study cohort, and less than half of the patients were adherent to their index LLTs during the 12-month follow-up period. Even with substantial (63.7%) adherence, over 36% of the patients in the statin monotherapy group had either no change or increase in LDL-C during the 12-month follow-up period. Moreover, less than one-third of the patients achieved the LDL-C target level (<70 mg/dL) during the 12-months of follow-up. This study highlighted unmet need in terms of suboptimal utilization of non-stain LLTs, high discontinuation rates, and poor adherence to LLTs. A sizable proportion (35.8%) of patients experienced an increase in LDL-C levels, thereby indicating a lack of adequate lipid control post-treatment, which needs to be addressed to improve outcomes in this patient cohort. Quality metrics in healthcare service provision could be designed to address the unmet need observed in patients with ASCVD, including patient education on the importance of adherence and persistence to LLTs, and raise awareness to the healthcare providers on the current poor lipid measurement and management of patients with hypercholesterolemia.
Transparency
Declaration of funding
The study was funded by Novartis Pharma AG, Basel. Novartis was involved in all stages of this study including the protocol to submission of the manuscript.
Declaration of financial/other relationships
R. Lahoz, D. Seshagiri, A. Achouba, and R. Studer are employees of Novartis Pharma AG, Basel. R. Lahoz and R. Studer are also shareholders of Novartis. At the time of the conduct of the study, J. Cristino was an employee of Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. B. Electricwala is an employee of Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. Y. Ding is an employee of Genesis Research, USA. J.-H. Heo was an employee of Genesis Research, USA. Y. Ding and J.-H. Heo received consulting fees from Novartis Pharma AG, Basel. A reviewer on this article has disclosed that they have received consultancy fees from Amgen and Novartis. Peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Author contributions
R. Lahoz, D. Seshagiri, B. Electricwala, A. Achouba, J. Cristino, R. Studer, Y. Ding, and J.-H. Heo contributed to the study design. R. Lahoz, Y. Ding, J.-H. and Heo contributed to the data analysis. All authors contributed to study results interpretation, drafting and revision of the manuscript, and provided final approval of the version submitted for publication.
Supplemental Material
Download MS Word (315 KB)Acknowledgements
Jahnavi Yenamandra, Amit Ahuja, and Debajyoti Bhowmik [all of whom were employees of Novartis Healthcare Private Limited, India at the time of the study] provided medical writing support.
Data availability statement
The data used for the analysis which support the findings of this study are available from CDM. Restrictions apply to the availability of these data, which were used under license for this study.
References
- Abdullah SM, Defina LF, Leonard D, et al. Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease. Circulation. 2018;138(21):2315–2325. doi: 10.1161/CIRCULATIONAHA.118.034273.
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950.
- Wong ND, Young D, Zhao Y, et al. Prevalence of the American College of Cardiology/American Heart Association statin eligibility groups, statin use, and low-density lipoprotein cholesterol control in US adults using the national health and Nutrition Examination Survey 2011–2012. J Clin Lipidol. 2016;10(5):1109–1118. doi: 10.1016/j.jacl.2016.06.011.
- Armitage J, Baigent C, Barnes E, et al. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–415. doi: 10.1016/S0140-6736(18)31942-1.
- Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–1297. doi: 10.1001/jama.2016.13985.
- Koskinas KC, Siontis GC, Piccolo R, et al. Effect of statins and non-statin LDL-lowering medications on cardiovascular outcomes in secondary prevention: a meta-analysis of randomized trials. Eur Heart J. 2018;39(14):1172–1180. doi: 10.1093/eurheartj/ehx566.
- Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–2472. doi: 10.1093/eurheartj/ehx144.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3168–3209. doi: 10.1016/j.jacc.2018.11.002.
- Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2017 focused update of the 2016 ACC Expert Consensus Decision Pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2017;70(14):1785–1822. doi: 10.1016/j.jacc.2017.07.745.
