Abstract
Objectives
Ureteral injuries (UIs) during surgical procedures can have serious consequences for patients. Although UIs can result in substantial clinical burden, few studies report the impact of these injuries on payer reimbursement and patient cost-sharing. This retrospective study evaluated 30-day, 90-day, and 1-year healthcare resource utilization for patients with UIs and estimated patient and payer costs.
Methods
Patients aged ≥ 12 years who underwent abdominopelvic surgery from January 2016 to December 2018 were identified in a United States claims database. Patients were followed for 1 year to estimate all-cause healthcare visits and costs for patients and payers. Surgeries resulting in UIs within 30 days from the surgery date were matched to surgeries without UIs to estimate UI-attributable visits and costs.
Results
Five hundred and twenty-two patients with UIs were included. Almost a third (29.9%) of patients with UIs had outpatient surgery. Patients with UIs had slightly more healthcare visits and a 15.3% higher 30-day hospital readmission rate than patients without UIs. Patient costs due to UIs were not statistically significant, but annual payer costs attributable to UIs were $38,859 (95% CI = 28,142–49,576), largely driven by inpatient costs.
Conclusions
UIs add substantial cost for payers and result in more healthcare visits for patients. These findings highlight the importance of including inpatient and outpatient settings for UI prevention. Although UIs are rare, the associated patient and payer burdens are high; thus, protocols or techniques are needed to recognize and avert UIs as current guideline recommendations are lacking.
PLAIN LANGUAGE SUMMARY
Though not common, injuries to the ureters, which carry urine from the kidneys to the bladder, can occur during surgeries on the abdomen. Ureter injuries can lead to discomfort, pain, infection, and death. Patients with ureter injuries can also require additional care from doctors, leading to increased costs for both patients and insurance companies. The researchers in this study calculated the costs of ureter injuries at 30-days, 90-days, and 1-year after surgery using anonymous information from insurance claims from patients who received abdominal surgery.
Compared with patients who did not have a ureter injury from surgery, a higher percentage of those with ureter injuries had healthcare visits in the year following surgery and a greater chance of being readmitted to the hospital in the 30 days after surgery. Costs for both patients and insurance companies increased in the year after surgery. Insurance companies paid almost $39,000 more on average per patient with ureter injury in the year after surgery compared with costs for patients who did not have ureter injuries. Patients with ureter injuries paid approximately $1,000 more out-of-pocket in the year after surgery compared with patients without ureter injuries.
This study showed that ureter injuries increased costs for both patients and insurance companies. Patients with ureter injuries needed more healthcare and the insurance companies for those patients had higher financial costs. Though ureter injuries are uncommon, this study supports efforts to minimize their occurrence to prevent these impacts on patients and the healthcare system.
Introduction
The proximity of the ureters to important abdominal structures makes them susceptible to ureteral injuries (UIs) during surgical procedures; these injuries include inadvertent ligature, transection, or thermal injuries during abdominopelvic and gynecologic (GY) surgeryCitation1–3. UIs are relatively rare, occurring in < 1% of all GY and gastrointestinal (GI) surgeries, including colorectal surgeries, but they can cause substantial patient burdenCitation2–7. These injuries may lead to urinary leaks or fistula, sepsis, acute and permanent renal failure, wound dehiscence, urinomas, abscesses, and deathCitation2,Citation3, and substantially increase the risk of life-threatening complications within 1 year of surgeryCitation2. Patients who experience UIs may be unable to work, need non-prescription therapies, have physical and psychological discomfort, and incur other indirect costs that impact quality-of-lifeCitation3,Citation8.
Patients with UIs tend to accrue higher hospital charges, driven largely by longer lengths of stay. A study examining ureteral and bladder injuries in hysterectomy surgeries found that patients with an injury had higher hospital costs ($29,889 vs $15,808) than patients without injuryCitation4. Similarly, patients who experienced a UI during colorectal surgery had an additional $31,497 in-hospital charges versus patients with surgeries that did not result in a UICitation3. The literature is scant on the costs to other stakeholders, including reimbursement by payers and cost-sharing by patients, who bear costs for any care received. In addition, data are limited on UI occurrence in the outpatient surgery setting.
