Abstract
Evidence suggests that much of the digital technology available and provided to older adults to enable self-management of long-term conditions is under-utilised. This research focuses on three conditions prevalent amongst older adults: diabetes, dementia and chronic kidney disease and explores the individual enablers and barriers to the use of digital self-management technology. The paper reports findings from a series of three systematic reviews of qualitative research (qualitative evidence syntheses). These reviews informed the design of a Delphi study. The first round of the Delphi involving 15 expert interviews is reported. The findings highlight common themes across the three conditions: how technology is used; barriers to use; assessing individual needs when selecting technology; support requirements; multi-functional self-management technologies; trust, privacy and data sharing; achieving accessible and aspirational design. Some emerging recommendations have been suggested to guide the design, and provision of technology to older adults. These will extended and refined through subsequent rounds of the Delphi method.
1. Introduction
Self-management technology that has proven to be clinically effective can remain underused, or abandoned by older users of health services [Citation1]. Examples of self-management technologies include home dialysis machines, alerts systems, smart insulin pens, glucometers, intelligent medication dispensers, voice reminders, electronic memory aids, etc. Whilst clinical trials and evaluations may prove the technology works, they do not always ensure the technology is accepted and can, and will, be used [Citation2]. Unused technology can lead to poor management of health, lower quality of life and further medical complications [Citation3]. As a result, older people may not experience the benefits offered, manage their condition less effectively [Citation4], whilst wasted equipment and increased treatment costs places a heavy financial burden on the healthcare system [Citation5].
Smartphones and tablets continue to offer increasing functionalities (such as geographical positioning, sensors, computing power, and interactivity). Collectively they have transformed the way mHealth (services that support personal healthcare through the use of mobile technologies) interventions support chronic disease management and self-management. Examples include access to, and ownership of, electronic records, self-monitoring and record-keeping, contact with the health professional team, patient education and information, activity planning for daily living and devices to stimulate activity, or cognition.
Research has explored the systematic factors, barriers and enablers to the development, adoption and uptake of technology in health and social care [Citation6]. Despite this, issues remain at the individual level in terms of provision, acceptance and use, especially amongst older adults. We sought to better understand these reasons in relation to the self-management of chronic kidney disease (CKD), dementia and diabetes; three common conditions that manifest themselves in a senior population (e.g., 65 years old plus) [Citation7–9]. Support for self-management can be assumed to share similarities across these three conditions (for example the need to manage medication, following guidelines, make decisions). At the same time, each condition has a specific disease profile that imposes extra requirements on any supportive technology, person who is self-managing and their social support network.
This research aimed to identify the individual enablers and barriers to the use of digital technology for the self-management of diabetes, dementia and chronic kidney disease by older adults. In the longer term, the team seek to develop recommendations and interventions for practitioners and technology developers to guide the design of, and provision of technology to older adults. As outlined below three systematic reviews of qualitative research (qualitative evidence syntheses) were undertaken; one focussed on each of chronic kidney disease, diabetes and dementia. These reviews sought to inform a Delphi study to build consensus through systematic collection and aggregation of expert views on the review findings.
2. Systematic reviews of qualitative studies
The value of theory-based, document-driven, and user-centred frameworks in the development of digital technology is increasingly recognised [Citation10,Citation11]. Although the use of literature reviews in intervention development is well established, fewer instances make use of systematic reviews, and even more so of systematic reviews of qualitative research (qualitative evidence syntheses) [Citation12]. Methods for reviewing qualitative evidence are now well developed with three principal methods to the fore; thematic synthesis, framework synthesis and meta-ethnography. In planning to inform the development of digital technology for the self-management of long-term conditions by older adults, we recognised that relevant research would likely lack the richness required for an interpretive method such as meta-ethnography. However, the team wanted to harness the value of available theoretical frameworks and this positively affirmed the usefulness of a framework synthesis-based approach [Citation13,Citation14]. The aim was to identify the individual enablers and barriers to the use of digital technology for the self-management of long-term conditions by older adults in the highly prevalent conditions of diabetes, dementia and CKD through three reviews.
2.1. Review process
An outline of the seven-step review process [Citation13] is briefly characterised in .
Table 1. Seven step framework synthesis process.
Searches were undertaken for studies published in English between January 2011 and December 2020 to reflect current technologies. The following databases were searched, as well as publications identified through reference checking: PubMed/MEDLINE, PsycINFO, EMBASE, CINAHL, Scopus, the Web of Science indexes. The review only considered studies with qualitative outcome and design and where the majority of participants included were 65 years or older.
Abstracts identified by the searches were evaluated and potentially eligible articles selected for full text review. A pilot selection exercise was undertaken by two reviewers using a random sample and the criteria amended as required. Any discrepancies were resolved by discussion between the reviewers.
