ABSTRACT
Objectives
Motor functional neurological disorder (mFND) is a condition where individuals may experience difficulties such as tremors, gait impairments, and paralysis which are not explained by identified structural damage to the brain. Studies on chronic conditions have suggested that psychological interventions such as compassion-focused therapy (CFT) may be effective in improving well-being in people with mFND. However, no evidence is currently available on psychotherapy for older people with mFND.
Methods
A 12-session CFT intervention was delivered to an 81-year-old British male with mFND. Standardized measures were administered at baseline and post-intervention.
Results
At post-intervention, a 30% decrease in perceived psychological impact of mFND was found, along with clinically significant changes in anxiety and depression. Good levels of feasibility and acceptability were also observed.
Conclusions
To our knowledge, this is the first evidence of the feasibility, acceptability, and potential effectiveness of CFT for psychological difficulties linked with mFND, as well as the first evidence for any psychotherapy with an older adult with mFND.
Clinical Implications
CFT shows the potential to be effective, feasible, and acceptable for treating difficulties linked with mFND in older people. However, further high-quality investigations based on experimental designs are needed to build on the present preliminary findings.
Introduction
Functional neurological disorder (FND) is a condition where individuals experience neurological signs and symptoms which are not explained by any identified structural damage to the brain (Garcin, Citation2018). Traditionally considered purely psychogenic (Forejtová et al., Citation2022), in the past few decades FND has started to be conceptualized as underlain by a complex intersection of psychological factors with alterations in the way brain networks function (Hallett et al., Citation2022) – i.e., an issue of “software” rather than “hardware” (Stone, Burton, & Carson, Citation2020). Currently, FND is estimated to represent over 15% of all referrals to neurology (Stone et al., Citation2010) with an annual incidence of 12 in 100,000 worldwide (Bennett et al., Citation2021).
A number of different presentations of FND have also been identified (Hallett et al., Citation2022). Of these, the two most common are functional seizures (i.e., not associated with epileptiform evidence in the electroencephalogram; Asadi-Pooya, Brigo, Mildon, & Nicholson, Citation2020) and motor functional neurological disorder (mFND, also known as “functional movement disorder”), whereby people experience medically unexplained motor difficulties including tremors, gait impairments, and paralysis. mFND is thought to represent up to 3% of all movement disorders (Batla et al., Citation2013) and often poses a diagnostic challenge due to its similarity with the clinical manifestations of neurological diseases of both young and old age, such as multiple sclerosis and Parkinson’s (Hallett et al., Citation2022; Walzl, Solomon, & Stone, Citation2022). Similarly, these manifestations can often translate into a number of disabling impairments which impact the quality of life of affected individuals just as severely as nonfunctional conditions (Garcin, Citation2018). For instance, basic everyday activities such as cooking, driving, or working can be made progressively unfeasible (whether partially or completely) by the motor difficulties experiences by people with mFND, and often require input from Occupational Therapists (Nicholson et al., Citation2020).
Despite its similarity with some conditions typical of old age, mFND has been traditionally considered uncommon in older people – particularly in the older male population, in which it is often unrecognized or misdiagnosed (Stone et al., Citation2020). However, while current research has been mostly focusing on younger populations (Harris, Citation2019; Hull, Parnes, & Jankovic, Citation2021), recent evidence has shown that mFND may be just as frequent in older adults (Chouksey & Pandey, Citation2019), with up to one in five patients experiencing the onset of motor difficulties after age 60 (Batla et al., Citation2013).
A number of psychological interventions such as cognitive-behavioral therapy (CBT) and psychodynamic psychotherapy have been investigated with people with functional seizures in recent years, showing positive results (for a meta-analysis, see Carlson & Nicholson Perry, Citation2017). However, the evidence on psychological approaches for mFND is much sparser, with the latest systematic review (Gutkin, McLean, Brown, & Kanaan, Citation2021) identifying only three studies addressing it specifically – all reporting promising findings for either CBT (Dallocchio, Tinazzi, Bombieri, Arnó, & Erro, Citation2016) or short-term dynamic psychotherapy (Hinson, Weinstein, Bernard, Leurgans, & Goetz, Citation2006; Kompoliti, Wilson, Stebbins, Bernard, & Hinson, Citation2014), yet none involving older populations.