The objectives of this study were to use a United States (US) claims database to determine UI-attributable healthcare visits and estimate costs in the 30-day, 90-day, and 1-year time points in patients with UIs, compared to propensity score-matched patients without UIs. For patients with inpatient index surgeries, the 30-day readmission rate was estimated.
Methods
Data source and study population
This was a retrospective cohort analysis using a US claims database, PharMetrics® Plus, IQVIA. This database is a longitudinal health plan database of adjudicated medical and pharmacy claims from > 200 million enrollees.
Patients were included if they underwent a prespecified abdominopelvic surgery from January 2016 to December 2018, were aged ≥12 years at the time of surgery, and were continuously enrolled in a healthcare insurance plan for ≥6 months before the surgery date and ≥1 year after the surgery date, with a ≤1 month gap in coverage permitted. Eligible surgeries included all GI, GY, and other abdominopelvic surgeries that put the patient at risk of a UI. Both urologic and endoscopic surgeries were excluded. Surgeries were defined by current procedural terminology (CPT) and the International Classification of Diseases, 10th revision, Procedure Coding System (ICD-10-PCS) codes. UIs were defined by diagnosis codes or by procedure codes (Supplementary Table S1)Citation6,Citation9.
All surgeries with a UI were identified from the IQVIA database. The index date was defined as the date of surgery within 30 days prior to the earliest UI identification date. If multiple targeted surgeries were identified, the closest surgery to the UI identification date was selected as the index surgery. If multiple surgery dates and UI pairs were identified with the same interval, the index surgery was selected at random. Patients were excluded if they had a UI diagnosis during the pre-index surgery period, a prespecified ureteral diagnosis or procedures (e.g. ureteral stone) during the period between the surgery day and the UI identification date, or a UI identification date more than 30 days after the closest index surgery date. Other surgeries were classified in the non-UI cohort and used for matching.
Statistical analysis
Propensity scores for UIs were estimated with a logistic regression model with patient demographics (age, gender, region, payer plan, and comorbidities), index year, surgery characteristics (setting [inpatient, outpatient], approach [minimally invasive (MI) or open], type, and indication), and same-day surgery count (i.e. number of secondary procedures) as covariates. To create the matched cohort, patients were stratified by index surgery date, and surgeries resulting in UIs were matched to surgeries without UIs using the estimated propensity scores with a ratio of 1:3 on a caliper value of 0.2Citation10,Citation11. A patient without a UI could be matched to multiple patients with UIs if they had multiple index surgeries during the study period.
The number of healthcare visits and all-cause costs during the 30-day, 90-day, and 1-year post-index period were summarized. Healthcare visits and all-cause costs were summative, in that visits and costs occurring in earlier post-index periods were also captured in later post-index visits and costs. UI-attributable visits and costs for patients (i.e. out-of-pocket payments) and for payers (i.e. reimbursement) were defined as the mean difference between the matched pairs. As Medicare payments were excluded from the database used for this analysis, patients covered by Medicare were excluded from cost analyses in this study. Thirty-day readmission rates were estimated only in patients with inpatient index surgeries. Ranking of the types of index surgeries with the most UI cases (i.e. ≥5% of all UI cases) were summarized by CPT and ICD-10-PCS code ranges, separately.
Results
Patient characteristics
The total cohort included 522 patients with UIs (). Patient demographics and surgery characteristics are summarized in . Briefly, patients with and without UIs were similar in age, with 11.9% and 8.6% of each cohort aged ≥65 years, respectively. Compared with patients without UIs, patients with UIs had a higher mean Charlson Comorbidity Index (CCI) score, greater prevalence of GY surgeries and open surgical approaches, and more surgical procedures on the index surgery date. For patients with UIs, 29.9% of the index surgeries were performed in an outpatient setting. Other characteristics are summarized in Supplementary Table S2.
