Abstract
The anatomical, physiological, and developmental changes which arise as children mature through childhood and adolescence support the need to develop new health technologies that meet the specific requirements of children and young people (CYP). Failing to involve CYP during the development of technology increases the risk that the outcome falls short of their expectations and needs, leading to rejection of novel interventions. Through participation in health technology development, CYP and their families can provide context, insight, personal experience and tacit knowledge to ensure that the end-product is usable, acceptable, and can be integrated into its intended environment. A nuanced, balanced understanding of the methods that can be used to facilitate participation will support researchers in choosing an effective approach to involving CYP in health technology development. Methodological approaches include patient and public involvement and engagement, co-design, and experienced based co-design. These methods can be used in isolation or in combination, to facilitate meaningful involvement of CYP and encourage the development of impactful solutions, in consideration of the context, stakeholders, and objectives of the project. We provide the rationale and justification for involving CYP in health technology design and development, an explanation of the methods supporting meaningful involvement, and case studies exemplifying real world application of these methods with positive outputs.
Keywords:
1. Introduction
The 1989 United Nations Convention on the Rights of the Child [Citation1] states that children and young people (CYP) have the right to express their views freely in all matters that affect them, without discrimination and with the best interests of the child as the primary consideration. CYP should therefore be involved in the development of technologies and innovations that affect their health and wellbeing. The development of technology for child health carries specific challenges that have the potential to be influenced by the involvement of CYP during every stage of the innovation pathway; children undergo anatomical, physiological, psychological, cognitive development changes as they mature requiring considerable versatility in technological solutions; the importance of social development and integration of CYP can influence the type of technology and the modality in which it is delivered; many CYP have a clear understanding of the current trends in technology use; and a process of transition or transfer of technology takes place through developmental maturation in which technology is primarily used by parents (with or without children), and subsequently transitions to a semi- or total autonomous use by young people meaning that health technology for CYP has to be versatile and adaptive if used in longer-term conditions.
Many of these challenges can be overcome by meaningfully involving stakeholders and end users throughout the design and development process; the lack of meaningful involvement of CYP often results in a poor understanding of CYP’s experiences and opinions, which can in turn limit the effectiveness and applicability of the research, developmentally inappropriate technologies, and worse still could result in rejection of a developed technology after many years of development.
Meaningfully involving CYP ensures that unmet needs are identified and validated, and that solutions effectively address real problems in contexts that are relevant to the young person. Involving CYP in child health technology development is therefore not just the right thing to do, it also results in solutions that are more effective and contextually-appropriate [Citation2]. Meaningful involvement requires consulting and listening to CYP and families with relevant and lived experience throughout the research process, and modifying designs and plans in response to CYP’s unique and insightful contributions. The meaningful involvement of CYP not only benefits researchers, but often provides significant benefits to CYP and families; it gives CYP the opportunity to voice their opinions resulting in a coalition of knowledge from the younger generation, to make a contribution to their community, to develop transferable and social skills, as well as to grow in confidence, self-esteem, and knowledge [Citation3].
There are many approaches to facilitate the meaningful involvement of CYP in health technology development, including patient and public involvement and engagement (PPIE), co-design, and experience-based co-design (EBCD). However, as the involvement of patients and end users gains increasing momentum and support in healthcare research, a plurality of uses and understandings of what is “best practice” is emerging, as well as a number of novel challenges. For example, the Covid-19 pandemic rapidly brought issues of digital exclusion, privacy, and data protection sharply into focus [Citation4–6]. Furthermore, a recent scoping review revealed that CYP have clear concerns and anxieties about the development and use of health technologies that need to be considered [Citation7]. There is therefore often confusion as to what each of these approaches entail and the situations where it is appropriate to use them. This problem is often compounded by the misuse of terminology or substitution of approaches without proper consideration.
2. Patient and public involvement and engagement (PPIE)
PPIE is an umbrella term to refer to both patient and public involvement (PPI) and patient and public engagement (PPE). PPI is defined as research that is done “with” or “by” patients or members of the public rather than “to”, “about”, or “for” them [Citation8], meaning that patients and members of the public with relevant experience contribute to how research studies are designed, conducted, and disseminated. PPI may also involve patients or members of the public being co-applicants on research funding applications and joining project steering groups. In contrast, PPE refers to information about research studies being shared with patients and the public [Citation9]. Importantly, PPIE is not the same as patients or members of the public participating in research studies.
