Abstract
The development of medical technologies that effectively meet clinical and patient needs increasingly relies upon collaborative working between clinicians, businesses and universities. While this “open” innovation process may provide access to additional resources, knowledge, and expertise the process is not frictionless. At the personal level, individuals may have different ways of working and incentives and at the organisational level, partners may have their own cultures and processes. Thus, interorganisational collaboration is not necessarily a panacea, but has advantages and disadvantages. The challenges are somewhat heightened in the MedTech sector where collaborative working cuts across established professional boundaries, brings together diverse knowledge from an array of disciplines, and often disrupts existing medical practice. Given these factors, this article presents a review of the extant management literature examining the complexities within multi-party collaboration and ways to drive these partnerships forwards. The article emphasises the critical value of interpersonal relationships within collaborations and offers means of strengthening them.
1. Introduction
Collaboration between universities and industry are relatively common in the pursuit of innovation, enabling a fusion of diverse perspectives, expertise and resources, and often unlocking the ability to solve complex socio-economic problems [Citation1]. For MedTech development, a clinical partner is required to account for the centrality of user engagement in this sector [Citation2]. A clinical partner offers a vital perspective on practical need and application, but they can also support access to patients and families to enable a user-centric approach to MedTech development [Citation3]. Consequently, where the innovation process involves multiple actors, i.e., the commercial sector, universities and clinicians, these partnerships are typically more complex [Citation2,Citation3]. This complexity results in numerous challenges. First, at the organisational level, partnerships can amplify differing incentives, processes, priorities, timelines, approaches to intellectual property (IP) and working cultures [Citation4–6]. Second, at the individual level, partners may have contradictory motivations, knowledge bases, expertise, experience and communication styles. Indeed, where partners are particularly diverse at the organisational level, such as industry, universities and clinicians, there may be a greater number of differences. Sometimes dissimilarities can have a tangible impact on the collaboration and can lead to many promising discoveries failing at the early stages of development [Citation7–10].
Several factors can enhance the likelihood of success, such as partners having prior experience of similar collaborations, prior trusting relationships between partners, and the employment of intermediaries to bridge the differences [Citation11]. Alongside these conditions, partnering organisations can actively strengthen a collaboration by increasing contextual and geographic proximities between partners. Recognising that collaborations are inherently relational in nature suggests that the social aspect of a collaboration is important in this endeavour [Citation10,Citation12,Citation13]. Interpersonal relationships are complex and often organic; yet, there are certain elements that can be nurtured, managed or mobilised to enhance collaboration.
To date, there is little evidence published that defines the factors that support a successful triadic collaboration between industry, academia and healthcare; thus, underpinning the need for future research in this area. Previous work in this field focuses on strategic alliances or collaborative projects between universities and industry, demonstrating the value of individuals and their interpersonal relationships and the drivers for successful collaboration. Nonetheless, research exploring biomedical and medical device development hints at the potential relevance of these individual level factors within the MedTech industry [Citation14–16].
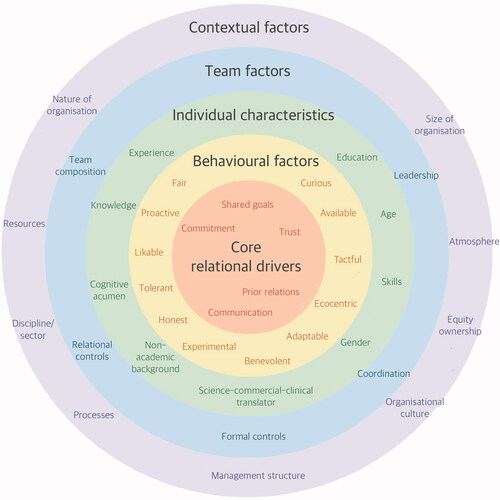
The purpose of this article is to draw on evidence from social science research to provide a review of the factors that underpin successful interorganisational collaborations. The framework presented examines contextual factors, team factors, individual characteristics and relational drivers. The subsequent sections provide an overview of each factor and the final section summarises these and offers ideas for future research.
2. Factors that influence collaboration
Collaborative relationships are complex in nature. Since they develop and evolve between the individuals within partnering organisations they are influenced by several factors. outlines the myriad influences on these collaborations including core relational drivers such as trust and commitment at the centre, behavioural factors such as an individual’s flexibility and tact, individual characteristics, including their demographic, skills and experience, team level factors, such as team composition and leadership and contextual factors such as the nature and size of the organisation, the management structure and the wider discipline or sector the relationship is operating within.
Proximities (i.e., similarities or closeness) between partners, at either an individual or organisational level, can bridge partners’ differences and enhance the effectiveness of collaborations [Citation17–19]. These proximities can exist in various dimensions such as sharing similar knowledge or expertise (“cognitive”); processes (“organisational”); existing relationships (“social”); shared rules, habits or values (“institutional”); or geographic closeness [Citation17,Citation20,Citation21]. Even if partners differ in some dimensions, closeness in other elements can offset this diversity, for example, geographic proximity can act as a substitute for the organisational, institutional and social proximities by enabling greater face-to-face interaction [Citation22]. Geographic closeness between university and clinical partners appears relatively common in MedTech collaborations, with some progressing to long-term partnerships at the organisational level (e.g., the Centre for Healthcare Technologies in Nottingham [Citation23] and the Christobel Pankhurst Institute for Health Technology being created in Manchester [Citation24], both of which involve a local university and NHS Trust). However, the current COVID-19 pandemic may have somewhat levelled the playing field in terms of geographic proximity, promoting virtual meetings through video calls in place of face-to-face meetings. Thus, partners may be more reliant on developing temporary proximity through online meetings [Citation25] given that the traditional boundaries related to geographic proximity (e.g., travel time between partners) are reduced by technology.
Furthermore, although academic, industry and clinical partners are institutionally diverse, the level of proximity across various dimensions should not be viewed as fixed, rather they should be viewed as dynamic and open to change [Citation11]. In the early stages, proximity on one level can tether collaborating organisations whilst other dimensions of proximity are built, for example, social proximity or interpersonal relationships holding partners together whilst mutual understanding and a shared language is developed [Citation20]. For example, a study of innovation within hospitals found that in addition to geographical differences, the managerial, cultural and organisational differences between hospitals and other organisations, particularly subcontracted organisations, hampered the effectiveness of their interactions [Citation2]. However, a common cultural background was advantageous to establish tacit codes of conduct and enhance communication [Citation2].
As organisations learn to work together, proximity can therefore develop and evolve (and potentially change), with collaborators becoming closer, albeit challenges may occur during this evolution [Citation26]. In some cases, proximities may develop passively under the right circumstances (e.g., frequent interaction). However, in other cases they need to be actively managed and strengthened. Therefore, to facilitate greater proximity, partners can undertake activities that reduce the institutional differences; for example, investing in the interpersonal relationships between key individuals (i.e., recognising their value and making time and other resources available to build and nurture social connections) [Citation27].