Figure 1. Patient disposition.
a≤1 month gap in enrollment was permitted.
bPatients with prespecified diagnoses and procedures on the index surgery date or by the date of UI identification were excluded. Examples include urological surgeries, ureter/kidney stones, or trauma.
cIf multiple targeted surgeries were identified within 30 days prior to the earliest UI identification date, the closest surgery to the UI identification date was selected as the index surgery. If multiple qualifying surgeries occurred on the date of injury, the index surgery was selected randomly.
dUI identified ≤30 days from index surgery.
Abbreviation: UI, ureteral injury.
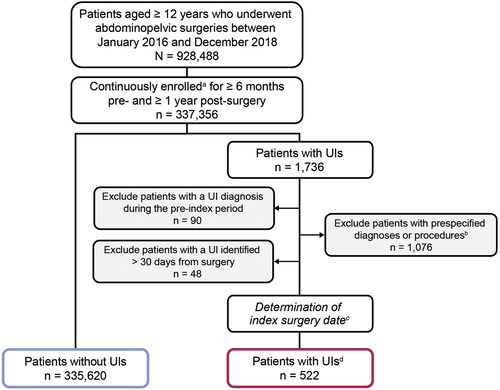
Table 1. Baseline demographic and surgical characteristics of patients with and without UIs in the total and matched cohorts.a
Characteristics and utilization of patients with UIs
Most UI cases were identified on the index surgery date, while 71 (13.6%) UI cases were identified postoperatively and within 30 days from the index surgery date (). Among patients with postoperative UI identification, the median days to UI identification was 7.0 days (interquartile range of 3.0–15.0). Of the postoperatively identified UIs, 63.4% (45/71) were identified due to hospitalization or during hospital readmission.
Table 2. Characteristics of patients with UIs in the total cohort.a
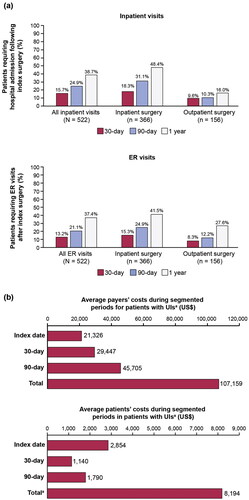
Among patients with UIs, the proportion of patients who required hospital admission was 15.7% within 30 days, 24.9% within 90 days, and 38.7% within 1 year following the index surgery (). Additionally, 13.2% of all patients with UIs had at least one emergency room (ER) visit within 30 days of surgery; this number increased to 37.4% in the year following the index surgery. The estimated payer and patient costs of all patients with UIs are presented in . The total average annual payer costs for patients with UIs was $107,159. The total average annual costs for patients with UIs was $8,194, with the index surgery date costs contributing the greatest proportion.
Figure 2. (a) Patients in the total cohort requiring hospital admission or ER visits after the index surgery, anmd (b) payer and patient costs for patients with UIs in the total cohort.
aCosts were calculated in a subset of patients with UIs by excluding Medicare Supplemental population (n = 501). Thirty-day and 90-day costs were excluded from costs on the index date.
Abbreviations: ER, emergency room; UI, ureteral injury.
UI-attributable healthcare visits and costs
Because baseline characteristics were different between surgeries with and without UI, propensity score matching was performed for a better comparison. After matching, patients with and without UIs had well-balanced characteristics (). By comparing the differences between patients with and without UIs in the matched cohorts, we estimated the proportion of healthcare visits and costs attributable to UIs. During the 1-year follow-up period, patients with UIs had higher proportions of healthcare visits than patients without UIs (Supplementary Table S3), with 12% more inpatient visits and 5.8% more ER visits. Patients with UIs also had a 15.3% higher rate of 30-day hospital readmission than patients without UIs (Supplementary Figure S1).
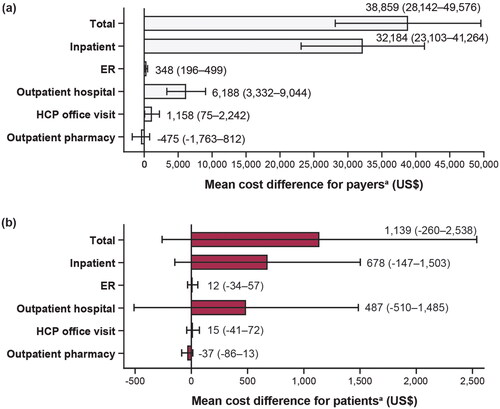
Payer costs, but not patient costs, were statistically higher in patients with UIs than patients without UIs in the matched cohort (). The total annual UI-attributable costs for payers were $38,859 (95% CI = 28,142–49,576), which were largely driven by inpatient costs ($32,184 [95% CI = 23,103–41,264]) (). The total costs for patients were $1,139 (95% CI = −260 to 2,538) ().
