Abstract
We investigated the follow-up (3- and 6-month) intervention effects of two ACT-interventions for parents of children with chronic and developmental conditions. Parents (N = 110) were randomly assigned to the supported iACT (n = 57) or to the Self-help ACT (n = 53). At 3-month follow-up, symptoms of burnout decreased more in the supported iACT group, whereas, unexpectedly, psychological flexibility decreased in both groups. However, at the 6-month follow-up, the iACT group reported decreased symptoms and increased psychological flexibility skills. Online and self-help ACT interventions may be beneficial to this population and decrease their risk of psychopathology.
Introduction
Children with long-term conditions and complex needs require several hours of additional care and assistance on a daily basis compared to their healthy peers (Heyman et al., Citation2004). Accordingly, research has reported that parents of these children experience higher levels of stress, burnout, and poorer sleep, mental health, and quality of life when compared with parents of healthy children (Cohn et al., Citation2020; Cousino & Hazen, Citation2013; Khamis, Citation2007; Lindström et al., Citation2010; Pinquart, Citation2018). Parental burnout is defined as a prolonged response to chronic and overwhelming parental stress (Mikolajczak & Roskam, Citation2018) and refers to a state of intense exhaustion, emotional distancing, and reduced personal accomplishment, i.e., detachment from children and feelings of incompetence as a parent (Gérain & Zech, Citation2018; Roskam et al., Citation2017). Caring for a child with a chronic illness or disability implies an even greater risk of burnout (Basaran et al., Citation2013; Gérain & Zech, Citation2018). Indeed, higher levels of burnout have been found in caregivers of children with chronic conditions and developmental disabilities (Ahmadi et al., Citation2021; Basaran et al., Citation2013). Parental burnout and distress can have harmful consequences, not only for the parent but also for the children, including depressive symptoms and greater internalizing and externalizing problems (Fang et al., Citation2022; Fedele et al., Citation2011; Mikolajczak et al., Citation2019; Mullins et al., Citation2004). Owing to this growing burden, parental burnout needs urgent attention (Mikolajczak et al., Citation2019) as well as interventions to improve the well-being of caregivers of children with disabilities (Basaran et al., Citation2013). In particular, it is important to explore and better understand long-term effects of interventions supporting parental well-being. There is a limited evidence base regarding the long-term effects of online interventions targeting the well-being of parents of children with chronic conditions.
According to Whittingham (Citation2014), a third-wave approach may be particularly relevant and fruitful to parents of children with disabilities, as it may improve parental adjustment to the child’s illness, support parents’ grief, encourage flexible parenting, i.e., responding to the needs of their child in the present moment, even when the parent experiences significant stress (see also Blackledge & Hayes, Citation2006). Acceptance and commitment therapy (ACT) is a model from the third wave of cognitive behavioral therapy, with the ultimate goal to improve psychological flexibility (Hayes et al., Citation1999), that is, the ability to be mindful of experiences in the present moment, in an accepting and non-judgmental way, while behaving consistently in accordance with one’s values and in spite of unhelpful thoughts and feelings (Levin et al., Citation2014). For parents of children with chronic conditions, increased psychological flexibility may manifest in accepting difficult thoughts and emotions that may arise in caregiving situations and increasing time for personally meaningful activities in accordance with personal values (Han et al., Citation2020). Studies suggest that interventions with parents based on ACT can lead to positive outcomes that can be maintained in the long term (Chong et al., Citation2019; Lunsky et al., Citation2018). The systematic review and meta-analysis by Han et al. (Citation2021) found 24 studies on the effects of ACT interventions on family caregivers, most of whom were parents of the care recipients. The findings showed moderate effects of ACT on depressive symptoms and quality of life, small to moderate effects on stress, and small effects on anxiety. Further meta-analyses and reviews (Byrne et al., Citation2021; Parmar et al., Citation2019; Ruskin et al., Citation2021; Yu et al., Citation2019) found that ACT and mindfulness-based interventions produced moderate effects in improving caregiver psychosocial outcomes in pre-post comparisons, whereas social support and psychoeducation showed no effect. In addition, research suggest that the effects of online ACT interventions can be useful independent of the severity of the symptoms of the participants and for many different subpopulations (Pots et al., Citation2016).
These findings suggest that ACT-based interventions can provide parents with skills that they can utilize in their everyday life as a way of reducing parental stress, anxiety, and depression.
Highly qualified mental health professionals are a scarce resource, suggesting that offering one-to-one psychotherapy to the whole population is not a viable option (Bennet-Levy et al., Citation2010). Furthermore, traditional face-to-face interventions may be difficult for many parents to commit to due to time constraints and multiple demands at home (Rayner et al., Citation2016). Therefore, the use of low-intensity self-help formats would provide parents a good alternative to face-to-face psychological support, as these interventions may be delivered in self-paced pieces in the home environment. Low-intensity interventions include, among others, guided or self-guided Internet-based programs and self-help books which are the lowest-intensity type of service (Bennet-Levy et al., Citation2010). Caregivers of children with special needs and high treatment burden may find a virtual format particularly accessible.
Internet-based interventions have been found to be effective treatments for many populations (e.g., Richards & Richardson, Citation2012). They can either be delivered with some form of guidance or support from a therapist, counselor, or a coach (guided interventions) or without any support (self-guided interventions, Karyotaki et al., Citation2019). Guided Internet-based treatments have been found equally effective for psychiatric and somatic disorders as traditionally delivered treatments (Andersson et al., Citation2014, Citation2019; Carlbring et al., Citation2018; Cuijpers et al., Citation2010). Online interventions with support have been found to be associated with a larger between-group effect size (d = 0.61), whereas a smaller effect has been found in unsupported treatments (d = 0.25; Andersson & Cuijpers, Citation2009). Despite of lower effects, the evidence suggests that self-guided Internet-based cognitive behavioral interventions can alleviate symptoms associated with high prevalence disorders to some extent (Karyotaki et al., Citation2017). However, these come with limitations such as high drop-out rates (Karyotaki et al., Citation2017).
