Disclaimer
As a service to authors and researchers we are providing this version of an accepted manuscript (AM). Copyediting, typesetting, and review of the resulting proofs will be undertaken on this manuscript before final publication of the Version of Record (VoR). During production and pre-press, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal relate to these versions also.Cervical cancer develops gradually due to aberrant cell proliferation and starts in the cervix, which is the vital pathway connecting the uterus and vagina. This global health risk is primarily caused by histological subtype of cervical cancer which are: squamous cell carcinoma, responsible for 90% of cases, and adenocarcinoma. The most common culprit is the human papillomavirus, HPV, which is frequently acquired through sexual contact. Although the majority of infections heal on their own, a few factors raise the possibility of HPV infection persisting and developing into cervical cancer. These include using birth control tablets regularly, obesity, smoking, and compromised immune systems [1]. Cervical cancer is the fourth most frequent cancer worldwide among women, with 23% of cases occurring in India alone. Population-based cervical cancer screening is not yet widely used in the India because of conflicting healthcare goals, a lack of funding, and an inadequate number of qualified healthcare professionals. As a result, many instances appear at advanced stages, leading to higher death rates and worse survival rates. Cervical cancer can be detected early using a variety of screening tools, including cytology, visual-based methods, and testing for high-risk HPV [2]. Globally cervical cancer accounts for around 604,000 cases annually. As the most common cancer among women, cervical cancer is highly widespread in India. With 365.71 million women over 15, thought to be at risk, the nation is responsible for around one-third of all cervical cancer fatalities globally [3]. Based on this data, India leads Asia in the number of instances of cervical cancer, with China following closely behind. According to a Lancet study, cervical cancer caused 40% of all deaths; 23% of these deaths happened in India and 17% in China. Based on estimates from The Global Cancer Observatory (GLOBOCAN) 2020, the study takes temporal, socioeconomic, and geographic factors into account [4]. Over 600,000 new instances of cervical cancer are expected worldwide in 2020, of which over 340,000 will result in fatalities. In densely populated nations including China, India, Indonesia, Russia, and Brazil, the incidence surpassed the 4 cases per 100,000 women, World Health Organisation (WHO) criterion. In particular, India recorded a startling 18 instances for per 100,000 females. According to the report, it will be difficult to reach the WHO eradication threshold by 2030 unless nations strengthen their screening initiatives and raise the rate of HPV vaccination [5]. It is estimated that in a medium HDI country like India, efforts for scaling up HPV vaccination covering 80–100% of target population together with two cervical cancer screenings per lifetime would help
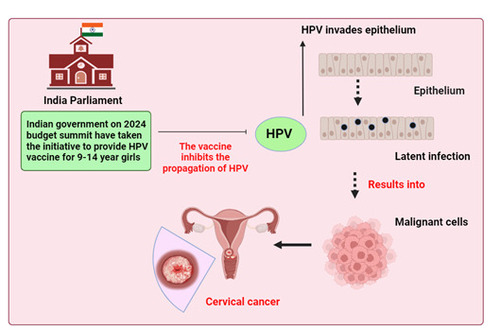
achieve cervical cancer elimination by 2070–79 [6]. Union Finance Minister Nirmala Sitharaman stated plans to concentrate on cervical cancer vaccination for girls aged 9 to 14 in the Interim Budget 2024 on 1st of February 2024, acknowledging the necessity of combating the disease. This pledge supports the fight against the illness and offers hope for more preventive actions. During her speech, the finance minister also revealed a number of additional health-related initiatives, such as expanding Ayushman Bharat coverage to include all Asha workers and Anganwadi workers and assistants [7]. To prevent cervical cancer, the National Technical Advisory Group for Immunisation (NTAGI) of India proposed two years ago that the HPV vaccine be included in the Universal Immunisation Programme (UIP). Nevertheless, specifics regarding the government's plan are still unknown. While Sitharaman declared in her budget address that “our government will encourage vaccination for girls aged 9 to 14 years as a preventive measure against cervical cancer, there is no clear information in the plan of action. Cervical cancer is the second most frequent cancer among women worldwide, and it is largely due India. The Human Papillomavirus (HPV) is the