The team selected a framework based on the Seniors Technology Acceptance Model [Citation15] as a structure against which to extract data and analyse results. Data were extracted using a standardised data extraction table to assign the main themes to the predetermined categories. The extraction included a mix of descriptive variables about the subjects (age group, gender, clinical condition, rural/urban residential area, income, and level of management) and the study (place of publication, number of participants, technology type). The populated framework was used to code the key themes from each of the studies to determine how each of them relate to one another.
By conducting the three syntheses as a sequential series, the team was able to build in incremental learning from the methods and the findings of successive reviews, and focus on new, unique and emerging findings rather than restating common features. We started with CKD because it was conceptually the most straightforward with a relatively manageable literature. We then proceeded to dementia, with the added complexity of cognitive difficulties. Finally, the third of the reviews, in diabetes, was principally used to confirm and augment the developing framework and, in view of the sizable literature, was constrained within a review of reviews (“mega-aggregation”) [Citation14]. captures the characteristics of the three reviews.
Table 2. Overview of study selection process.
The methods of the three reviews are available in a formally registered open access protocol: Identifying individual enablers and barriers to the use of digital technology for the self-management of long-term conditions by older adults (PROSPERO 2021 CRD42021237745 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021237745).
2.2. Common issues across conditions
The in-depth findings will be extensively documented in a set of three condition specific publications. This paper briefly characterises some of the principal themes across the three syntheses.
2.2.1. Challenges attributable to ageing
An older person’s use of technology is determined by multiple factors including their previous knowledge, age, the symptoms and severity of their condition, the therapies that they are receiving, motivation, digital literacy, levels of support, language and communication skills, age-related mobility or cognitive restrictions, and behavioural choices [Citation15,Citation16]. Their need for information may also be influenced by their support networks, including their significant others, and their relationship with their health professional team [Citation16].
Surprisingly little attention is paid to functional difficulties in the use of technology attributable to ageing itself (e.g., manual dexterity and vision difficulties) [Citation17,Citation18]. The focus of studies is typically on the condition itself which may or may not be directly associated with ageing. Of greater importance seems to be generational aspects associated with ageing – a lack of intuitive knowledge about how smart technologies operate, an absence of a willingness to learn new skills, and a lack of motivation to use technology to address the challenges faced [Citation19]. Not to be overlooked is the importance of co-morbidities or other pertinent symptoms; for example, chronic disease may also be associated with fatigue, which may impair prolonged use of mobile apps. A recent qualitative scoping review on the use of smartphone technologies confirmed a relative lack of a gerontological focus in studies of smart device usage [Citation20].
2.2.2. Use of devices for self-management
The findings for the three reviews reflected use of smart devices in line with eight self-management strategies identified by Kim and Lee 2017 [Citation20] (see ). Self-monitoring, automated feedback [Citation19,Citation21,Citation22], and patient education appeared to be the most commonly used self-management support strategies [Citation1]. Dementia carried a distinctive use; unlike the other two conditions, in the importance of cognitive stimulation in the form of games, puzzles, etc.
Table 3. Identified self-management strategies (adapted from [Citation20]).
2.2.3. Attitudes towards technology
Relatively few older people are interested in technology for its own sake [Citation23]. Typically, they want to know what activities the technology will help them to carry out. Many older people are aware that technologies have a time cost; particularly during the “run in” towards gaining skill and awareness of the new technology [Citation24]. They are much more likely to contemplate use of a new technology if it supports them in an activity in which they have previously enjoyed participating. For many “mundane” activities of daily living, older people are not interested in using technology at all – where they are able to continue to achieve what they want from low-tech or non-technological resources then these will readily suffice [Citation25].
2.2.4. Denial of a need
In connection with chronic disease management, many older people will try to continue managing as they have done previously until they are forced to recognise their dependence upon technology and/or other people [Citation23–25]. The patient may not accept that they have a problem, either in terms of the condition itself, or in regards to the severity of their condition or their own susceptibility to it [Citation25]. They often seek to continue to live life as normal, not necessarily as a form of denial but as an active coping strategy.
2.2.5. Acceptance of the need for technology
Effective use of self-management technology requires the patient to accept that they have a particular need that the technology can meet. Generically, two types of need satisfy this requirement. The first type are new needs arising as a result of the onset of the condition; for example dietary information or information on monitoring levels (for CKD and Diabetes [Citation21]) or for monitoring of balance and falls (for Dementia) [Citation24,Citation25]. Second, are existing needs, associated with maintaining normal activities of life, for which the older adult may need assistance.
In addition to accepting these needs, the older adult may have to accept and accommodate characteristics of the ageing process – for example adaptation of, or alternatives to, keyboards for deteriorating manual dexterity, or displays or audio facilities to counter visual impairment [Citation15]. The distinction between condition-specific and age-related need is important – one involves specific tailoring to the challenges presented by the condition while the other requires age-specific adaptation across technology for all conditions (e.g. for visibility etc.). Aside from meeting new needs created by the condition, older adults, with few exceptions, are not interested in functionality that accommodates a new interest or area of activity [Citation26]. Where non-disease related new needs arise these may relate to new types of communication, for example, increased use of text messages or to the augmented functions of a phone or tablet (e.g., in playing music).