Historically, the importance of PPIE has not been recognised, with researchers asking patients and members of the public to approve their largely finalised plans without sufficient consideration of their feedback. This poorly conducted PPIE “rubber-stamping” adds limited value to research [Citation10]. To counteract this, in 2019 the NIHR published a framework to improve the quality and consistency of PPIE across research studies [Citation11]. NIHR INVOLVE guidelines have also been published to improve PPIE with CYP and act as a guide and template to involve and appropriately remunerate patients and the public [Citation12].
There is an increasing awareness that PPIE can add significant value to research studies; well-conducted PPIE provides research teams with valuable and unique insights from people with relevant and lived experience, thereby improving the quality and relevance of research studies, which in turn results in improved participant recruitment and retention [Citation13] and greater impact of study findings. PPIE is now also a requirement from most funding bodies and there are dedicated grants to support PPIE in the planning and grant application stages (e.g., NIHR Research Delivery Service Public Involvement Fund).
However, there remains a lot of variability and uncertainty around what constitutes PPIE and there is still considerable room for improvement [Citation14]. For example, many PPIE groups lack sufficient diversity and are therefore under-represented. This has clear implications for the generalisability of the PPIE feedback and guidance. Moreover, many organisations struggle to recruit CYP to take part in PPIE activities, and therefore similar groups of CYP often provide their input and expertise across multiple research projects. The involvement of CYP in PPIE activities also remains poorly reported in research studies [Citation15]. Researchers therefore need to evaluate their recruitment strategies and ensure that PPIE groups are representative of the specific patient population. It is also essential to involve CYP in every stage of the research process, including in the initial ideation and planning stages. Using creative, developmentally appropriate methods to engage younger children and CYP with learning difficulties and/or disabilities is also key to ensure meaningful involvement from often overlooked groups.
3. Co-design
Co-design is defined as “the creativity of designers and people not trained in design coming together in the design development process” [Citation16]. It has emerged from the field of Participatory Design, which is characterised by a focus on fostering a sense of agency within the “users” or stakeholders in the project, so that they are able to contribute their unique, situated expertise as equal partners [Citation17].
Co-design also recognises, and gives equal importance to, the different types of knowledge that participants may have, such as experiential (gained through experience), tacit (gained through learning a skill or activity), and institutional (gained through participation in an organisation or community). Some of these knowledge types are harder to elicit and communicate than others, and over recent decades, the field has developed a rich catalogue of methods and tools that utilise creative or “making” activities to access the “deep” levels of knowledge [Citation18].
The use of creative methods gains particular significance when working with CYP, by providing a range of ways for CYP to reflect on and share their lived experiences and hopes for the future, without privileging (potentially less developed) verbal communication skills.
Unlike traditional forms of “design”, users are involved from earlier stages of a project, not simply asked to give feedback on a fully formed concept. As such, co-design projects can involve stakeholders across the entire innovation pipeline, from learning about the problem, to ideation, development, testing, implementation and evaluation. However, the realities of time and funding constraints may limit projects’ co-design approach to a particular phase, such as ideation or development.
In some projects, the use of the Design Council’s “Double Diamond” model () [Citation19] provides a useful framework to describe the cycles of “divergent thinking” (opening up the field of inquiry) and “convergent thinking” (prioritising key issues/ideas) as applied to both understanding the problem and developing the solution.
Figure 1. The Design Council’s “Double Diamond” model [Citation19], illustrating the “Discover” phase (divergent thinking to think broadly about the context of the problem), “Define” phase (convergent thinking to narrow down the scope of the problem in light of this broader understanding of the context), “Develop” phase (divergent thinking to generate many, diverse ideas that could address the problem) and the “Deliver” phase (convergent thinking to prioritise the best ideas and create a considered solution).