Figure 3. Costs attributed to UIs from index surgery date to 1 year for (a) payers and (b) patients.
aValues are mean cost differences with 95% CL for UI-related out-of-pocket all-cause costs between matched pairs. Excludes patients with Medicare Supplemental payer type.
Abbreviations: CL, confidence limits; ER, emergency room; HCP, healthcare provider; UI, ureteral injury.
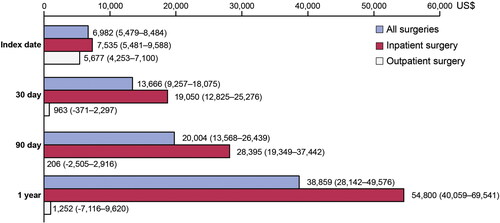
We further analyzed UI-attributable payer costs by index surgery setting at different timepoints in the matched cohort (). Payers had higher costs for patients with UIs than patients without UIs for all surgeries and inpatient surgeries at all timepoints, including the index date, 30-days post-surgery, 90-days, and 1-year timepoints. In patients with an inpatient index surgery, UI-attributable payer costs at 1 year were $54,800. Alternatively, in patients with an outpatient index surgery, payer costs were statistically higher only on the index date in patients with UIs than in patients without UIs.
Frequently identified surgeries with UI
The ranking of surgery types most frequently identified with a UI are presented in Supplementary Figure S2. As CPT and ICD-10-PCS codes define surgeries differently, the findings for each code are presented separately. By CPT code, open colon resection procedures were the most commonly identified surgery type with a UI (16.3%), followed by laparoscopic procedures of the abdomen/peritoneum/omentum (14.9%) and open abdominal hysterectomy (14.8%) (Supplementary Figure 2a). By ICD-10-PCS code, open surgery of the uterus (16.1%) was the most frequently reported with a UI, followed by open surgery of bilateral ovaries/fallopian tubes (10.9%) and open surgery of the sigmoid colon (10.7%) (Supplementary Figure 2b).
Discussion
UIs, overall occurring in less than 1% of GI and GY procedures, are rare but serious complications of these surgeriesCitation2–7. UIs can lead to a drastic change in quality-of-life and increase morbidity in otherwise healthy patientsCitation3,Citation8,Citation12. Previous studies that examined sequalae of UIs generally did not extend to 1 yearCitation4–6, and outcome studies primarily examined inpatient hospital cohorts to characterize the excess burden conferred by UIs, including length of hospital stay and healthcare costsCitation3. To build on the current literature, this study has three main novel findings: (1) over the 1-year follow-up period, patients with UIs had more healthcare visits than patients without UIs, and among patients with inpatient index surgeries, patients with UIs had a higher rate of 30-day readmissions than patients without UIs; (2) annual costs for payers were higher for patients with UIs than patients without UIs; and (3) nearly one-third of surgeries that resulted in UIs were carried out in an outpatient setting.
Publications on follow-up visits for patients with UIs are limitedCitation2. This study found that over the 1-year follow-up period, there were 12.0% more inpatient visits and 5.8% more ER visits among patients with UIs than patients without UIs. Further, in the inpatient setting, the rate of 30-day hospital readmission was 15.3% higher for patients with UIs than patients without UIs, and 15.3% of patients with UIs had an ER visit within 30 days. These findings are notable because hospital readmissions within 30 days are subject to readmission review and may result in denial of payment to the hospital. Moreover, readmissions within 30 days are reportable under the Merit-based Incentive Pay System as an indicator of quality. Similarly, ER visits shortly after an inpatient hospitalization are also used by many hospitals as an administrative measure of quality.
