Abstract
Telehealth has long been highlighted as a way to solve issues of efficiency and effectiveness in healthcare and to improve patients’ care and has become fundamental to address patients’ needs during the COVID-19 pandemic; however previous studies have shown mixed results in the user acceptance of such technologies. Whilst many previous studies have focussed on clinical application of telehealth, we focus on the adoption of telehealth for virtual assessments visits aimed to evaluate the suitability of a property where a patient is discharged, and eventual adaptations needed. We present a study of stakeholders’ attitudes towards such virtual assessment visits. The study has been carried out with healthcare professionals and patients and allowed us to identify user attitudes, barriers and facilitators for the success of virtual assessment visits from the point of view of healthcare professionals and patients. Finally, we discuss implications for designers of telehealth services and guidelines that can be derived from our study.
1. Introduction
Population ageing is a worldwide phenomenon: the number of older persons (over 60) is expected to reach nearly 2.1 billion by 2050.Footnote1 This demographic shift correlates with an increasing numbers of health issues and healthcare system worldwide are struggling to respond appropriately to the growing demands of the ageing population, as service demand is widely expected to rise. This, coupled with budget restrictions and pushes for cost efficiency have increased the importance of finding alternative ways to deliver healthcare.
Telehealth, i.e., “the use of telecommunications and virtual technology to deliver health care outside of traditional health-care facilities”,Footnote2 has long been regarded as one of the most promising ways to deliver efficient and effective healthcare. Telehealth can be adopted for a wide range of interventions, from clinical visits to telemonitoring interventions [Citation1,Citation2].
During the COVID-19 pandemic, a number or telehealth or remote visit solutions have been trialled worldwide, as they offered a safe way to deliver healthcare services in an optimal manner whilst minimising face-to-face exposure [Citation3]. In UK several digital solutions for video consultations or for symptoms checking were rapidly inserted into practice, especially in non-acute care (e.g., “AccuRx”Footnote3 or “Attend Anywhere”Footnote4).
In this study we focus on the use of telehealth to deliver virtual home assessments, seeking to understand the cultural, organisational and technical barriers and facilitators to the adoption of telehealth technologies in Occupational Therapy (OT) services. As an outcome of the study, we have derived design guidelines that will support future studies in all areas of health care practice where home visiting is standard practice e.g., such as district nursing, social care, dietetics, emergency services etc.
1.1. Study background
The work presented in this paper is part of a larger project aimed at understanding how to reduce “unnecessary care costs and hospital admissions through prevention and better self-care in people with multi-morbidity” [Citation4]. The study used a user-centred design process (in consultations with OTs and other healthcare professionals) to design a prototype for virtual home assessments [Citation5], presented in Section “Materials and methods”. This prototype has been used as an input in this study, to understand barriers and enablers and to derive design guidelines for a future version of the system and services.
1.2. Related work
1.2.1. What is the time and cost associated with home visits?
A UK based study by Drummond et al. [Citation6] questioned therapists working in stroke units, to identify current practice in relation to people with stroke. The main reason for conducting visits was to “assess or practice activities of daily living in the home environment” and to “identify or address safety issues.” The length of time taken to conduct home visits varied greatly with a mean time of 63 min at the home environment (not including travel time) and a further mean time of 61 min for writing a home visit report. Visits were generally conducted by an occupational therapist, with an occupational therapy/physiotherapy assistant.
In comparison, during our study we carried out an audit of the local hospital data on home visits from which we derived that a visit could take up to 4 h in total from arranging, doing and writing up and reporting (including travel time).
The cost of home visits is a significant factor both to the service both in terms of releasing staff and also of personnel being away from the workplace for long periods of time. Drummond et al. [Citation6] estimated the average cost of a home visit to be £208.
1.2.2. How can remote technological solutions enhance the home visit process?
Remote video consultation has been applied in a number of clinical areas e.g., patients with obesity [Citation7]; patients with diabetes [Citation8] and as a way of including relatives and carers as part of the ward round [Citation9] and in specialised palliative care [Citation10].
Sturesson and Goth [Citation7] wanted to understand when and in what circumstances remote technology would be suitable to use with certain patients with obesity. Three main themes emerged from the data that indicated that decisions to use video technology were influenced by practicalities, patient’s ability and the content of the outpatient meeting. A set of selection criteria was developed to help with this decision making of which patients were most suitable and how to engage them with this approach, which was seen to strengthen patient responsibility but also the relationship they had with their clinician.