2.2.6. The role of family and significant others
The role of the family and significant others emerges as important across conditions [Citation17,Citation25]. Just as the family may instigate the seeking of medical advice, they may also instigate use and facilitate the adoption of technology [Citation23,Citation24]. They may help the older person to recognise their condition or the impact of their symptoms on their daily life, they may identify the need and encourage use of technology (perhaps even purchasing the equipment or tailoring it to the person’s needs) acting as a resource in providing instruction or technical support [Citation24,Citation25]. In view of the considerable time, effort and energy that an older person may have to invest in learning a new technology, powerful motivators may be involved if a family member has bought the equipment or if the technology may enhance communication or activity with the family members [Citation27]. Choice to use technologies is therefore not simply a cognitive decision but also displays a strong affective and interpersonal component.
2.2.7. Trust
The likelihood of patients accepting their own need or choosing to use technology can depend on how much the patient trusts their family member and/or the health professional, whether GP or specialist, who advises on the condition [Citation24]. Trust in the technology and in the information and/or instructions that it contains is also critical [Citation25,Citation28]. Technology requires both dependability (it works much more frequently than it does not) and reliability (it is likely to work at a particular critical time that it is needed [Citation15,Citation24]. The information needs to be current, tailored to the specific need (linked to personalisation below), authoritative and do no harm [Citation29–31].
2.2.8. Information provision
The literature is underpinned by a prevailing assumption of empowerment through knowledge [Citation3,Citation15,Citation29]. Therefore, evaluation of the usefulness extends beyond the functionality to the appropriateness of the information that it contains or frames. This poses a considerable challenge; for some individuals information is perceived as too much while the same information for other individuals is considered sufficient, or even not enough [Citation24,Citation28]. To add complexity, the same information may be viewed positively or negatively depending upon whether it is received at an opportune time or an inconvenient time. For example, stress and urgency affect how people with CKD process information provided by healthcare professionals. Older people and their carers are often overwhelmed by the information provided by the health care professional and may not be able to articulate their questions during the consultation, thus favouring an app that can be consulted at one’s own convenient time [Citation24].
2.2.9. Personalisation
It is important that the information is tailored [Citation23,Citation32] or personalised to the patient’s specific needs [Citation2,Citation27]. Older people express frustration if, for example, an otherwise comprehensive dietary management function does not accommodate their specific food choices [Citation30,Citation33]. The prevailing requirement for personalised and individually tailored information provides a very demanding requirement: to provide the right quantity and level of information, of the right amount, at the right time to meet the needs of the individual and their carer [Citation21,Citation28].
2.3. Condition-specific issues
2.3.1. Chronic kidney disease
Barriers to technology use specific to CKD include poor understanding of CKD-related health risks among patients and poor prioritisation of CKD among primary care providers [Citation26,Citation33–35]. The synthesis indicated that patients and caregivers express preferences for diverse tool content across the condition, self-management but also across wider aspects of affordability of medication, equipment, food, financial resources and planning; travel limitations, insurance, access to health care, travel checklists; screening and supports to address mental health, cultural sensitivity, adjusting to new normal; and support to help integrate at work [Citation36,Citation37]. The burden of dietary and fluid restriction in CKD in terms of “fighting temptations” and “navigating change” requires support [Citation35,Citation36].
The My Kidneys My Health prototype in Canada [Citation38–41], invokes a three component response; data from the hospital/laboratories, data from the individual’s self-monitoring and information from the physician and other authoritative sources. Personalisation derives from placing these three important sources in juxtaposition and then achieving filtering to an individual’s personal needs. Mobile apps should include visuals, the ability to enter and track health information and interact with health care providers, “on-the-go” access, links to resources and access to personal health information [Citation39].
Multiple approaches are required to further understand the needs of older CKD patients. While qualitative research reveals specific topics of importance to older people with respect to disease management, there remains an outstanding need for information directly from older people about their experience of symptoms and outcomes in CKD [Citation26,Citation36,Citation38]. They often face a double challenge presented by both their condition and by advancing age. They may initially be helped to navigate the technology by a health professional or a family member but find it increasingly challenging to keep on top of the functions as physical or cognitive limitations increase [Citation26–28,Citation33,Citation34].
2.3.2. Dementia
While older people may be able to incorporate technology in their routines as they plan ahead for future life changes, and with a view to mitigating the onset of symptoms, they cannot always envisage the eventual impact of the condition on their activities of daily living [Citation42]. People with dementia in particular are likely to experience increasing cognitive challenges in understanding and using the technology [Citation32,Citation42]. Functionality that may prove advantageous in the early stages of the condition may pose unforeseen challenges later in the disease course. The use of technologies that are functioning as intended may become a cause of anxiety or distress; use of an automated calendar for reminders provoked such worry that the people with dementia returned to use of a manual pocket diary notwithstanding the risk of missing planned events [Citation32,Citation42]. A substantial literature relates to the use of technology for cognitive stimulation in dementia [Citation43,Citation44]. While the advantages of regular cognitive stimulation are commonly advocated, this may carry the detrimental and undesired effect of providing independent evidence of the person’s own deterioration, thereby heightening anxiety.
