Abstract
Clinically, oedema is described as an abnormal build-up of interstitial fluid in the body that is enough to produce palpable swelling. Its assessment offers valuable information to clinicians as this can inform management interventions; and help monitor adherence to home therapy programmes and activity levels. The aim of this systematic review is to establish the utility of 3D scanning technologies in the assessment of lower limb oedema. A computer-based search was completed in October 2020. Four studies were identified which utilised a 3D scanner to measure lower limb oedema. A review of the studies found very little evidence to support the efficacy of 3D laser scanning technology, although they show that the use of the technology is feasible. Current methods of lower leg oedema measurement have issues with reliability, practicability and time taken. There is a need for future studies to validate new methods of oedema assessment using technologies such as 3D laser scanning.
1. Introduction
Clinically, oedema is described as an abnormal build-up of interstitial fluid in the body that is enough to produce palpable swelling [Citation1]. Oedema occurs mainly in the lower limb (80% of cases) but can also happen in other parts of body including trunk, face, arm and external genitalia [Citation2]. The formation of oedema may have an impact on overall functionality of an individual including joint range of motion, soft tissue mobility, function and strength. Studies [Citation2] have shown that these factors are associated with longer length of stay, increased number of outpatient appointments, delay in patient’s recovery and return to normal activities of daily living. Thus, an objective assessment of oedema after surgery or trauma can offer insight to clinicians about the efficiency of oedema management interventions, compliance to home therapy programmes and activity levels [Citation3].
Different measures for assessing lower limb oedema are available for clinical use. The circumferential or figure of eight method [Citation4] using a tape measure, and volumetric water displacement (WD) [Citation5], are methods that have been used since the 1950s. However, their clinical usage appears to be reducing due to practical aspects, questions in regards to their accuracy, and the length of time that is required to carry out the assessment [Citation6]. An alternative for measuring lower limb volume is optometry [Citation7]. This technique uses infra-red rays to measure limb reference points from which the volume is calculated electronically. The volume of the reference point can then be calculated to provide an estimate of limb volume mainly in the side lying position. Despite a satisfactory level of reproducibility [Citation8], optometry requires reflective markers to identify reference points which can be time consuming to use and are not always practical in day-to-day clinical use. Furthermore, measurements are taken in the side lying position, which is not ideal for determining the volume of the lower limb with regards to venous or lymphatic disease.
More recently, three-dimensional (3D) imaging technology has become available, offering a quick method for quantifying lower limb volume. An advantage of 3D imaging is that the circumference and volume of body segments and/or the entire body can be measured vertically and noninvasively. Whilst this method is not routinely used by lower limb therapists to measure oedema, its potential merits a more in depth look at the various 3D systems that are currently used in clinical trials for measuring lower limb oedema. Therefore, the aim of this systematic review is to establish the utility of 3D scanning technologies in the assessment of lower limb oedema.
2. Methods
2.1. Searching strategy
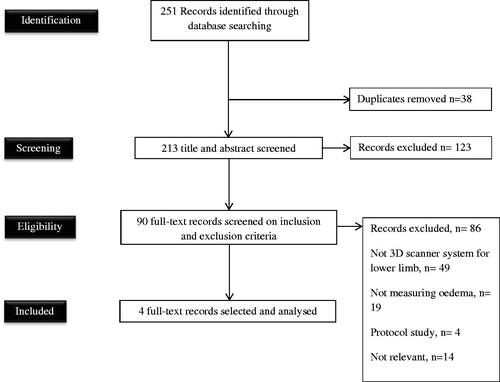
This review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Citation9]. A computer-based search was completed in October 2020 using the mySearch Database (Bournemouth University), which includes the Cochrane Database of Systematic Reviews library, CINAHL Complete®, Science Citation Index and Medline®. The search was for studies published in the English language up to October 2020, in an adult population with lower limb oedema. Search strategy terms are outlined in .
Table 1. Literature search strategy.
One reviewer (SB) read the titles of all citations retrieved from the electronic database searches and removed all citations which were not related to the assessment of lower limb oedema. Abstracts of the remaining articles were screened to check for eligibility by two reviewers (SB and TI) until only four papers remained (see for flowchart). Any disagreements between reviewers were discussed with TW and resolved by consensus. Full text articles were obtained for all abstracts meeting the inclusion criteria.
2.2. Data extraction process
SB extracted data to a standardised table, details found in .
Table 2. Summary of articles.