Greenhalgh et al. [Citation8] through a mixed method design wanted to define good practice guidance around the use of virtual consultations. Video consultations were deemed to be safe and were popular with some patients and staff when they were clinically relevant and technical conditions were right. Video consultations were found to be slightly shorter but the patients did more talking and there was a need to be more explicit in terms of the content covered. Familiarity between the patient and clinician as well as a perception of trust was also linked with success of a video consultation and an outcome for the patient of improved self-management. Challenges in scaling up the intervention included technical consideration and the fact that organisations were reluctant to make a wholescale change especially at times of austerity. The qualitative study by [Citation9] suggested that the use of video consultations allowed health care professionals to engage patients’ relatives without them being present. However, implementation of new technology with relatives was challenged by time, culture, and change of work routines in complex health care systems. Frydenrejn Funderskov et al. [Citation10] found the use of video allowed patients to take a more active role, along with increased active input from relatives.
A scoping review synthesised the findings of studies concerned with information and communication technologies used as part of a home visit intervention [Citation11]. The review recognised that home visits did not always take place due to time constrains for occupational therapists but also geographical barriers. The use of technological solutions was identified in this review as a possible solution.
A recent study reported on a technology-enhanced solution called “Home Quick” [Citation12], that allowed to substitute direct home visits with remote visits for a range of home visiting scenarios traditionally performed by occupational therapists.
2. Materials and methods
2.1. The prototype
The project technology used in our study was co-designed and developed in a previous research project aiming at building Occupational Therapy research [Citation4], in cooperation with OTs, patients and other healthcare professionals.
It is a video consultation prototype that offers the ability to undertake audio/video home assessments by using a computer browser, with no need to install applications or to register. The process used to establish the connection and carry out the visit is illustrated in . The patients will receive from the hospital or the service a link to a webpage via text message or email and a reminder just before the visit. The text message contains a hyperlink that the user can click, either on a smartphone or on a browser, at the allocated time, to connect to the Occupational Therapist. If the patient needs support with the visit, the hyperlink can be texted to a smartphone controlled by a trusted visitor (such as a relative or member of a third sector organisation).
Once the connection is established the patient will simply see the Occupational Therapist as they would in any video call. The Occupational Therapist will see an interface that allows to see the patient’s video feed, record audio or video of the call for later viewing/evidence purposes, take screenshots, take digital notes to be saved alongside the video (a screenshot is presented in ). Moreover, the Occupational Therapist can take control of the patient’s camera and flash to be able to focus the video as needed for the virtual assessment and to zoom in and out to appreciate details, etc.
All data (notes, pictures, etc.) are stored securely on a central server. As the visit may involve different services beyond the hospital (e.g., care homes, social services, city councils, etc.), the technology supports simultaneous participation of multiple users from multiple locations. That can include remote family members or carers. This enables:
Sharing of essential care planning and information among services.
User engagement and personalisation of care, through the ability of involving patients and remote family/carers in decision making.
A rapid and efficient solution for post-discharge follow-up.
2.2. Study phases
The study was carried out in different phases.
2.2.1. Phase 1 – literature and policy review
The first phase of the study involved carrying out a literature and policy review, to lay the foundations for our research. We used the recommendations from the NHS Digital design principlesFootnote5 and the principles stipulated in the TOPOL review (an NHS England report on how to prepare the healthcare workforce, through education and training, to deliver the digital future) [Citation13] to establish the methodology for our study.
2.2.2. Phase 2 – Initial design – definition of a stakeholders map
As an outcome of the interviews with OTs we defined a stakeholders’ map, including Primary stakeholders (stakeholders that are directly concerned and/or affected by the technology):
Patients, especially patients that have reduced mobility or physical or mental disabilities that can affect their ability to attend standard assessment visits.