Co-ordination of care is a major challenge for dementia. A contrast is made between the typical coordination through a single health professional (such as a diabetic nurse) for diabetes, as opposed to the fragmented care delivered for dementia. One attraction of a technology for dementia is the facility to organise a coordinated “one stop shop” response [Citation52].
2.3.3. Diabetes
Self-monitoring and dietary management are revealed as specific requirements for older people managing diabetes that are prominent throughout the literature [Citation7,Citation19,Citation23,Citation45]. Self-monitoring is intended to help the individual seek balance in terms of their activities of daily living, in particular their intake, but it holds the added value, if communicated to the health practitioner, of providing additional data to inform their formal care [Citation21,Citation22,Citation53].
CKD shares with Diabetes a requirement for dietary management and self-monitoring. Of note is the fact that these two conditions are not completely independent with significant numbers of older people experiencing both CKD and diabetes [Citation7,Citation46]. While both CKD and diabetes have disease-specific requirements in terms of diet, a third requirement relates to the overlap of requirements to shape a third profile of those managing both conditions. Therefore, the shared functionality may simplify requirements but the common comorbidity of the two conditions may further complicate the information requirements [Citation46].
2.4. Gaps in the evidence base
The gerontological perspective is largely missing from the identified literature. The specific technological and information requirements precipitated by normal ageing are eclipsed by the considerations of each individual condition. The literature assigns limited consideration to the characteristics of technology and the adaptations required to meet the needs of older people. Despite some evidence of the older person’s perspective, this tends to relate to generational aspects of lack of awareness of the technology functions rather than to practical difficulties with using the equipment. Older people experience the same frustrations of users in general, for example, not being able to save information, losing data and having to retype etc. [Citation18].
3. Expert interviews
The synthesis of qualitative studies enabled further definition of the research problem to be extended through consultation with experts. Semi-structured interviews were undertaken as the first stage of a Delphi method [Citation47], a multi-stage approach involving an expert panel seeking to achieve a consensus through systematic collection and aggregation of views [Citation48,Citation49]. Whilst the review considered articles specific to the three conditions separately, the Delphi sought to build on the findings and consider commonalities across the conditions to take forward through future research and development. The full Delphi study will be reported elsewhere; here we focus on the first round of interviews. The study gained was approved by Coventry University Research Ethics Committee (P124976).
3.1. Participants
A virtual expert panel was assembled through purposive sampling from within academia, and through partner organisations, relevant experts and recommendations from recruited panellists. Heterogeneous panel membership sought to represent a broad spectrum of opinion [Citation50]. The inclusion criteria applied required expertise in one of the following:
Academic or practical expertise in self-management software and older people,
Academic or practical expertise in assistive technologies and older people,
Advanced clinical experience in provision of care to older people with either diabetes, chronic kidney failure or dementia,
Lived experience – personal experience of self-management of either diabetes, chronic kidney failure or dementia.
All potential panellists were provided with the project patient information sheet and given the opportunity to speak with the researcher online/by telephone to ask any questions before providing their consent to take part in the study. Fourteen panellists were recruited and their specific expertise is shown in .
Table 4. Panel composition and participant expertise.
3.2. Data collection
Qualitative data were collected through a series of one to one interviews employing Zoom video conferencing software (during 2021 and the COVID-19 pandemic).
A scripted list of questions guided the interviews. The panellists were asked to view a list of self-management technologies, developed by Kim and Lee [Citation20] and identified from the reviews as a useful tool for describing the self-care strategies behind the different forms of technology (see ). The interview questions (see ) allowed the panellists to respond to recommendations emerging from the literature and provide their own responses and suggestions. This allowed exploration of the three different long-term conditions with panellists with condition specific expertise. The fifth interview question was directed to panellists based upon their expertise. Automatically generated transcripts were downloaded, checked and edited for accuracy.
Table 5. Interview questions.
3.3. Data analysis
Inductive thematic analysis was undertaken [Citation51]. Potential themes and ideas were highlighted from within the text of each transcript and then grouped together to identify commonalities, differences, patterns and concepts of note. Panellist interviews were analysed together by long-term condition, to ensure concepts and condition specific data was not missed, and then combined and grouped in overall themes. Condition-specific analysis will be reported elsewhere on completion of the full Delphi study.
4. Results
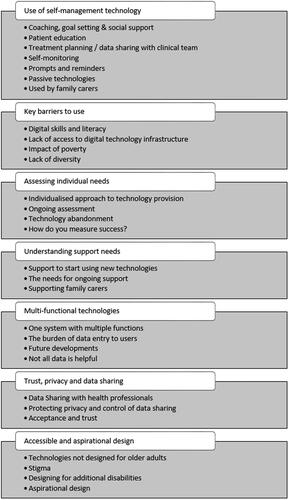
The seven themes that emerged across the three conditions are summarised in . summarises the issues found through the reviews and then additional findings ascertained through the interviews.