main culprit, and because immunisation programmes are not widely available and awareness is low, the virus's prevalence is still significant. The prevalence of HPV and cervical cancer endures despite national cancer screening programmes being implemented by the central government. The International Agency for Research on Cancer (IARC) predicted 77,348 fatalities and 123,907 new cases of cervical cancer in India, according GLOBOCAN 2020. Precancerous lesions can be found with routine screening with Pap smears or HPV tests, allowing for early intervention and the prevention of cancer. Unfortunately, screening rates remain shockingly low in India, especially in rural regions. This results in late-stage diagnoses and inadequate access to prompt treatment, which prevents unnecessary deaths and unrealized potential. Dr. Krithiga Shridhar, an epidemiologist at the Centre for Chronic Disease Control (CDC) of United States of America, highlights the commitment made by all countries to eradicate cervical cancer by early detection, treatment, vaccine, and screening. Based on data from the National Cancer Registry, cervical cancer is the most prevalent cancer among women in rural areas and the second most common cancer among Indian women overall, accounting for almost one-fifth of all female cancer cases. On June 28, 2022, the NTAGI recommended the HPV vaccine be added to the UIP. It suggested a one-time catch-up programme for teenage girls between the ages of 9 and 14 and a regular introduction programme starting at age nine. The current bill, which was passed on February 1st, will be a significant step in the fight against cervical cancer in India because it addresses a worrying issue i.e., HPV which is a major cause of cervical cancer, and vaccination against it is a fantastic way to protect Indian girls from this deadly disease in the future. Already, a number of states have moved aggressively in this direction. Delhi launched a programme in 2016 with high coverage rates for girls between the ages of 9 and 14. As part of pilot programmes, schools in certain districts in Punjab, Sikkim, Karnataka, Tamil Nadu, Chhattisgarh, and Maharashtra will receive free HPV vaccinations for their female students. While Uttar Pradesh has recently announced free HPV vaccination for schoolgirls in certain districts as part of a pilot programme, Mizoram has incorporated free HPV vaccination in its regular immunisation programme for girls aged 10 to 12 years [8]. In a response to a query in the Lok Sabha on Friday 2nd of February 2024, Minister of State for Health Satya Pal Singh Baghel disclosed that the National Cancer Registry Programme (ICMR-NCRP) under the Indian Council of Medical Research estimated a staggering over 3.4 lakh cases of cervical cancer in India in 2023. He conveyed in writing that the National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD), a constituent of the National Health Mission (NHM), provides financial and technical assistance to states and Union territories through the Department of Health and Family Welfare at the central level [9]. In a recent study a total of 545 patients met the inclusion criteria for the study. Positive margins were identified in 160 patients (29.3%). Among the patients, 247 (45.3%) had documented infections from HPV16/18, and 123 (22.6%) had infections from other high-risk HPV types. Persistent HPV infections were diagnosed in 187 patients (34.3%) at 12 months, 73 patients (13.4%) at 18 months, and 40 patients (7.3%) at 24 months. Patients with HPV persistence at 6 months faced a 7.46% risk of recurrence. Twelve-month HPV persistence was strongly associated with an increased risk of recurrent disease, with a recurrence risk of 13.1% [10]. India continues to endure a heavy burden from cervical cancer, which is still a serious global health concern. To battle this preventable disease, solid implementation methods, enhanced awareness, and proactive measures are required, especially in addition to the efforts being made to address the difficulties through vaccination plans and screening programmes. Government leaders like Finance Minister Sitharaman's dedication is critical in advancing the cause, but long-term initiatives involving communities, healthcare systems, and individuals are needed to make a significant impact in the fight against cervical cancer. Given below is the representation of the initiative taken by Indian government.