This is a considerable gap in the literature, not only due to the aforementioned disabling impact of mFND (comparable to nonfunctional neurological conditions; (O’Connell, Nicholson, Wessely, & David, Citation2020), but also because psychological interventions can successfully address difficulties such as shame, stigma, and social isolation (Eccles et al., Citation2021; Eccles, Sowter, Spokes, Zarotti, & Simpson, Citation2022) – which may be even more prevalent in people with mFND (Macduffie et al., Citation2021; Myers, Gray, Roberts, Levita, & Reuber, Citation2022). In this regard, the literature on functional seizures, chronic conditions, and nonfunctional neurological diseases appear to suggest that psychotherapeutic approaches based on self-compassion – such as compassion-focused therapy (CFT), an integrative model which aims to reduce shaming through compassion (Gilbert, Citation2010, Citation2014) – may represent a successful avenue for people with mFND (Collins, Gilligan, & Poz, Citation2018; Myers et al., Citation2022; Zarotti et al., Citation2022).
In particular, early conceptualizations of hysteria, somatization, or functional motor conditions – dating back to Freud in the late 19th century – formulated the extent of the emotional distress as being too great to be tolerated at a conscious level, resulting in its “conversion” into physical impairments (Kanaan, Citation2016). Although not unique to this approach, CFT differentiates somewhat from other psychotherapies such as traditional CBT in the ways it first works on the conditions that enable emotional distress to be tolerated sufficiently to bring it to conscious awareness, before then applying additional behavioral, physiological, and cognitive techniques to enable change (Gilbert, Citation2009). This includes working with attachment history to enable access to social safeness and deliberately creating compassionate brain states, for example through compassionate imagery (Gilbert, Citation2010). Further key CFT components for distress tolerance include facilitating “body and mind” work (i.e., Compassionate Mind Training or CMT; Gilbert, Citation2022a, p. 273) and understanding and accepting the “tricky brain,” paired with a commitment to take responsibility to alter unintentionally unhelpful processes (Gilbert & Simos, Citation2022b, p. 79).
Considering the predominant focus on physical dysfunction and the search for a potential cause that is often observed in people with mFND (Garcin, Citation2018; Nielsen, Buszewicz, Edwards, & Stevenson, Citation2020), CFT appears to represent a conceptually appropriate therapeutic avenue for this population. In addition, it may be considered particularly appropriate for older individuals specifically, who not only have been long recognized as the target of higher levels of stigmatization (Graham et al., Citation2003), shaming (Gullette, Citation2017), and social isolation (Cotterell, Buffel, & Phillipson, Citation2018), but may also struggle at times with the cognitive flexibility required by therapies such as CBT (Gould, Coulson, & Howard, Citation2012). This view is also complemented by the evidence that CFT is acceptable in older people (McConnell, Citation2021) – including those with additional neurocognitive decline (Collins et al., Citation2018; Craig, Hiskey, Royan, Poz, & Spector, Citation2018; Poz, Citation2018) – and that compassion plays a pivotal role in both the psychological and physical well-being and quality of life of older adults (Allen, Goldwasser, & Leary, Citation2012; Homan, Citation2016; Tavares, Vagos, & Xavier, Citation2020).
Despite all of the above, to our knowledge no investigation has so far explored the adoption of CFT nor any other psychotherapies with older populations with mFND. As a consequence, in this study we illustrate the case of an older adult with mFND who was successfully treated with 12 weeks of CFT.
Methods
Case presentation and initial assessment
AlbertFootnote1 was an 81-year-old white British male living in England with his wife. Five years previously he started losing strength in his legs and had experienced walking problems since then. Following several medical examinations, all of which returned normal results, Albert was eventually diagnosed with mFND and referred to the local Older People’s Psychology Service due to low mood.
During the initial assessment, Albert explained that his legs would suddenly stop working without any specific trigger, often in the middle of social situations, leaving him unable to stand or walk. While his mobility would mostly return after hours or days, these episodes caused Albert to feel ashamed and embarrassed, and led him to avoid social gatherings and stay at home. Here he would spend his time feeling depressed, demoralized, and guilty – particularly due to the inability to enjoy his retirement with his wife by going out for meals, plan holidays, or attend social gatherings with friends in general. These feelings were also reinforced by Albert’s struggle to understand and explain his condition to others, which he believed had led a number of friends and healthcare professionals to suggest that he was “faking it.”
Personal history
Albert reported a good childhood, with a decent relationship with his parents and siblings and no major traumatic experiences. However, he mentioned never feeling the need to have his family around throughout his life, and not maintaining a close relationship with his siblings after the death of their parents. He remembered being taught to always keep a “stiff upper lip” in life, since “big boys don’t cry.” This belief was also rooted in some early life episodes, in which he wet his bed at age four and was bitten by a dog he was playing with at age seven. In both instances, Albert recalled being scolded and punished for his behavior, and feeling ashamed after being told that he deserved his punishment and was not supposed to complain.