Table 6. A summary of key issues identified from the literature and interviews.
4.1. Use of self-management technology
The interview findings indicated that older adults use self-management technology in a variety of different ways, seeking to undertake a range of functional tasks based on their individual needs. Although some technologies are commonly associated with condition-specific needs (e.g., self-monitoring with diabetes and reminder prompts for people with dementia), there is considerable crossover and users often seek combined technologies. Technology designed for self-management is often used in partnership with family carers or on behalf of people with long-term conditions by their carers, and therefore a greater understanding of their joint use to promote independent lifestyles is needed.
4.2. Key barriers to use
Significant barriers to the effective use of self-management technology are varied and, in many cases, are non-age specific; limited digital skills and confidence in using new technology, and variation in access and to the required infrastructure. The most significant demographic factor in the development of these skills, or accessing the right technology was reported to be the impact of poverty, and the financial implications of relying on technology that may be expensive to purchase, maintain or keep connected. Other barriers included a lack of diversity in design, such as English language only apps and poor representation in research and development, potentially excluding those outside of “normative” academic views of users, for example, those from different cultural backgrounds, or those with different needs as a result of their health condition.
4.3. Assessing individual need
The interviews highlighted that whether purchased privately, or provided though statutory services, the introduction of technology requires considerable planning. Inappropriate provision that does not suit the needs of the user can set older adults up to fail, damaging their trust and confidence. Rather than a “one size fits all” solution, technology should be designed to be adaptable, and to be easily incorporated into the lives and homes of older adults. Technology is best provided in a customised and individualised way, following detailed holistic assessment of the individual’s needs and wishes. Assessment of needs should be ongoing, recognising a person’s changing needs or wishes, supporting the use of technology to enable the user, and acknowledging (for dementia in particular) a need for timely provision.
Although successful commercially, “plug and play” technologies, often lack opportunity for re-assessment and can lead to early abandonment and then offer little value to the user. Measures of value to the user is not always considered in technology provision, with success often measured by impact on clinical services, sales figures or reduced carer burden.
4.4. Understanding the right support needs
Introducing self-management technology was felt to require a greater level of support to ensure older adults have the appropriate skills and knowledge to use it effectively. The initial setting up, or on boarding of users is crucial to the person’s sense of trust in the technology. Difficulties in set up are a significant indicator of poor use or early abandonment.
It was indicated that older adults might also need additional ongoing support to manage the changes and updates to the technology they use, or to identify when to move from one type of supportive technology to another as their condition changes. This may also be required to deal with the psychological impact of collecting and viewing detailed health data, especially when it indicates a decline, or difficulties in managing a condition. Technology is often used within a supportive environment, where use by older adults is dependent upon the active involvement of others. In such cases, it is important to provide support and guidance to all those involved.
4.5. Multi-functional self-management technologies
There was recognition amongst participants that self-management technologies need to support multiple and diverse functional tasks. The “joining up” of technologies such as connected apps, wearable data collection tools, and internet-enabled household objects or online support groups was seen to have real potential in meeting a recognised need, particularly for older adults living with diabetes, who currently use multiple self-management technologies in their daily lives.
Greater connectivity between existing technologies as seen in “looping” (use of an automated insulin delivery system to maintain optimal glucose levels) or in apps and real-world products, such as bar code scanners for carb counters have shown to be helpful for some, but older people exhibit limited trust in this type of technology and the personal consequences for reliance on poor technology are significant.
The interviewees indicated that not all users want to view and record all aspects of their health and well-being. The ability to personalise technology set up was recognised as important, whilst also limiting the potential data entry burden on users requiring only appropriate data to be recorded that supports and enables the user in managing their condition.
4.6. Trust, privacy and data sharing
Trust in the credibility, reliability and usability of self-management technology leads to greater acceptance. Participants indicated that older adults seek reassurance from organisations such as the NHS, that the apps, technologies and wearables they have access to are both appropriate for the intended use and trustworthy.
Technology is increasingly used to collect, record, track and monitor patient data [Citation52–54]. There are many benefits from sharing data such as promoting greater collaborative management, improving communication and informing day-to-day decision making for both the older person and clinical team. It was raised that potentially sharing of data can lead to a decrease in personal responsibility for managing one’s own health and raise expectations about the degree to which the clinical team will monitor and respond to it. Interviewees also indicated that there is a need to address concerns and provide reassurance around the sharing of “big data”, use of inbuilt artificial intelligence and selling of patient data.
Patient privacy and control over who can access personal health data raises both pragmatic and ethical questions. Ultimately control over who accesses data should rest with the individual, and if they feel that their privacy is both valued and respected they are more likely to opt to share data more widely in instances where it may be beneficial (e.g., with online support groups who can offer peer feedback, motivation and encouragement in response).
