Abstract
Background: Preconception health and care aims to reduce parental risk factors before pregnancy through health promotion and intervention. Little is known about the preconception interventions that general practitioners (GPs) provide. The aim of this study was to examine GPs’ knowledge, attitudes, and views towards preconception health and care in the general practice setting.
Methods: As part of a large mixed-methods study to explore preconception care in England, we surveyed 1,173 women attending maternity units and GP services in London and interviewed women and health professionals. Seven GPs were interviewed, and the framework analysis method was used to analyse the data.
Findings: Seven themes emerged from the data: Knowledge of preconception guidelines; Content of preconception advice; Who should deliver preconception care?; Targeting provision of preconception care; Preconception health for men; Barriers to providing preconception care; and Ways of improving preconception care. A lack of knowledge and demand for preconception care was found, and although reaching women before they are pregnant was seen as important it was not a responsibility that could be adequately met by GPs. Specialist preconception services were not provided within GP surgeries, and care was mainly targeted at women with medical conditions. GPs described diverse patient groups with very different health needs.
Conclusion: Implementation of preconception policy and guidelines is required to engage women and men and to develop proactive delivery of care with the potential to improve pregnancy and neonatal outcomes. The role of education and of nurses in improving preconception health was acknowledged but remains under-developed.
Background
Preconception health and care aims to reduce parental risk factors before pregnancy and improve outcomes through health promotion and intervention (Citation1). Optimizing maternal and paternal health before conception can influence a child’s future life-course (Citation2–4). Current demographic and epidemiological trends such as obesity, diabetes, and delayed child-bearing increase the potential for preconception care to lead to significant health gain (Citation5,Citation6).
The importance of preconception care has gained greater recognition with the World Health Organization (WHO) Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013–2020 (Citation7). Within the UK, government policy aims to reduce perinatal morbidity and mortality through promotion of pre-pregnancy care (Citation8). Recommendations incorporate promotion of health-related behaviours including reducing the incidence of neural tube defects through folic acid supplementation; reducing pre-term births, low birth weight, and poor neonatal and maternal outcomes through smoking cessation, alcohol reduction, and achievement of healthy weight and nutrition prior to conception; reducing infections through screening and vaccination; and identifying medications and occupational and environmental hazards that could be teratogenic. This is reinforced by the recommendation for couples to plan their pregnancies in order to improve maternal outcomes (Citation9).
In order to explore and provide an overview of preconception care in England, we undertook a mixed-methods study which surveyed 1,173 women and their partners attending maternity units and general practitioner (GP) services in London. The survey aimed to explore how they had prepared for pregnancy. We also carried out semi-structured interviews with a sub-sample of this group to investigate reasons and motivations as to why they invested in pre-pregnancy care. The findings reported elsewhere (Citation10,Citation11) showed that two-thirds of women plan their pregnancies, but despite this there was little change in preconception health behaviours such as uptake of folic acid by these women. It was found that prospective parents in the UK have little access to specific preconception care services but that 51% received advice from a health professional prior to pregnancy in relation to the importance of healthy lifestyle behaviours such as diet, smoking, and alcohol. A quarter of the women in our study had a medical condition, and 26% were taking regular medications and potentially needed specialist advice before trying to conceive.
Little is known about the specific preconception interventions that GPs provide for women of child-bearing age. As part of the study we interviewed GPs with the aim of examining knowledge, attitudes, and views towards preconception health and care in the general practice setting. This paper reports the findings.
Method
Qualitative methodology with a qualitative description framework (Citation12) was used to describe phenomena attained from GP’s experiences and their views of the organization of preconception care services.
Purposive sampling was used to recruit from general practice networks in London. Fifteen GPs with a remit for obstetrics and gynaecology within their practice were invited by email to participate in the study, and seven agreed to be interviewed. The sample size was based on previous experience within qualitative research in relation to the study scope and a mix of other factors such as the funding and the time available (Citation13).
Interviews were conducted in private offices within the GP practices and carried out by three researchers (B.H., J.A.S., O.O.) who had a women’s health care focus and were trained in qualitative research interviewing. Confidentiality was upheld and written consent obtained before proceeding with the interviews. Interviews lasted up to 45 minutes, and the GPs received an honorarium as compensation for their time.
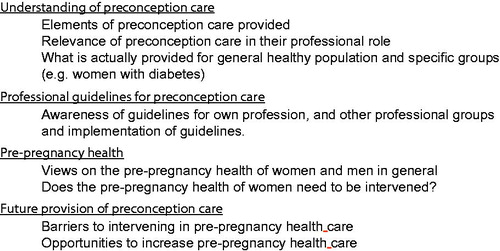
A topic guide () was used during the semi-structured interviews which explored: the GP’s own experiences of how preconception care policy, guidelines, and recommendations are implemented in day-to-day practice; the GP’s understanding of content of preconception care; the nature of current service provision; who in the GPs opinion should have responsibility for providing preconception care; and opportunities and barriers to future service delivery.