Family, friends and carers
Healthcare professionals in several fields
neurorehabilitation
speech and language therapy
stroke
orthopaedic therapists
major trauma
spines rehab
head injuries
dietetics
Cystic Fibrosis Clinical Specialist Physiotherapist
Specialised Medicine
Community care
Secondary stakeholders are those who are more distant from day-to-day healthcare but still can have an input in it/be affected, e.g.:
Local authorities
Adults and Social Care Service Managers
Housing Services
Equipment and adaptations services
2.2.3. Phase 3 – workshops to discuss the prototype with identified stakeholders
Three stakeholder events were held in the city at locations close to an acute hospital, in the community in a care home and at a local authority building with the intention of attracting a variety of health and social care professionals. There were 52 participants in the workshops included; Occupational Therapists (n = 25), Physiotherapists (n = 6), Dieticians (n = 5), Nurses (n = 2), GPs (n = 1), Social care workers (n = 2), Voluntary Sector workers (n = 2), Mental health workers (n = 1), Housing Officers (n = 1), Equipment and adaption team members (n = 3) and Speech and Language Therapists (n = 4). The project run three consultation workshops with Patient and Public Involvement Groups, during scheduled sessions of the PPI groups:
Stroke and Aphasia PPI Group Sheffield Teaching Hospitals (10 service users, 2 support officers, 1 stroke consultant, 1 Speech and language Therapist)
Therapeutics and Palliative Care PPI Group Sheffield Teaching Hospitals (5 service users, 1 Physiotherapist, 1 Dietician, 1 Supporting Officer)
Sheffield City Council Adult Service Improvement Forum (4 service users, 1 personal assistant to service user, 1 head of service, 1 volunteer, 1 patient representative, 1 support officer)
Participants were not reimbursed for attendance. Participants were given a leaflet containing information about the project and provided with an introductory presentation and demonstration of the technology. A “mock remote visit” was simulated and videoed for training purposes and this video was used to exemplify the technology to the participants. They were then asked to reflect on any issues they thought would be a barrier to deployment of the technology, likely benefits of utilising the technology for remote home visits, other potential uses for the technology in clinical practice to improve and/or enhance patient care and they were asked how they would change in the prototype design (see ).
Figure 2. Screen shot of the occupational therapists remote ‘virtual visit’ control panel, showing the control buttons on the left, which allow the therapist to control the visitor’s smartphone and right-hand panel for them to capture real-time notes.
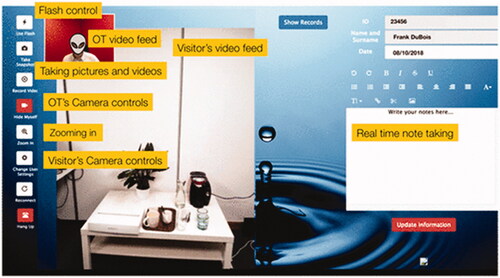
Figure 3. Snapshot from one of the workshops showing the grouping of participants in tables and the post-it notes activity.

Four guide questions were used to stimulate the discussion during the workshops and the PPI events:
What are the barriers to introducing this technology that you could foresee?
Are there any potential benefits of introducing a technology for remote home visits?
Share your thoughts on any potential uses for the technology to improve and/or enhance patients’ care
Share your thoughts for developing the technology to suit your needs.
2.2.4. Phase 4 – user stories
In this phase we adopted user stories as a design technique. User stories are a real-life example, taken in retrospective, of user experiences in a specific context: they can for example illustrate a user experience and how a technological solution could have been used in that context [Citation14]. We chose this technique as it facilitates end users in expressing their experiences and context of interactions but also is a very useful feedback tool for designers [Citation15].
We collected 5 user stories from OT for clinical examples where the use of technology would have enhanced care provided, saved time and staff resources or solved a problem which required a home assessment, but a virtual visit would have been an improvement to usual care. An example of a user story is presented in .
Table 1. An example of a user story collected during the user studies.
2.3. Data collection and analytic approach
Qualitative data was collected during all the workshops with the stakeholders, in the forms of post-it notes produced by the participants, photos taken during the workshops, notes taken by all the project researchers. Our mixed-methods approach was inductive and data-driven [Citation16], consisting in a thematic analysis of the data [Citation17] to identify barriers and facilitators for the adoption of the technology and to derive design guidelines. The feedback from the stakeholders was recorded during the event discussions by using colour-coded physical post-it notes, photos and notes taken by the observers. The data was colour-coded according to the type of stakeholder (e.g., patient, hospital worker, community worker or voluntary sector) and organised on an axial-diagram with dimensions corresponding to the research questions [Citation18]. The post-its were subsequently clustered by affinity to reveal themes [Citation19–21].