In his adult years, Albert enjoyed a satisfying career in construction until his retirement. He had three children, with whom he shared a very good relationship. However, he also reported a history of severe depression predating his mFND onset by 20 years, treated unsuccessfully with electro-convulsive therapy, for which he felt he had often struggled to seek help due to feeling ashamed. This appeared to extend to other areas of Albert’s life as well, as both he and his wife felt that he was often reluctant to express his emotions or ask for help in their daily life.
Case formulation
Albert’s psychological difficulties were conceptualized using the CFT framework (Gilbert & Simos, Citation2022c), an integrative biopsychosocial approach combining elements of cognitive therapy, evolutionary psychology, neurobiology, and Buddhist philosophy which aims to reduce shame and improve psychological well-being by developing compassion (Collins et al., Citation2018). From this perspective, Albert’s early experiences of shame were seen as paving the way to the development of perceptions of self and others based on feelings of punishment, judgment, and distrust. As he grew up, these led to a number of key fears and threats about other people and himself. Over time, Albert’s attempts to cope, influenced by his emotional shame memories, led him to get stuck in a vicious circle in which other people were not seen as sources of comfort and safeness, but as threats in themselves.
Based on the fundamental evolutionary responses to threats (i.e., “fight,” “flight,” or “freeze”; Gilbert, Citation2010), it was hypothesized that Albert’s mFND was a manifestation of a “freeze” response, with his brain taking the “low road” or “quick and dirty route” – i.e., a fast subcortical pathway which directly connects the thalamus to the amygdala, bypassing the neocortex and thus bypassing individual control via higher cognitive functions (LeDoux, Citation1998, Citation2000). In turn, this triggered the development of several external and internal safety behaviors based on avoidance, lack of self-compassion, and reluctance to seek help, which led him to experience unintended negative consequences (e.g., isolation) and strong self-critical views (e.g., “I should be ashamed”). Ultimately, these elements also appeared to exacerbate Albert’s worries about mFND, for which he felt further shamed by hospital staff who “dismissed” his symptoms, thus reinforcing the vicious circle itself. presents an illustration of Albert’s case formulation.
Intervention
Albert’s wish for therapy was to find out why his “brain was saying don’t move,” reduce mFND’s impact on his daily mood and anxiety, and improve his ability to seek help without feeling shame. As a consequence, a plan for a CFT intervention informed by Gilbert’s framework (Citation2010) was discussed and agreed with him. More specifically, based on the abovementioned “freeze” response hypothesis, the intervention was focused on bringing Albert’s emotional triggers into his conscious awareness, providing him with new strategies to regulate his emotions (Gilbert, Citation2014, p. 14). This was aimed at enabling the option of the “high road” or “slower route” for his brain – i.e., a less impulsive pathway which connects the thalamus to the neocortex first and only then to the amygdala, effectively allowing for the conscious processing of stimuli (LeDoux, Citation1998). Elements of psychoeducation and problem-focused strategies, considered integral to CFT (Gilbert & Simos, Citation2022a, p. 79), were included in the intervention (Tolin, Citation2016, p. 193).
Outcome measures
As recommended by the latest systematic review on the topic (Nicholson et al., Citation2020), an individualized approach based on a patient-generated outcome measure was adopted for this case study. More specifically, since no standardized measure is currently available for the psychological impact of mFND, Albert’s perceived impact of mFND across the intervention was monitored with the Psychological Outcome Profiles (PSYCHLOPS; Ashworth et al., Citation2004), a short questionnaire which allows patients to define each item according to their own specific mental health difficulties, whose impact is then measured on a 5-point Likert scale. The Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, Citation1983) was also chosen to measure Albert’s difficulties with anxiety and low mood, while his levels of self-compassion were monitored with the Self-Compassion Scale (SCS; Neff, Citation2016). All measures were administered at baseline and post-intervention.
Results
Course of treatment
Albert’s treatment consisted of 12 weekly 1-hour sessions, delivered face-to-face by NZ while on clinical training under the supervision of RP.
Sessions 1-2
The first two sessions were dedicated to exploring Albert’s personal history and practising a number of CMT skills including soothing rhythm breathing (SRB), imagery (Gilbert & Simos, Citation2022a, pp. 284–285; Neff & Germer, Citation2018, p. 46) and self-compassion breaks (Neff & Germer, Citation2018, p. 34). These aimed to provide Albert with some novel coping techniques to deal with everyday feelings of overwhelming anxiety and low mood triggered by mFND, whilst also promoting his tolerance of self-compassion and interpersonal connections. CMT techniques were practised in each session thereafter and recordings were left with Albert to practise on his own while also promoting a collaborative approach with his wife by inviting them to practise together.