![Figure 1. The Design Council’s “Double Diamond” model [Citation19], illustrating the “Discover” phase (divergent thinking to think broadly about the context of the problem), “Define” phase (convergent thinking to narrow down the scope of the problem in light of this broader understanding of the context), “Develop” phase (divergent thinking to generate many, diverse ideas that could address the problem) and the “Deliver” phase (convergent thinking to prioritise the best ideas and create a considered solution).](/cms/asset/c4c5d545-f826-4f32-8aad-874be78ff72c/ijmt_a_2089252_f0001_c.jpg)
Again, a range of tools can be used to support each stage of the process, such as personas, Lego® Serious Play®, service journey mapping, and prototyping [Citation20].
In recent decades, co-design approaches have expanded in healthcare research and development spaces. There is growing evidence demonstrating the benefit of this approach to bring together diverse stakeholders [Citation21] within healthcare contexts [Citation22–23] as it “implies that no viewpoint is afforded greater legitimacy than another” [Citation24]. This is critical when bringing together stakeholders who may traditionally work together with established (if unspoken) power dynamics (i.e., patients and doctors, or adults and children).
There is no fixed “route” through a co-design project, and it takes experience in order to strategically use appropriate co-design methods to meaningfully involve stakeholders. This can be perceived as both a strength and a weakness. The adaptable nature of co-design means that methods and tools can be adapted to suit the physical, cognitive, emotional, and/or logistical needs of participants, as well as respond to unexpected challenges or changes in circumstances. Beyond individual tools, the process itself is iterative in nature and allows for the incorporation of new insights as the project progresses. However, the context-specific and non-linear nature of each co-design project is at odds with the “scientific method” that dominates healthcare research. Moreover, the subjective and unquantifiable nature of the knowledge types it champions (i.e., experiential or embodied/tacit knowledge) can be viewed as less “rigorous” alongside more traditional, positivist notions of objectivity within research.
Practically, the skills needed to deliver a co-design project demand that a professional designer is involved. Whilst this has limitations in terms of cost in delivering the project, it could be argued that having designers present from an early stage (with their experience in creating products/services) help to enhance the practicality of ideas generated and implemented.
4. Experience-Based Co-design (EBCD)
In the early 2000s, the NHS Institute for Innovation and Improvement (NHS III) began to develop a new approach to service improvement, in response to a call for a more patient-centred NHS [Citation25–26]. This new approach was called Experience-Based Co-design (EBCD), and drew on design theory, tools, and techniques. Whilst EBCD resonates with “design” as a practice, there are several key differences between “co-design” and “EBCD”.
In contrast to the organic and adaptive nature of co-design, which requires design professionals in the planning and conduct of projects, EBCD is characterised by a repeatable process that can be taught to, and led by, healthcare professionals. Robert and colleagues suggest using a six-stage process over approximately 9 to 12 months, including; (1) Project set up, (2) Gathering staff experiences through observation & interviews, (3) Gathering patient and carer experiences through 12–15 filmed narrative-based interviews, (4) Workshop with staff, patients and carers to share experiences, prompted by a “trigger film” edited from patient narratives, (5) Small working groups create ideas to address 4–6 priority issues over 3–4 months, (6) Celebration & review event [Citation27]. An “accelerated” version of EBCD (AEBCD) is also available, using stock footage rather than creating project-specific patient narratives films and, more recently, the Point of Care Foundation (PoCF) Toolkit recommends an eight-stage approach [Citation28]. Overall, the EBCD approach represents a replicable set of methods, with a growing focus on the evaluation of EBCD projects, making it a trusted methodology in healthcare research [Citation26].
Through a “co-design” process, EBCD entails staff, patients and carers reflecting on their experiences of a service, working together to identify improvement priorities, devising and implementing changes, and then jointly reflecting on their achievements. It is perhaps best aligned with the earlier stages of the innovation pipeline and research process, due to its emphasis on capturing diverse perspectives of an existing healthcare service, with implementation mostly occurring locally as a “test” of these initial concepts. Whilst this process draws on some methods that have long been a part of design practice (such as collaboratively mapping the emotional highs and lows of existing service journeys), it has been suggested that the solutions generated by EBCD approaches can be incremental rather than innovative in nature, perhaps due to a lack of ideation tools [Citation29]. In addition, it has been noted that specific guidance on how to address inherent power imbalances between patients and healthcare professionals when collaborating in an EBCD process is lacking [Citation26,Citation30].