There is limited evidence on ACT-based online interventions targeting parents of children with chronic conditions and developmental disabilities (Ahola Kohut et al., Citation2021; Lappalainen et al., Citation2021; Sairanen et al., Citation2019). Ahola Kohut (Citation2021) investigated a three-session online workshop for parents of children with inflammatory bowel disease and found that the brief online ACT was feasible and acceptable in providing parents support, however, no significant group improvements in any quantitative measures were detected. The study by Sairanen et al. (Citation2019) showed that an ACT-based online intervention for parentsof children with type 1 diabetes or functional disabilities was successful without face-to-face contact. Lastly, the study of Lappalainen et al. (Citation2021) compared the effects of supported online ACT intervention with the Self-help ACT for parents of children with chronic conditions and suggested that the psychologist-supported web-based ACT produced broader improvements in parents’ psychological well-being than the self-help ACT material offered to parents. Nevertheless, both interventions decreased the symptoms of burnout and showed a beneficial impact on parents’ quality of life. The study of Sairanen et al. (Citation2019) found that that all improvements were maintained four months post-intervention. However, the long-term impact of other online ACT interventions for parents of children with chronic conditions and developmental disabilities is not known. After all, caregiver burnout and distress are serious health problems that require more attention. It is imperative to investigate alternative ways of supporting these parents.
The main aim of this randomized controlled trial was to investigate whether the effects of the two differently delivered ACT-based interventions, a supported online ACT intervention (iACT), and an ACT-based self-help (Self-help ACT), were maintained after three months after the intervention (i.e., follow-up 1). For the iACT group only, our aim was also to examine the results at six months post-intervention (follow-up 2). We expected, based on previous research of guided online interventions (e.g., Andersson & Cuijpers, Citation2009), that participation in a supported web-based intervention would be associated with significantly larger decreases in burnout and depressive symptoms and with significantly larger increases in psychological flexibility and mindfulness skills in comparison to the Self-help ACT group from post to follow-up measurement.
Methods
Participants and procedure
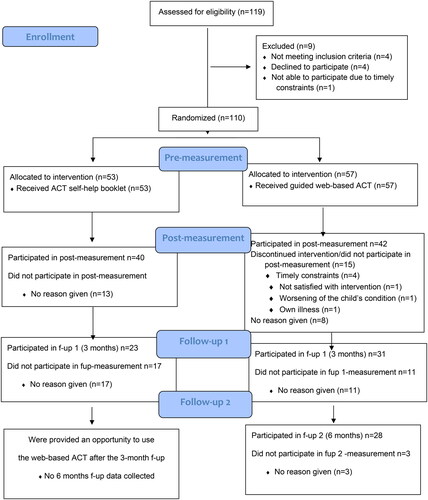
Parents were recruited through advertisements in local newspapers and the Facebook pages of diverse caregiver and family organizations. Those interested in taking part were invited to a telephone screening interview. The eligible participants (1) had a child under the age of 18 with a chronic condition or developmental disability; (2) scored greater than 2.75 points on the Shirom-Melamed Burnout Questionnaire (SMBQ), indicating mild symptoms of burnout (Lundgren-Nilsson et al., Citation2012; Melamed et al., Citation1999); (3) had no parallel psychological treatment; (4) did not suffer from a serious mental disorder; (5) had sufficient Finnish language skills; and (6) had access to the Internet through a computer or other device. Eligible parents (n = 110), most of them being females (n = 103; 93.6%) and with a mean age of 40.1 years (SD = 6.68, range 27–55) were randomized to supported web-based ACT (iACT; n = 57) and ACT self-help group (Self-help ACT; n = 53, ). Participants were highly educated, with nearly 70% (n = 76, 69.1%) of them having a university-level education. Most of the children were male (n = 76, 68.5%), with a mean age of nine years (SD = 4.29), and with predominantly developmental disabilities. At pre-measurement, more than 60% of the parents were classified as experiencing severe levels of burnout (Shirom-Melamed Burnout Questionnaire; Lundgren-Nilsson et al., Citation2012; Melamed et al., Citation1999; SMBQ ≥ 4.47), and nearly 56% had at least moderate levels of depression (Patient Health Questionnaire-9; Kroenke et al., Citation2001; PHQ-9 > 10). Detailed characteristics are reported in .
Table 1. Characteristics of parents.
Among the parents who participated in the 6-month follow-up (follow-up 2; iACT, n = 28), all except for one parent (n = 27, 96.4%) were female, and their age was, on average, 39.1 years, (SD = 7.3). Nearly all of them were married or co-habiting (n = 26, 92.9%), had a university education (n = 21, 75%), and worked fulltime (n = 14, 50%). The most common diseases in their children were autism spectrum disorders (n = 7, 25%) and developmental conditions (n = 6, 21.4%).
0.02w?>Data on parents’ psychological well-being were collected at baseline (pre-measurement; n = 110, ), at 10-week post-measurement (n = 82/75%), three months after the post-measurement (follow-up 1; n = 54/49%; iACT, n = 31/54%; Self-help ACT, n = 23/43%), and for the supported iACT group only, six months post-intervention (follow-up 2; n = 28/49%). For the flow of the intervention, see . As the Self-help ACT group was offered the intervention after the first follow-up measurement (follow-up 1, three months), the six-month follow-up (follow-up 2) could not be conducted for this group.
The study was conducted in the Psychology Department Clinic at the University of Jyväskylä in 2019–2020. Ethical approval for the study was obtained from the Ethical Committee of the Central Finland Health Care District (board affiliation: Central Finland Central Hospital; approval number 12/U2018 on November 6, 2018, registered at www.clinicaltrials.gov; ClinicalTrials.gov, Identifier: NCT04250012, Protocol ID 18/26/2018). The participants took part in the study on a voluntary basis and gave written informed consent for their participation.
Interventions
A detailed description of the interventions has been provided elsewhere (Lappalainen et al., Citation2021). In short, the supported iACT intervention consisted of a web program and three videoconferencing meetings with a psychologist. The program included five modules, and the participants were instructed to spend two weeks per module (10 weeks in total). The modules were based on the processes of ACT: (1) What is important to you? (2) meaningful actions; (3) present moment; (4) distance to thoughts and feelings; and (5) acceptance and self-compassion (see for the program content). The iACT intervention included three 45-min videoconferencing meetings with a clinical psychologist using the Doxy.me telecommunication application (www.doxy.me). Two clinical psychologists with several years of experience in ACT worked as coaches. The first videoconference meeting was arranged at the beginning of the intervention—before access to the web program—the second after the first two modules (i.e., four weeks from the start), and the third took place at the end of the intervention (i.e., weeks 8–9).