This study found that annual costs for payers were almost $39,000 higher in patients with UIs than patients without UIs, driven by inpatient costs ($32,184) throughout the year. Compared with patients without UIs, patients with UIs had higher payer costs at 1 year, on the index date, and at 30 days and 90 days post-surgery for all surgeries and inpatient surgeries. Annual costs for patients were not statistically different between patients with or without UIs.
To our knowledge, there is no literature examining costs and outcomes of UIs associated with outpatient surgeries. As outpatient procedures tend to be less complex, and a rapid return to normal activities is typicalCitation13,Citation14, a lower UI rate for surgeries in an outpatient setting was expected. Surprisingly, in the current study, nearly one-third of patients with UIs had outpatient surgeries. Further, as shown in , some of these patients required subsequent inpatient (16.0%) and/or ER (27.6%) visits. For patients with an index surgery in the outpatient setting, payer costs on the index date were higher in patients with UIs than those without UIs ($5,677); however, payer costs at short-, middle-, and long-term timepoints were not statistically different between patients with or without UIs. Nonetheless, outpatient surgeries should not be overlooked when thinking about preventing UIs or the need for better ureter visualization during surgery.
The patient population in this study was different from prior studies in two aspects. First, this study evaluated a wide range of abdominopelvic surgeries, without restricting surgical procedures, settings, or approaches. This allowed us to rank surgeries that are most frequently identified with a UI, thus providing an understanding of UIs in the context of a wide range of types of surgeries. Coakley et al.Citation6 reported that patients with a UI after colectomy with a prophylactic ureteral catheter placement had a 9.9% 30-day readmission rate, which increased to 12.4% for patients without the prophylactic catheter. In our study, the 30-day readmission rate for patients with inpatient index surgery was 25.3%. In addition to differences in databases, surgery codes, or UI definitions between the two studies, the discrepancy may also stem from the broader surgical population in our study, as it included both GY and GI surgeries. Similarly, when comparing our study with a study using the Healthcare Cost and Utilization Project–Nationwide Inpatient Sample, the cohort in our study was more likely to be female, likely due to inclusion of GY surgeriesCitation3.
The second difference of our study from prior studies is that we identified UIs from commercial insurance claims, in which the elderly population is limited. When comparing our study with the study by Halabi et al.Citation3, the cohort in our study was younger (median age of patients with UIs: 49 vs 64 years old; patients without UIs: 47 vs 63 years old), healthier (CCI score among the patients with UIs: 2.0 vs 6.0; patients with malignancy: 17.2% vs 30.4%), and more likely to have commercial health insurance coverage versus Medicare coverage. Halabi et al.Citation3 examined hospital charges rather than reimbursements and found the average UI-attributable hospital charge was $31,497, which is comparable to our findings of the UI-attributable reimbursement for the inpatient setting of $32,184.
Finally, this study found that most UIs were detected on the day of surgery and they may have been identified intraoperatively, although this finding is, in part, due to the inclusion criterion that UIs had to have been observed within 30 days of the index surgery. The timely identification of UIs is important because UIs caught intraoperatively can generally be repaired during surgery, thus improving patient outcomesCitation2,Citation12. There is debate in the literature about the timing of UI identifications. Several studies found that most UIs were identified post-operativelyCitation2,Citation15,Citation16, while others observed more intraoperatively identified UIsCitation17. Heterogeneity exists in the populations, surgical types, and study designs among these publications; however, studies that identified more postoperative UIs focused on GY surgeriesCitation2,Citation15,Citation16, while studies that identified more intraoperative UIs examined colorectal surgeriesCitation17. Although we included both types of surgeries, there were more GI surgeries, including colorectal surgeries, in the database; this likely explains our observation that most UIs were detected on the day of surgery.