Interviews were digitally recorded and transcribed verbatim by O.O., B.H., and D.P. Transcripts were imported into NVivo 10 computer software (Citation14), and data workshops were then held with four researchers (B.H., D.P., J.A.S., O.O.). Thematic analysis using framework method (Citation15) ensured systematic and rigorous exploration of the text in five stages: (1) familiarization with data, (2) identification of a thematic framework, (3) indexing, (4) charting, and (5) mapping and interpretation.
Mapping and interpretation was an iterative process. Using NVivo 10, we developed a matrix and examined charts, codes, and the full transcripts to develop a description of the phenomena and the concepts that evolved.
Favourable ethical opinion was given by the National Research Ethics Service (NRES) Committee London, Bromley (REC reference 11/LO/0881) as part of the larger study ‘Pre-Pregnancy Health and Care in England’.
Findings
The seven GPs (4 male and 3 female) who agreed to be interviewed were all partners in their practices with the exception of one who was a part-time salaried GP. The GPs had qualified between 1987 and 2006 and had an average of 13.7 years’ experience since qualification. Five GPs had previous experience in obstetrics and gynaecology; three had DRCOG qualifications; four were also GP Trainers.
Seven main themes emerged from the data: (1) Knowledge of preconception guidelines; (2) Content of preconception advice; (3) Who should deliver preconception care?; (4) Targeting provision of preconception care; (5) Preconception health for men; (6) Barriers to providing preconception care; and (7) Ways of improving preconception care.
Knowledge of preconception guidelines
GPs stated that they had gained their knowledge of the elements of preconception care from clinical experience, from past training, or from patient information sources rather than from guidelines.
… no … I didn’t know the specific guidelines, I tend to just kind of, erm, I kind of work from information given to patients really. (GP 5)
We found that GPs were not familiar with preconception guidelines. They mentioned that there ‘must be’ guidelines available from the National Institute for Health and Care Excellence (NICE) or the Royal College of Obstetricians and Gynaecologists but confessed they had not always read or were aware of them, as the following comments show:
Interviewer: Can I ask what is your awareness of the professional guidelines of preconception care.
Respondent: Limited.
Interviewer: Right. That is very honest.
Respondent: I have not read them. (GP 1)
I would have thought that was in the NICE guidelines, because, obviously, we go via the NICE guidelines giving folic acid and immunizations, diets, all the things at the beginning … (GP 2)
Content of preconception advice
All GPs agreed on the main issues that they would discuss as part of preconception care and mentioned healthy eating, being a healthy weight; starting folic acid supplementation; stopping smoking; and reducing or abstaining from alcohol use.
In addition to folic acid, GPs also mentioned that they gave advice on other vitamin supplementation if required. This was particularly in the context of vitamin D for specific ethnic populations who were deemed to be more at risk of deficiency. In general, the GPs also recommended a multivitamin supplement to their patients.
we have quite a high, also got quite, umm, a number of patients who have a low vitamin D. […] so… generally I would be probably be recommending a multivitamin. (GP 4)
The GPs talked about other relevant elements of preconception care, and it was frequently mentioned that they would check that women were rubella-immune or had had a rubella injection, and one also mentioned asking women if they had had chicken pox. They also said that they would do a risk assessment for mental health issues before pregnancy.
We risk-assess in terms of mental health problems, if they have got a history of depression, bipolar, schizophrenia—really any sort of mental health issues. (GP 7)
The GPs appeared very aware that when prescribing medications to any women of child-bearing age that the safety of the medicine in pregnancy needed to be considered.
if you assume all women of child-bearing age are either pregnant or are about to get pregnant, you try to do least or less harm as possible. (GP 1)
We found that there was lack of consistency given about the specific content of the advice given in relation to alcohol consumption. Before conception some GPs advised abstinence, whilst others just a reduction of alcohol to less than a unit per day, and others consumption within sensible limits. GPs acknowledged that more consistency in the advice provided by health professionals to women was needed.
It should be consistent because I think like with ante-natal care it’s really quite difficult […] I say no, you shouldn’t drink alcohol at all and other people say well, you know, I drank through my pregnancy so it’s ok, you can have a glass now and again. Umm, it’s not consistent. (GP 6)
Who should deliver preconception care?