Table 2. Content for the supported iACT online intervention.
The parents in the self-help group (n = 53) received a 20-page self-help booklet highlighting the ACT approach, which was sent to them by regular mail. In addition, the participants in this group were encouraged to visit the Oivamieli website (www.oivamieli.fi), a publicly accessible web page that included a series of ACT-based exercises. The participants in the Self-help ACT group did not have access to the same website as the supported iACT group, neither did they not receive any professional support during the intervention period (see ).
Table 3. Content of the self-help booklet, 20 pages with text and pictures.
Symptom measures
The Shirom-Melamed Burnout Questionnaire (SMBQ, Lundgren-Nilsson et al., Citation2012; Melamed et al., Citation1999) was used as the main outcome measure to assess parental burnout symptoms. The measure comprises four subscales: emotional exhaustion, physical fatigue, listlessness, and tension. The statements are answered on a 7-point Likert scale, ranging from 1 (almost never) to 7 (almost always). Based on the SMBQ, burnout can be divided into low (2.75–3.74), high (3.75–4.46), and pathological (≥ 4.47) levels. The validity and reliability of the SMBQ have been found to be good in previous studies (Lundgren-Nilsson et al., Citation2012). In this study, Cronbach’s alpha at baseline was excellent, 0.92.
Depressive symptoms were measured by the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., Citation2001), which is used for diagnosing and assessing the severity of depressive disorders. The PHQ-9 contains nine items, which are answered on a 4-point Likert scale, ranging from 0 (not at all) and 3 (almost every day). The total score on the PHQ-9 ranges from 0 to 27, with a higher score indicating more depressive symptoms. PHQ-9 scores of 5 (5–9), 10 (10–14), 15 (15–19), and 20 (20–27) represent mild, moderate, moderately severe, and severe depression, respectively. The validity and reliability of the PHQ-9 have been found to be good (Kroenke et al., Citation2001). In this study, Cronbach’s alpha indicated adequate reliability, α = 0.78.
Process measures
Psychological flexibility was measured with the Comprehensive Assessment of ACT processes (CompACT; Francis et al., Citation2016), a 23-item questionnaire that includes three subscales: openness to experience (CompACT-OE), behavioral awareness (CompACT-BA), and valued action (CompACT-VA). The items are answered on a 7-point Likert scale ranging from 0 (strongly disagree) to 6 (strongly agree), with higher scores representing greater levels of psychological flexibility (openness, awareness, action). The total score of the CompACT ranges from 0 to 138, with the CompACT-OE ranging from 0 to 60, the CompACT-BA ranging from 0 to 30, and the CompACT-VA ranging from 0 to 48. In this study, the CompACT showed adequate to good internal consistency for the total score (α = 0.83), α = 0.79 for the CompACT-OE, α = 0.76 for the CompACT-VA, and α = 0.80 for the CompACT-BA.
The Five Facet Mindfulness Questionnaire (FFMQ) was used to assess mindfulness skills (Baer et al., Citation2006). The measure includes five aspects of mindfulness: observing (noticing internal and external experiences), describing (naming and labeling internal experiences), acting with awareness (paying attention to one’s activities in the present moment), non-judging of inner experiences (having a non-evaluative stance toward inner experiences), and non-reactivity to inner experiences (ability to let thoughts and feelings come and go without struggle). The scale comprises 39 items rated on a 5-point Likert-type scale ranging from 1 (never or very rarely true) to 5 (very often or always true), with higher scores indicating higher levels of mindfulness. The reliability and validity of the FFMQ have been found to be good (Baer et al., Citation2006). In this study, the FFMQ showed adequate to high reliability for the total score (α = 0.87), with α = 0.74 for observing, α = 0.91 for describing, α = 0.79 for non-judging and non-reacting, and α = 0.82 for acting with awareness.
Statistical analysis
All statistical analyses were conducted using Mplus version 8 (Muthén and Muthén, Citation2017). Descriptive statistics were carried out to provide an overview of the mean and change scores of the process and outcome measures. Path model using change scores was used to analyze the group x time interaction, i.e., whether the groups changed differently between the measured time points (Pre, Post, Fup). If there was a difference, post hoc tests were conducted to determine between the groups whether the difference was during the intensive intervention period or after the intensive intervention period. HLM accounts for missing values at random (MAR) and includes all available data. The parameters were estimated using the full-information maximum likelihood method (MLR estimation in Mplus). Separate within-group analyses were done in the supported iACT group investigating changes from Pre to Post, and to Follow-Up at three months and six months. Effect sizes (ES) between groups at post- and follow-up 1 measurements were investigated using the pre-measurement corrected Cohen’s d values to consider the possible difference between the groups before the intervention. Effect sizes within the supported web-based iACT were also investigated. Effect sizes (ESs) were reported using Cohen’s d. An effect size (d) value = 0.20 was considered small, d = 0.50 medium, and d = 0.80 large. Because the within-group effects sizes tend to be larger than the between-group ES, we interpreted that a change had occurred when the with 95% Confidence Interval of the ES did not include zero. In our data, this change was equal to at least medium-size ES (d > 0.50).
Results
Before treatment, a significant difference between the groups was observed in age, with the parents in the supported iACT group being slightly younger (iACT, M = 38.9 years; SD = 6.85; Self-help ACT, M = 41.5 years; SD = 6.29, ). However, this difference (39 vs. 42 years) was considered as clinically non-significant.
Dropouts
Among the supported iACT group, the dropout rate from the pre-measurement to the three-month follow-up measurement was 45.6% (n = 26) compared to 56.6% (n = 30) in the self-help condition. For the iACT condition only, the dropout rate from the pre-measurement to the six-month post-intervention measurement was 50.9% (n = 29).