Relationships between individuals are fundamental in shaping successful collaborations [Citation28–32]. In the beginning, relationships can catalyse the formation of a collaboration and allow organisations to gather information about a potential partner’s abilities and resources [Citation32]. Relationships can also speed up the formation process and help to build and strengthen trust [Citation32]. Relationships can reduce real or perceived risk and uncertainty in the collaboration, deal with issues effectively and help to resolve small conflicts before they escalate [Citation32,Citation33]. They can also foster joint problem solving, reduce the need for excessive monitoring and create a moral obligation that encourages individuals to exceed their contractual agreements [Citation32,Citation33]. Furthermore, relationships not only assist the smooth running of a project, but they can open up other collaborative opportunities [Citation28]. Social and relational exchange theories also argue that relational-based exchanges (i.e., exchanges made as part of building a longer-term relationship) outperform transactional-based exchanges (e.g., a basic exchange of services for payment) because they enable partners to adapt to new conditions [Citation34]. Within MedTech development, relationships are said to be particularly important during the early development phase where scientific, clinical, commercial and regulatory expertise need to be combined [Citation14,Citation35]. In this phase, partners likely begin working together more closely and intensely. During this “intermeshing,” and perhaps whilst trust is yet to be established, it is likely that differences (e.g., in motivations, expectations, cultures and processes) are brought to the surface and require harmonisation to avoid the ill effects of conflict. Thus, relationships help to temper these differences and find a mutually agreeable way forwards.
Certain elements of a relationship can improve collaborative success. The extent and quality of communication enables easier exchange of information and facilitates the development of trust and commitment [Citation31]. In collaborative innovation, strong relationships facilitate the exchange of information, which is particularly crucial in order to define and complete the project, generate mutual value, and drive success in research projects through to commercialisation, acknowledging that relationships are important in this field due to the inherent complexity and risks [Citation36]. In MedTech development, clinicians and patients share knowledge about clinical needs, service integration and user requirements in a different setting, and thus a relationship with these key stakeholders will enhance the chances of success. This exchange of expertise not only helps in creating a product, but also in ensuring it meets users’ needs. Organisations must however acknowledge that relational factors alone cannot guarantee relationship success [Citation31,Citation37]. Additional elements augment the influence of relationships such as complementary resources and each partner’s ability to effectively deploy their resources [Citation37,Citation38]. Additionally, it is possible for relationships to break down or individuals can move on to new ventures. Though individuals can be replaced, it takes time for new relationships to be forged, and replacements may not share the same enthusiasm or chemistry of their predecessors [Citation32]. In spite of these caveats, collaborations must have relationships placed at the core [Citation28]. Considering their deep influence, partners must value the importance of interpersonal relationships and socio-psychological aspects of a collaboration, just as they invest in the financial and technical elements to achieve success [Citation12]. Understanding the key dimensions of relationships and how they can be nurtured can allow partners to unlock the ability to strengthen collaborations.
3. Key roles in collaboration
The individuals at the interface between collaborating organisations can be extremely influential [Citation14]. Ultimately, these individuals help to nurture the relational drivers that improve proximities between partners.
Where partners do not have prior experience of working together, intermediaries can help to broker relationships, acting as translators for the different languages spoken by partners [Citation8]. In this way, intermediaries can strengthen cognitive proximities between partners (shared knowledge and understanding) and potentially also organisational proximities by offering “neutral” processes. In the UK, there are government funded intermediaries, including those specialising in MedTech collaborations, such as the NIHR MedTech and In-Vitro Diagnostics Cooperatives (NIHR MICs) [Citation39], Medilink [Citation40] and the AHSN network [Citation41]. They serve to facilitate collaborations between the commercial sector, academics across multiple specialty areas and clinicians to support the development of health technology. In addition, there are agencies such as the Medipex Healthcare Innovation Hub [Citation42] that support regulation and commercialisation to accelerate technology development to market. Universities can also introduce and bridge clinical partners to industry [Citation2], perhaps because they are seen as a public sector ally with similar habits and values (i.e., greater institutional proximity). Furthermore, where collaborative innovation involves a university, the university’s Technology Transfer Office, University Incubators or Collaborative Research Centres offer an intermediary to support relationship building and collaboration.
The aim of an intermediary is to reduce the organisational complexity and distance between the different logics within partners, e.g., their different values, beliefs, assumptions and rules [Citation11]. Towards this, they use various activities to increase proximity and improve technology transfer, such as employing people with hybrid backgrounds (backgrounds or experience from different professions) to reduce cognitive distance; promoting frequent meetings and open discussions to reduce geographical distance; simplifying bureaucracy to increase organisational proximity and promoting and organising events and workshops to expand social networks [Citation11]. Proximities are strongly related to context-specific characteristics, so the type of activities implemented will be influenced by the complexity of the knowledge being transferred and the type of actors involved [Citation11]. As an example, the NIHR Children and Young People MedTech Co-operative (NIHR CYP MedTech) is one of 11 MICs across UK who work with clinical teams, academics, businesses and service users (e.g., patients and their families) to support the development and adoption of new medical devices, healthcare technologies and technology-dependent interventions in the NHS. Each of these MICs focuses on a specialist area, such as in-vitro diagnostics, trauma management, community healthcare and surgical, and tailor their services accordingly. NIHR CYP MedTech is the only MIC dedicated to child health and paediatrics, and offers a broad range of support for academics, clinicians and industry who are developing MedTech for children and young people. They organise networking events including an annual conference, enabling attendees to network, see live demonstrations, debate and hear from opinion leaders [Citation43]. They also go beyond helping to develop relationships to support partners in identifying and validating unmet needs, accessing the NHS, gaining input from patients and their families, and undertaking clinical evaluation [Citation44]. As the MICs are embedded within and hosted by the NHS, this access to clinicians and patients can be highly valuable as user involvement in design and verification is a critical success factor for MedTech development [Citation2,Citation15,Citation16,Citation45,Citation46]. NIHR CYP MedTech also offer regulatory and IP guidance, project management, and market-specific knowledge such as the nuances of paediatric MedTech development. Those employed within NIHR CYP MedTech have a range of backgrounds, from nursing and clinical research to academic research and MedTech patenting [Citation47]. This breadth of experience and expertise enables them to offer guidance throughout the journey of paediatric MedTech development, and potentially also fill gaps in knowledge/experience left by collaboration partners. This can be particularly valuable as team experience has been found to improve overall development time by up to 50%—and shorter-time-to-market is something MedTech companies constantly aim for [Citation15,Citation48]. Knowledge of regulatory requirements is similarly important and these set the sector aside from general product development as they provide additional constraints for development, manufacture and marketing [Citation15,Citation16,Citation49,Citation50].
Individuals working across organisational boundaries are often referred to as “boundary spanners” [Citation51]. Boundary spanners act as a relationship catalyst as they possess the ability to work across the partnering organisations, their teams and resources. Within MedTech development, in addition to cross-organisation activities, boundary spanning can also take the form of clinicians bringing patients and their families into the collaboration, likely driven by a trusted relationship between the two. Within university-industry collaborations, boundary spanners have been identified as key actors in overcoming organisational barriers [Citation52]—potentially leveraging social connections to improve other proximities, such as organisational proximity. They are also found to be instrumental in the biomedical context, providing connections to scientific networks and increasing firms’ absorptive capacity—the ability to recognise new information, assimilate it and apply it within a commercial setting [Citation14]. In doing so, they are arguably reducing the cognitive distance between partners. These individuals are commonly in charge of interorganisational collaborations, acting as the lynchpins between the social groups [Citation53,Citation54]. They are particularly important when bridging differences in language and understanding [Citation21]. In industry, this role may lie with a senior executive, partnership manager or business development manager, and within universities it may be the principal investigator (PI), business development manager, PhD student or even a recent graduate working within the partnering company. In MedTech, healthcare professionals from various backgrounds may act as boundary spanners. Additionally, other organisations such as the NIHR MICs and the AHSN Network for example, may offer individuals to support collaboration between industry, universities and healthcare through their established networks. Despite the significant research on boundary spanners in an intra-organisational context, detailed understanding of boundary spanning roles is limited within collaborative innovation. Yet, evidence to date suggests that boundary spanners play key roles in connecting diverse organisations/groups (coupling different structures, operations, organisational routines and professional environments) [Citation51,Citation52,Citation55], acting as entrepreneur and innovator: scanning for ideas and translating knowledge back into the organisation and combining scientific/technical/industry/market/organisation knowledge [Citation51,Citation52,Citation55,Citation56]. Moreover, boundary spanners help to assemble and coordinate project teams, identify and secure buy-in from senior-level champions [Citation52,Citation56] and acknowledge, manage and balance the different time horizons of partners, particularly where small and medium-sized businesses (SMEs) are involved [Citation52].