2.4. Ethics
Given the sensitive topic of our study and the involvement of patients and carers the research team paid special attention to ethics. In particular an effort was made to prepare tailored presentations for every user group, test all the materials before the workshops and use the feedback from each workshop to improve the quality of materials. The preparation for the workshop with Stroke and Aphasia patients required particular attention to ensure the presentation of the prototype was clear and concise and the language was understandable. The study had ethical approvals for the literature review and the user studies from the participating universities’ Ethics boards. The stakeholder engagement and consultations were also governed by a service evaluation registration with the local hospital trust.
3. Results
A number of key themes emerged from the data analysis; those were then divided into barriers and facilitators.
3.1. Barriers
Barriers were identified in relation to the prototype itself but also to the broader context of adoption and the environment where the software could be deployed.
The main barrier related to the prototype itself was security, in terms of video connection but also of data storage and levels of access and sharing of information. Whilst one of the main benefits of a virtual visit solution was perceived to be the possibility of sharing information with other agencies, therefore avoiding duplication of efforts, questions were raised about how the system would allow sharing whilst respecting patient confidentiality and information governance.
The training required for the Occupational Therapists to use the software would also represent a barrier, in the form of initial training course and time to attend them and in the form of guidance inbuilt in the application, to support staff during the initial period in gaining confidence.
Other barriers were linked to broader context and environment of deployment, and to the fear of inequalities, such as availability of IT resources, reliability of network connection, cost for patients/health professionals.
The availability of suitable IT resources and environments was seen as potentially negatively impacting the adoption of a remote visit system. From the point of view of patients this was mostly related to the need to own a smartphone with a suitable internet connection and/or a mobile data allowance plan. Whilst ownership of smartphones with contract is widespread in UK and worldwide, not all patients might own one, thus potentially causing inequalities in access to the service. One stakeholder from Social care pointed out how “Many clients are elderly/frail and have no family and therefore have no access to technology”. This might also in some cases cause social anxiety: “Could be stressful for people if they struggle to respond to request for info or use technology”.
Healthcare professionals discussed how the lack of suitable IT resources (such as laptops or desktop computers) in a private consultation room can negatively impact adoption. Not only the workforce should have a computer available to carry out the virtual visit, but this should have sufficient specifications for the virtual visit to be carried out smoothly. Moreover the computer should be placed ideally in a consultation room that is private and decorated as a face-to-face consultation room. One stakeholder from intermediate care pointed out how they have “3 PCs in our office for 20 staff”: clearly this would not be an adequate environment to carry out a virtual visit.
The issue of quality of network connection was also explored: whilst hospitals in UK tend to have widespread and high-speed WIFI connection, this is not accurate for every unit. For example, Intensive Care Units tend to have poor internet connection. The same concerns emerged from patients as they discussed the potential lack of suitable 3 G/4G connection or WIFI – again this might exacerbate inequalities in care.
The cost of using the telehealth solution was much debated as there was a fear it would increase inequalities (e.g., a patient might not want to pay for the data traffic required to carry out the virtual visit). In a future perspective, there will be the need to find models of effective reimbursement for adopters of telehealth.
In addition to these more practical barriers there were worries about trust and reliability and fear of missing important information due to the visits being virtual.
Whilst a virtual visit could allow healthcare professionals to assess the state of a property and establish any adjustments that should be considered, they would not be able to use sensory information as they would for face-to-face visits. For example, a participant pointed out they often test the bed to see if it is too soft or they can pick up issues with the patient/environment by using their sense of smell (“If only we could have smellivision”).
One participant put forward the worry that the patient or carer might not be in his actual home when the visit is carried out: “how do we know this is really their home? How do I know the individual is who I think it is?”.
The reliability of measurements and assessment carried out precisely during such a visit (such as room size, height of counters, steps etc.) was also questioned, as it would rely on the ability of the patient or carer to carry out the actions appropriately.