Changes in symptoms at the three-month follow-up
Significant time-by-group interactions (from the pre-measurement to the three-month follow-up) were found in burnout (SMBQ) total, SMBQ physical fatigue, SMBQ emotional exhaustion, and depression symptoms (PHQ-9). At the three-month follow-up, when compared with parents who had participated in the self-help condition, parents in the supported iACT group reported having significantly fewer symptoms of burnout (SMBQ total score: the between-group effect size, db = 0.44). In particular, the parents in the iACT condition experienced less physical fatigue with medium effect size (ES, db > 0.50) and emotional exhaustion (db = 0.44), as well as fewer symptoms of depression, with small ES (db = 0.29; see ). In addition, based on the within-effect sizes (95% CI), the self-help ACT produced beneficial changes for up to three months in SMBQ total (dw = 0.57; 0.07; 1.06) and SMBQ tension (dw = 0.66; 0.16; 1.16). Overall, as shown in , symptoms for participants in both interventions remained at a lower level at follow-up compared to the pre-measurements.
Table 4. Symptom measures, estimated mean values, and standard deviations, p-values, between (db) and within (dw) group effect sizes at Pre, Post, and 3-month Follow-up.
Changes in process measures at the three-month follow-up
The participants’ scores for psychological flexibility (their CompACT total scores) as well as their scores on the three subscales—Openness to Experiences (OE), Behavioral Awareness (BA), and Valued Action (VA)—changed differently in the two intervention groups from the pre-measurement to the three-month follow-up (). However, this difference was due to a larger increase in their CompACT scores from pre- to post-measurement. From the post-intervention measurement to the three-month follow-up, the iACT and self-help ACT groups did not change differently in psychological flexibility (their CompACT total scores). Interestingly, psychological flexibility skills decreased to the pre-measurement level or below during the three-month follow-up period in both groups. This was especially true for the Valued Actions subscale, where the decrease was large (d > 0.80) from pre-measurement to follow-up 1. Mindfulness skills as measured by the FFMQ Total and FFMQ Describing increased significantly more from the pre- to post-measurement in the iACT group compared to the self-help ACT, but from the post-intervention measurement to the three-month follow-up, they decreased in both groups, with larger decreases in the self-help ACT group with small ES (d = 0.20–0.49). The decreases in psychological flexibility and mindfulness skills were significant in both groups; within ES, this decrease was large (d > 0.80; CompACT Total, with a 95% CI: iACT, d = 0.68; 1.79, self-help, d = 0.28; 1.58; FFMQ Total, iACT, d = 0.60; 1.71, self-help ACT, d = 0.81; 2.21).
Table 5. Process measures, estimated mean values, and standard deviations, p-values, between (db) and within (dw) group effect sizes at pre, post, and 3-month follow-up.
Changes in the iACT group at the six-month follow-up (follow-up 2)
When investigating the change in the supported iACT group only (n = 28) from the pre-measurement to the six-month follow-up (follow-up 2; ), the results showed significant changes over time in both symptom and process measures. Burnout and depression symptoms decreased during the iACT intervention and remained at a lower level up to six months following the intervention (dw = 0.69–0.86). As described above, psychological flexibility (CompACT) and mindfulness (FFMQ) increased significantly from the pre- to the post-intervention measurement, decreased from the post-intervention to the three-month follow-up (follow-up 1), but increased again between the three-month and six-month follow-ups. The levels of CompACT and FFMQ were higher at the six-month follow-up (follow-up 2) compared to the pre-measurement levels (within ES, CompACT Total, d = 0.21; 1.14; FFMQ Total, d = 0.08; 1.00). The mean scores, standard deviations, and effect sizes for the supported iACT condition are presented in .
Table 6. The follow-up (Fup1 = three months; Fup2 = six months post-intervention) results of the supported iACT intervention for parents of children with chronic conditions.
Discussion
Parents of children with chronic illnesses and developmental disabilities may be at risk of suboptimal health outcomes. Therefore, interventions aimed at improving their health and well-being are warranted. There is limited evidence regarding the effects of online ACT interventions targeting the well-being of parents of children with chronic and developmental conditions. Therefore, it is important to explore and better understand what kinds of interventions are effective in maintaining positive parent outcomes over a longer period.
The current study set out to investigate the three-month follow-up results of a web-based, psychologist-supported ACT intervention (iACT) for parents of children with chronic conditions and developmental disabilities in comparison to the results of an ACT-based self-help intervention (self-help ACT). The primary aim of the study was to examine whether the effects of (1) a supported iACT intervention and (2) a self-help ACT intervention were maintained at three months post-intervention for both intervention groups and at six months post-intervention for the iACT group only. Our hypothesis was that participation in a 10-week web-based intervention would be associated with significantly larger decreases between the pre-measurement and the follow-up measurements in burnout and depressive symptoms and significantly larger increases in psychological flexibility and mindfulness skills in comparison to participation in the ACT self-help intervention.
Our hypothesis was partially supported. The supported online iACT intervention produced larger changes in the main outcome of burnout symptoms, including physical fatigue and emotional exhaustion as well as depressive symptoms from the pre-measurement to the three-month follow-up compared to the self-help ACT condition, showing small to medium-sized differences between the groups (db = 0.29–0.64). Regarding the symptoms of burnout and depression, these results are partly in line with earlier findings from studies on online ACT interventions for parents of children with chronic conditions and developmental disabilities. For example, these results are congruent with the results obtained by Sairanen et al. (Citation2019) in their online intervention for parents of children with chronic conditions, which showed a decrease in symptoms of burnout and maintenance of depressive symptoms between the pre-measurement and the four-month follow-up measurement. Our results are also consistent with earlier findings suggesting that the effects of online ACT interventions are maintained for between one and six months (Karekla et al., Citation2022; Kiuru et al., Citation2021) and that these interventions can be useful independent of the severity of the symptoms of the participants and for many different subpopulations (Pots et al., Citation2016). Importantly, although the supported online iACT resulted in a larger decrease in burnout symptoms at the three-month follow-up, the self-help ACT without any support also resulted in a decrease in burnout symptoms. As our study did not include a non-treatment comparison group, the results were compared with a similar study by Sairanen et al. (Citation2019) which used a waitlist control condition. Consequently, at the four-month follow-up in the Sairanen et al. (Citation2019) study, the within ES in the wait list control group was very small or non-existent (d = 0.09, 95% CI, −0.42; 0.59), whereas it was considerably larger in the self-help as well as in the online group at the three-month follow-up in the current study (Self-help: d = 0.57, 95% CI, 0.07; 1.06; Online: d = 0.88, 95% CI, 0.41; 1.32). However, it should be remembered that these results were obtained from participants in different countries and at different time points.