4.7. Accessible and aspirational design
Participants felt that self-management technology designed to support a particular long term-condition, such as diet management apps for people with chronic kidney disease, is rarely designed with older adults in mind. As identified through the literature, it is often assumed that older adults require the same design features and accessibility levels as all other users, and so often fail to take into consideration common disabilities associated with older age. Yet those that are designed with these disabilities in mind are often unappealing, clinical or stigmatising. Participants indicated that few older adults are keen to have equipment on display in their homes that looks “clinical” and “medical”, and the wearing of obviously “disability friendly” trackers and pendants can increase stigma in the community and increase vulnerability. Participants recognised that the challenge is to design aspirational self-management technologies that take into consideration potential age related disabilities but are attractive and desirable in order to increase uptake and use.
5. Discussion
This paper outlines three syntheses of qualitative studies as well as new qualitative research undertaken to extend understanding of the barriers and enablers to the uptake and adoption of self-management technology by older adults with CKD, dementia and diabetes. The systematic reviews enabled identification of issues affecting older adults across conditions. The condition specific issues will be discussed more fully elsewhere. It was identified that the gerontological perspective is largely missing from the reviewed literature. The specific technological and information requirements precipitated by normal ageing tend to be eclipsed by the considerations of each individual condition and further consideration is needed of the characteristics of the technology and the adaptations required to meet the needs of older people.
The interviews (as the first phase of the Delphi study) sought to explore the literature themes in more depth. Whilst the systematic reviews considered articles specific to the three conditions separately, the interviews with condition specific and technology experts sought to consider commonalities across the conditions to take forward through future research and development to add value across long-term conditions. The results led to 7 key themes across conditions (1) Use of self-management technology; (2) Key barriers to use; (3) Assessing individual needs; (4) Understanding support needs; (5) Multi-functional technologies; (6) Trust, privacy and data sharing; (7) Accessible and aspirational design. Within these themes, similar barriers and challenges were evident across conditions. The inter-related nature of the three conditions and potential for co-morbidity was highlighted; this presents challenges of self-managing multiple conditions, and the requirement for technologies that can enable self-management of more than one condition.
As the interview panel included healthcare professionals and expert patients, the interviews allowed focussed consideration on the prescription process, which received less direct attention in the reviewed articles. The participants argued that the current prescription approach does not cater sufficiently for a change in someone’s condition or capabilities. They emphasised the valued the sharing of data between the patient, clinical team and carers, and felt this encourages greater collaborative management, improved communication and informed day to day decision making by the older adult and their clinical team. They also recognised the expectations that patients may have of their clinical team, or their own personal responsibility for care, once technology is involved in condition monitoring and their health data is shared with others.
The initial assessment and provision of self-management technologies is complex, and therefore adequate time and resources should be allocated to the assessment, and when necessary re-assessment of needs. The critical role family members and informal carers play in assisting self-management is evident in the literature and interview data. Training, support and general information about the use of self-management apps and technologies should be extended to the wider circle of care recognising their role in condition management and technology use. Consideration of the skills, training, building of trust and support needs should include older adults and those that assist them, through tailored, individualised support packages to “on-board” or set up users. Ongoing technology support is also needed to encourage long-term adoption.
Based on the findings here and a focus on widening access, research should explore strategies to overcome common barriers to self-management technology use by older adults. A focus is needed on enabling and supporting those with limited private funds, or technology skills, as well as those from diverse groups (clinical and demographic) within UK communities, and those living with more than one long-term condition. The interview data particularly highlighted the significance of poverty and the recognition that many older adults have poor access to the required infrastructure to maintain technology or keep it connected, and are unable to buy technologies. Widening access in terms of the language of available systems, and diversity and representation in technology research and development is also a priority.
Further focus on the characteristics of technology, and the prescription and adaptations required to meet the needs of older people and address the practical and psychological difficulties associated with use is required. The Delphi method is a multi-stage approach; two further rounds of expert enquiry will be undertaken to systematically collect and aggregate views. Without pre-empting the results of that further research, there are a number of areas that have emerged so far to guide further research and development, and an initial set of recommendations have been formed. These are summarised in . These begin to address our long-term aim to inform and guide the design and development of self-management technology, and its provision by healthcare professionals. The recommendations will be extended and revised through the next two rounds of the Delphi.
Table 7. Emerging recommendations for the design and prescription of self-management technology to older adults.
The combination of factors affecting the use of digital technology for the self-management of long-term conditions by older adults requires that disease-specific, age-specific and general requirements align through the design process. Technology should be aspirational taking into consideration capabilities, whilst ensuring it is attractive and desirable to own and use. This requires sustained involvement of older adults as advisors, users and customers, Involvement and empowered decisions are critical to encourage buy-in, acceptance and sustained use. A specific focus on the barriers to use of self-management technology enables the developed of tailored strategies to enable more people to benefit. By tackling both the design and prescription of self-management technologies, we hope to improve acceptance and use by older people, thereby increasing quality of life, and reducing abandonment and the resulting health service costs.