2.3. Data quality
The Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) [Citation14] tool was used to assess the risk of bias. ROBINS-I includes seven domains including confounding, selection of participants into the study, classification of interventions, deviations from the intended interventions, missing data, measurement of outcomes, and selection of the reported result. The categories for risk of bias judgements for ROBINS-I are “low risk”, “moderate risk”, “serious risk” and “critical risk” of bias [Citation14].
3. Results
Four studies were identified (see for flowchart) which utilised a 3D scanner to measure lower limb oedema.
A total of 163 participants were included in the four studies, with sample size ranging from 18 to 90. Participants had a range of musculoskeletal, post orthopaedic surgery, venous inefficiency, heart or obesity conditions. One study [Citation13] used only healthy female participants when assessing the reliability of the 3D scanning system.
Two systems for assessing oedema using a 3D scanner were used: platform-based standing and hand-held. Two studies [Citation11,Citation12] used tape measure, and one [Citation10] used WD volumetry as a “gold standard method” for assessing reliability of the 3D scanners.
3.1. Hand-held 3D scanner
Mestre et al. [Citation10] performed 3D laser scanning using a Handyscan 3D REVscan system. REVscan is a self-positioning laser scanner with dynamic referencing for acquisition and real-time 3D reconstruction of the lower limb volume. Two independent observers performed either one or two laser scans, and results were tested for intra- and interobserver reproducibility and compared with WD volumetry. Data showed high interobserver reproducibility and reliability. However, the scanner overestimated the volume by 90 ml in contrast to WD. The authors suggested that the main reason for this may be to do with the different posture: the patient standing upright for WD measurement whereas being seated for 3D laser scanning. Mestre et al. [Citation10] commented that one of the main limitation of this technique was that the scanning lasted 3–5 min, and some participants struggled to keep perfectly still. Moreover, automatic volume calculation from 3D laser scanning data failed in one patient with a large limb (about 7300 ml) size. The size of the limb was not in itself an obstacle for 3D laser scanning, but its irregular shape required more varied angles of incidence to avoid local shadowing from skin folds.
Cau et al. [Citation12] performed 3D laser scanning on a group of obese females using a Rodin4D O&P scanner. This is also a self-positioning laser scanner, but it does not require referencing markers for data acquisition. The circumferences and volume of the lower limb were measured using a normal tape and the 3D laser scanner. Measurements were taken with an interval of 5 cm from the centre of patella. Results showed a statistically significant differences between the two methods. The investigators suggested that the shape of the limb was the main cause of the disagreement between the data. This is because in lean participants the leg shape is anatomically defined. In the obese group, the gibbousness and uneven limb shapes can be overlooked by the tape measurement technique. Therefore, the 3D laser scanner may be more suitable than the tape measure for all body shapes as it is better at detecting uneven limb shapes.
3.2. Platform-based standing 3D scanner
Hayn et al. [Citation11] introduced a 3D camera-based scanning system to measure leg oedema in patients with heart failure. 3D images of legs were taken whilst the participant was in a standing position and geometric parameters were extracted semi-automatically from the images. Manual image preparation and marker selection took less than 15 min per image. Intra-subject variability was evaluated. The study concluded that the system is reliable and cost effective in detection of oedema and could be offered as a home monitoring system to patients with a heart condition. However, the study suffered from very complicated methodology resulting in the authors admitting that the study data could only be reproduced with limited reliability.
In Hirai et al.’s [Citation13] study, oedema was evaluated with a 3D measurement system called GRASP. A four directional grid pattern of halogen lights scanned calf, ankle and foot from left, right and top and bottom. After a 3D image of the superficial configuration of the leg was built, the circumference and volume of the leg were calculated automatically using a computerised analysis system. The findings of the study concluded that the scanner is a reliable and useful tool for evaluating oedema at the calf and ankle.
Despite a brief clarification on the reproducibility of the methodology, there were many confounding issues on the foot positioning. The authors reported that one of the main reasons for poor reproducibility of the foot results is the anatomy of the foot. They reported that the project pattern method may not be best suited for uneven surfaces such as foot which has superficial veins and wrinkles.
3.3. Risk of bias
The studies were assessed using the ROBINS-I risk of bias tool. They were all judged to be at serious risk as there were issues with bias in more than one domain.
4. Discussion
The aim of this systematic review was to establish the quantity and quality of the evidence on the utilisation of 3D scanning technology in assessing lower limb oedema. The systematic search found no suitable randomised controlled trials, and only four comparative studies that assessed the utility of 3D scanners for the assessment of lower limb oedema. The studies were all judged to be at a serious risk of bias.