Sessions 3-5
These sessions were dedicated to psychoeducation around the brain, FND and its potential explanations, and the rationale for CFT. Resources from FND Hope International (ww.fndhope.org/living-fnd/healthy-living) and Compassionate Mind Australia (www.compassionatemind.org.au/practitioner-tools) were adopted to facilitate this process. However, since Albert’s natural strategy was to avoid confrontation even with his own emotions, efforts were made to avoid overreliance on cognitive components such as psychoeducation. In particular, he was reorientated to his memories of being well cared for to enable him to connect with his own physiological experiences of compassion and replicate them more often. (Gilbert, Citation2022a, pp. 112–113, 298–304). This further developed the therapeutic relationship and allowed Albert to see therapy as a safe haven from his key fears about the external world (Gilbert, Citation2022a, pp. 388–389).
Session 6
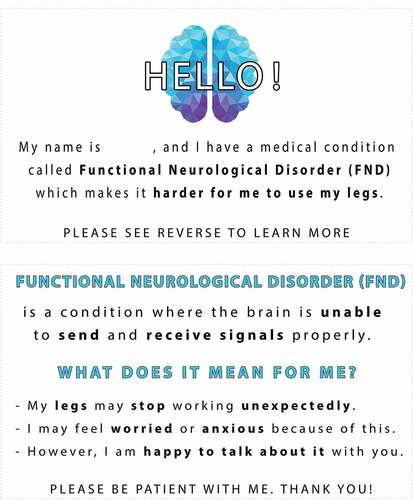
This session drew on an incident whereby the previous weekend Albert had suddenly lost the use of his legs while in public with friends – causing significant shame and embarrassment. This experience was used as a real-life example to explore the concepts of shame, humiliation, and guilt more in detail, and their impact on his social life (Gilbert, Citation2022b, p. 122). A problem-focused approach to avoid similar episodes and enhance social cohesion and acceptance was also agreed (Tolin, Citation2016, p. 292), particularly in the form of an mFND Info Card () which Albert could carry and show to people on necessary occasions. Examples of these included meeting new people, answering questions from friends, and advising staff at specific venues in case he felt he could have motor difficulties (e.g., restaurant waiters). Within a CFT conceptualization, this process also builds the wisdom and ability to balance self-care and self-regulation, with being open to and seeking the help of others; meeting that human evolved need for interpersonal comfort.
Sessions 7-9
Throughout these sessions, the formulation model was shared and discussed with Albert, and linked with the elements explored in Sessions 3–5, such as brain functioning, the psychological impact of mFND, and his memories of being well cared for. Albert mentioned not having the right to be self-compassionate (Neff & Germer, Citation2018, p. 40), which enabled an exploration of his fears, blocks, and resistances (FBRs) to compassion (Gilbert & Simos, Citation2022b, p. 207).
Sessions 10-12
The last three sessions were dedicated to the consolidation and further development of CMT (Gilbert, Citation2022a, p. 273). More specifically, continuing to explore using the body to support a compassionate mind through posture and breathing (Gilbert & Simos, Citation2022a, pp. 284–285) discussing Multiple Selves (Gilbert, Citation2022a, p. 316), and highlighting Albert’s right to self-compassion, to have his needs met, and to seek help if needed (Neff & Germer, Citation2018, p. 40). In the last session, elements of psychoeducation on FND were reviewed again to enhance feelings of validation (Gilbert, Citation2022a, p. 328).
Outcome
Albert’s results on the outcome measures across the intervention are listed in and illustrated in . At the end of therapy, improvements were observed for all outcomes. Albert’s perceived psychological impact of mFND, as measured by the PSYCHLOPS score, decreased from 19 to 13. While the patient-generated nature of the tool did not allow for the calculation of a Reliable Change Index (i.e., whether the change is sufficiently large to exclude variation related to measurement unreliability; Jacobson & Truax, Citation1991), this score difference represented a 30% decrease against the PSYCHLOPS’ maximum score of 20.
Table 1. Albert’s scores on all outcome measures across the intervention.
Figure 3. Overview of Albert’s scores on all outcome measures.