In addition, our findings indicated that both psychological flexibility and mindfulness skills increased more during the intervention period in the iACT group compared to the self-help ACT group; however, these changes were not maintained three months post-intervention.
Unexpectedly, and opposite to earlier studies (e.g., Sairanen et al., Citation2019), we noticed a dramatic decrease in psychological flexibility during the three-month period following the intervention. Interestingly, this decrease was not reflected in the level of symptoms of burnout or depression. The large decreases in both psychological flexibility and mindfulness from post-intervention measurement to the three-month follow-up may indicate that many parents either stopped applying psychological flexibility skills when the intervention period ended or were not able to apply them in their daily life. An alternative or additional explanation is that the COVID-19 pandemic possibly affected this unexpected change. The decrease in psychological flexibility scores may have been a consequence of the outbreak of the COVID-19 pandemic as most of the three-month follow-up data was being collected during the COVID-19 pandemic. Previously, we have observed that psychological flexibility and self-compassion skills may have protected against the psychological distress caused by the COVID-19 pandemic in adult and adolescent populations (Dawson & Golijani-Moghaddam, Citation2020; Lappalainen et al., Citation2023; McCracken et al., Citation2021). Interestingly, and in accordance with earlier studies (Lappalainen et al., Citation2023), parents’ burnout and depressive symptoms remained at a lower level throughout the study and during the pandemic. In terms of psychological flexibility and mindfulness, as well as symptom outcomes, our results are consistent with earlier studies showing that the effects of an ACT-based online intervention for parents of children with chronic conditions were maintained following the intervention (see Sairanen et al., Citation2019). In line with a study by de Wit et al. (Citation2019), this study suggests that delivering online support seems to be beneficial in supporting parents and caregivers of children with chronic illnesses.
Adherence, which is the degree to which users engage with the content of an intervention as intended, is a critical topic in digital interventions (Karekla et al., Citation2019), as greater adherence leads to improved health outcomes (Donkin et al., Citation2011). In contrast, low adherence impacts the effectiveness of the intervention and increases the dropout rate (Hilvert-Bruce et al., Citation2012; Trompetter et al., Citation2015). In this study, the dropout rates were relatively high over the study period. In the iACT condition, more than 40% of the parents dropped out between the pre-measurement and the three-month follow-up, whereas in the self-help condition, the dropout rate was more than half, 56.6%. An adherence rate of this size is not rare in online interventions (Christensen et al., Citation2009), however, this is a relatively low percentage. Lack of time is a commonly reported dropout reason in caregiver studies (Blom et al., Citation2015), which may also have been one of the most common reasons for dropout in the current study. As some of these parents were caregivers of more than one child with special needs, they may have been so occupied by caregiving that any more obligations were perceived as burdensome. This is a common finding in studies with caregivers (see, e.g., de Wit et al., Citation2020).
Limitations
Although the results of the current study confirm earlier findings of studies of online interventions supporting parents of children with chronic conditions and developmental disabilities, definitive conclusions cannot be made based on the limited number of studies conducted thus far. In the current study, we are not able to rule out the possibility that changes could have occurred without any intervention. However, in their study, Sairanen et al. (Citation2019) observed no changes in the non-treatment control group. A further limitation concerns the study sample. It must be noted that the investigated sample of children included a wide range of conditions, and in the current study, it was not possible to study the effectiveness and the acceptability of the intervention in different subgroups of children. Although we intended to recruit mothers and fathers in the same proportion, nearly all the participants were mothers (94%). Thus, future studies should include an equal number of mothers and fathers to assess gender differences more accurately among parents of children with chronic conditions and developmental disabilities. In addition, the representativeness of the sample may be compromised because nearly 70% of the parents were highly educated. Participants from more heterogeneous social backgrounds would ensure a more representative sample of parents. Also, the large number of dropouts during the follow-up period is a problem, and more attention should be paid to how to motivate parents to participate in follow-up measurements. However, there were no differences at pre-measurement between those participated in the 6-month follow-up and drop-outs in terms of burnout symptoms, symptoms of depression, psychological flexibility age, gender, and education level. Finally, the use of self-report questionnaires should be considered a limitation. Therefore, a multi-method measurement approach should be considered in future studies.
Future directions and conclusions
The present study is one of the first to provide evidence that a brief online ACT intervention with minimum support may decrease the pathological symptoms of burnout among parents with children with chronic conditions and developmental disabilities in the long term. Our results are in line with earlier research suggesting that online interventions with support have been found to be associated with larger between-group effect sizes compared to unsupported online treatments (Andersson & Cuijpers, Citation2009). Andersson and Cuijpers (Citation2009) found, on average, a between-group effect size of d = 0.61 for guided and d = 0.25 for unsupported online interventions. It must be noted that our iACT online intervention for parents was brief and included, in addition to the online program, only three videoconferencing sessions facilitated by a psychologist, implying that it offered fewer resources than the traditional support provided to parents. In addition, this study suggests that if supported or face-to-face interventions are not available, a cost-effective self-help ACT delivered without any professional contact may also bring some, although limited, health benefits to parents who are struggling to care for their children with special needs. Our results are in accordance with findings showing that, despite lower effects, low-intensity self-guided interventions, such as the self-help ACT condition in the current study, can bring benefits (Karyotaki et al., Citation2017; Richards & Richardson, Citation2012). Self-guided interventions, such as the self-help ACT intervention, may be a viable alternative as a first-step treatment approach for symptoms of burnout and depression. In addition, the two low-intensity treatment options described in the current study can provide treatment access at low cost to large numbers of parents worldwide.
In accordance with earlier studies (e.g., Bradshaw et al., Citation2019), the current study revealed that over half of the parents reported severe levels of burnout and moderate depression, and, therefore, significant support needs must be addressed to improve parent outcomes. These two examples of remote and flexible interventions demonstrate that geography or busy schedules do not need to be a barrier to delivery or prevent parents from participating in psychological intervention. This study also suggests that distressed parents may benefit significantly from cost-effective interventions where support can be provided through minimal contact videoconferencing sessions.