This retrospective study in a real-world population has some limitations. With the nature of claims data, many unknowns exist. For example, it is difficult to determine if patient visits to healthcare providers’ office were for UI treatment, or if visits were for other reasons and happened to occur at the time the patients had UIs. UIs identified during surgery may be less costly than those identified post-operatively. However, as there is no timestamp for the procedures and UI diagnosis in the claims database, these data are not able to distinguish between UIs identified intraoperatively during surgery or after closure of the index surgery (but still on the same day). The place of service on the date of UI identification may not have been the same location where the UI was identified. Another limitation is that the claims data used for this study were derived from a commercially insured population and had low enrollment of patients aged ≥65 years, so these findings may not be representative of older patients or patients with non-commercial or no insurance coverage. As healthcare resource utilization tends to be higher in older adults, the resource costs estimated in this study are likely lower than would be seen in a more representative population. We also required 1-year post-index continuous enrollment for estimation of 1-year costs, introducing survivor bias. However, the dropout rates for patients with and without UIs were similar (about 46% for both groups), so the impact for the comparison between the matched groups is likely small. As this was a retrospective claims-based analysis, we did not assess the incidence of UI by specific procedure codes. Additionally, unmeasured factors related to patients (e.g. frailty, types of anesthesia), hospital procedures (e.g. prophylactic protocols), and reimbursement (e.g. disparities in coding) may affect the results of the analysis. Future studies of UI will be necessary to explore the variability introduced by each factor.
It is noteworthy that most patients in our study were middle-aged and had few comorbidities with low CCI scores. Given that our findings showed that UIs conferred additional healthcare visits and higher system costs for patients who were otherwise healthy, that current methods of UI prevention and identification may not be reliableCitation18,Citation19, and the lack of guidelines on this topic, research into newer non-invasive techniques for UI prevention may be warrantedCitation18,Citation19.
Conclusions
In this study, we found that UIs lead to increased costs for payers at 30-day, 90-day, and 1-year timepoints, with statistically insignificant cost increases for patients. Patients with an inpatient index surgery with UIs had a 30-day readmission rate that was 15.3% higher than patients without UIs. Unexpectedly, we found that about one-third of index surgeries that resulted in UIs occurred in the outpatient setting. While much of the literature supports the burden of UI on hospitals, our results demonstrate that UIs also add significant costs to payers and results in more healthcare visits for patients. Though UIs are rare, the substantial patient and payer burden outlined in this study point to the need for attention to protocols or techniques to minimize the risk of these injuries.
Transparency
Declaration of funding
This study was sponsored by Astellas Pharma Global Development, Inc.
Author contributions
EFS, TK, and QF contributed to the study design. TK and QF contributed to the data acquisition and statistical analysis. All authors contributed to the data analysis. SDM, EFS, TK, and QF contributed to the interpretation of the data. EFS and TK contributed to the supervision of the study. All authors contributed to the drafting of the article, provided critical review, and approved the version to be published.
Ethics statement
Given the retrospective nature of this study, institutional review board approval was not deemed necessary. In accordance with the HIPAA Privacy Rule, disclosed Premier Healthcare Database data are considered deidentified per 45 CFR 164.506(d)(2)(ii)(B) through the “Expert Determination” method. This study was conducted in compliance with national requirements for non-interventional studies using deidentified data. Analysis of PharMetrics Plus, IQVIA database was permitted per the data licensing agreement.
Supplemental Material
Download MS Word (440.7 KB)Declaration of financial/other relationships
SM receives consulting fees from Astellas Pharma Global Development, Inc. EFS, TK, QF, WH, and BJ are employees of Astellas Pharma Global Development, Inc.
Medical writing support was provided by Caroline Leitschuh, PhD, and Jing Xu, PhD, of Oxford PharmaGenesis Inc., Newtown, PA, USA, and was funded by Astellas Pharma Global Development, Inc.
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Data availability statement
Researchers may request access to anonymized participant level data, trial level data, and protocols from Astellas sponsored clinical trials at www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing see: https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx
References
- Abboudi H, Ahmed K, Royle J, et al. Ureteric injury: a challenging condition to diagnose and manage. Nat Rev Urol. 2013;10(2):108–115. doi: 10.1038/nrurol.2012.254.
- Blackwell RH, Kirshenbaum EJ, Shah AS, et al. Complications of recognized and unrecognized iatrogenic ureteral injury at time of hysterectomy: a population based analysis. J Urol. 2018;199(6):1540–1545. doi: 10.1016/j.juro.2017.12.067.