3.2. Facilitators/benefits
The main facilitators were related to three different classes of users:
health professionals/NHS services
patients
society at large
For health professionals the main facilitators were related to service efficiency. First of all, the discharge process would be sped up by virtual visits, as it would reduce the time needed for travelling to the home and carrying out the visit, therefore increasing the number of visits that an OT can carry out and decreasing waiting lists, as evidenced by the User story in . This would match the “Discharge to assessFootnote6” framework guidelines of ensuring visits and follow ups are rapid and efficient. The cost of each visit would also be reduced, as it would require less time and less transport costs. The consequences of a patient not attending an appointment would also be minimised, as the OT would not have spent the time and the money on transport. The prototype also allowed OTs to compile reports during the visit itself instead of afterwards, therefore reducing again the time needed. Moreover, the possibility of sharing a virtual visit (or its content) would allow linking in with other agencies without the need for all agencies to travel.
Safety of remote visits was also seen as a very important facilitator; several workshops’ participants pointed out risks to their safety due to travelling at unusual times of the day to reach a destination, or due to dangerous or unhygienic homes. Sometimes if a visit is deemed particularly dangerous more than one OT needs to carry out the visit. A virtual visit would shield the OTs from the risk.
Patients would benefit from the new technology as it would allow them to be more involved in the management of their health and of their visits. The involvement of patients and their families in the management of their condition is a topic at the core of NHS digital guidelines, TOPOL review and “Discharge to assessFootnote7” framework. Family and carers could easily be involved in the process, even if they do not live near their relative or they have a busy schedule. Time savings derived from increased service efficiency would mean better care for the patients, as they would be able to carry out visits that currently are deemed non-essentials (and therefore not carried out). The possibility of supporting patients in a larger geographic area was also identified, as patients are often not local (e.g., holidaymakers) and they need to be discharged either with a costly home visit or without a visit. The possibility of sharing visits between agencies would enable a more integrated patient care, again fitting in the “Discharge to assess” guidelines: for example mental health specialists could be involved in a virtual visit for a patient in a convenient manner and the patient would not need to have different assessment carried out by different agencies at different times.
A remote home assessment could also support patients having mobility issues as they would not need to travel to their appointment. One example was that of a wheelchair user that mentioned how sometimes he needs to book an appointment because a part of his wheelchair is not working properly. After the appointment is carried out, he then needs to wait for the equipment to be fixed in a follow up visit. Using a virtual visit this process could be simplified, thus reducing discomfort and anxiety.
Society at large would benefit as reducing travel time would immediately bring social and environmental benefits. Less travel time equals less pollutions and indirectly improves population’s health.
4. Discussion
In light of the identified barriers and facilitators, we discussed how the prototype could be designed to increase chances of adoption. From these discussions a set of guidelines was identified, related both to the interface of the proposed system and to the design of the service itself. The discussion section is concluded by an overview of how virtual home assessments solutions should be compliant with policies and a presentation of limitations in the current study and future work.
4.1. Guidelines
4.1.1. Guideline 1: Security must not be invisible
All participants, independently from their role, expressed a desire to be visually reminded in the interface of the security precautions, for example with a pop-up or a textual message over-impressed on the interface when the connection is established that details the security of the connection and allows a participant to click on a button or a link to find out more information about the security level.
Participants also asked to have a visual reminder of where the data is stored every time new data is archived and for how long. Whilst information storage details depend on the information governance requirements of the organisation, patients would like to decide how long the information would be stored for; for example, authorising information to be stored for longer than the maximum should they want to (and should longer storage be of clinical value). This information should be presented in multi-modal manner to allow for accessibility (see guideline below for more details).
In summary, we recommend that future systems should provide evidence of security at every step to gain and maintain the trust of users.
4.1.2. Guideline 2: Guidance/help features should be customisable and multimodal
All participants recommended having customisable and multimodal help features, to increase accessibility. For example, they would like to request help by using a Help Button or by Voice Activation. The help should then be provided using the same modality it was requested as. This will support patients that might have eyesight or motor disabilities.
4.1.3. Guideline 3: Give back control to patients
Most telehealth pilots are implemented by choosing a service where the new solution will be deployed and by evaluating the outcomes. In the preliminary phases of this study the project team elected an opt-in approach, where the team would pre-select which patients were suitable for the remote assessment and they were then offered the possibility to join. Based on the results of our study, we recommend a different, patient-centred, process: patients should be offered the new service and be the ones to choose if they want to use it instead of being pre-screened.