Future Direction
Building upon the current initiatives, here are some potential future directions that the Indian government could consider in the ongoing fight against cervical cancer i.e. Expanding Vaccination Coverage, Awareness and Education Campaigns, Integration with Primary Healthcare, Mobile Health Technologies, Capacity Building, Research and Innovation, Collaboration with NGOs and International Organizations, Monitoring and Evaluation. Two effective strategies to prevent cervical cancer are getting vaccinated against HPV to protect against the virus types most often causing cervical cancer and undergoing regular Pap smear and HPV tests to detect and treat precancerous conditions early. By incorporating these future directions into existing efforts, the Indian government can further strengthen its commitment to combating cervical cancer and improve the health outcomes of women across the country.
Transparency
Declaration of funding
This paper was not funded.
Declaration of financial/other relationships
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
The author KC Sharma thanks to ISF Moga for providing necessary facility for carryout the work.
References
- Ankush B. Cervical Cancer: All Ypo Need to Know About. The Times of India [Internet]. 2024 Feb 02 [Cited on 2024 Feb 03];Health. Available from: https://weather.com/en-IN/india/health/news/2024-02-02-cervical-cancer-all-about-causes-symptoms-prevention-more.
- Mishra GA, Pimple SA, Shastri SS. Prevention of cervix cancer in India. Oncology. 2016;91:1-7. doi: 10.1159/000447575.
- Incidence of Cervical Cancers in India- Role of HPV testing & Vaccination. Apollo Diagnostics. 2023 Sep 23 [Cited on 2024 Feb 03]. Available from: https://www.apollodiagnostics.in/blog/incidence-of-cervical-cancers-in-india-role-of-hpv-testing-&-vaccination
- Singh D, Vignat J, Lorenzoni V et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob. Health 2023;11(2):E197-E206. doi: 10.1016/S2214-109X.(22)00501-0
- Thacker T. India has the most cervical cancer patients in Asia: Lancet. The Economic Times [Internet]. 2022 Dec 15 [Cited on 2024 Feb 04];Industry. Available from: https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/india-has-the-most-cervical-cancer-patients-in-asia-lancet/articleshow/96234392.cms?from=mdr
- Simms KT, Steinberg J, Caruana M, Smith MA, Lew JB, Soerjomataram I, Castle PE, Bray F, Canfell K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–99: a modelling study. The lancet oncology. 2019; 20(3); 394-407.
- Govt to focus on vaccination against cervical cancer announces Finance Minister Nirmala Sitharaman. The Hindu Bureau [Internet]. 2024 Feb 01 [Cited 2024 Feb 04]; Business. Available from: https://www.thehindu.com/business/budget/govt-to-focus-on-vaccination-against-cervical-cancer-announces-finance-minister-nirmala-sitharaman/article67799549.ece
- Sharma NC. Budget 2024: Gov to promote HPV vaccination for girls aged 9-14 to prevent cervical cancer, announces FM Sitharaman. Business Today [Internet]. 2024 Feb 01 [Cited 2024 Feb 04]; Union Budget. Available from: https://www.businesstoday.in/union-budget/story/budget-2024-gov-to-promote-hpv-vaccination-for-girls-aged-9-14-to-prevent-cervical-cancer-announces-fm-sitharaman-415776-2024-02-01
- Over 3.4 Lakh Cervical Cancer Cases In India In 2023: Parliament Informed. NDTV. [Internet]. 2024 Feb 02 [Cited 2024 Feb 04]; India News. Available from: https://www.ndtv.com/india-news/over-3-4-lakh-cervical-cancer-cases-in-india-in-2023-parliament-informed-4982338
- Bogani G, Sopracordevole F, Ciavattini A, Vizza E, Vercellini P, Giannini A, Ghezzi F, Scambia G, Raspagliesi F, Di Donato V, Investigators of the Italian HPV study group. Duration of human papillomavirus persistence and its relationship with recurrent cervical dysplasia. European Journal of Cancer Prevention. 2023; 32(6); 525-32.