Despite the lack of consistency in the reported leg components and positioning used, in general all the studies proposed that 3D scanning technology may be a reliable and useful tool for evaluating leg oedema. However, it appears that handheld laser scanners have poorer reliability compared to the standing scanners because participants struggle to keep perfectly still whilst being scanned. This was one of the main reasons Mestre et al. [Citation10] reported an overestimation of 90 ml for limb volume in contrast to WD. However, whilst a lightweight and portable version of the standing 3D scanner exists, the standard version would require a permanent space in a clinical setting and costs between £15,000 and £150,000 depending on the model [Citation15]. The handheld scanners are available at a much lower cost of between of £1000 and £10,000 [Citation15], and so in some settings this lower cost may justify the loss of some accuracy. Therefore, it remains to be decided whether the cost of equipment justifies the accuracy offered by the standing 3D scanning system [Citation16,Citation17].
Two of the studies included [Citation11,Citation12] employed methodologies in which bony landmark reference points were selected. However, in areas where bony landmarks do not exist, such as the mid-thigh, identifying an appropriate reference point in the 3D image may cause inter-user variability, even when reference points are well documented [Citation10]. In addition, there was a lack of focus by all of the papers on the timing of the evaluation. Standardisation of the timing of measurement is important due to diurnal variation, as there is a natural increase in leg volume throughout the day.
The standing laser scanners are reported as requiring 1–3 min for an automated scan, whereas the handheld device requires 5–20 min for a full lower limb scan and a further 3 min for the 3D image to be generated. The average time reported for a WD assessment is around 20–30 min and for tape measurement it is 15–20 min [Citation16,Citation17]. The standing laser scanner technique therefore offers the quickest assessment time and is more reliable than the handheld scanner as it has less movement artefact. The advantage of WD volumetry is the direct measurement of objects with an irregular form. However, in addition to being time consuming, this method has potential logistical and hygiene difficulties, and is not always suitable for taking measurements in certain clinical settings and patient groups. For example, measuring the lower limb volume of patients in the immediate postoperative period who have restricted mobility [Citation17]. A limitation of the tape measure technique is that it does not automatically provide a clinician with a measurement of limb volume, as measures require further calculations using a formula such as Frustum Sign Model [Citation18]. Moreover, there are issues [Citation17] with the reliability of this technique and it is not recommended for clinical assessment [Citation17]. However, this method has its advantages because it is much faster than WD volumetry, and in many cases (such as routine clinical care) its accuracy may be sufficient.
It is worth noting that none of the studies report on the economic aspects of using 3D scanning technology. However, it is evident that a capital cost of 3D laser scanner is far greater than the cost to complete measurements using WD or a tape measure. Therefore, it is necessary to acknowledge that despite the potential benefits that 3D scanners may provide (i.e., accuracy), the utilisation of 3D scanning technologies may be more suited to clinical research settings where accuracy is a key factor and funding may be available. Their current cost means that at the present time, it is unlikely that they will be widely adopted in health care systems.
Given the acknowledged and prohibitive current cost of 3D scanning devices, a range of other techniques that can be used to quantify leg oedema have recently attracted attention. These techniques have been explored in an effort to more accurately measure oedema, but do not directly measure limb volume. Examples include, high frequency ultrasound imaging, which can be used to produce high resolution images of the dermis. This permits accurate determination of changes in oedema by evaluating increases or decreases in dermal thickness [Citation19]. Also, electrical bioimpedance measurement has been reported as a reliable bedside measure for the evaluation of oedema [Citation20]. This technique uses a single-frequency, low voltage electric current to determine extracellular fluid volume [Citation20,Citation21]. In contrast to the 3D scanning techniques, it has advantages of not requiring clothing to be removed; however, there are often reliability issues, calculations are based on non-clinical patient algorithms, and it does not directly measure limb volume.
In summary, 3D laser scanning technology offers a solution for visualising and quantifying lower limb volume, and standing scanners offer advantages over handheld devices. Studies have reported that 3D scanners are best suited for measuring limbs where there is swelling, and the shape of the limb is uneven. Furthermore, in methodologies such as WD volumetry or tape measure use, the opportunities for observer bias and human error in measurement are great. In contrast, 3D laser scanning technology can provide better reproducibility; however, the comparative cost of equipment may currently be prohibitive for routine clinical use.