Acknowledgements
The authors wish to acknowledge the participants who have shared their valuable time, views and experiences through this research.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Chalfont G, Mateus C, Varey S, et al. Self-Efficacy of older people using technology to Self-Manage COPD, hypertension, heart failure, or dementia at home: an overview of systematic reviews. Gerontologist. 2021;1(6):e318–e334.
- Hirakawa K, Umemuro H. Technology acceptance model with social factors for older people. Gerontechnology. 2010;9(2):214–214.
- Stellefson M, Chaney B, Barry AE, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. 2013;15(2):e35.
- Alexander S. MHealth technologies for the self-management of diabetes in the older population. SIGACCESS Access Comput. 2015;111(111):14–18.
- Goodacre K, McCreadie C, Flanagan S, et al. Enabling older people to stay at home: the costs of substituting and supplementing care with assistive technology. Br J Occup Therapy. 2008;71(4):130–140.
- Greenhalgh T, Wherton J, Papoutsi C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e367.
- Clemens KK, O’Regan N, Rhee JJ. Diabetes management in older adults with chronic kidney disease. Curr Diab Rep. 2019;19(3):1–11.
- Marston HR, Smith ST. Interactive videogame technologies to support independence in the elderly: a narrative Review. Games Health J. 2012;1(2):139–152.
- Parker L, Moran GM, Roberts LM, et al. The burden of common chronic disease on health-related quality of life in an elderly community-dwelling population in the UK. Family Practice. 2014;31(5):557–563.
- Taymoori P, Khazaee-Pool M, Pashaei T, et al. Design and development of a mobile app framework to facilitate breast Cancer-Preventive behaviors (m-BCPB) in the at-Risk women: Qualitative study. PREPRINT (Version 1) Available at Research Square.
- Flemming K, Closs SJ, Hughes ND, et al. Using qualitative research to overcome the shortcomings of systematic reviews when designing of a self-management intervention for advanced cancer pain. Int J Qual Methods. 2016;15(1):160940691667065.
- Booth A, Carroll C. How to build up the actionable knowledge base: the role of 'best fit' framework synthesis for studies of improvement in healthcare. BMJ Qual Saf. 2015;24(11):700–708.
- Carroll C, Booth A, Leaviss J, et al. Best fit” framework synthesis: refining the method. BMC Med Res Methodol. 2013;13(1):37–36.
- Hendricks L, Eshun-Wilson I, Rohwer A. A mega-aggregation framework synthesis of the barriers and facilitators to linkage, adherence to ART and retention in care among people living with HIV. Syst Rev. 2021;10(1):54.
- Renaud K, Van Biljon J. Predicting technology acceptance and adoption by the elderly: a qualitative study In Proceedings of the 2008 annual research conference of the South African Institute of Computer Scientists and Information Technologists on IT research in developing countries: riding the wave of technology 2008. New York, NY, USA, 2008, p. 210–219.
- Choi HW, DiMaria-Ghalili RA, Kelly M, et al. Older adults and technology use: a systematic literature review. Innovation in Aging. 2020;4(Supplement_1):823–823.
- Jakobsson E, Nygård L, Kottorp A, et al. Experiences from using eHealth in contact with health care among older adults with cognitive impairment. Scand J Caring Sci. 2019;33(2):380–389.
- Rogers WA, Meyer B, Walker N, et al. Functional limitations to daily living tasks in the aged: a focus group analysis. Hum Factors. 1998;40(1):111–125.
- Armstrong DG, Najafi B, Shahinpoor M. Potential applications of smart multifunctional wearable materials to gerontology. Gerontology. 2017;63(3):287–298.
- Kim BY, Lee J. Smart devices for older adults managing chronic disease: a scoping review. JMIR Mhealth Uhealth. 2017;5(5):e7141.
- Macdonald EM, Perrin BM, Kingsley MI. Enablers and barriers to using two-way information technology in the management of adults with diabetes: a descriptive systematic review. J Telemed Telecare. 2018;24(5):319–340.
- Waite M, Martin C, Franklin R, et al. Human factors and data logging processes with the use of advanced technology for adults with type 1 diabetes: systematic integrative review. JMIR Hum Factors. 2018;5(1):e9049.
- Shang L, Zhou J, Zuo M. Understanding older adults' intention to share health information on social media: the role of health belief and information processing. INTR. 2020;31(1):100–122.
- Curtis K, Price K. Factors that influence older people's engagement with digital health technology. Nurs Older People. 2017;29(10):27–30.
- Dahler AM, Rasmussen DM, Andersen PT. Meanings and experiences of assistive technologies in everyday lives of older citizens: a Meta-interpretive review. Disabil Rehabil Assist Technol. 2016;11(8):619–629.
- Roberti J, Cummings A, Myall M, et al. Work of being an adult patient with chronic kidney disease: a systematic review of qualitative studies. BMJ Open. 2018;8(9):e023507.
- Lucca DC, Hammerschmidt KS, Girondi JB, et al. Game of attitudes: educational gerontotechnology for the elderly undergoing haemodialysis. Rev Bras Enferm. 2020;73(suppl 3):e20180694.