Another recommendation is to prepare a leaflet containing details of the new virtual visit service, with requirements for technology and friend/carer/volunteer support, availability of times/hours and description of the process. Any information given should be able to support patients with learning difficulties and it was recommended that a Speech and Language Therapist be involved with this.
4.1.4. Guideline 4: the visit should leave no traces
Given the application can be used on any private phone, it is fundamental to ensure no record of any visit remains on the phone. All images or videos captured must not be saved in any form on the users’ phone.
4.1.5. Guideline 5: Environment should be private, comfortable and professional
The virtual visit should be carried out in a professional environment, so that the patient is reassured that the healthcare professional is paying full attention and there are no patient confidentiality issues. No distracting background images, or sound should be present during the virtual visit. The healthcare professional should always ensure at the beginning of the visit that the quality of the audio and video is suitable before starting.
4.1.6. Guideline 6: Multi-user support
The system should support adding more than one user to the virtual visit, so that other healthcare professionals could be involved or that patients could have support from family/carers.
4.1.7. Guideline 7: Identity/location check
Any telehealth system should have inbuilt strategies to enable confirmation of the patient’s identity and home location. This could be a technological solution, for example GPS collection from the device to confirm the location where the visit takes place is the same as the address on the patient’s record, or a process solution or a mixture of both. For example, in the protocol of the site visit there could be the request of seeing the property being approached and accessed to confirm this is the agreed location, comparing it with GPS reading and map information. ID could be verified by using an online government approved solutions, such as Government Gateway, or by showing ID to the camera and keeping a recording of the ID for future reference.
4.2. Policy compliance
In order for new healthcare technologies to be adopted in practice it is fundamental to prove their compliance with policies and guidelines. Here we illustrate how out study has complied with the NHS Digital Design principles:Footnote8
Put people at the heart of everything you do: our study has adopted a patient centric approach, focussing on what the patient needs and thinks about this technology. We have ensured we have patient representatives on our strategic steering group and we have consulted three different patient and public involvement groups.
Design for the Outcome: stakeholder consultations have informed the design of the technology and also the clinical development. The outcome we aim for is to improve the lives of frail elderly or people with long term conditions by reducing the time spent waiting for visits or for decisions to be made about the home environment which impact on the length of stay in hospital, we want to prevent admission by having quick assessments of the home and making decisions quicker therefore reducing time spent in hospital.
Be Inclusive: we carried out wide consultations with a variety of users, with different roles and characteristics. Our solution is designed to be inclusive by enabling home assessments that would not be possible otherwise.
Design for context: The full project this study is part of has been testing solutions in context to prove the feasibility of the concept.
Design for trust: we have addressed in detail how to achieve users’ trust, resulting in design recommendations.
Test your assumptions: We have been iteratively testing assumptions we made with user and stakeholder feedback.
Make, learn, iterate: this has been the founding basis of our mixed method approach.
Do the hard work to make it simple: we put emphasis on understanding the factors that enable a fairly “simple” technology (from a technical point of view) to be translated into clinical practice.
Make things open, it makes things better: We have had workshops, conferences and celebration events to feedback to our stakeholders.
Moreover, this project has approached the development and exploration of deployment of telehealth technology based on the three principles proposed by the TOPOL Review [Citation13]:
Patients included as partners and informed about health technologies.
The healthcare workforce needs expertise and guidance to evaluate new technologies, grounded in real-world evidence.
The gift of time; wherever possible the adoption of new technologies should enable staff to gain more time to care.
The approach described in this project fits within the “Discharge to assessFootnote9” framework as it would facilitate assessments to be done promptly (within 2 h) and any follow-up to be quickly triggered, as some other services could be involved in the video consultation, or a new assessment could be scheduled for any other relevant services that would need to act rapidly. It would also support patient-centred care, by providing a platform that patients and their families can use to be involved in decision-making and supporting continuity of communication (all services could share the same notes and access the same system to be in touch with the patient and the families).
4.3. Study limitations and future studies
In our study we have not looked at the implication that different type of diseases/illnesses and disabilities have on the use of telehealth applications. A future study should understand the illness-related factors that influence the usage of telehealth applications and what are the design implications.