Although there was agreement on the important elements of preconception care, views were mixed on the role of GPs providing such care. Most were comfortable referring women with medical diseases such as diabetes and epilepsy to secondary care for preconception counselling. Interestingly, some of the GPs did not feel they should be the gatekeepers of preconception care. Instead, they felt strongly that pre-pregnancy health should be a public health issue and that campaigns to increase public awareness would empower women to seek information and facilitate their own reproductive choices.
Respondent: I think most of it is educational … in certain population groups, but it seems to be more a matter of education, providing information.
Interviewer: So, would that be education by GPs and medics, or where would you put the education?
Respondent: Well, I’m not, it depends on where, is this a job of the medical profession? Or is it a job of the education services? They overlap, don’t they? I think education is more important than medicine. (GP 1)
Again, education isn’t it? Yeah. Education, education, and education. (GP 3)
There was no broad consensus that GPs could play a greater role and become more involved in the delivery of preconception care. Central to that was the lack of discussion on the provision of a specialized preconception service. Instead, many GPs discussed the integration of care into the consultations.
Regarding a potential service delivery model, the most common opinion was that pre-pregnancy care could be delivered by nurses who could provide information when carrying out contraception consultations or whilst undertaking cervical screening, during postnatal review, or when seeing adolescents in schools.
… If they come in specifically asking for preconception advice, I usually refer to the nurse, they have another consultation and see actually what the agenda is. (GP 1)
Because it tends to be more with nurses than it does the doctor, to be honest, because when people make a doctor’s appointment, it’s usually because they’re sick or there’s something going on. But when they see the nurse for a smear or a pill check, that’s when they often sort of indulge, you know, because one of the questions they have to do before they have the smear is, you know, are they planning on getting pregnant, are they on contraception. Then they can get that information quite quickly and then be able to have an opportunistic counselling session then probably. (GP 2)
Targeting provision of preconception care
The interviews demonstrated that GPs would promote healthy lifestyle behaviour to women attending the surgery that were trying to have a baby or thinking of having one in the future.
OK, so that could be anybody who’s contemplating pregnancy at any stage so it might be a conversation from, ummm […], the obvious one you know, I’m thinking about getting pregnant what do you think I should do? Or I’m not, or when you’re giving contraceptive advice sometimes it’s actually not now but later I might think about getting pregnant … you know, how long should I take it till I … till I stop my contraception so. (GP 6)
The GPs targeted care and preconception advice to women with established medical conditions such as diabetes or epilepsy. This involved specific advice about the need for good glucose control before conception for women with diabetes, and the need to review medications that may be teratogenic in other chronic medical conditions.
For the diabetics, to make sure their sugar is well controlled and that they might need more interventions when they’re pregnant in the sense of testing their blood glucose levels when they’re pregnant and they might need to be on insulin … (GP 2)
For those with epilepsy we, sort of, give them a neurology review. Before you fall pregnant, let’s just see whether we can we change to a medication which is least likely to cause problems […] in terms of diabetes. (GP 7)
The GPs were more likely to see a woman of child-bearing age to discuss contraception rather than preconception health. GPs acknowledged that they did not have consultations that centred on preconception care, and those that did stated this was prompted by patient request for information rather than being initiated by the GP. Many GPs talked about women attending with concerns and anxiety about becoming pregnant because of their age, for example:
So I think it tends to be women who, in my experience […], people who are worried that they’re in their 30s and they want to try and conceive and they’ve waited a long time and they want to make sure that they’re doing everything they can to try and conceive a healthy baby. And I think that kind of anxiety is what brings them to the GP to ask for counselling in the first place, because I don’t think I really get people younger than 30 asking for pre-pregnancy counselling. (GP 2)
It was generally reported that this group of women, in their 30s or older, tended to be from a higher socioeconomic class and were more educated on preconception health, health-conscious, and more likely to seek preconception care from their GP.
Middle-class professional women who are all taking folic acid, they have all been for their rubella check and they are exercising and eating healthily and all that kind of stuff and then are getting ready for pregnancy and their diet, and they are on top of things. (GP 5)
In contrast, it was mentioned by a GP serving a student population that students were educated about preconception care and therefore less likely to seek advice from their GP.
They are quite informed [about preconception health]. I think a lot them seem to be pretty well informed and do all the right things you know, they may drink within normal limits and they don’t smoke and they exercise. (GP 7)
The interviews demonstrated that GPs identified women who were perhaps in greater need of preconception care as being younger, often from immigrant populations, and less educated on preconception health and hence less prepared for pregnancy. These women were less likely to seek preconception advice from their GP. Even trying to discuss ideas and attitudes towards pre-pregnancy health and care was challenging as women presented during pregnancy.