As a result of the complexity of these roles, multiple accountabilities and often managing without power, boundary spanners may face paradox, ambiguity and tensions [Citation51]. Furthermore, partners’ opposing forces of self-interest and collaboration, managing different forms of organising and personal and professional interests can also present challenges [Citation51]. For example, a particular route may be best for the collaboration in the long-term, but in the short term it may impact one partner negatively. Similarly, an individual may wish to continue to invest in a course of action due to personal responsibility or self-imposed pressure, whilst it may not be in the interest of their parent organisation [Citation32]. Finding the right balance between involvement and separation or dependence and autonomy can be yet another difficulty [Citation55]. As this role is demanding, it is important that partners ensure they select the right candidate with appropriate levels of experience and skill sets. Individuals can also be developed through postgraduate education, secondments, mentoring and job rotation [Citation51], although personal attributes and traits are likely to influence the manner in which a boundary spanner undertakes the role. Thus, careful selection and recruitment is potentially more important than training [Citation51].
The role of champion is also important within collaborative innovation. Champions are individuals who aggressively pursue ideas and make important contributions by persevering and overcoming barriers to enthusiastically promote an idea through organisational stages [Citation57]. In overcoming these barriers it is likely that a Champion will be able to draw collaborators closer together and reduce organisational gaps due to differing knowledge and expertise, working practices, processes, outines and even habits and values. These individuals are often critical to innovation and without them many new innovations would never progress [Citation57]. Who plays the role of champion appears to differ between collaborations. Some suggest that it is the individuals who created the partnership [Citation32,Citation58], whilst others advise that managers with strong networks should take up the position [Citation32], or that a boundary spanner adopts the role [Citation52,Citation56]. Arguably, all three of these positions could be held by a single individual. In any case, volunteer champions are viewed as the most effective, likely because the passion and drive behind a project cannot be consigned [Citation32]. Within MedTech collaborations the champion may reside within any of the partnering organisations—a clinician with an idea that would improve his/her practice, an academic wanting to develop an application for their latest science, or an individual within industry who sees a gap in the market. It could also be someone sitting at the intersection of these networks who sees potential for collaboration, or even a patient’s family or family friend, driven by first-hand experience to find a solution to an unmet need.
Champions are engaged in two basic activities: adopting an innovation during its development, and contributing to the development of that innovation by selling the idea to others and gaining resources [Citation59]. To this effect, they commonly display four behaviours: pursuing innovative ideas; network building; persisting under adversity; and taking responsibility for the idea [Citation57]. Champions are often independent in their mission; yet, they bring together teams and actively bridge the innovation subsystems to the larger organisation and external partners [Citation57]. These networks provide the champion with the vital resources and expertise to translate the idea into a successful innovation thus fulfilling the role of the champion in driving the innovation into a tangible and successful product [Citation60,Citation61]. Albeit enthusiastic to the cause, champions must maintain rapport with critical individuals (particularly senior managers) and also be open to, and encourage, contributions from others—by withholding total responsibility they may discourage colleagues from engaging and contributing [Citation57].
This ability to engage others is essential to collaboration success, as it takes a whole team, working across all partnering organisations, to drive an innovation forwards. Whether a team works together effectively is influenced considerably by several relational drivers.
4. Core relational drivers
Boundary spanners, champions and intermediaries develop relationships within and across partnering organisations. At the very core of these relationships lie a variety of relational drivers, including trust, commitment, shared vision/goals, communication and prior relations between partners [Citation36,Citation62,Citation63]. Not only do relational drivers influence the relationship, but they have also been found to influence collaborative outcomes [Citation29,Citation31,Citation34,Citation64]. Furthermore, these relational drivers help to develop social proximity, which can connect partnering organisations whilst other forms of proximity are strengthened, such as shared processes, values and mutual understanding [Citation20].
Trust between collaborative partners is recognised as key to collaboration success [Citation29] and is one of the main measures cited for strengthening collaborations between hospitals and external partners [Citation2]. It is critical in building and maintaining organisational collaborations as it reduces both orientation and transaction related barriers in what can be an uncertain and risky venture [Citation9,Citation36,Citation65]. Where trust exists, partners are more likely to respect one another and empathise with each other’s viewpoints, which can help to manage challenges once collaborations become established [Citation66,Citation67]. It can be built in a variety of ways, either through a “third party guarantor” (e.g., a known intermediary or contact who can vouch for another partner’s credibility [Citation68,Citation69]) or via continued interaction—starting with low risk transactions and gradually progressing to more major transactions over time as partners prove their trustworthiness [Citation37]. As trust is largely developed through face-to-face dialogue [Citation15], the process may take longer or require additional effort in the wake of the COVID-19 pandemic when interactions have largely become remote. Furthermore, where partners are committed and trusting they are sometimes willing to endure periods where they receive fewer outcomes. Collaborations may not always deliver equal results for partners in the short term, but the longer-term goals of each partner should always be considered. Where there is greater uncertainty, e.g., in the market or wider economy, trust becomes particularly important [Citation34]. Where trust is lacking partners can often hold back information or take unfair advantage of each other given the opportunity, meaning a collaboration will rarely produce all the possible mutual benefits [Citation12].
Commitment is often twinned with trust, and is seen as central to success in interorganisational collaborations as it emphasises a desire to maintain the relationship and its evolution [Citation29,Citation34,Citation36,Citation64]. Committed partners are more likely to resist attractive short-term alternatives and balance short-term problems against long-term plans and benefits, understanding the need to work through any issues [Citation12,Citation66,Citation70,Citation71]. The development of commitment within a collaboration involves signalling between partners and the interpretation and reaction to those signals [Citation12]. Shared decision-making is often used to signify a commitment to the relationship [Citation72]; yet, other signals could have similar results such as financial investment or openness, e.g., sharing commercially sensitive information. Within hospitals, the ability to share information is much more complex as patient data is highly protected. In this case, it may be a clinician’s resolve to provide data that actually highlights their commitment to the project more so than the willingness to share the data. Nonetheless, such means of signalling and a willingness to be open is directly connected with communication.
Communication is a consistent predictor of success across all phases of a collaboration [Citation31]. Communication enhances the success of collaborations, as it can help individuals to form shared meanings and relationships and enables the exchange of information, ideas and concepts [Citation29]. It can also influence trust [Citation71]. Due to the many differences between partnering organisations, communication can be challenging [Citation73]. For example, in terms of exchanging information, due to highly complex administrative processes within hospitals, the information needed for innovation is not readily available across hospitals and to external stakeholders [Citation2]. As a result, communication [information] gaps are cited as one of the main obstacles to healthcare innovation. Having access to the right people and a means to accelerate processes is often challenging yet can be helpful in this endeavour. Nonetheless, communication is not just about sharing practical information, it is also about the language used, such as specialist terminology and jargon or understanding the context of communications. Boundary spanners and other intermediaries, such as Medilink and the NIHR MICs referenced earlier, can help to improve these aspects of communication between partners by “translating” [Citation21]. Investing in cross-cultural training for employees can be another means of improving communication—for example, enabling partners to spend a few hours or a day in the workplace of the clinical/industry/academic partner, enabling them to better understand the context each partner is operating within. Alternatively, encouraging ongoing engagement by complementing frequent scheduled meetings with general accessibility for spontaneous exchanges [Citation12,Citation31]. As repeated contact and communication strengthens personal relationships (particularly informal contact), this can lead to mutual understanding, greater levels of trust and some of the barriers being overcome [Citation64,Citation74]. In this sense, some relational drivers catalyse the development of others.