As research to reduce health care costs over the long term should be promoted (Cohn et al., Citation2020), the current two interventions could be offered for delivery within routine care settings, without any support or including minimal contact from health professionals. However, these two approaches are unlikely to meet the needs of all parents. Therefore, further development of these interventions is needed to make them relevant and meaningful and to maximize the intervention effects for parents of children with chronic conditions and developmental disabilities. To ensure that interventions are acceptable and meaningful to parents, parents should be involved in the development of interventions in future studies. Overall, future research is needed to better understand the short- and long-term health outcomes of parental caregiving and the optimal ways to deliver online support for parents. Online interventions based on an acceptance and mindfulness approach—such as ACT—may form part of the support offered to these parents and may decrease their risk of psychopathology. At the same time, these interventions may also assist parents in flexible parenting—responding to the needs of their child, even in the presence of significant parental stress.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data supporting the conclusions of this article will be made available by the authors by request.
Additional information
Funding
References
- Ahmadi, B., Sabery, M., & Adib-Hajbaghery, M. (2021). Burnout in the primary caregivers of children with chronic conditions and its related factors. Journal of Client-Centered Nursing Care, 7(2), 139–148. https://doi.org/10.32598/JCCNC.7.2.360
- Ahola Kohut, S., Martincevic, I., Turrell, S. L., Church, P. C., Walters, T. D., Weiser, N., & Iuliano, A. (2021). online acceptance and commitment therapy and nutrition workshop for parents of children with inflammatory bowel disease: Feasibility, acceptability, and initial effectiveness. Children, 8(5), 396. https://doi.org/10.3390/children8050396
- Andersson, G., & Cuijpers, P. (2009). Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy, 38(4), 196–205. https://doi.org/10.1080/16506070903318960
- Andersson, G., Cuijpers, P., Carlbring, P., Riper, H., & Hedman, E. (2014). Guided Internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: A systematic review and meta‐analysis. World Psychiatry, 13(3), 288–295. https://doi.org/10.1002/wps.20151
- Andersson, G., Titov, N., Dear, B. F., Rozental, A., & Carlbring, P. (2019). Internet-delivered psychological treatments: From innovation to implementation. World Psychiatry, 18(1), 20–28. https://doi.org/10.1002/wps.20610
- Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
- Basaran, A., Karadavut, K. I., Uneri, S. O., Balbaloglu, O., & Atasoy, N. (2013). The effect of having a children with cerebral palsy on quality of life, burn-out, depression and anxiety scores: A comparative study. European Journal of Physical and Rehabilitation Medicine, 49(6), 815–822.
- Bennet-Levy, J., Richards, D. A., & Farrand, P. (2010). Low-intensity CBT interventions: a revolution in mental health care. In J. Bennett-Levy, D. A. Richards, P. Farrand, H. Christensen, K. M Griffiths, D. J. Kavanagh, B. Klein, M. A. Lau, J. Proudfoot, L. Ritterband, J. White, & C. Williams (Eds.), Oxford Guide to Low Intensity CBT Interventions. Oxford University Press.
- Blackledge, J. T., & Hayes, S. C. (2006). Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child & Family Behavior Therapy, 28(1), 1–18. https://doi.org/10.1300/J019v28n01_01
- Blom, M. M., Zarit, S. H., Groot Zwaaftink, R. B., Cuijpers, P., & Pot, A. M. (2015). Effectiveness of an internet intervention for family caregivers of people with dementia: results of a randomized controlled trial. PLOS One, 10(2), e0116622. https://doi.org/10.1371/journal.pone.0116622
- Bradshaw, S., Bem, D., Shaw, K., Taylor, B., Chiswell, C., Salama, M., Bassett, E., Kaur, G., & Cummins, C. (2019). Improving health, wellbeing and parenting skills in parents of children with special health care needs and medical complexity – a scoping review. BMC Pediatrics, 19(1), 301. https://doi.org/10.1186/s12887-019-1648-7
- Byrne, G., Ghráda, Á. N., O’Mahony, T., & Brennan, E. (2021). A systematic review of the use of acceptance and commitment therapy in supporting parents. Psychology and Psychotherapy, 94(S2), 378–407. https://doi.org/10.1111/papt.12282
- Carlbring, P., Andersson, G., Cuijpers, P., Riper, H., & Hedman-Lagerlöf, E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behaviour Therapy, 47(1), 1–18. https://doi.org/10.1080/16506073.2017.1401115
- Chong, Y. Y., Mak, Y. W., Leung, S. P., Lam, S. Y., & Loke, A. Y. (2019). Acceptance and commitment therapy for parental management of childhood asthma: An RCT. Pediatrics, 143(2), 1–16. https://doi.org/10.1542/peds.2018-1723
- Cohn, L. N., Pechlivanoglou, P., Lee, Y., Mahant, S., Orkin, J., Marson, A., & Cohen, E. (2020). Health outcomes of parents of children with chronic illness: A systematic review and meta-analysis. Journal of Pediatrics, 218, 166.e2–177.e2. https://doi.org/10.1016/j.jpeds.2019.10.068
- Cousino, M. K., & Hazen, R. A. (2013). Parenting stress among caregivers of children with chronic illness: a systematic review. Journal of Pediatric Psychology, 38(8), 809–828. https://doi.org/10.1093/jpepsy/jst049
- Christensen, H., Griffiths, K. M., & Farrer, L. (2009). Adherence in internet interventions for anxiety and depression. Journal of Medical Internet Research, 11(2), e13. https://doi.org/10.2196/jmir.1194
- Cuijpers, P., Donker, T., van Straten, A., Li, J., & Andersson, G. (2010). Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychological Medicine, 40(12), 1943–1957. https://doi.org/10.1017/S0033291710000772