Similarly, at baseline Albert’s levels of anxiety (HADS_A = 8) and depression (HADS_D = 10) placed him within the clinically significant range (cutoff = 8/21; Bjelland, Dahl, Haug, & Neckelmann, Citation2002). At post-intervention, both scores fell below this threshold, showing a clinically significant change (Jacobson & Truax, Citation1991), with depression also showing a reliable change (RCI = 2.34). Finally, a slight improvement was also observed for Albert’s levels of self-compassion, although with no reliable change (RCI = −0.44).
Acceptability
Based on Albert’s comments throughout the sessions, the intervention appeared to be acceptable for him. More specifically, he expressed particular appreciation for the increased feelings of validation felt during and after the psychoeducation sessions (“I like being told about what I have in a positive way”), as well as the reduced stigma and increased social engagement linked to using the Info Card (“It’s a relief to know that someone believes me!”). He also found comfort in breathing exercises (“Now I know I can breathe when I’m feeling low”), and experienced increased sense of worth and received-compassion (“It’s helpful when people care about how I’m doing”). While no clear improvements were observed in Albert’s motor abilities, by the end of therapy he showed higher levels of acceptance (“I’ve more or less accepted what I’ve got”) and a more positive attitude (“Maybe I’ll get better if I’m positive”). This translated into a number of practical improvements in his daily functioning and coping – e.g., spending meaningful time with his wife practising CFT exercises (“We’ve been doing some of the breathing together”), changing his goals when attending social gatherings (“I might not be able to play bowls, but I’m going to meet my mates there anyway”), or accepting alternative ways to work around his physical limitations (“I’m giving up driving and going to get a mobility scooter, that’ll work just fine”).
Discussion
The present case study reported the adoption of a compassion-focused intervention for an 81-year-old man with mFND (“Albert”). To our knowledge, this is the first report on the implementation and delivery of CFT in a person with this condition, and the first investigation of any psychotherapy with an older adult with mFND. The results showed the intervention to be feasible and acceptable, and effective in decreasing Albert’s perceived psychological impact of mFND by 30%, while also reducing his anxiety and depression to non-clinical levels and leading to a number of functional daily improvements. These findings are consistent with previous studies highlighting how compassion-focused interventions can be feasible, acceptable, and effective in improving mental health and reducing distress in older people (Perez-Blasco, Sales, Meléndez, & Mayordomo, Citation2016) – especially those living with a chronic condition (Birdsey, Citation2020; Collins et al., Citation2018).
A small increase in feelings of self-compassion, as measured by the SCS, was also observed in Albert, although it did not represent a reliable change. While this may appear unexpected in an intervention focused on compassion, it should be noted that – unlike more narrowly targeted programmes, such as Mindful Self-Compassion (MSC; Germer & Neff, Citation2013) – self-compassion represents only one of the dimensions of compassion which are addressed by CFT (Gilbert, Citation2010, p. 159). Moreover, the development of a more compassionate self has sometimes been observed to occur via an “outside-in” path, through which “people develop social trust, gratitude, to be open to the compassion of others and be compassionate to others,” so that “it is in this flow that the healing of the self occurs” (Gilbert, Citation2022a, p. 306). Thus, a longer therapy course and additional more comprehensive measures covering multiple components of the flow of compassion (e.g., Fears of Compassion Scales; Kirby, Day, & Sagar, Citation2019) may be necessary for more reliable changes to be observed in this construct.
Limitations
A number of limitations should be considered along with the present results. First, the nature of single case studies, along with the absence of comparisons with other treatments or an untreated control, prevents any form of generalization of our evidence. Moreover, no follow-up sessions were carried out with Albert after 12 weeks. While this adhered to the minimum number of sessions indicated to achieve therapeutic impact with CFT (Craig, Hiskey, & Spector, Citation2020), the trajectory of Albert’s improvements over time remains unclear, particularly around his feelings of self-compassion and their interaction with other dimensions of compassion. Therefore, further high-quality investigations, based on experimental designs adopting longer therapy courses and additional measures of compassion, are needed in the future to build on the preliminary findings observed in this study.
Clinical implications
Psychotherapies focused on compassion have shown to be effective with people with chronic conditions, yet no evidence is currently available for older people with motor functional neurological disorder (mFND).
In this study, a 12-session compassion-focused intervention was effective in improving the psychological impact of mFND clinical levels of anxiety and depression in an 81-year-old man.
Psychoeducation, breathing exercises, reduction of stigma through validation, interpersonal connection, and problem-focused strategies to prevent shaming appeared feasible and acceptable, although further high-quality longitudinal investigations are needed to build on these preliminary findings.
Ethical principles
The authors affirm having followed professional ethical guidelines in preparing this work. These guidelines include obtaining informed consent from human participants, maintaining ethical treatment and respect for the rights of human or animal participants, and ensuring the privacy of participants and their data, such as ensuring that individual participants cannot be identified in reported results or from publicly available original or archival data.