Developing shared goals is another relational driver and involves partners harmonising their differing expectations [Citation73]. In doing so, they are able to reduce the potential for misunderstandings and conflict and set manageable project boundaries [Citation36,Citation75]. In order to do this, partners need to have a good understanding of the interests and motivations of all partners, highlighting the need for effective communication, transparency and mutual trust in order for partners to be open and honest about their aims and objectives [Citation9,Citation36]. A recent study looking into the lessons learned during the set-up and management of medical device design and manufacture during the COVID-19 ventilator emergency highlights the importance of a single, easily understood and compelling objective [Citation15]. Despite the extremely challenging backdrop, lack of face-to-face communications, barriers to information sharing and an inability to immerse themselves in each others’ cultures, the collaborative teams were able to rapidly and successfully develop new medical devices [Citation15]. The study found that where there is a sufficient and focussed motivation, employees can overcome potentially constraining factors, stimulated by the strong common goal [Citation15]. Obviously, the national imperative made it far easier to override the more common commercial selfish behaviours, but the situation goes to show what can be achieved where partners are fully committed to achieving a shared goal.
In order to foster the various relational drivers those working at the interface of a collaboration must display a range of behaviours. This is important as an individual’s relationship skills are generally difficult to observe directly; yet, the resulting behaviour (what they do) is more observable, and thus act as signals to other partners.
5. Behavioural factors
“Relational behaviour” refers to the actions taken to promote, create and shape positive relationships between collaborators [Citation76,Citation77]. These behaviours are a display of individuals’ relational capabilities, including personal qualities, communication skills, behavioural skills (e.g., team working) and broader management skills. To achieve this, these individuals need certain relational capabilities such as being frank, honest, available, adaptable, likeable, fair, proactive, tolerant, compassionate, benevolent, [Citation77–82] and “ecocentric”—someone who cares about the needs of a collaborative ecosystem, not solely one aspect [Citation52].
Additionally, there is also need for team members to be open to engaging with areas beyond their traditional “work boundaries.” Professional identities (i.e., what individuals see as their role in the work environment) and work boundaries (boundaries used to gain legitimacy and distinguish between experts from different disciplines or from lay people) influence how open individuals are to input from people outside of their organisation [Citation83,Citation84]. A study examining NASA R&D professionals’ response to Open Innovation found that those who were less open saw themselves as problem solvers, whereas those who saw themselves as an integrator of information (a “solution seeker”) were more welcoming of input from outside of their organisation. Whether partners view themselves as independent problem solvers or are open to contributions from those beyond their “work boundaries” (e.g., industry, academia or healthcare) will likely influence the collaborative relationship and its outcomes. Ensuring that individuals working across the organisational boundaries are open in this manner would therefore appear important.
6. Individual characteristics
The characteristics and traits of individuals can also influence collaborative relationships. Individuals’ managing collaborations should be adept at building sustainable relationships (diplomatic, resolving conflict and building trust), managing through influencing and negotiation, managing complexities and interdependencies and managing different roles, accountabilities and motivations [Citation55]. Importantly, technical knowledge specific to the collaboration is second to these personal skills, suggesting that individuals’ characteristics are more important than understanding the technical aspects for these roles [Citation85]. For those based in industry, research suggests that these individuals should also be a leader who is able to lobby ideas at management and operational levels and display an ability to manage interdisciplinarian and heterogeneous teams [Citation52]. They should also be able to think laterally and vertically to enable creative thinking—necessary for combining scientific/technical knowledge with knowledge of the industry, the market, the university structure and decision-making processes. In MedTech developments, this characteristic is likely even more important considering the additional dimensions related to user centrality, clinical adoption and regulatory frameworks. Furthermore, they require “cognitive acumen” to compensate for short-comings in their experience (through intensive learning or asking advice) as the dual-environment work experience needed would rarely be found in one person [Citation52]. Whether these roles are replicated in university and clinical partners is yet to be established. Things could potentially differ on the need for cognitive acumen for example, as many clinicians have teaching and/or research roles linked with a university, providing them with some dual environment work experience. Similarly, in the US, it is common for scientists to move between academic and commercial pursuits [Citation14], again providing them with dual environment work experience. Nonetheless, the ability to form effective relationships does not rest solely on the shoulders of an individual. It is how key individuals come together and the blend of their various behaviours and characteristics.
7. Team level factors
The composition of a team (configuration of member attributes) can have a powerful influence on team processes and outcomes [Citation86]. Team composition can be considered on two planes. There are surface level composition variables, which refer to overt demographic characteristics, such as age, race, educational level and organisational tenure [Citation86]. Deep level composition variables refer to underlying psychological characteristics such as personality factors, values and attitudes [Citation86]. Interestingly, surface level variables have failed to demonstrate a relationship between demographic heterogeneity and team performance [Citation86]. This appears to support the notion of proximities, i.e., that homogeneity or similarity between partners is perhaps more conducive to collaboration performance, rather than heterogeneity [Citation17]. Similarly, the homogenous demographics of group members (at least at the surface level) are likely to create less conflict, fewer differences in opinion, freer communication and more interaction [Citation87]. However, heterogeneous groups are more likely to be productive where complex tasks require creative efforts [Citation87], which is likely the case within collaborative innovation. Thus, there is likely a tension, or trade off, between the need for homogeneity to drive proximity and the value of heterogeneity to drive innovation. In the MedTech sector where teams have increasingly diverse technical specialisms we are yet to identify whether individuals are similar in core characteristics. Perhaps deep level composition variables provide the key factor that enables the interorganisational team to function, or perhaps shared goals are sufficient. Nonetheless, Trait Theory suggests that generally teams should be composed of conscientious individuals with high agreeableness, “general mental ability” and openness to experience as these traits are positively related to team performance [Citation86].
Though similarity in certain characteristics and traits appear favourable, diversity in individuals’ motivation types may be beneficial for innovation. One study suggests that a combination of those who are driven to explore and seek knowledge are complemented by those who want to apply knowledge and derive external recognition or reward—pushing the collective efforts towards successful completion [Citation88]. The stereotypes of academics and industry professionals could arguably fit into the two roles respectively—academics seeking new understanding whilst industry seeks commercial gain. Though this has not been explored within the MedTech context it is plausible that clinicians add a third valuable motivation—a desire to help patients. Thus, whereas the stereotypical academic may wish to explore, and industry partners wish to reap rewards, the clinician’s role is perhaps ensuring that the end product meets users’ needs and delivers benefits to patients. In situations such as this where partners have diverse motivation types, it will likely be even more important to ensure they develop shared goals to unify their interests.
Though team composition is thus a core component for success, this is not to suggest that the team should be static. Beyond a few core individuals, other employees should be brought into the collaboration only when appropriate to the project [Citation89]. This results in flexible and effective use of resources with a variety of perspectives, knowledge and experience being applied to the collaboration at key project milestones. Leaders should mobilise different, often new participants across phases and encourage others to involve new participants too [Citation89]. Having some stable roles to facilitate and coordinate is important however [Citation89]. These individuals are required to recruit and instruct employees as the process of innovation unfolds and ensure that those recruited fit with the demands of that particular phase [Citation89].