- Dawson, D. L., & Golijani-Moghaddam, N. (2020). COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134. https://doi.org/10.1016/j.jcbs.2020.07.010
- De Wit, J., Beelen, A., Drossaert, C. H. C., Kolijn, R., Van Den Berg, L. H., SchrÖder, C. D., & Visser-Meily, J. M. A. (2020). Blended psychosocial support for partners of patients with ALS and PMA: Results of a randomized controlled trial. Amyotrophic Lateral Sclerosis & Frontotemporal Degeneration, 21(5–6), 344–354. https://doi.org/10.1080/21678421.2020.1757114
- De Wit, J., Vervoort, S. C., van Eerden, E., van den Berg, L. H., Visser-Meily, J. M., Beelen, A., & Schröder, C. D. (2019). User perspectives on a psychosocial blended support program for partners of patients with amyotrophic lateral sclerosis and progressive muscular atrophy: A qualitative study. BMC Psychology, 7(1), 1–13. https://doi.org/10.1186/s40359-019-0308-x
- Donkin, L., Christensen, H., Naismith, S. L., Neal, B., Hickie, I. B., & Glozier, N. (2011). A systematic review of the impact of adherence on the effectiveness of e-therapies. Journal of Medical Internet Research, 13(3), e52. https://doi.org/10.2196/jmir.1772
- Fang, Y., Luo, J., Boele, M., Windhorst, D., van Grieken, A., & Raat, H. (2022). Parent, child, and situational factors associated with parenting stress: A systematic review. European Child & Adolescent Psychiatry. Advance online publication. https://doi.org/10.1007/s00787-022-02027-1
- Fedele, D. A., Mullins, L. L., Wolfe-Christensen, C., & Carpentier, M. Y. (2011). Longitudinal assessment of maternal parenting capacity variables and child adjustment outcomes in pediatric cancer. Journal of Pediatric Hematology/Oncology, 33(3), 199–202. https://doi.org/10.1097/mph.0b013e3182025221
- Francis, A. W., Dawson, D. L., & Golijani-Moghaddam, N. (2016). The development and validation of the comprehensive assessment of acceptance and commitment therapy processes (CompACT). Journal of Contextual Behavioral Science, 5(3), 134–145. https://doi.org/10.1016/j.jcbs.2016.05.003
- Gérain, P., & Zech, E. (2018). does informal caregiving lead to parental burnout? Comparing parents having (or not) children with mental and physical issues. Frontiers in Psychology, 9, 884. https://doi.org/10.3389/fpsyg.2018.00884
- Han, A., Yuen, H. K., Hee Yun Lee, H. Y., & Zhou, X. (2020). Effects of acceptance and commitment therapy on process measures of family caregivers: A systematic review and meta-analysis. Journal of Contextual Behavioral Science, 18, 201–213. https://doi.org/10.1016/j.jcbs.2020.10.004
- Han, A., Yuen, H. K., & Jenkins, J. (2021). Acceptance and commitment therapy for family caregivers: A systematic review and meta-analysis. Journal of Health Psychology, 26(1), 82–102. https://doi.org/10.1177/1359105320941217
- Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press. https://doi.org/10.1177/1359105320941217
- Heyman, M. B., Harmatz, P., Acree, M., Wilson, L., Moskowitz, J. T., Ferrando, S., & Folkman, S. (2004). Economic and psychologic costs for maternal caregivers of gastrostomy-dependent children. Journal of Pediatrics, 145(4), 511–516. https://doi.org/10.1016/j.jpeds.2004.06.023
- Hilvert-Bruce, Z., Rossouw, P. J., Wong, N., Sunderland, M., & Andrews, G. (2012). Adherence as a determinant of effectiveness of Internet cognitive behavioural therapy for anxiety and depressive disorders. Behaviour Research and Therapy, 50(7–8), 463–468. https://doi.org/10.1016/j.brat.2012.04.001
- Karyotaki, E., Furukawa, T. A., Efthimiou, O., Riper, H., & Cuijpers, P. (2019). Guided or self-guided internet-based cognitive-behavioural therapy (iCBT) for depression? Study protocol of an individual participant data network meta-analysis. BMJ Open, 9(6), e026820. https://doi.org/10.1136/bmjopen-2018-026820
- Karyotaki, E., Riper, H., Twisk, J., Hoogendoorn, A., Kleiboer, A., Mira, A., Mackinnon, A., Meyer, B., Botella, C., Littlewood, E., Andersson, G., Christensen, H., Klein, J. P., Schröder, J., Bretón-López, J., Scheider, J., Griffiths, K., Farrer, L., Huibers, M. J. H., … Cuijpers, P. (2017). Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: A meta-analysis of individual participant data. JAMA Psychiatry, 74(4), 351–359. https://doi.org/10.1001/jamapsychiatry.2017.0044
- Karekla, M., Kasinopoulos, O., Neto, D. D., Ebert, D. D., Van Daele, T., Nordgreen, T., Höfer, S., Oeverland, S., & Jensen, K. L. (2019). Best practices and recommendations for digital interventions to improve engagement and adherence in chronic illness sufferers. European Psychologist, 24(1), 49–67. https://doi.org/10.1027/1016-9040/a000349
- Karekla, M., Nikolaou, P., & Merwin, R. M. (2022). Randomized clinical trial evaluating AcceptME—A digital gamified acceptance and commitment early intervention program for individuals at high risk for eating disorders. Journal of Clinical Medicine, 11(7). https://doi.org/10.3390/jcm11071775
- Khamis, V. (2007). Psychological distress among parents of children with mental retardation in the United Arab Emirates. Social Science & Medicine, 64(4), 850–857. https://doi.org/10.1016/j.socscimed.2006.10.022
- Kiuru, N., Puolakanaho, A., Lappalainen, P., Keinonen, K., Mauno, S., Muotka, J., & Lappalainen, R. (2021). Effectiveness of a web-based acceptance and commitment therapy program for adolescent career preparation: A randomized controlled trial. Journal of Vocational Behavior, 127, 103578. https://doi.org/10.1016/j.jvb.2021.103578
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Lappalainen, P., Lappalainen, R., Keinonen, K., Kaipainen, K., Puolakanaho, A., Muotka, J., & Kiuru, N. (2023). In the shadow of COVID-19: A randomized controlled online ACT trial promoting adolescent psychological flexibility and self-compassion. Journal of Contextual Behavioral Science, 27, 34–44. https://doi.org/10.1016/j.jcbs.2022.12.001