We have got two big housing estates who tend to be unfit and they are still smoking and they are drinking and they often [have] unplanned pregnancies. I mean they would never come to, for pre-pregnancy counselling. It would all be just ‘I am pregnant, doctor, … can I have a termination?’ (GP 7)
The ethnic minorities probably, and they’re probably the people who have undiagnosed issues so, umm … whether it’s maybe things like sickle cell or thalassemia, or they’re carriers of genetic diseases, but they don’t really sort of voice these things … or issues with other previous pregnancies. (GP 6)
GPs associated the trend of women who smoked as having poorer preconception health. On further questioning, they felt that offering pre-pregnancy advice to this particular group of women did not always guarantee a positive change in healthy lifestyle resulting in smoking cessation:
We, I mean, we offer advice, but it is up to them to take it on board. I mean you continue to tell them stop smoking and, yeah, live healthily, reduce weight and exercise and, but if they take it on board, because not everyone is willing to accept these things, isn’t it? (GP 3)
Many GPs felt that the women in the ‘poorer’ pre-pregnancy health group did not perceive them as a source of information on preconception health.
we’ve got a massive Somali and Bangladeshi community that are having a lot of babies, but they don’t ever come and see me for advice or anything, they just have them … (GP 2)
Preconception care for men
The GPs were asked whether they provided preconception care to men. The general consensus was that preconception care focused on women’s health and was not an issue to raise with men unless subfertility was involved.
a handful of patients I see are men that come to see me [because] their partners are trying to get pregnant, it is usually just subfertility. (GP 7)
One mentioned that the only time he would see a male in the context of pregnancy was if he was with his partner in order to interpret for her.
the only time I would see a man for pre-pregnancy is actually when the women is booking in for an antenatal booking and the partner is coming in to interpret for them. (GP 4)
The interviews demonstrated that GPs did not offer specific preconception care to the general population of men except rarely in the context of a need for genetic counselling or screening for haemoglobinopathies when couples were planning pregnancy.
The GPs said that they would include men in the general healthy living advice they were giving to women such as smoking cessation and maintaining a healthy diet. This was extended to asking about the partner’s occupation in respect of any hazards that might affect his fertility.
if I’m giving counselling advice to a woman, I often transfer that to their partner as well, so […] only probably with the smoking and the drinking, the only thing I’ll extend to their partner is something along the lines of if they work with chemicals or anything like that. (GP 2)
It was felt that the health of women was more important and that more evidence-based information was needed to show the effectiveness of preconception interventions for men before this became more of a focus within consultations.
Barriers to providing preconception care
The barriers to GPs providing preconception care included women not planning their pregnancies; lack of perceived need, motivation, or attendance for health care; and time and financial constraints.
The GPs acknowledged that unplanned pregnancies or short inter-pregnancy intervals meant women do not seek advice on preconception health and there is a lack of time to improve health behaviours.
She hasn’t sought any pre-pregnancy advice, whether you would think of it as contraception or scheduled information or done any of the things, that she knows she [should] have done, […], so the whole thing about folic acid and all that, talking about lifestyle things … there’s a big hole there. (GP 6)
In general, the GPs specifically had concerns about the ethnic populations they served in regard to high levels of deprivation, language barriers, and cultural health beliefs that resulted in them not accessing health care before pregnancy.
… language may or may not be a barrier. Umm … they often don’t seek advice until they are pregnant. They don’t think about things, even if they are diabetic or have risk properties, they don’t tend to see that as an issue, or if they’re on medication […] they’re probably the people who have undiagnosed issues, whether it’s maybe things like sickle cell or thalassemia, or they’re carriers of genetic diseases, but they don’t really sort of voice these things. (GP 6)
GPs communicated both a lack of motivation from health care professionals to provide preconception care and a perceived lack of knowledge of the need for such a service from patients.
… lack of knowledge, education on the patient’s part, both health care professional and patients I think. One, we probably don’t provide enough … and patients don’t seek enough because they don’t understand enough … [of] what’s important. If you’re trying to deliver something that the general population doesn’t want, then you’re probably just wasting your time. (GP 6)
There was also concern that preconception care could be seen as a political issue with the ‘nanny state’ dictating personal behaviour.
There is something much wider and again anthropological about education and the need to prepare to have a family, all sounds a little bit, too patronizing, doesn’t it? One has to be a little bit careful not to overstep the political mark here. (GP 1)
GPs frequently perceived a lack of time and lack of financial incentives as a barrier to providing preconception care. GP consultations were already restricted to 10-minute appointments, and preconception care would increase consultation times.