Data availability
Due to the nature of this work, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1. The name has been changed to preserve anonymity.
References
- Allen, A. B., Goldwasser, E. R., & Leary, M. R. (2012). Self-compassion and well-being among older adults. Self and Identity, 11(4), 428–453. doi:10.1080/15298868.2011.595082
- Asadi-Pooya, A. A., Brigo, F., Mildon, B., & Nicholson, T. R. (2020). Terminology for psychogenic nonepileptic seizures: Making the case for “functional seizures.” Epilepsy & Behavior, 104, 106895. https://doi.org/10.1016/j.yebeh.2019.106895
- Ashworth, M., Shepherd, M., Christey, J., Matthews, V., Wright, K., Parmentier, H., … Godfrey, E. (2004). A client-generated psychometric instrument: The development of. ‘PSYCHLOPS.’ Counselling and Psychotherapy Research, 4(2), 27–31. doi:10.1080/14733140412331383913
- Batla, A., Stamelou, M., Edwards, M. J., Pareés, I., Saifee, T. A., Fox, Z., & Bhatia, K. P. (2013). Functional movement disorders are not uncommon in the elderly. Movement Disorders, 28(4), 540–543. doi:10.1002/mds.25350
- Bennett, K., Diamond, C., Hoeritzauer, I., Gardiner, P., McWhirter, L., Carson, A., & Stone, J. (2021). A practical review of functional neurological disorder (FND) for the general physician. Clinical Medicine, Journal of the Royal College of Physicians of London, 21(1), Royal College of Physicians, 28–36. doi:10.7861/CLINMED.2020-0987
- Birdsey, N. (2020). Integrating CBT and CFT within a case formulation approach to reduce depression and anxiety in an older adult with a complex mental and physical health history: A single case study. Cognitive Behaviour Therapist, 13. doi:10.1017/S1754470X20000410
- Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale: An updated literature review. Journal of Psychosomatic Research, 52(2), 69–77. doi:10.1016/S0022-3999(01)00296-3
- Carlson, P., & Nicholson Perry, K. (2017). Psychological interventions for psychogenic non-epileptic seizures: A meta-analysis. Seizure, 45, 142–150. doi:10.1016/j.seizure.2016.12.007
- Chouksey, A., & Pandey, S. (2019). Functional movement disorders in elderly. Tremor and Other Hyperkinetic Movements, 9, 1–6. doi:10.7916/tohm.v0.691
- Collins, R. N., Gilligan, L. J., & Poz, R. (2018). The evaluation of a compassion-focused therapy group for couples experiencing a dementia diagnosis. Clinical Gerontologist, 41(5), 474–486. doi:10.1080/07317115.2017.1397830
- Cotterell, N., Buffel, T., & Phillipson, C. (2018). Preventing social isolation in older people. Maturitas, 113, 80–84. Elsevier Ireland Ltd. doi:10.1016/j.maturitas.2018.04.014
- Craig, C., Hiskey, S., Royan, L., Poz, R., & Spector, A. (2018). Compassion focused therapy for people with dementia: A feasibility study. International Journal of Geriatric Psychiatry, 33(12), 1727–1735. doi:10.1002/gps.4977
- Craig, C., Hiskey, S., & Spector, A. (2020). Compassion focused therapy: A systematic review of its effectiveness and acceptability in clinical populations. Expert Review of Neurotherapeutics, 20(4), Taylor and Francis Ltd, 385–400. doi:10.1080/14737175.2020.1746184
- Dallocchio, C., Tinazzi, M., Bombieri, F., Arnó, N., & Erro, R. (2016). Cognitive behavioural therapy and adjunctive physical activity for functional movement disorders (Conversion Disorder): A pilot, single-blinded, randomized study. Psychotherapy and Psychosomatics, 85(6), S. Karger AG, 381–383. doi:10.1159/000446660
- Eccles, F. J. R., Craufurd, D., Smith, A., Davies, R., Glenny, K., Homberger, M., … Simpson, J. (2021). Experiences of mindfulness-based cognitive therapy for premanifest Huntington’s disease. Journal of Huntington’s Disease, 10(2), 277–291. doi:10.3233/JHD-210471
- Eccles, F. J. R., Sowter, N., Spokes, T., Zarotti, N., & Simpson, J. (2022). Stigma, self-compassion, and psychological distress among people with Parkinson’s. Disability and Rehabilitation, 1–9. doi:10.1080/09638288.2022.2037743
- Forejtová, Z., Serranová, T., Sieger, T., Slovák, M., Nováková, L., Věchetová, G., … Edwards, M. J. (2022). The complex syndrome of functional neurological disorder. Psychological Medicine, 1–11. doi:10.1017/S0033291721005225
- Garcin, B. (2018). Motor functional neurological disorders: An update. Revue Neurologique, 174(4), 203–211. doi:10.1016/j.neurol.2017.11.003
- Germer, C. K., & Neff, K. D. (2013). Self-compassion in clinical practice. Journal of Clinical Psychology, 69(8), 856–867. doi:10.1002/jclp.22021
- Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15(3), 199–208. doi:10.1192/apt.bp.107.005264
- Gilbert, P. (2010). Compassion focussed therapy: Distinctive features. London: Routledge.
- Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. doi:10.1111/bjc.12043
- Gilbert, P. (2022a). Compassionate mind training. In Paul Gilbert, Gregoris Simos (eds.), Compassion focused therapy (pp. 273–312). New York: Routledge. doi:10.4324/9781003035879-10
- Gilbert, P. (2022b). Shame, humiliation, guilt, and social status. In Paul Gilbert, Gregoris Simos (eds.), Compassion focused therapy (pp. 122–163). New York: Routledge. doi:10.4324/9781003035879-5
- Gilbert, P., & Simos, G. (2022a). Compassion focused therapy: Clinical practice and applications. New York: Routledge.
- Gilbert, P., & Simos, G. (2022b). Compassion focused therapy. In Compassion focused therapy (pp. 24–89). New York: Routledge. doi:10.4324/9781003035879-3
- Gilbert, P., & Simos, G. (2022c). Formulation and fears, blocks, and resistances. In Paul Gilbert, Gregoris Simos (eds.), Compassion focused therapy (pp. 207–239). New York: Routledge. doi:10.4324/9781003035879-7
- Gould, R. L., Coulson, M. C., & Howard, R. J. (2012). Efficacy of cognitive behavioral therapy for anxiety disorders in older people: A meta-analysis and meta-regression of randomized controlled trials. Journal of the American Geriatrics Society, 60(2), 218–229. doi:10.1111/j.1532-5415.2011.03824.x
- Graham, N., Lindesay, J., Katona, C., Bertolote, J. M., Camus, V., Copeland, J. R. M., … Chiu, E. (2003). Reducing stigma and discrimination against older people with mental disorders: A technical consensus statement. International Journal of Geriatric Psychiatry, 18(8), 670–678. doi:10.1002/gps.876
- Gullette, M. M. (2017). Ending ageism, or how not to shoot old people. New Brunswick, NJ: Rutgers University Press. https://doi.org/10.2307/j.ctt1q1cqsm
- Gutkin, M., McLean, L., Brown, R., & Kanaan, R. A. (2021). Systematic review of psychotherapy for adults with functional neurological disorder. Journal of Neurology, Neurosurgery and Psychiatry, 92(1), 36–44. doi:10.1136/jnnp-2019-321926
- Hallett, M., Aybek, S., Dworetzky, B. A., McWhirter, L., Staab, J. P., & Stone, J. (2022). Functional neurological disorder: New subtypes and shared mechanisms. The Lancet Neurology, 21(6), 537–550. doi:10.1016/S1474-4422(21)00422-1
- Harris, S. R. (2019). Psychogenic movement disorders in children and adolescents: An update. European Journal of Pediatrics, 178(4), 581–585. doi:10.1007/s00431-019-03317-8
- Hinson, V. K., Weinstein, S., Bernard, B., Leurgans, S. E., & Goetz, C. G. (2006). Single-blind clinical trial of psychotherapy for treatment of psychogenic movement disorders. Parkinsonism and Related Disorders, 12(3), 177–180. doi:10.1016/j.parkreldis.2005.10.006
- Homan, K. J. (2016). Self-Compassion and psychological well-being in older adults. Journal of Adult Development, 23(2), 111–119. doi:10.1007/s10804-016-9227-8
- Hull, M., Parnes, M., & Jankovic, J. (2021). Increased incidence of functional (Psychogenic) movement disorders in children and adults amid the COVID-19 Pandemic. Neurology: Clinical Practice, 11(5), e686–e690. doi:10.1212/cpj.0000000000001082
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to denning meaningful change in psychotherapy research. Journal of Consulting Psychology, 59(1), 12–19. doi:10.7224/1537-2073.2013-007
- Kanaan, R. A. A. (2016). Freud’s hysteria and its legacy. In Mark Hallett, Jon Stone, Alan Carson (eds.)., Handbook of clinical neurology (Vol. 139, pp. 37–44). Oxford: Elsevier B.V. doi:10.1016/B978-0-12-801772-2.00004-7
- Kirby, J. N., Day, J., & Sagar, V. (2019). The ‘Flow’ of compassion: A meta-analysis of the fears of compassion scales and psychological functioning. Clinical psychology Review, 70, 26–39. https://doi.org/10.1016/j.cpr.2019.03.001
- Kompoliti, K., Wilson, B., Stebbins, G., Bernard, B., & Hinson, V. (2014). Immediate vs. delayed treatment of psychogenic movement disorders with short term psychodynamic psychotherapy: Randomized clinical trial. Parkinsonism and Related Disorders, 20(1), 60–63. doi:10.1016/j.parkreldis.2013.09.018
- LeDoux, J. (1998). The emotional brain: The mysterious underpinnings of emotional life. New York: Simon and Schuster.