Beyond mobilising different team members, there is also a need for coordination and leadership.
Research has shown that team coordination enhances team performance and innovation [Citation88]. Coordination is broadly understood as the linking, meshing, synchronisation or alignment of actions [Citation90,Citation91]. A lack of coordination amongst participants is one of the main problems in unsuccessful projects [Citation63]. In strategic collaborations, this is often due to the excessive effort required to coordinate and integrate two independent organisations [Citation92]. Coordination failures can take the form of omissions of crucial activities, misallocation of resources and incompatibility of activities intended to be complementary, leading to uncertainty over the teams’ tasks and division of labour [Citation93]. Co-ordination failures can cause inefficiencies and delays [Citation94], and may prevent teams and partners from attaining specific collaborative goals [Citation95]. They can also lead team members to doubt the feasibility of the collaboration, which in turn, may work to undermine their commitment and even trust levels. On the other hand, effective coordination can enable partners to reconcile differences in areas such as decision making, objectives, participants and established processes [Citation89]. For example, clearly defined objectives in the formal contract of the collaboration can achieve immediate strategic alignment between partners or offer contingency plans for coping with environmental volatility [Citation66].
Interpersonal relationships should be central to effective team co-ordination within MedTech collaborations. Although formal co-ordination mechanisms (e.g., contracts, plans) will be used in most collaborations, many collaborations function through informal co-ordination as well, or what is termed “relational co-ordination.” Relational co-ordination can be defined as the management of task interdependencies within the context of relationships with other group members [Citation96]. While it requires further research, relational co-ordination likely constitutes an essential process within MedTech collaborations. For example, relational co-ordination should enhance problem-solving, mutual respect, shared goals and shared knowledge among team members. Indeed, relational co-ordination provides channels for information exchange among members [Citation97], which can increase the opportunities for knowledge transfer—formal systems are often not appropriate for sharing complex knowledge [Citation98]. While formal systems of co-ordination, such as planning and standards, allow the sharing of easily transferrable knowledge, relational co-ordination is more suitable for intense sharing of complex knowledge, which MedTech collaboration often involves.
In addition to the different types of coordination (formal and relational), the amount of coordination needed may also change during a collaboration. For example, in the context of innovation, research suggests that coordination should be achieved without constraining innovation with too much structure [Citation89,Citation99], as this may impact upon innovation outcomes. In this setting, formal coordination becomes more important as the innovation process draws closer to the commercialisation phase [Citation88]. In contrast, during the earlier phase of generating ideas, looser coordination is more effective to give innovators the freedom to generate ideas at their own discretion [Citation88]. However, when discussing interorganisational collaboration, it may be that the need for formal coordination is greater in the earlier stages, for example, when establishing trust and boundaries (via agreements over data sharing, IP and revenue share following commercialisation). In light of this, it may be that within the context of collaborative innovation there are two separate yet interlinked planes requiring different approaches to coordination—one regarding the collaboration, and one regarding the innovation process. In consideration of this, flexible and adaptable leadership is recommended—using different approaches for the different facets and stages of the collaboration.
Alongside coordination, rotating the leadership role between partners may also lead to much better collaboration performance than using a dominating or consensus approach to decision-making [Citation89,Citation100]. Leaders influence innovation—they decide which avenues to pursue, how to allocate resources and impart their knowledge to assist innovation processes [Citation101]. “Rotating leadership” involves three components—alternating decision control (planned and unplanned) between partners—this facilitates access to their complementary capabilities; zig-zagging objectives—by enabling partners to pursue their own objectives when they are leading a phase, it continually provides new perspectives and leads to broad and deep search trajectories; and mobilising diverse participants over time [Citation89]. Within MedTech development, it may be that one partner leads during different phases of the project, for example, the clinician leads during the elicitation of clinical requirements and end-user needs, and later clinical evaluation; the academic partner leads during the conceptualisation and development phase; and the industry partner takes the lead during the commercialisation phase. Input from all partners during each phase is still required, but leadership and decision-making may lean towards a certain partner. Within the COVID ventilator emergency study, a similar approach is described, devolving leadership and empowering employees [Citation15]. Here, decision making was not top-down, but placed at the point of “greatest knowledge” [Citation15]. Though leadership is essential for providing direction, other controls are also required to ensure partners progress in the same direction.
Using formal and relational controls can help to steer partners away from the potentially ill effects of their divergent interests or non-alignment across collaborative activities [Citation78]. Formal controls can include setting joint targets, operational reviews, information systems, evaluating achievements, feedback mechanisms and follow-up meetings [Citation78,Citation102]. However, partners will not achieve effective control by purely implementing this type of control mechanism [Citation103]. Additionally, formal control measures can be inflexible and thus unable to cope with the changing environment and needs of partners [Citation102]. Furthermore, where there is excessive use of formal control measures this can foster an atmosphere of distrust between partners and increase the likelihood of conflict [Citation102,Citation104]. Relational controls are therefore also needed, referring to the extent to which exchanges are governed by social relations, informal structures, and self-enforcement [Citation78,Citation102,Citation105]. Trust and relational norms (e.g., flexibility, solidarity and information exchange) are the two main relational control mechanisms [Citation78,Citation106,Citation107]. Although a foundational level of trust and relational norms may exist based on reputation or past experience, relational controls are generally built step-by-step during repeated exchanges [Citation78]. This is unlike formal mechanisms, which are more actively created—through selection, design or implementation [Citation78]. Relational controls are said to be particularly valuable in collaborations that have narrow scope (where there are fewer overlapping activities), though formal controls can be more beneficial for broader and more complex collaborations [Citation78].
8. Contextual factors
The circumstances and environment in which a collaboration builds and operates can influence the relationship and also moderate the effects of relational factors on collaboration performance [Citation34]. Organisational culture, processes, atmosphere and availability of resources all play a role in facilitating and shaping interorganisational relationships [Citation37,Citation108,Citation109]. For example, SMEs often have greater reliance on personal networks and may be more opposed to longer academic timescales [Citation52], meaning that partners’ behaviours need to acknowledge and support this, perhaps by trying to speed up processes or offering more frequent updates to allay fears of delays/lack of progress. At the level of international joint ventures, the structure/organisational architecture (i.e., equity ownership and management control) can also shape partner relations [Citation66,Citation102,Citation104,Citation107,Citation110–112].
Additionally, the discipline or sector can influence relationships. For instance, some may require different types and frequency of interaction between collaborators [Citation108]. Within MedTech development, it may be that academics or industry partners need to work around the clinical partner’s commitments as patient care may be prioritised over medtech collaboration and development activities. Additionally, other sector-related matters may influence the relationship, such as the considerable regulation within the MedTech sector. In paediatric MedTech development, there are additional challenges to address as technology development has to be versatile to support changes in anatomy and physiology through growth and development, paediatric-specific regulations, child safeguarding and a shift from parental use (with their children) to more independent use later by adolescents (Dimitri et al, 2021). Each of these considerations not only affect the technology being developed, but also how the relationship between collaborators must adapt and accommodate these sector-specific requirements, for example, greater communication to share knowledge of regulatory requirements or user needs. Though the environment in which MedTech development takes place may be challenging, where the right individuals work together effectively they are more likely to find a way to succeed.