If you have got a consultation […] you know you have only got 10 or 15 minutes, if you are dealing with a particular problem then to include other health promotion activities as part of that is going to be a barrier. (GP 5)
Ways of improving preconception care
Overall the GPs had a variety of opinions as to how preconception care can be improved, but raising awareness through continual education and training of both GPs and patients was seen as the main impetus together with media campaigns and financial incentives. Specific evidence-based guidelines for use in primary care and leaflets that could be offered to women and men were suggested.
I think it would be good to have more information out there, probably a standardized guideline for GP surgeries so what is the minimal we should be offering because I don’t think that we’re very consistent. (GP 6)
GPs viewed the media as an effective method to empower women to seek advice and improve healthy behaviour before pregnancy. Another proposal was a screening programme for preconception health from the age of 15.
GPs agreed that there were opportunities to increase the uptake of preconception care in primary care. They welcomed using the practice nurse to provide care to all women of child-bearing age during routine contraception checks and cervical screening.
80% of your lists are seen within three years so you are seeing these people all the time. So, I think, there is, primary care is a really good place to do this. So I think the opportunities are great actually. (GP 5)
The Quality and Outcomes Framework (QOF) was seen as both an opportunity currently and for a future intervention for preconception care. Targets such as cervical screening and smoking cessation could be used indirectly as an opportunity for pre-pregnancy health promotion.
So inadvertently […], we are always calling patients up all the time at random about their smoking history, making sure they have had their cervical smears […] we are inadvertently but not proactively screening women of child-bearing age to say, you know, come in for [preconception care]. (GP 7)
GPs suggested contacting at-risk women through disease registers to target those with higher risk of need for preconception care.
Targeting those, I guess if you do demographic studies on those particular at-risk groups that are more prone to problems and, going through your disease registers […] I guess it would be those groups that you want to target. (GP 7)
In addition, it was suggested that incentivizing preconception care through the development of suitable clinical indicators in QOF would improve provision. Financial incentives would then be paid for preconception care activity incorporated into routine appointments.
Discussion
Interviews with GPs raised seven key themes: Knowledge of preconception guidelines; Content of preconception advice; Who should deliver preconception care?; Targeting provision of preconception care; Preconception health for men; Barriers to providing preconception care; Ways of improving preconception care.
GPs’ knowledge and awareness of preconception guidelines was low. They tended to rely on knowledge gained from clinical experience, past training, and from patient information sources rather than from guidelines. At the time the interviews were carried out, as in other European countries (Citation16), there were limited specific guidelines available in the UK for preconception care. There were, however, guidelines within antenatal care management which covered folic acid supplementation, smoking cessation, and alcohol consumption prior to pregnancy. More recently in the UK, NICE (Citation8) has produced specific guidelines for women and men planning pregnancy, including guidance for both the healthy population and those with medical conditions, and this may lead to greater awareness amongst health professionals.
The GPs in our study did not feel they should be responsible for providing routine pre-pregnancy health and care advice; they considered nurses to have a more prominent role in delivery of care. Women of child-bearing age accessing the practice nurse for their contraception or routine cervical screening could be targeted, and importantly this concurs with women’s views of when preconception care can be appropriately raised (Citation17). Other studies have found low motivation from GPs to promote preconception care such as folate supplementation because of their own personal beliefs. In a study of Australian GPs (Citation18), some GPs did not promote use of folic acid as they held the belief that neural tube defects (NTDs) were so rare that folate was not needed or that folate did not always prevent NTDs anyway.
Although the GPs considered preconception care desirable in order to improve maternal and child health, they stated that there was little demand for the service. The small numbers of patients presenting for advice when trying to conceive have been identified by several other studies (Citation10,Citation18–20), with reasons including a lack of familiarity with the concept of preconception care, not knowing that GPs would provide such care, poor knowledge in relation to folic acid supplementation, and concerns of over-medicalization of a normal ‘life’ event.
GPs mainly provided care to women when prompted by fertility issues such as difficulty in conceiving or when patients asked for advice. Otherwise preconception care focused on women with pre-existing health conditions such as diabetes or epilepsy where there was a recognized concern regarding prescription of potentially teratogenic medication. Although identified as a priority by the Centre for Maternal and Child Enquires to prevent poor pregnancy outcomes (Citation21–23), this targeted approach risks a lack of priority being given to women and men who also may be in high need of preventive care. GPs identified that women with ‘poorer’ pre-pregnancy health and of greater deprivation were less likely to attend for health care and more likely to present at the surgery with unintended pregnancies. These women are less likely to take folic acid supplements and are more likely to participate in unhealthy behaviour such as smoking, drinking alcohol, and taking illicit drugs (Citation24–26).