As such, it is argued that whilst co-design can be considered “designerly” (led by design-trained professional(s) who deliver a bespoke, innovative process, but is hard to predict and evidence) [Citation31], EBCD is “design-like” (i.e., a repeatable process that can be planned within rigid schedules and led by in-house healthcare teams, but can be limited in terms of creative, equal involvement of patients).
Despite its origins in service re-design, EBCD can still provide a useful approach to innovation in health technologies through its consideration of the “journey” that users undertake in their use of a new technology. This can be useful in ensuring that new technologies can adapt to and/or fit within existing healthcare services, and the lifestyles of users themselves. This is vital in paediatrics in particular, when the “users” may be parents, teachers, healthcare professionals or the child themselves. Moreover, applying an EBCD approach increases the likelihood that the “human” elements (such as emotions and experiences elicited by the technology) are considered as equally important to other factors (such as efficiency or sustainability) when designing the functionality of the new technologies.
5. Choosing an approach
Each of the three approaches have different objectives and strengths. As such, the authors advocate for a nuanced, balanced understanding of each, to support researchers in choosing an “effective” approach, as opposed to propagating the notion of a “right” approach. Here, “effective” can be defined as an approach that facilitates meaningful involvement of CYP as much as possible and encourages the development of impactful solutions, in consideration of the context, stakeholders, and objectives of the project. To support these decisions, some factors to consider relating to each approach are summarised in .
Table 1. An overview of some of the strengths, limitations and potential applications of PPIE, Co-design and EBCD approaches, informed by the authors’ experience and understanding of the relevant literature.
Since each approach has different objectives, it can often be most appropriate to use multiple approaches for one project. As such, four case studies are discussed below that harness both single and multiple approaches, to illustrate their strengths in practice.
5.1. Case study 1: Juvenile idiopathic arthritis (JIA) toolkit
5.1.1. Context and unmet need
Juvenile Idiopathic Arthritis (JIA) is an autoimmune disease that causes inflammation of the joints [Citation32] with 1,000–1,500 new diagnoses in the UK each year [Citation33]. JIA can affect CYP of all ages with experiences of the condition varying significantly, however key symptoms include ongoing pain and stiffness, making everyday activities difficult to achieve. Self-management activities to alleviate symptoms of JIA do exist, but they are currently not engaging for CYP. As such, a key unmet need for supporting CYP with JIA in the self-management of their condition was identified: using technology that can adapt to this plurality of experience.
5.1.2. Approach and findings/solution
Four key stakeholder groups were involved in this project, recognising that each group plays a crucial role in JIA management: CYP with JIA, their parents/carers, healthcare professionals, and school teachers.
A co-design approach was used as it enabled a flexibility that responded to the individual nature of the condition and the unique experiences of stakeholders. For example, storyboards were used for younger children to embody the ideas generated, whilst rough prototypes with prompts were used for older children, enabling them to engage by physicalising intangible aspects in an understandable format.
The stakeholder group priorities for innovation varied significantly and a diverse range of unexpected, but important unmet needs related to self-management were identified. For example, whilst CYP and parents were most concerned with pain management and symptom tracking (respectively), healthcare professionals focussed on motivating CYP to take part in physiotherapy exercises, and teachers requested better communication of when CYP genuinely needed help. In response to this, a suite of technology-based tools (the JIA Toolkit) were developed to support personalised condition management.
5.1.3. Key lessons
The creative nature of the co-design activities allowed CYP of a range of ages to reflect on and contribute deep levels of knowledge about their condition and the impacts on their daily lives, which might not have been achieved by verbal-only communication. The co-design approach also allowed competing (sometimes conflicting) priorities from each stakeholder group to co-exist and be considered equally, helping to reduce the hierarchical power dynamics that can exist within healthcare collaborations. This enabled deeper engagement, with participants building on each others’ ideas with the understanding that their point of view had also been considered. In this way, co-design can enable a space for non-consensus. Rather than forcing a convergence on a single (inappropriate) solution, a toolbox of innovations were created (currently being developed further), with each stakeholder need being addressed by a different tool (a key challenge of innovating for CYP as previously discussed). This allowed CYP and their parents to tailor condition management according to their specific needs, improved communication in the classroom for school teachers and provided a source of motivation for physio stretches, thereby also responding to the need of healthcare professionals [Citation34].