- Burke JP, Simpson RJ, Jr, Paoli CJ, et al. Longitudinal treatment patterns among US patients with atherosclerotic cardiovascular disease or familial hypercholesterolemia initiating lipid-lowering pharmacotherapy. J Clin Lipidol. 2016;10(6):1470–1480.e3. doi: 10.1016/j.jacl.2016.09.002.
- Marrett E, Zhao C, Zhang NJ, et al. Limitations of real-world treatment with atorvastatin monotherapy for lowering LDL-C in high-risk cardiovascular patients in the US. Vasc Health Risk Manag. 2014;10:237–246. doi: 10.2147/VHRM.S54886.
- Yao X, Shah ND, Gersh BJ, et al. Assessment of trends in statin therapy for secondary prevention of atherosclerotic cardiovascular disease in US adults from 2007 to 2016. JAMA Netw Open. 2020;3(11):e2025505. doi: 10.1001/jamanetworkopen.2020.25505.
- Public Policy Committee ISoP. Guidelines for good pharmacoepidemiology practice (GPP). Pharmacoepidemiol Drug Saf. 2016;25(1):2–10. doi: 10.1002/pds.3891.
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. doi: 10.1097/EDE.0b013e3181577511.
- Clinformatics®Data Mart USA: Optum; 2017 [cited 2021 Jun 24]. Available from: https://www.optum.com/content/dam/optum/resources/productSheets/Clinformatics_for_Data_Mart.pdf
- O’Byrne ML, DeCost G, Katcoff H, et al. Resource utilization in the first 2 years following operative correction for tetralogy of fallot: study using data from the Optum’s de-identified Clinformatics Data Mart Insurance Claims Database. J Am Heart Assoc. 2020;9(15):e016581.
- CMS. What’s a medicare advantage plan: CMS; 2015 [updated 2015 Apr]. Available from: https://www.medicare.gov/sites/default/files/2018-07/11474.pdf
- Booth JN, Colantonio LD, Chen L, et al. Statin discontinuation, reinitiation, and persistence patterns among medicare beneficiaries after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2017;10(10):e003626.
- Cannon CP, de Lemos JA, Rosenson RS, et al. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021;6(9):1–9.
- Hines DM, Rane P, Patel J, et al. Treatment patterns and patient characteristics among early initiators of PCSK9 inhibitors. Vasc Health Risk Manag. 2018;14:409–418. doi: 10.2147/VHRM.S180496.
- Klimchak AC, Patel MY, Iorga ŞR, et al. Lipid treatment and goal attainment characteristics among persons with atherosclerotic cardiovascular disease in the United States. Am J Prev Cardiol. 2020;1:100010. doi: 10.1016/j.ajpc.2020.100010.
- Cannon CP, Khan I, Klimchak AC, et al. Simulation of lipid-lowering therapy intensification in a population with atherosclerotic cardiovascular disease. JAMA Cardiol. 2017;2(9):959–966. doi: 10.1001/jamacardio.2017.2289.
- Nordstrom B, Collins J, Donaldson R, et al. Treatment patterns and lipid levels among patients with high-risk atherosclerotic CVD in the UK. Br J Cardiol. 2015;10(01):22.
- Gu J, Sanchez RJ, Chauhan A, et al. Lipid treatment status and goal attainment among patients with atherosclerotic cardiovascular disease in the United States: a 2019 update. Am J Prev Cardiol. 2022;10:100336. doi: 10.1016/j.ajpc.2022.100336.
- De Backer G, Jankowski P, Kotseva K, et al. Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis. 2019;285:135–146. doi: 10.1016/j.atherosclerosis.2019.03.014.
- Davis LE, Pogge EK. A retrospective chart review evaluating efficacy, tolerability, and cost of proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i) in older adults. High Blood Press Cardiovasc Prev. 2020;27(4):331–338. doi: 10.1007/s40292-020-00399-6.
- Donald DR, Reynolds VW, Hall N, et al. Exploring rates of PCSK9 inhibitor persistence and reasons for treatment non-persistence in an integrated specialty pharmacy model. J Clin Lipidol. 2022;16(3):315–324. doi: 10.1016/j.jacl.2022.03.004.