4.1. Recommendation for future research
As 3D laser scanning technology research for oedema evolves, the challenges outlined that prevent routine clinical use need to be addressed before these devices are broadly adapted as an assessment tool. Randomised-controlled trials are clearly needed, and such studies must seek to confirm that devices; offer an improved accuracy of measurement against routinely used clinical measures, ensure that measurements are not distorted due to motion, are quick to use, are cost effective, and have built in software for quick results and ease of use.
5. Conclusions
3D laser scanning technology offers a quick, efficient method of visualising and quantifying the lower limb. However, this review finds very little evidence to confirm its efficacy. The small numbers of studies do, however, show it is feasible, and like most new technologies it will improve and become more affordable over time. In addition, current methods of lower leg oedema measurement have problems in standardising measurement conditions. There is a need for future studies to validate new methods of oedema assessment using 3D laser scanning technologies.
Ethical approval
As this study utilised information that was available in the public domain and there was no interaction with patients or retrieval of personal data, ethics approval was not required and therefore not sought.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Kerchner K, Fleischer A, Yosipovitch G. Lower extremity lymphedema update: pathophysiology, diagnosis, and treatment guidelines. J Am Acad Dermatol. 2008;59(2):324–331.
- Szuba A, Rockson SG. Lymphedema: classification, diagnosis and therapy. Vasc Med. 1998;3(2):145–156.
- Do JH, Choi KH, Ahn JS, et al. Effects of a complex rehabilitation program on edema status, physical function, and quality of life in lower-limb lymphedema after gynecological cancer surgery. Gynecol Oncol. 2017;147(2):450–455.
- Pellecchia GL. Figure-of-eight method of measuring hand size: reliability and concurrent validity. J Hand Ther. 2003;16(4):300–304.
- Thulesius O, Norgren L, Gjöres JE. Foot-volumetry, a new method for objective assessment of edema and venous function. Vasa. 1973;2(4):325–329.
- Miller LK, Jerosch-Herold C, Shepstone L. Clinical assessment of hand oedema: a systematic review. Hand Ther. 2017;22(4):153–164.
- Tierney S, Aslam M, Rennie K, et al. Infrared optoelectronic volumetry, the ideal way to measure limb volume. Eur J Vasc Endovasc Surg. 1996;12(4):412–417.
- Engelberger RP, Blazek C, Amsler F, et al. Reproducibility and day time bias correction of optoelectronic leg volumetry: a prospective cohort study. BMC Med Res Methodol. 2011;11(1):138.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341.
- Mestre S, Veye F, Perez-Martin A, et al. Validation of lower limb segmental volumetry with hand-held, self-positioning three-dimensional laser scanner against water displacement. J Vasc Surg Venous Lymphat Disord. 2014;2(1):39–45.
- Hayn D, Fruhwald F, Riedel A, et al. Leg edema quantification for heart failure patients via 3D imaging. Sensors. 2013;13(8):10584–10598.
- Cau N, Corna S, Aspesi V, et al. Circumferential versus hand-held laser scanner method for the evaluation of lower limb volumes in normal-weight and obese subjects. J Nov Physiother. 2016;6(4):2.
- Hirai M, Iwata H, Niimi K, et al. Improvement of a three-dimensional measurement system for the evaluation of foot edema. Skin Res Technol. 2012;18(1):120–124.
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
- Zeraatkar M, Khalili K. A fast and low-cost human body 3D scanner using 100 cameras. J Imaging. 2020;6(4):21.
- Rabe E, Stücker M, Ottillinger B. Water displacement leg volumetry in clinical studies – a discussion of error sources. BMC Med Res Methodol. 2010;10(1):5.
- Kaulesar Sukul DM, den Hoed PT, Johannes EJ, et al. Direct and indirect methods for the quantification of leg volume: comparison between water displacement volumetry, the disk model method and the Frustum Sign Model method, using the correlation coefficient and the limits of agreement. J Biomed Eng. 1993;15(6):477–480.
- Chromy A, Zalud L, Dobsak P, et al. Limb volume measurements: comparison of accuracy and decisive parameters of the most used present methods. Springerplus. 2015;4(1):707.
- Eisenbeiss C, Welzel J, Eichler W, et al. Influence of body water distribution on skin thickness: measurements using high-frequency ultrasound. Br J Dermatol. 2001;144(5):947–951.
- Pichonnaz C, Bassin J-P, Lécureux E, et al. Bioimpedance spectroscopy for swelling evaluation following total knee arthroplasty: a validation study. BMC Musculoskelet Disord. 2015;16(1):100.
- Rutkove SBJM. Electrical impedance myography: background, current state, and future directions. Muscle Nerve. 2009;40(6):936–946.