- Lappalainen, P., Pakkala, I., Strömmer, J., Sairanen, E., Kaipainen, K., & Lappalainen, R. (2021). Supporting parents of children with chronic conditions: A randomized controlled trial of web-based and self-help ACT interventions. Internet Interventions. 24, 100382. https://doi.org/10.1016/j.invent.2021.100382
- Levin, M. E., Pistorello, J., Seeley, J. R., & Hayes, S. C. (2014). Feasibility of a prototype web-based acceptance and commitment therapy prevention program for college students. Journal of American College Health, 62(1), 20–30. https://doi.org/10.1080/07448481.2013.843533
- Lindström, C., Åman, J., & Norberg, A. (2010). Increased prevalence of burnout symptoms in parents of chronically ill children. Acta Paediatrica, 99(3), 427–432. https://doi.org/10.1111/j.1651-2227.2009.01586.x
- Lundgren-Nilsson, Å., Jonsdottir, I. H., Pallant, J., & Ahlborg, G. (2012). Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ). BMC Public Health, 12(1), 1–8. https://doi.org/10.1186/1471-2458-12-1
- Lunsky, Y., Fung, K., Lake, J., Steel, L., & Bryce, K. (2018). Evaluation of acceptance and commitment therapy (ACT) for mothers of children and youth with autism spectrum disorder. Mindfulness, 9(4), 1110–1116. https://doi.org/10.1007/s12671-017-0846-3
- McCracken, L. M., Badinlou, F., Buhrman, M., & Brocki, K. C. (2021). The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. Journal of Contextual Behavioral Science, 19, 28–35. https://doi.org/10.1016/j.jcbs.2020.11.003
- Melamed, S., Ugarten, U., Shirom, A., Kahana, L., Lerman, Y., & Froom, P. (1999). Chronic burnout, somatic arousal and elevated salivary cortisol levels. Journal of Psychosomatic Research, 46(6), 591–598. https://doi.org/10.1016/s0022-3999(99)00007-0
- Mikolajczak, M., Gross, J. J., & Roskam, I. (2019). Parental burnout: What is it, and why does it matter? Clinical Psychological Science, 7(6), 1319–1329. https://doi.org/10.1177/2167702619858430
- Mikolajczak, M., & Roskam, I. (2018). A theoretical and clinical framework for parental burnout: The balance between risks and resources. Frontiers in Psychology, 9, 886. https://doi.org/10.3389/fpsyg.2018.00886
- Mullins, L. L., Fuemmeler, B. F., Hoff, A., Chaney, J. M., Van Pelt, J., & Ewing, C. A. (2004). The relationship of parental overprotection and perceived child vulnerability to depressive symptomotology in children with type 1 diabetes mellitus: The moderating influence of parenting stress. Children’s Health Care, 33(1), 21–34. https://doi.org/10.1207/s15326888chc3301_2
- Muthén, L. K., & Muthén, B. O. (2017). Mplus: Statistical analysis with latent variables: User’s guide (Version 8).
- Parmar, A., Morinis, L., Barreira, L., Miller, D., Major, N., Church, P., Cohen, E., & Orkin, J. (2019). 24 acceptance and commitment therapy (ACT) for parents of children with a chronic medical condition: A systematic review. Paediatrics & Child Health, 24(Suppl 2), e10. https://doi.org/10.1093/pch/pxz066.023
- Pinquart, M. (2018). Parenting stress in caregivers of children with chronic physical condition-A meta-analysis. Stress and Health, 34(2), 197–207. https://doi.org/10.1002/smi.2780
- Pots, W. T., Trompetter, H. R., Schreurs, K. M., & Bohlmeijer, E. T. (2016). How and for whom does web-based acceptance and commitment therapy work? Mediation and moderation analyses of web-based ACT for depressive symptoms. BMC Psychiatry, 16(1), 158. https://doi.org/10.1186/s12888-016-0841-6
- Rayner, M., Muscara, F., Dimovski, A., McCarthy, M. C., Yamada, J., Anderson, V. A., Burke, K., Walser, R., & Nicholson, J. M. (2016). Take a breath: Study protocol for a randomized controlled trial of an online group intervention to reduce traumatic stress in parents of children with a life threatening illness or injury. BMC Psychiatry, 16, Article 169. https://doi.org/10.1186/s12888-016-0861-2
- Richards, D., & Richardson, T. (2012). Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clinical Psychology Review, 32(4), 329–342. https://doi.org/10.1016/j.cpr.2012.02.004
- Roskam, I., Raes, M. E., & Mikolajczak, M. (2017). Exhausted parents: Development and preliminary validation of the parental burnout inventory. Frontiers in Psychology, 8, 163. https://doi.org/10.3389/fpsyg.2017.00163
- Ruskin, D., Young, M., Sugar, C., & Nofech-Mozes, J. (2021). Mindfulness and acceptance interventions for parents of children and adolescents diagnosed with chronic medical conditions: A systematic review. The Journal of Alternative and Complementary Medicine, 27(2), 120–135. https://doi.org/10.1089/acm.2020.0191
- Sairanen, E., Lappalainen, R., Lappalainen, P., Kaipainen, K., Carlstedt, F., Anclair, M., & Hiltunen, A. (2019). Effectiveness of a web-based acceptance and commitment therapy intervention for wellbeing of parents whose children have chronic conditions: A randomized controlled trial. Journal of Contextual Behavioral Science, 13, 94–102. https://doi.org/10.1016/j.jcbs.2019.07.004
- Yu, Y., McGrew, J. H., & Boloor, J. (2019). Effects of caregiver-focused programs on psychosocial outcomes in caregivers of individuals with ASD: A meta-analysis. Journal of Autism and Developmental Disorders, 49(12), 4761–4779. https://doi.org/10.1007/s10803-019-04181-z
- Trompetter, H. R., Bohlmeijer, E. T., Veehof, M. M., & Schreurs, K. M. (2015). Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: A randomized controlled trial. Journal of Behavioral Medicine, 38(1), 66–80. https://doi.org/10.1007/s10865-014-9579-0
- Whittingham, K. (2014). Parents of children with disabilities, mindfulness and acceptance: A review and a call for research. Mindfulness, 5(6), 704–709. https://doi.org/10.1007/s12671-013-0224-8