GPs stated that not only their own awareness and knowledge needed to be improved to enable preconception care counselling, but awareness was needed in the general population by those that required care. Other studies (Citation11,Citation18) have found a low knowledge of behaviours related to preconception care and a need to increase general awareness. Women who receive preconception counselling are more likely to adopt healthier behaviours before pregnancy, leading to an improved diet, folic acid supplementation, and cutting down or stopping smoking (Citation10,Citation27). This reinforces the potential for the role of GPs in improving awareness and uptake of preconception care if interventions in primary care were provided. There was, however, a lack of motivation from GPs to provide specialist preconception services within their surgeries.
There is limited evidence on the implementation of preconception care strategies in primary care (Citation18), and studies are conflicting. Routine provision of preconception care for all women is supported by some (Citation28,Citation29), including starting in adolescence (Citation30), whilst the World Health Organization (WHO) suggests targeting specific groups (Citation7). A study (Citation31), in which GPs invited women to complete a risk assessment and to attend for preconception care, indicated that only a quarter of the women who became pregnant in the year afterwards had attended. The study protocol, however, excluded many women due to their adverse social circumstances, and it was concluded that it was important to develop ways to increase the range of women invited for the intervention. A study is currently targeting populations from specific neighbourhoods of the Netherlands which have high levels of deprivation in order to try to decrease the high levels of perinatal mortality. Community and general practice preconception interventions are to be implemented with the aim of achieving positive change in preconception risk behaviours (Citation32).
GPs have an important role in how preconception care should be delivered and in the allocation of resources to support and deliver this service effectively. A review by Shannon et al. (Citation33) identified primary care as the most common setting for preconception health service delivery; however, the authors also concluded that there is no agreed consensus on the best method to deliver care within primary care. It is possible that many strategies acting synergistically are needed to improve service delivery. This is consistent with findings from a qualitative study (Citation11), which showed that women who take a micronutrient supplement are more likely to invest in their preconception health and care. The authors identified women belonging to three groups—the ‘prepared’ group, the ‘poor knowledge’ group, and the ‘absent pre-pregnancy’ group—and argued that different preconception strategies are needed to target different women.
Men were found not to attend the surgery for pre-pregnancy advice unless subfertility was a concern. The lack of interest and practice of preconception care for men was consistent in our study and in line with other research (Citation34); the majority of the GPs did not view men’s preconception health as a priority. Studies show that men have a lower knowledge of preconception care and are less likely to see their GP for preconception interventions (Citation35). This is congruent with men’s limited involvement in reproductive and sexual health for preventive health care in general (Citation36). However, the importance of preconception care for men has been highlighted by a US study (Citation37) which found that 60% of men aged between 15 and 64 years have a need for preconception care with concerns of obesity, binge drinking, use of illicit substances, and their high risk for sexually transmitted infections. Few had attended screening or preventive services, and there was the opportunity to increase uptake of such interventions. There is growing evidence that men’s health at conception plays a significant role in pregnancy and neonatal outcomes through direct and epigenetic influence on the health of spermatozoa (Citation38,Citation39). Greater attention needs to be given to involving men in preconception care by reviewing factors such as lifestyle choices (Citation8,Citation40), medical conditions and medications (Citation17,Citation41), environmental exposures (Citation40,Citation42), and screening for infection (Citation40).
GPs discussed barriers to providing care, which centred on need, awareness, and capacity. In agreement with other studies (Citation10,Citation43), limited consultation time and lack of resources were seen as the main barriers to providing care. Currently there is no direct financial reimbursement to GPs for integrating preconception care into consultations with women of reproductive age. Although GPs felt that financial incentives were needed to increase the provision of preconception care, evidence for using incentivized frameworks has been found to be debatable. Such frameworks have improved asthma and diabetes care in the short term (Citation44), but in a qualitative pilot study, aimed at increasing antismoking advice to smokers by GPs (Citation45), it was found that GPs changed the way they documented smoking advice to meet the incentives rather than significantly give more advice in clinical practice.
Strengths and limitations of the study
This is, to our knowledge, the first paper that considers GPs’ perspectives on providing preconception care to a general population. The study was undertaken as part of a larger publicly funded study of preconception care in England, and it is an exploration of GPs’ views rather than an unbiased evaluation of preconception care. The study does not provide information on the frequency with which women receive care from their GPs or the effectiveness of preconception care provided. Interviews were undertaken by three researchers which may prevent bias from personal interest, but the context of the study and knowledge that they were from the ‘Institute of Women’s Health’ may have influenced the GPs’ conversation. The GPs appeared to give honest opinions in regard to their knowledge base and views of service provision, for example in confessing to not having read preconception guidelines, which enhanced the trustworthiness of the findings.