- Halabi WJ, Jafari MD, Nguyen VQ, et al. Ureteral injuries in colorectal surgery: an analysis of trends, outcomes, and risk factors over a 10-year period in the United States. Dis Colon Rectum. 2014;57(2):179–186. doi: 10.1097/DCR.0000000000000033.
- Benson CR, Thompson S, Li G, et al. Bladder and ureteral injuries during benign hysterectomy: an observational cohort analysis in New York state. World J Urol. 2020;38(8):2049–2054. doi: 10.1007/s00345-018-2541-y.
- Adelman MR, Bardsley TR, Sharp HT. Urinary tract injuries in laparoscopic hysterectomy: a systematic review. J Minim Invasive Gynecol. 2014;21(4):558–566. doi: 10.1016/j.jmig.2014.01.006.
- Coakley KM, Kasten KR, Sims SM, et al. Prophylactic ureteral catheters for colectomy: a national surgical quality improvement program-based analysis. Dis Colon Rectum. 2018;61(1):84–88. doi: 10.1097/DCR.0000000000000976.
- McCarus SD, Alexandre AF, Kimura T, et al. Abdominopelvic surgery: intraoperative ureteral injury and prophylaxis in the United States, 2015-2019. Adv Ther. 2023;40(7):3169–3185. doi: 10.1007/s12325-023-02515-z.
- Institute of Medicine (US) Committee on Quality of Health Care in America. To err is human: building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. doi: 10.17226/9728.
- Zafar SN, Ahaghotu CA, Libuit L, et al. Ureteral injury after laparoscopic versus open colectomy. JSLS. 2014;18(3):e2014.00158. doi: 10.4293/JSLS.2014.00158.
- Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172(9):1092–1097. doi: 10.1093/aje/kwq224.
- Chen JW, Maldonado DR, Kowalski BL, et al. Best practice guidelines for propensity score methods in medical research: consideration on theory, implementation, and reporting. A review. Arthroscopy. 2022;38(2):632–642. doi: 10.1016/j.arthro.2021.06.037.
- Chalya PL, Massinde AN, Kihunrwa A, et al. Iatrogenic ureteric injuries following abdomino-pelvic operations: a 10-year tertiary care hospital experience in Tanzania. World J Emerg Surg. 2015;10(1):17. doi: 10.1186/s13017-015-0011-z.
- Manohar A, Cheung K, Wu CL, et al. Burden incurred by patients and their caregivers after outpatient surgery: a prospective observational study. Clin Orthop Relat Res. 2014;472(5):1416–1426. doi: 10.1007/s11999-013-3270-6.
- Gabriel RA, Waterman RS, Burton BN, et al. Patient health status and case complexity of outpatient surgeries at various facility types in the United States: an analysis using the national anesthesia clinical outcomes registry. J Clin Anesth. 2021;68:110109. doi: 10.1016/j.jclinane.2020.110109.
- Brummer TH, Jalkanen J, Fraser J, et al. FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Hum Reprod. 2011;26(7):1741–1751. doi: 10.1093/humrep/der116.
- Wong JMK, Bortoletto P, Tolentino J, et al. Urinary tract injury in gynecologic laparoscopy for benign indication: a systematic review. Obstet Gynecol. 2018;131(1):100–108. doi: 10.1097/AOG.0000000000002414.
- Andersen P, Andersen LM, Iversen LH. Iatrogenic ureteral injury in colorectal cancer surgery: a nationwide study comparing laparoscopic and open approaches. Surg Endosc. 2015;29(6):1406–1412. doi: 10.1007/s00464-014-3814-1.
- Lee Z, Kaplan J, Giusto L, et al. Prevention of iatrogenic ureteral injuries during robotic gynecologic surgery: a review. Am J Obstet Gynecol. 2016;214(5):566–571. doi: 10.1016/j.ajog.2015.10.150.
- Mazzarella G, Muttillo EM, Picardi B, et al. Real-Time intraoperative ureteral identification in minimally invasive colorectal surgery: a systematic review. J Laparoendosc Adv Surg Tech A. 2022;32(6):627–633. doi: 10.1089/lap.2021.0292.