9. Conclusion
In the MedTech sector where collaborative innovation is complex due to a greater number of partners and a range of disciplines and professions involved, finding ways to encourage effective working across organisations can be challenging. Nonetheless, there are many examples of successful collaborations developing a range of innovative new products, such as non-invasive customised ventilation masks for children [Citation113]; neonatal heartrate monitors [Citation114]; and novel diagnostic equipment for early detection of cancers [Citation115]. Drawing upon literature within the social sciences provides an opportunity to better understand the dynamics of this type of interorganisational working, and importantly, the elements that can be actively facilitated to enhance success.
Studies suggest that collaborations are driven by interpersonal relationships and so it is argued that investing in these relationships is key to success. Relationships are influenced by a range of factors across five levels: Relational drivers; Behavioural factors; Individuals’ characteristics; Team level factors; and Contextual factors. Within each of these dimensions certain elements can be leveraged, fostered or mobilised to enhance collaborative working.
More specifically, fostering the relational drivers of trust, commitment, communication and shared goals can help to strengthen relationships. These are encouraged by partners being open, honest, and signalling their commitment to the collaboration. Finding the right balance between formal and relational controls (e.g., social norms) can also help to shepherd partners in the right direction—enabling adaptability, reducing costs and promoting trust.
Certain individuals can play a particularly important role, such as employing “boundary spanners” or external intermediaries to broker relationships, open up communications and balance partners’ needs. In the last decade, the NHS has invested in organisational development to support this through the creation of the NIHR MICs [Citation39], NHSX [Citation116] and the Academic Health Science Network [Citation41]. Equally, empowering a “champion” capable of bringing the necessary parties together to support MedTech development, can see the collaboration enthusiastically promoted, adversity overcome and the project propelled forward to completion. Perhaps more so than training and development, selecting individuals with the right traits and characteristics appears necessary for them to effectively bridge the diverse cultures and processes.
The wider composition of the team also needs careful consideration, for example, balancing heterogeneity (to foster idea generation) with the need for team cohesion. Aiming for team members who are open to working with others from outside of their traditional “work boundaries”—and able to span the organisational boundaries—appears conducive for collaborative innovation. Though the team should have a few core individuals, others should only be mobilised when appropriate as the project unfolds. Coordination of the team is also important—a mix of formal and informal coordination that enables freedom for idea generation whilst also driving the project towards commercialisation. Decision-making is perhaps best rotated between collaborative partners during the project, enabling depth and breadth of involvement from partners and their varied resources.
10. Future research
Though the extant management literature provides considerable understanding of interorganisational collaborations there are three identifiable gaps. First, few scholars consider how collaboration differs across sectors [Citation3,Citation78] and so empirical evidence is needed to understand the nuances within the MedTech sector. Second, though relationships are seen as vital, there is limited understanding of the individuals that build these relationships. Though we have a general appreciation of those working at the interface between partnering organisations, such as boundary spanners, there is limited research into their characteristics, or the impact they have on collaborative innovation, such as organisational processes and outcomes. For example, boundary spanners are central to interorganisational collaborations, thus future research should seek to understand the individual traits enabling such individuals to perform this role. Third, the overwhelming focus to date has been on dyadic relationships between two partners leaving many questions about how things differ where there are more than two partners involved. As collaborations with more than two partners are said to be more challenging, future research should explore the various dimensions within tripartite collaborations particularly those relating to collaborations between universities, industry and the health sector to drive MedTech development.
Acknowledgements
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Perkmann M, Salandra R, Tartari V, et al. Academic engagement: a review of the literature 2011-2019. Res Policy. 2021;50(1):104114.
- Dias C, Escoval A. The open nature of innovation in the hospital sector: the role of external collaboration networks. Heal Policy Technol. 2012;1(4):181–186.
- BEIS D for BE and IS. Science and Innovation Audits: Wave 2 [Internet]. University of York; [cited 2017]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/647784/BEIS_Document_Template_SIA.W2_Summary_Final.pdf.
- Savory C, Fortune J. From translational research to open technology innovation systems. J Health Organ Manag. 2015;29(05):200–220.
- Vick TE, Robertson M. A systematic literature review of UK university- industry collaboration for knowledge transfer: a future research agenda. Sci Public Policy. 2018;45(4):579–590.
- Hewitt-Dundas N, Gkypali A, Roper S. Does learning from prior collaboration help firms to overcome the ‘two-worlds’ paradox in university-business collaboration? Res Policy. 2019;48(5):1310–1322.
- Tartari V, Salter A, D’Este P. Crossing the rubicon: exploring the factors that shape academics’ perceptions of the barriers to working with industry. Cambridge J Econ. 2012;36:655–677.
- Valentin E. University-Industry cooperation: a framework of benefits and obstacles. Ind High Educ. 2000;14(3):165–172.
- Bruneel J, D’Este P, Salter A. Investigating the factors that diminish the barriers to university-industry collaboration. Res Policy. 2010;39(7):858–868.
- Santoro MD. Success breeds success: the linkage between relationship intensity and tangible outcomes in industry-university collaborative ventures. J High Technol Manag Res. 2000;11(2):255–273.
- Villani E, Rasmussen E, Grimaldi R. How intermediary organizations facilitate university–industry technology transfer: a proximity approach. Technol Forecast Soc Change. 2017;114:86–102.
- Cullen JB, Johnson JL, Sakano T. Success through commitment and trust: the soft side of strategic alliance management. J World Bus. 2000;35(3):223–240.
- Galán-Muros V, van der Sijde P, Groenewegen P, et al. Nurture over nature: how do european universities support their collaboration with business? J Technol Transf. 2017;42(1):184–205.
- Swan J, Goussevskaia A, Newell S, et al. Modes of organizing biomedical innovation in the UK and US and the role of integrative and relational capabilities. Res Policy. 2007;36(4):529–547.
- Von Behr C-M, Semple GA, Minshall T. Rapid setup and management of medical device design and manufacturing consortia: experiences from the COVID-19 crisis in the UK. R&D Mang 2022;52(2):220–234.
- Kirkire MS, Rane SB. Evaluation of success factors for medical device development using grey DEMATEL approach. J Model Manag. 2017;12(2):204–223.
- Boschma RA. Proximity and innovation: a critical assessment. Reg Stud. 2005;39(1):61–74.
- Johnston A, Huggins R. Networks, SMEs, and the university: the process of collaboration and open innovation. Cheltenham: Edward Elgar Publishing; 2021.
- Johnston A. Open innovation in science: assessing the formation and function of SME-University collaborations through the proximity matrix. Ind Innov. 2022;29(2):310–332.
- Kuttim M. The role of spatial and non-spatial forms of proximity in knowledge transfer: a case of technical university. EJIM. 2016;19(4):468–491.
- Steinmo M, Rasmussen E. The interplay of cognitive and relational social Capital dimensions in university-industry collaboration: overcoming the experience barrier. Res Policy. 2018;47(10):1964–1974.
- Gossling T, Knoben J. Proximity and duration in temporary organisations. IJSBA. 2011;2(3):207–220.
- University of Nottingham, Nottingham University Hospitals NHS Trust. Centre for Healthcare Technologies [Internet]. Website. [cited 2022 Mar 16]. Available from: http://www.healthcaretechnologies.ac.uk/cht-homepage.aspx.
- University of Manchester, Manchester Science Partnerships, Manchester University NHS Foundation Trust, Health Innovation Manchester. Christobel Pankhurst Institute for Health Technology and Innovation [Internet]. Website. [cited 2022 Mar 16]. Available from: https://www.manchester.ac.uk/discover/news/launch-of-multimillion-pound-institute-for-health-technology-research-and-innovation-in-manchester/.