- van Dipten C, de Grauw WJ, Wetzels JF, et al. What patients with mild-to-moderate kidney disease know, think, and feel about their disease: an in-depth interview study. J Am Board Fam Med. 2018;31(4):570–577.
- Linner T, Seeliger A, Vogt L, et al. REACH: Solutions for Technology-Based prevention and empowerment for older people and their caregivers. Population Ageing. 2020;13(2):131–137.
- Sánchez VG, Anker-Hansen C, Taylor I, et al. Older People's Attitudes And Perspectives Of Welfare Technology In Norway. J Multidiscip Healthc. 2019;12:841–853.
- Tay EYJ, Massaro S. Planning and shared decision making in elderly care. PsyArXiv: 2018. DOI:10.31234/osf.io/5svtn.
- Imbeault H, Langlois F, Bocti C, et al. Can people with Alzheimer's disease improve their day-to-day functioning with a tablet computer? Neuropsychol Rehabil. 2018;28(5):779–796.
- Bowling CB, Vandenberg AE, Phillips LS, et al. Older patients' perspectives on managing complexity in CKD Self-Management. Clin J Am Soc Nephrol. 2017;12(4):635–643.
- James G, Nyman E, Fitz-Randolph M, et al. Characteristics, symptom severity, and experiences of patients reporting chronic kidney disease in the PatientsLikeMe online health community: Retrospective and qualitative study. J Med Internet Res. 2020;22(7):e18548.
- Lambert K, Mansfield K, Mullan J. How do patients and carers make sense of renal dietary advice? A qualitative exploration. J Ren Care. 2018;44(4):238–250.
- Stomer UE, Wahl AK, Goransson LG, et al. Exploring health literacy in patients with chronic kidney disease: a qualitative study. BMC Nephrol. 2020;21(1):314.
- Stevenson J, Tong A, Gutman T, et al. Experiences and perspectives of dietary management among patients on hemodialysis: an interview study. J Ren Nutr. 2018;28(6):411–421.
- Donald M, Beanlands H, Straus SE, et al. A Web-Based Self-Management support prototype for adults with chronic kidney disease (My kidneys My health): Co-Design and usability testing. JMIR Form Res. 2021;5(2):e22220.
- Donald M, Beanlands H, Straus S, et al. Preferences for a self-management e-health tool for patients with chronic kidney disease: results of a patient-oriented consensus workshop. CMAJ Open. 2019;7(4):E713–e20.
- Smekal M, Gil S, Donald M, et al. Content and quality of websites for patients with chronic kidney disease: an environmental scan. Can J Kidney Health Dis. 2019;6:2054358119863091.
- Donald M, Beanlands H, Straus S, et al. Identifying needs for self-management interventions for adults with CKD and their caregivers: a qualitative study. Am J Kidney Dis. 2019;74(4):474–482.
- Lariviere M, Poland F, Woolham J, et al. Placing assistive technology and telecare in everyday practices of people with dementia and their caregivers: findings from an embedded ethnography of a national dementia trial. BMC Geriatr. 2021;21(1):121.
- Crete-Nishihata M, Baecker RM, Massimi M, et al. Reconstructing the past: personal memory technologies are not just personal and not just for memory. Human–Computer Interaction. 2012;27(1-2):92–123.
- Peeters MM, Harbers M, Neerincx MA. Designing a personal music assistant that enhances the social, cognitive, and affective experiences of people with dementia. Computers in Human Behavior. 2016;63:727–737.
- Mamykina L, Heitkemper EM, Smaldone AM, et al. Personal discovery in diabetes self-management: discovering cause and effect using self-monitoring data. J Biomed Inform. 2017;76:1–8.
- Shirazian S, Crnosija N, Weinger K, et al. The self-management experience of patients with type 2 diabetes and chronic kidney disease: a qualitative study. Chronic Illn. 2016;12(1):18–28.
- Iqbal S, Pipon-Young L. Methods-The delphi method–a guide from susanne iqbal and laura Pipon-Young. Psychologist. 2009;22(7):598.
- McKenna HP. The delphi technique: a worthwhile research approach for nursing? J Adv Nurs. 1994;19(6):1221–1225.
- Keeney S, McKenna H, Hasson F. The delphi technique in nursing and health research. Chichester, UK: John Wiley & Sons; 2011.
- Synowiez BB, Synowiez PM. Delphi forecasting as a planning tool. Nurs Manage. 1990;21(4):18–19.
- Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London, UK: Sage; 2013.
- Astell A, Smith S, Joddrell P, editors. Using technology in dementia care: a guide to technology solutions for everyday living. London, UK: Jessica Kingsley Publishers; 2019.
- Hunt CW. Technology and diabetes self-management: an integrative review. World J Diabetes. 2015;6(2):225–233.
- Wood E, Ward G, Woolham J. The development of safer walking technology: a review. Journal of Assistive Technologies. 2015;9(2):100–115.