5.2. Case study 2: “Belt Up”
5.2.1. Context and unmet need
Narcolepsy is a lifelong, debilitating condition that affects all areas of a child’s life. Narcolepsy is characterised by excessive daytime sleepiness and attacks of muscle weakness (known as “cataplexy”), and affects approximately 0.025% of the general population [Citation35]. Many of the impacts of living with narcolepsy can be difficult to recall outside of the contexts they are experienced in, and perhaps even harder to articulate – particularly for younger children. As such, a team of researchers, designers and clinicians set out to better understand the unmet needs of this population.
5.2.2. Approach and findings/solution
A PPIE focus group was held at a sleep clinic “family day” to learn about difficulties faced by CYP with narcolepsy. The key challenge raised by CYP and families was addressing the need for head and neck support during car journeys, as CYP with narcolepsy can sleep so deeply that they can damage their skin from leaning on the seatbelt, or even “end up in the footwell”. This finding supported a successful funding application to address this unmet need. A co-design process was then adopted, with families engaged at every step using creative storyboarding activities, sharing of current tips and tricks, assessing current travel aids, and interactive testing of new prototype head and neck supports. Through this process, the unmet need was refined further and a range of prototype supports were developed.
5.2.3. Key lessons
At the start of this project, PPIE activities were chosen as a quick, cheap, and easy way of conducting a broad scoping exercise in contexts where there has not yet been a great deal of research, as such it was considered an appropriate approach at the initial narcolepsy “family day”. In this case study, PPIE allowed families to be involved from the inception of a project, ensuring the application for further funding addressed real and validated needs of CYP and families.
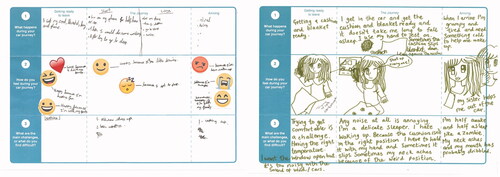
The complexity of this identified need was then further explored by a subsequent co-design process. Whilst a co-design process may be more costly in terms of time and resource, it was chosen in this project because, as in case study 1, the use of creative tools to support CYP’s reflection and sharing of their experiences was crucial in properly framing the challenges they face (see ).
Figure 2. An example tool used to support the co-design process in this project. In this activity, CYP and parents are asked to describe the different steps they go through in a typical car journey (the top row of the tool). They then map the emotions felt at each of these steps (the second row of the tool). Finally, they explain the challenges at the points where negative emotions are recorded (the third row of the tool). These challenges are the focus of subsequent ideation activities.
Beyond experiential knowledge, the development of a head and neck support for these CYP also required tacit knowledge (i.e., what “feels” right in the car, or how easy it is to get on & off). As such, the use of prototypes within the co-design approach was key, and allowed CYP to explore the new ideas in an embodied way, and express their thoughts by altering the prototypes as necessary. Indeed, the use of making activities with CYP helped to reframe the problem entirely, highlighting the need for a full body support, rather than simply the head and neck [Citation36].
5.3. Case study 3: “type 1 diabetes mellitus chatbot”
5.3.1. Context and unmet need
NIHR CYP MedTech is leading on an NIHR funded project to design and evaluate the first NHS clinically approved chatbot to support YP with type 1 diabetes mellitus (T1DM) as they move from paediatric to adult health services. A chatbot is a computer program that people can access on their phone, tablet, or computer that simulates conversation and answers questions in real-time. The chatbot will provide YP with 24/7 access to relevant, developmentally appropriate, and clinically approved information. The need for a chatbot was identified via a PPIE survey completed by YP before or after one of their clinic appointments. Over 75% of 13–21 year olds with T1DM (n = 30) thought that a chatbot would enhance their care.
5.3.2. Approach and findings/solution
The project is inviting YP with T1DM, their parents/carers, and health professionals to take part in a series of focus groups and interviews. These focus groups and interviews are using an iterative, co-design approach to gain an in-depth understanding of YP’s needs, preferences, and opinions about the chatbot. The diabetes clinical teams at the four NHS trusts are also advising on and approving the clinical information within the chatbot. Self-management theory and the COM-B (capability, opportunity, motivation – behaviour) model of behaviour change [Citation37] are being used to guide focus group discussions.