The study was carried out in a borough of London where a there is a disparity of wealth and a large ethnic minority population and therefore may be different to many other areas of the UK. However, the findings have similarities to those of other UK studies examining the patient perspective of provision and uptake of care (Citation17,Citation19), which agree that GPs could provide more information and be more proactive in respect of preconception care provision. In addition, we found that GPs were more likely to provide preconception care to women with medical conditions, and this targeted approach highlighted issues similar to those found by Mortagy et al. (Citation46) who interviewed GPs and secondary care health professionals focusing on women with diabetes.
Conclusion
This qualitative study set out to examine GPs’ knowledge, attitudes, and views towards preconception health and care in the general practice setting. The findings provide an insight into how care is currently delivered in primary care, and the GPs described diverse patient groups with very different health needs before pregnancy. A lack of both knowledge and demand for preconception care was found, and, although reaching women before they are pregnant was seen as important, it was not a responsibility that could be adequately met by GPs. Strategies need to be developed to increase awareness in women with ‘poorer’ pre-pregnancy health, who are more likely to have unintended pregnancies, and to find ways to engage men in preconception care. The role of education and of nurses in improving preconception health was acknowledged but remains under-developed in primary care.
Declaration of interest
The authors report no conflicts of interest.
References
- Atrash H, Jack BW, Johnson K. Preconception care: a 2008 update. Curr Opin Obstet Gynecol. 2008;20:581–9.
- World Health Organization [Internet]. WHO: Preconception care: Maximizing the gains for maternal and child health. Policy brief. c2013. Available from: http://www.who.int/maternal_child_adolescent/documents/preconception_care_policy_brief.pdf [cited 2016 Jul 6].
- Barker DJ. Mothers, babies, and health in later life. Elsevier Health Sciences; 1998.
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–93.
- Gillman MW. Epidemiological challenges in studying the fetal origins of adult chronic disease. Int J Epidemiol. 2002;31:294–9.
- Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73.
- World Health Organization [Internet]. WHO: Global action plan for the prevention and control of noncommunicable disease 2013–2020. c2013. Available from: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf [cited 2016 Jul 6].
- National Institute for Health and Care Excellence (NICE) Preconception – advice and management [Internet]. Clinical knowledge summaries. NICE 2013. Available from: http://cks.nice.org.uk/pre-conception-advice-and-management#!topicsummary [cited 2016 Jul 6].
- Draycott T, Lewis G, Stephens I. Confidential enquiry executive summary. Br J Obstet Gynaecol. 2011;118:12–21.
- Stephenson J, Patel D, Barrett G, Howden B, Copas A, Ojukwu O, et al. How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PLoS One. 2014;9:e103085.
- Barrett G, Shawe J, Howden B, Patel D, Ojukwu O, Pandya P, et al. Why do women invest in pre-pregnancy health and care? A qualitative investigation with women attending maternity services. BMC Pregnancy Childbirth. 2015;15:236.
- Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description—the poor cousin of health research? BMC Med Res Methodol. 2009;9:1.
- Morse JM. Determining sample size. Qual Health Res. 2000;10:3–5.
- NVivo 10, QSR International. Available from: http://www.qsrinternational.com/products_nvivo.aspx [accessed 2016 Jul 6].
- Ritchie J, Lewis J, Nicholls CM, Ormston R, editors. Qualitative research practice: a guide for social science students and researchers. 2nd ed. London: Sage; 2013.
- Shawe J, Delbaere I, Ekstrand M, Hegaard HK, Larsson M, Mastroiacovo P, et al. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur J Contracept Reprod Health Care. 2015;20:77–87.
- Tuomainen H, Cross-Bardell L, Bhoday M, Qureshi N, Kai J. Opportunities and challenges for enhancing preconception health in primary care: qualitative study with women from ethnically diverse communities. BMJ Open. 2013;3:e002977.
- Mazza D, Chapman A, Michie S. Barriers to the implementation of preconception care guidelines as perceived by general practitioners: a qualitative study. BMC Health Serv Res. 2013;13:1.
- Mazza D, Chapman A. Improving the uptake of preconception care and periconceptional folate supplementation: what do women think? BMC Public Health. 2010;10:1.
- Wallace M, Hurwitz B. Preconception care: who needs it, who wants it, and how should it be provided? Br J Gen Pract. 1998;48:963–6.
- Lewis GH. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006–08. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG. 2007;118(Suppl 1):1–203.