Another limitation of our study was the local dimension: all the user studies were run in the same city in UK, therefore potentially missing out on the analysis of geographical and cultural factors that may affect the use of telehealth. In a future study we would look at replicating our analysis in a different cultural context, to understand if the outcomes are the same or different and what are the main variances.
Future steps for our work are the implementation of a revised prototype, re-designed considering the design guidelines identified and the pilot of the system in real life case study. We have already identified three pilot areas with interested users, such as dieticians (where remote visits could be used in an educational manner, to show the patient how to cook a specific meal and observe their progress), neurologists (to perform remote memory clinics) and emergency services (to support ambulance professionals in having immediately visibility of the emergency scene before they reach it). In these pilots we would look to run not only user acceptance and usability studies but also health economic studies analysing the cost-saving impact of virtual visits. Whilst a previous study has already proven that for just one service in a local hospital trust (stroke and wheelchair services) there was an estimate of £81,000 savings per year without accounting for reduced delayed transfers of care, more health economics analysis should be performed to ensure effective translation into healthcare services.
Acknowledgments
We thank all the volunteers that took part to the workshops and provided us with insightful comments and design advice. The authors gratefully acknowledge grants from RESEARCH ENGLAND/HEFCE, HEIF (Viva feasibility in practice, Grant number: 162509).
Disclosure statement
No potential competing interest was reported by the author(s).
Additional information
Funding
Notes
References
- Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736–771.
- Wootton R. Twenty years of telemedicine in chronic disease management-an evidence synthesis. J Telemed Telecare. 2012;18(4):211–220.
- Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for Coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309–313.
- Read J, Cudd P, Mazumdar S, et al. Digitising the acute service home assessment. Thousand Oaks: SAGE Publications; 2017.
- Zimmerman J, Forlizzi J. 2008. The role of design artifacts in design theory construction. Artifact 2:41–45.
- Drummond A, Whitehead P, Fellows K, et al. Occupational therapy predischarge home visits for patients with a stroke: What is national practice? Br J Occup Ther. 2012;75(9):396–402.
- Sturesson L, Groth K. Clinicians’ selection criteria for video visits in outpatient care: qualitative study. J Med Internet Res. 2018;20(11):e288.
- Greenhalgh T, Shaw S, Wherton J, et al. Desirée Campbell-Richards, seendy ramoutar, anna collard and Isabel hodkinson. 2018. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J Med Internet Res. 2018;20(4):e150. https://www.jmir.org/2018/4/e150/
- Østervang C, Vedel Vestergaard L, Dieperink KB, et al. Patient rounds with video-consulted relatives: qualitative study on possibilities and barriers from the perspective of healthcare providers. J Med Internet Res. 2019;21(3):e12584.
- Frydenrejn Funderskov K, Raunkiaer M, Boe Danbjørg D, et al. Experiences with video consultations in specialized palliative home-care: qualitative study of patient and relative perspectives. J Med Internet Res. 2019;21(3):e10208–e10208.
- Ninnis K, Van Den Berg M, Lannin NA, et al. Information and communication technology use within occupational therapy home assessments: a scoping review. Br J Occup Ther. 2019;82(3):141–152.
- Nix J, Comans T. Home quick – occupational therapy home visits using mHealth, to facilitate discharge from acute admission back to the community. Int J Telerehab. 2017;9(1):47–54.
- TOPOL Review. Preparing the healthcare workforce to deliver the digital future (2019). 2019.
- Mäkelä A, Mattelmäki T. Collecting stories on user experiences to inspire design. Milton Park: Taylor and Francis; 2002.
- Özçelik Buskermolen D, Terken J, Eggenm B. Informing user experience design about users: insights from practice. In Proceedings of the CHI '12 Extended Abstracts on Human Factors in Computing Systems. Austin, Texas: ACM; 2012.
- Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):748.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks: Sage Publications; 1998.
- Beyer H, Holtzblatt K. Contextual design: defining customer-centered systems. San Francisco: Morgan Kaufmann; 1998.
- Harboe G, Huang EM. Real-world affinity diagramming practices: bridging the paper-digital gap. In Proceedings of the proceedings of the 33rd annual ACM conference on human factors in computing systems. Seoul, Republic of Korea: ACM; 2015.
- Hartson R, Pyla PS. The UX book: process and guidelines for ensuring a quality user experience. San Diego: Morgan Kaufmann; 2012.