In addition, the steering group is working in partnership with a diverse and inclusive group of YP who are helping to guide the project. The steering group is following NIHR INVOLVE guidance and asking the PPIE group to provide input into all stages of the project. The team have also partnered with a digital inclusion agency to explore barriers faced by YP from under-served groups to ensure the chatbot is relevant and accessible to as many YP as possible. Combining co-design and PPIE approaches ensures that the content and design of the chatbot is informed by YP’s lived experiences (co-design) and that the study is designed and conducted in a way that meets YP’s needs and maximises YP’s involvement.
5.3.3. Key lessons
Whilst case study 2 used a staged blended approach (i.e., a PPIE phase followed by a co-design phase), this case study demonstrates the possibility of creating a concurrent blended approach (i.e., facilitating a PPIE steering group alongside a co-design process). This case study also demonstrates the possibility and benefits of conducting a multi-site NHS research study that combines PPIE, co-design, and a clinical evaluation in collaboration with multiple university, NHS, and industry partners.
5.4. Case study 4: “superhero vest”
5.4.1. Context and unmet need
NHS patients and families face a number of challenges when securing and maintaining enteral feeding lines and devices. Children and infants with complex nutritional needs usually require invasive devices which are vital for survival and management of conditions. Children with learning disabilities may tug on their device and not fully understand the implications of doing so. Trauma to the device site and subsequent accidental removal of the device can cause significant bleeding, stress of child and carer, risk of infection, and delayed nutrition and medication [Citation38]. As such, there is a need for a device to secure enteral feeding equipment designed specifically for CYP.
5.4.2. Approach and findings/solution
Initially, a co-design approach was used to understand the needs of families and healthcare professionals around designing a new secure system for enteral feeding equipment. Whilst this approach was successful in creating a range of solutions for many children, it also became clear that one child had highly complex needs that could not be addressed by any of the proposed prototypes. As such, a separate spin out EBCD project was conducted between Tookie Limited (small company) and NIHR CYP MedTech to accommodate the bespoke, emergent needs of this child.
The EBCD approach [Citation28], used knowledge of appropriate materials and utilised Pioneering 3 D body mapping technology to map the lines and devices on the child’s torso, negating any stress that may have been caused by taking repeated physical measurements (see ). These measurements were combined with photo images of the child to provide accurate marker points during the garment design process. Several design features were developed with maximum input from the family (e.g., embedding neoprene into garment sections to prevent pulling of lines and devices) before a prototype was provided and trialled and a finished garment provided.
5.4.3. Key lessons
The problem addressed in this case study emerged thanks to the initial co-design approach facilitating the expression of a diversity of opinion, as described in case study 1. In this instance, taking a separate, subsequent EBCD approach, chosen to enable a relatively quick and effective turnaround time involving both the family and the clinical team due to the urgent need and highly individualised nature of the solution. In other words, whilst the costs associated with an in-depth co-design approach would be difficult to implement for a solution aimed at a very small patient population (in this case, one child), there are still ways to meaningfully involve CYP in these niche, but highly impactful, opportunities for innovation. Moreover, the garment has improved the child’s and family’s overall quality of life; the child has stated that he loves the superhero aesthetic and wearing the garment.
6. Discussion
Whilst the studies above took place prior to 2020, it is pertinent to note that approaches to the “meaningful involvement” of CYP in health technology development must be responsive to emerging challenges and contexts of use. The onset of the Covid-19 pandemic has had significant impacts on all areas of our lives, and the field of healthcare research is no exception. In many instances, the need for social distancing and the merging of home, school, and work lives called for a pause in many projects, whilst others looked to novel, online solutions to continue involving research participants in different ways. Whilst this has opened up previously challenging opportunities to engage under-served groups, some researchers also critique the default to digital/online approaches that were prevalent throughout the research landscape in 2020 and 2021 [Citation39]. During the pandemic, NIHR CYP MedTech explored the use of online focus groups, online patient advisory groups, postal activity packs, online surveys, online whiteboard spaces, and more, with a high level of success. However, further work is needed to assess the effectiveness of remote involvement during and beyond the pandemic. The topic of challenges and opportunities in the Covid-19 era is discussed further in our companion paper in this special issue [Citation40].