- NICE guidance on diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. NICE clinical guideline 3. c2015. Available from: https://www.nice.org.uk/guidance/ng3 [accessed July 6, 2016].
- NICE guidance on epilepsies diagnosis and management. NICE clinical guideline CG137 c2012. Available from: https://www.nice.org.uk/guidance/cg137 [accessed July 6, 2016].
- Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79:194–8.
- Dott M, Rasmussen SA, Hogue CJ, Reefhuis J. Association between pregnancy intention and reproductive-health related behaviors before and after pregnancy recognition, National Birth Defects Prevention Study, 1997–2002. Matern Child Health. 2010;14:373–81.
- McCrory C, McNally S. The effect of pregnancy intention on maternal prenatal behaviours and parent and child health: results of an Irish cohort study. Paediatr Perinat Epidemiol. 2013;27:208–15.
- Temel S, van Voorst SF, Jack BW, Denktaş S, Steegers EA. Evidence-based preconceptional lifestyle interventions. Epidemiol Rev. 2014;36:19–30.
- Czeizel AE. Ten years of experience in periconceptional care. Eur J Obstet Gynaecol Reprod Biol. 1999;84:43–9.
- Moos MK, Bangdiwala SI, Meibohm AR, Cefalo RC. The impact of a preconceptional health promotion program on intendedness of pregnancy. Am J Perinatol. 1996;13:103–8.
- Curtis M, Abelman S, Schulkin J, Williams JL, Fassett EM. Do we practice what we preach? A review of actual clinical practice with regards to preconception care guidelines. Matern Child Health. 2006;10:53–8.
- Elsinga J, Van der Pal-de Bruin KM, Le Cessie S, de Jong-Potjer LC, Verloove-Vanhorick SP, Assendelft WJ. Preconception counselling initiated by general practitioners in the Netherlands: reaching couples contemplating pregnancy [ISRCTN53942912]. BMC Fam Pract. 2006;7:1.
- van Voorst SF, Vos AA, de Jong-Potjer LC, Waelput AJ, Steegers EA, Denktas S. Effectiveness of general preconception care accompanied by a recruitment approach: protocol of a community-based cohort study (the Healthy Pregnancy 4 All study). BMJ Open. 2015;5:e006284.
- Shannon GD, Alberg C, Nacul L, Pashayan N. Preconception healthcare delivery at a population level: construction of public health models of preconception care. Matern Child Health. 2014;18:1512–31.
- Frey KA, Engle R, Noble B. Preconception healthcare: what do men know and believe? J Mens Health. 2012;9:25–35.
- Mitchell EW, Levis DM, Prue CE. Preconception health: awareness, planning, and communication among a sample of US men and women. Matern Child Health. 2012;16:31–9.
- Sternberg P, Hubley J. Evaluating men’s involvement as a strategy in sexual and reproductive health promotion. Health Promot Int. 2004;19:389–96.
- Choiriyyah I, Sonenstein FL, Astone NM, Pleck JH, Dariotis JK, Marcell AV. Men aged 15–44 in need of preconception care. Matern Child Health. 2015;19:2358–65.
- Moss JL, Harris KM. Impact of maternal and paternal preconception health on birth outcomes using prospective couples’ data in Add Health. Arch Gynecol Obstet. 2015;291:287–98.
- van der Zee B, de Wert G, Steegers EA, de Beaufort ID. Ethical aspects of paternal preconception lifestyle modification. Am J Obstet Gynecol. 2013;209:11–16.
- Frey KA, Navarro SM, Kotelchuck M, Lu MC. The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol. 2008;199:S389–S95.
- Agbaje IM, Rogers DA, McVicar CM, McClure N, Atkinson AB, Mallidis C, et al. Insulin dependant diabetes mellitus: implications for male reproductive function. Hum Reprod. 2007;22:1871–7.
- Jensen TK, Bonde JP, Joffe M. The influence of occupational exposure on male reproductive function. Occup Med. 2006;56:544–53.
- Jack BW, Culpepper L, Babcock J, Kogan MD, Weismiller D. Addressing preconception risks identified at the time of a negative pregnancy test. J Fam Pract. 1998;47:33–8.
- Campbell SM, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Engl J Med. 2009;361:368–78.
- Coleman T, Wynn AT, Stevenson K, Cheater F. Qualitative study of pilot payment aimed at increasing general practitioners’ antismoking advice to smokers. BMJ. 2001;323:432.
- Mortagy I, Kielmann K, Baldeweg SE, Modder J, Pierce MB. Integrating preconception care for women with diabetes into primary care: a qualitative study. Br J Gen Pract. 2010;60:815–21.