- Maskell P, Bathelt H, Malmberg A. Building global knowledge pipelines: the role of temporary clusters. Eur Plan Stud. 2006;14(8):997–1013.
- Balland P, Boschma R, Frenken K. Papers in evolutionary economic geography proximity and innovation: from statics to dynamics. J Reg Stud. 2015;49(6):907–920.
- Foss NJ, Pedersen T. Foss and pedersen. Strateg Manag J. 2016;37(13):22–34.
- Davey T, Meerman A, Galan Muros V, et al. The State of University-Business Cooperation in Europe [Internet]. Luxembourg: Publications Office of the European Union; 2018.
- Mora-Valentin EM, Montoro-Sanchez A, Guerras-Martin LA. Determining factors in the success of R&D cooperative agreements between firms and research organizations. Res Policy. 2004;33(1):17–40.
- Rampersad G, Quester P, Troshani I. Managing innovation networks: exploratory evidence from ICT, biotechnology and nanotechnology networks. Ind Mark Manag. 2010;39(5):793–805.
- Plewa C, Korff N, Johnson C, et al. University-industry linkage evolution: an empirical investigation of relational success factors. J Eng Technol Manag. 2013;30(1):21–44.
- Adobor H. The role of personal relationships in inter-firm alliances: benefits, dysfunctions, and some suggestions. Bus Horiz. 2006;49(6):473–486.
- Dooley L, Gubbins C. Inter-organisational knowledge networks: synthesising dialectic tensions of university-industry knowledge discovery. J Knowl Manag. 2019;23(3):2113–2134.
- Palmatier R, Dant R, Grewal D, et al. A comparative longitudinal analysis of theoretical perspectives of interorganizational relationship performance. J Mark. 2007;71(4):172–194.
- Owen-Smith J, Riccaboni M, Pammolli F, et al. A comparison of U.S. and european university-industry relations in the life sciences. Manag Sci. 2002;48(1):24–43.
- Galan-Muros V, Plewa C. What drives and inhibits university-business cooperation in Europe? A comprehensive assessment. R&D Manag. 2016;46(2):369–382.
- Zineldin M, Vasicheva V. Strategic alliances, total relationship management (TRM) and 5 QS - Why most of the marriages and strategic alliances are not sustainable? Nang Yan Bus J. 2014;2(1):140–150.
- Wittmann CM, Hunt SD, Arnett DB. Explaining alliance success: competences, resources, relational factors, and resource-advantage theory. Ind Mark Manag. 2009;38(7):743–756.
- NIHR. MedTech and In-Vitro Diagnostics Co-Operatives (MICs) [Internet]. [cited 2022 Mar 14]. Available from: https://www.nihr.ac.uk/partners-and-industry/industry/access-to-expertise/medtech.htm.
- Medilink UK. Medilink National Health Technology Business Support Network [Internet]. Website. [cited 2022 Mar 14]. Available from: https://www.medilink.co.uk.
- The AHSN Network. Academic Health Science Networks [Internet]. [cited 2022 Mar 4]. Available from: https://www.ahsnnetwork.com.
- Medipex. Medipex Healthcare Innovation hub [Internet]. [cited 2022 Mar 14]. Available from: http://www.medipex.co.uk.
- NIHR Children and Young People MedTech Co-Operative. Child Health Technology Conference – CHT 2022. [Internet]. [cited 2022 Jan 31]. Available from: https://cypmedtech.nihr.ac.uk/child-health-technology/.
- NIHR Children and Young People MedTech Co-Operative. NIHR CYP MedTech Support and Services [Internet]. [cited 2022. Jan 31]. Available from: https://cypmedtech.nihr.ac.uk/support/.
- Brown A, Dixon D, Eatock J, et al. A survey of success factors in new product development in the medical devices industry. 2008 IEEE International Engineering Management Conference. 2008. p. 1–5.
- Eatock J, Dixon D, Young T. An exploratory survey of current practice in the medical device industry. J Manuf Technol Manag. 2009;20(2):218–234.
- NIHR Children and Young People MedTech Co-Operative. Meet the Team [Internet]. [cited 2022 Jan 31]. Available from: https://cypmedtech.nihr.ac.uk/about/.
- Lucke LE, Mickelson A, Anderson D. Proving experience speeds medical device time to market. Annu Int Conf IEEE Eng Med Biol Soc. 2009;2009:7057–7060.
- Pietzsch JB, Shluzas LA, Paté-Cornell ME, et al. Stage-gate process for the development of medical devices. J Med Device. 2009;3(2):021004.
- Medina LA, Kremer GEO, Wysk RA. Supporting medical device development: a standard product design process model. J Eng Des. 2013;24(2):83–119.
- Williams P. The life and times of the boundary spanner. J Integr Care. 2011;19(3):26–33.
- Albats E, Bogers M, Podmetina D. Companies’ human Capital for university partnerships: a micro-foundational perspective. Technol Forecast Soc Change. 2020;157:120085.
- Ebers M. The formation of inter- organizational networks. Oxford: Oxford University Press; 1997.
- Zhang C, Viswanathan S, Henke JW. The boundary spanning capabilities of purchasing agents in buyer-supplier trust development. J Oper Manag. 2011;29(4):318–328.
- Williams P. The competent boundary spanner. Public Adm. 2002;80(1):103–124.
- Chau VS, Gilman M, Serbanica C. Aligning university–industry interactions: the role of boundary spanning in intellectual Capital transfer. Technol Forecast Soc Change. 2017;1123:199–209.
- Walter A, Parboteeah KP, Riesenhuber F, et al. Championship behaviors and innovations success: an empirical investigation of university spin-offs. J Prod Innov Manag. 2011;28(4):586–598.
- Kanter RM. Collaborative advantage: the art of alliances. Harv Bus Rev. 1994;72(4):96–108.
- Markham SK, Green SG, Basu R. Champions and antagonists: relationships with R&D project characteristics and management. J Eng Tech Manage. 1991;8(3-4):217–242.
- Burgelman RA. A process model of internal corporate venturing in the diversified major firm. Quarterly. 1983;28:223–244.
- Tsai W, Ghoshal S. Social Capital and value creation: the role of intrafirm networks [internet]. Acad Manag J. 1998;41(4):464–476.
- Sharma A, Garg A. Knowledge transfer: an empirical study on factors yielding the effectiveness of the academia–industry interface (with special reference to moradabad city). Manag Econ Res J [Internet]. 2019;5:1.
- Barbolla AMB, Corredera JRC. Critical factors for success in university-industry research projects. Technol Anal Strateg Manag. 2009;21(5):599–616.
- Lauvås T, Steinmo M. The role of proximity dimensions and mutual commitment in shaping the performance of university-industry research centres. Innovation. 2021;23(2):182–208.
- Plewa C, Quester P. Satisfaction with university-industry relationships: the impact of commitment, trust and championship. Int J Technol Transfer Commercialisation. 2006;5:79–101.
- Owens M, Ramsey E, Loane S. Resolving post-formation challenges in shared IJVs: the impact of shared IJV structure on inter-partner relationships. Int Bus Rev. 2018;27(3):584–593.
- Krishnan R, Martin X, Noorderhaven NG. When does trust matter to alliance performance? [internet.]. AMJ. 2006;49(5):894–917.
- Johnston A, Huggins R. Partner selection and university-industry linkages: assessing small firms’ initial perceptions of the credibility of their partners. Technovation. 2018;78:15–26.
- Bachmann R, Inkpen AC. Understanding institutional-based trust building processes in inter-organizational relationships. Organ Stud. 2011;32(2):281–301.