7. Conclusions
Whilst there is a growing understanding of the benefits of meaningfully involving CYP in paediatric healthcare research, there is currently little reflection on what has been achieved using PPIE, Co-design, or EBCD approaches when developing health technology for CYP. It is essential that future research focuses on better understanding the benefits and limitations of different approaches to ensure that we utilise approaches that are effective and address the project objectives.
There is no “right” approach to meaningfully involve CYP in the development of health technology. Rather, a more nuanced understanding of the unique strengths of each is required, and a need for considered deployment of “effective” approaches according to the context, stakeholders, and objectives of each project.
Acknowledgements
The research reported in this publication was supported by the National Institute for Health Research (NIHR) Children and Young People MedTech Co-operative. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The authors would also like to acknowledge the CYP and families who have taken part in NIHR CYP MedTech and D4D activities. All images are included with consent from the owners and individuals featured.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- UNICEF. United Nations Convention on the Rights of the Child; 1989.
- Powell P, Wheeler G, Redford C, et al. The suitability and acceptability of a co-designed prototype psychoeducational activity book for seven- to eleven-year-olds with ADHD. Design for Health. 2021;5(1):4–25.
- Brady L-M, Graham B. Social research with children and young people a practical guide. Bristol: Policy Press Shorts; 2019.
- Fahey RA, Hino A. COVID-19, digital privacy, and the social limits on data-focused public health responses. Int J Inf Manage. 2020;55:102181.
- De’ R, Pandey N, Pal A. Impact of digital surge during Covid-19 pandemic: a viewpoint on research and practice. Int J Inf Manage. 2020;55:102171.
- Davis A, Gwilt I, Wallace N, et al. Low-contact co-design: considering more flexible spatiotemporal models for the co-design workshop. Strateg Des Res J. 2021;14(1):124–137.
- Blower S, Swallow V, Maturana C, et al. Children and young people’s concerns and needs relating to their use of health technology to self-manage long-term conditions: a scoping review. Arch Dis Child. 2020;105(11):1093–1104.
- NIHR Oxford BRC: a researchers guide to PPI [Internet]; [cited 2021 Nov 09]. Available from: https://oxfordbrc.nihr.ac.uk/wp-content/uploads/2017/03/A-Researchers-Guide-to-PPI.pdf.
- NIHR INVOLVE: What is public involvement in research? [Internet]; [cited 2021 Nov 09]. Available from: https://www.invo.org.uk/find-out-more/what-is-public-involvement-in-research-2/.
- Coulter A, Ellins J. Patient-focused interventions: a review of the evidence. London: The Health Foundation; 2006.
- NIHR INVOLVE: UK standards for Public Involvement in Research: better public involvement for better health and social care research. [Internet]; [cited 2021 Nov 09]. Available from: https://www.invo.org.uk/wp-content/uploads/2019/11/UK-standards-for-public-involvement-v6.pdf.
- NIHR: Briefing notes for researchers – public involvement in NHS, health and social care research [Internet]; [cited 2021 Nov 09] Available from: https://www.nihr.ac.uk/documents/briefing-notes-for-researchers-public-involvement-in-nhs-health-and-social-care-research/27371.
- Ennis L, Wykes T. Impact of patient involvement in mental health research: longitudinal study. Br J Psychiatry. 2013;203(5):381–386.
- Rouncefield-Swales A, Harris J, Carter B, et al. Children and young people’s contributions to public involvement and engagement activities in health-related research: a scoping review. PLoS One. 2021;16(6):e0252774.
- Price A, Schroter S, Snow R, et al. Frequency of reporting on patient and public involvement (PPI) in research studies published in a general medical journal: a descriptive study. BMJ Open. 2018;8(3):e020452.
- Sanders E, Stappers P. Co-creation and the new landscapes of design. CoDesign. 2008;4(1):5–18.
- Simonsen J, Robertson T. Routledge international handbook of participatory design. New York, Routledge; 2013.