- Nakos G, Brouthers KD. International alliance commitment and performance of small and medium-size enterprises: the mediating role of process control. J Int Manag. 2008;14(2):124–137.
- Morgan RM, Hunt SD. The Commitment-Trust theory of relationship marketing. J Mark. 1994;58(3):20–38.
- Saxton T. The effects of partner and relationship characteristics on alliance outcomes. Acad Manag J. 1997;40(2):443–461.
- Galán-Muros V, Plewa C. What drives and inhibits university-business cooperation in Europe? A comprehensive assessement. R&D Manag. 2015;46(2).
- Muscio A, Pozzali A. The effects of cognitive distance in university-industry collaborations: some evidence from italian universities. J Technol Transf. 2013;38(4):486–508.
- Lee K-J. From interpersonal networks to inter-organizational alliances for university-industry collaborations in Japan: the case of the Tokyo institute of technology. R&D Manag. 2011;41(2):190–201.
- Lusch RF, Brown JR. Interdependency, contracting, and relational behavior in marketing channels. J Mark. 1996;60(4):19–38.
- Walter A. Relationship promoters driving forces for successful customer relationships. Indus Market Manag. 1999;28(5):537–551.
- Dekker H, Donada C, Mothe C, et al. Boundary spanner relational behavior and inter-organizational control in supply chain relationships. Ind Mark Manag. 2019;77:143–154.
- Doney PM, Cannon JP. An examination of the nature of trust in Buyer-Seller relationships. J Mark. 1997;61(2):35–51.
- Jap SD. Pie-Expansion efforts: collaboration processes in Buyer-Supplier relationships. J Market Res. 1999;36(4):461.
- Lussier B, Grégoire Y, Vachon MA. The role of humor usage on creativity, trust and performance in business relationships: an analysis of the salesperson-customer dyad. Ind Mark Manag. 2017;65:168–181.
- Tangpong C, Hung KT, Ro YK. The interaction effect of relational norms and agent cooperativeness on opportunism in buyer-supplier relationships. J Oper Manag. 2010;28(5):398–414.
- Lifshitz-Assaf H. Dismantling knowledge boundaries at NASA: the critical role of professional identity in open innovation. Adm Sci Q. 2018;63(4):746–782.
- Carlile PR. Transferring, translating, and transforming: an integrative framework for managing knowledge across boundaries. Organ Sci. 2004;15(5):555–568.
- Wilson A, Charleton K. Making partnerships work: a practical guide for the public, private, voluntary and community sectors. York: YPS for the Joseph Rowntree Foundation; 1997.
- Bell ST. Deep-level composition variables as predictors of team performance: a meta-analysis. J Appl Psychol. 2007;92(3):595–615.
- McKenna E. Business psychology and organizational behaviour. 5th ed. Hove: Psychology Press; 2012.
- Emre Yildiz H, Murtic A, Klofsten M, et al. Individual and contextual determinants of innovation performance: a micro-foundations perspective. Technovation. 2021;99:102130.
- Davis JP, Eisenhardt KM. Rotating leadership and collaborative innovation: recombination processes in symbiotic relationships. Adm Sci Q. 2011;56(2):159–201.
- Okhuysen GA, Bechky BA. Coordination in organizations: an integrative perspective. Annals. 2009;3(1):463–502.
- Aiken M, Hage J. The organic organisation and innovation. Sociology. 1971;5(1):63–82.
- Park SH, Ungson GR. Interfirm rivalry and managerial complexity: a conceptual framework of alliance failure. Organ Sci. 2001;12(1):37–53.
- Gulati R, Wohlgezogen F, Zhelyazkov P. The two facets of collaboration: cooperation and coordination in strategic alliances. Annals. 2012;6(1):531–583.
- Gulati R, Lawrence PR, Puranam P. Adaptation in vertical relationships: beyond incentive conflict. Strat Manag J. 2005;26(5):415–440.
- Mohr J, Spekman R. Characteristics of partnership success: partnership attributes, communication behavior, and conflict resolution techniques. Manag J. 1994;15(2):135–152.
- Gittel JH. Paradox of coordination and control. Calif Manage Rev. 2000;42(3):471.
- Homans GC. Social behaviour: its elementary forms. New York: Harcourt Brace; 1961.
- Grant RM. Toward a knowledge-based theory of the firm. Strat Manag J. 1996;17(S2):109–122.
- Gonzalez RVD. Innovative performance of project teams: the role of organizational structure and knowledge-based dynamic capability. J Knowl Manag. 2022;26(5):1164–1186.
- Wang C, Cen Y, Sun R, et al. Optimal distribution of profit and leadership for a sustainable collaborative R&D projects. J Clean Prod. 2021;313.
- Cortes AF, Herrmann P. Strategic leadership of innovation: a framework for future research. Br Acad Manag. 2020;23(2):224–243.
- Fryxell G, Dooley R, Vryza M. After the ink dries: the interaction of trust and control in US-based international joint ventures. J Manag Stud. 2002;39(6):865–886.
- Das TK, Teng B-S. Between trust and control: developing confidence in partner cooperation in alliances [internet]. Acad Manag Rev. 1998;23(3):491.
- Ring PS, Van De Ven AH. Developmental processes of cooperative interorganizational relationships [internet]. Acad Manag Rev. 1994;19(1):90.
- Cao Z, Lumineau F. Revisiting the interplay between contractual and relational governance: a qualitative and Meta-analytic investigation. J Oper Manag. 2015;33-34(1):15–42.
- Liu Y, Luo Y, Liu T. Governing buyer-supplier relationships through transactional and relational mechanisms: evidence from China. J Oper Manag. 2009;27(4):294–309.
- Szczepański R, Światowiec-Szczepańska J. Risk management system in business relationships-Polish case studies. Ind Mark Manag. 2012;41(5):790–799.
- Filippetti A, Savona M. University–industry linkages and academic engagements: individual behaviours and firms’ barriers. Introduction to the special section. J Technol Transf. 2017;142(4):719–729.
- Arza V, Carattoli M. Personal ties in university-industry linkages: a case-study from Argentina. J Technol Transf. 2017;42(4):814–840.
- Hennart J-F, Zeng M. Structural determinants of joint venture performance. Eur Manag Rev. 2005;2(2):105–115.
- Gulati R, Singh H. The architecture of cooperation: managing coordination costs and appropriation concerns in strategic alliances. Quarterly. 1998;43(4):781–814.
- Yan A, Gray B. Bargaining power, management control, and performance in US-China joint ventures: a comparative case study. Acad Manag J. 1994;37:1478–1517.
- Sheffield Hallam University (Lab4Living), Sheffield Teaching Hospital, Sheffield Children’s Hospital, Medipex, Devices4Dignity. Non-invasive customised ventillation mask for children [Internet]. Website. [cited 2022 Mar 16]. Available from: https://lab4living.org.uk/projects/non-invasive-ventilation/.
- University of Nottingham, Nottingham University Hospitals NHS Trust, Tioga Ltd. Neonatal heartrate monitoring [Internet]. Website. [cited 2022 Mar 16]. Available from: http://www.healthcaretechnologies.ac.uk/case-studies/critical-care/newborn-baby-monitoring.aspx.
- Dxcover. Early detection of cancer through liquid biopsy and artificial intelligence [Internet]. Website. [cited 2022 Mar 16]. Available from: https://www.dxcover.com.
- National Health Service. NHSX [Internet]. Website. 2022. [cited 2022 Mar 10]. Available from: https://www.nhsx.nhs.uk.