- Sanders E, Stappers P. Convivial toolbox: generative research for the front end of design. Amsterdam, BIS Publishers; 2012.
- Design Council. Design methods for developing services; 2015; [cited 2021 Nov 09]. Available from: https://www.designcouncil.org.uk/resources/guide/design-methods-developing-services.
- Langley J, Wheeler G, Partridge R, et al. Designing with and for older people. In: Woodcock A, Moody L, McDonagh D editors. Design of assistive technology for ageing populations. Cham: Springer; 2020. p 3–15.
- Crabtree B, Erickson ME, Joseph-McCullough J, et al. Finding synergies between indigenous and designerly ways of knowing. Design 4 health. Sheffield: Sheffield Hallam University; 2020. p. 129–136.
- Langley J, Ankeny U, Partridge R, et al. Co-designing resources for knowledge based self-reflection for people living with Parkinson’s disease to better enable independent living. IADE/UNIDCOM’s 10th International Conference Sense & Sensibility. 2019. Lost in (G)localization. Lisbon; 2019.
- NESTA. By Us, For Us: the power of co-design and co-delivery [Internet]; [cited 2021 Nov 09]. Available from: https://www.nesta.org.uk/report/by-us-for-us-the-power-of-co-design-and-co-delivery/.
- Bradwell P, Marr S. Making the most of collaboration: an international survey of public service co-design. London: Demos in Association with PwC’s Public Sector Research Centre; 2008.
- Bate P, Robert G. Bringing user experience to healthcare improvement: the concepts, methods and practices of experience-based design. Abingdon: Radcliffe Publishing Ltd; 2007.
- Donetto S, Pierri P, Tsianakas V, et al. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Design J. 2015;18(2):227–248.
- Robert G, Cornwell J, Locock L, et al. Patients and staff as codesigners of healthcare services. BMJ. 2015;350:g7714.
- The Point of Care Foundation: EBCD: experience-based co-design toolkit [Internet]; [cited 2021 Nov 09]. Available from: https://www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/.
- Bowen S, Dearden P, Wright D, et al. Participatory healthcare service design and innovation. In: proceedings of the participatory design conference. New York, NY: ACM Press; 2010. p. 155–158.
- Bowen S, McSeveny KM, Lockley E, et al. How was it for you? Experiences of participatory design in the UK health service. CoDesign. 2013;9(4):230–246.
- Robert G, MacDonald AS. Infrastructuring for organisational creativity and quality improvement in the healthcare sector: ‘designerly’ or ‘design-like? In: Sangiorgi D, Prendiville A, editors. Designing for service: contemporary issues and novel spaces. London: Bloomsbury; 2017.
- Versus Arthritis: State of Musculoskeletal Health [Internet]; [cited 2021 Nov 09]. Available from: https://www.versusarthritis.org/media/14594/state-of-musculoskeletal-health-2019.pdf.
- JIA at NRAS: Sobi support #WearPurpleforJIA. [Internet]; [cited 2021 Nov 09]. Available from: https://jia.org.uk/2018/06/08/sobi-support-wearpurpleforjia/.
- Ankeny U. Using a co-design approach to develop technological interventions to help children with Arthritis to be more active and independent In: Proceedings of the 6th International Conference on Design4Health, Amsterdam; 2020.
- Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol. 2018;85:21–32.
- Wheeler G, Elphick H, Langley J, et al. Co-designing a neck stabilising aid for children with narcolepsy In Proceedings of the 6th International Conference on Design4Health. Lab 4 Living, Sheffield: Sheffield Hallam University; 2020.
- Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6(1):1–2.
- Showalter CD, Kerrey B, Spellman-Kennebeck S, et al. Gastrostomy tube replacement in a pediatric ED: frequency of complications and impact of confirmatory imaging. Am J Emerg Med. 2012;30(8):1501–1506.
- Langley J, Wheeler G, Mills N, et al. Starworks: politics, power and expertise in co-producing a research, patient, practice and industry partnership for child prosthetics. In Christer K, Craig C, & Chamberlain P, editors. Design 4 Health. Sheffield: Sheffield Hallam University; 2020. p. 314–322.
- Sproson L, Mills N, Pryde L. PPIE Methodology and Adaptations due to Covid-19. 2022. [submitted].