- LeDoux, J. (2000). Cognitive–emotional interactions: Listen to the brain. In Richard D Lane, Lynn Nadel (eds.)., Cognitive neuroscience of emotion (pp. 129–155). New York: Oxford University Press.
- Macduffie, K. E., Grubbs, L., Best, T., Laroche, S., Mildon, B., Myers, L., … Rommelfanger, K. S. (2021). Stigma and functional neurological disorder: A research agenda targeting the clinical encounter. CNS Spectrums, 26(6), Cambridge University Press, 587–592. doi:10.1017/S1092852920002084
- McConnell, F. (2021). Compassion focused therapy: Exploring mechanisms of change and investigating the feasibility of a transdiagnostic group for older adults [DClinPsy thesis]. University of Glasgow.
- Myers, L., Gray, C., Roberts, N., Levita, L., & Reuber, M. (2022). Shame in the treatment of patients with psychogenic nonepileptic seizures: The elephant in the room. Seizure, 94(July2021), 176–182. doi:10.1016/j.seizure.2021.10.018
- Neff, K. D. (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. doi:10.1007/s12671-015-0479-3
- Neff, K., & Germer, C. (2018). The mindful self-compassion workbook: A proven way to accept yourself, build inner strength, and thrive. New York: Guilford Publications.
- Nicholson, C., Edwards, M. J., Carson, A. J., Gardiner, P., Golder, D., Hayward, K., … Stone, J. (2020). Occupational therapy consensus recommendations for functional neurological disorder. Journal of Neurology, Neurosurgery and Psychiatry, 91(10), 1037–1045. doi:10.1136/jnnp-2019-322281
- Nicholson, T. R., Carson, A., Edwards, M. J., Goldstein, L. H., Hallett, M., Mildon, B., Nielsen, G., Nicholson, C., Perez, D. L., Pick, S., Stone, J., Anderson, D., Asadi-Pooya, A., Aybek, S., Baslet, G., Bloem, B. R., Brown, R. J., Chalder, T., Damianova, M., … Tinazzi, M. (2020). Outcome Measures for Functional Neurological Disorder: A Review of the Theoretical Complexities. The Journal of Neuropsychiatry and Clinical Neurosciences, 32(1), 33–42. https://doi.org/10.1176/appi.neuropsych.19060128
- Nielsen, G., Buszewicz, M., Edwards, M. J., & Stevenson, F. (2020). A qualitative study of the experiences and perceptions of patients with functional motor disorder. Disability and Rehabilitation, 42(14), 2043–2048. doi:10.1080/09638288.2018.1550685
- O’Connell, N., Nicholson, T. R., Wessely, S., & David, A. S. (2020). Characteristics of patients with motor functional neurological disorder in a large UK mental health service: A case-control study. Psychological Medicine, 50(3), 446–455. doi:10.1017/S0033291719000266
- Perez-Blasco, J., Sales, A., Meléndez, J. C., & Mayordomo, T. (2016). The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clinical Gerontologist, 39(2), 90–103. doi:10.1080/07317115.2015.1120253
- Poz, R. (2018). Facing degeneration with compassion on your side: Using compassion focused therapy with people with a diagnosis of a dementia *. In Eastern influences on neuropsychotherapy (pp. 121–142). New York: Routledge. doi:10.4324/9780429466618-5
- Stone, J., Burton, C., & Carson, A. (2020). Recognising and explaining functional neurological disorder. The BMJ, 371. doi:10.1136/bmj.m3745
- Stone, J., Carson, A., Duncan, R., Roberts, R., Warlow, C., Hibberd, C., … Sharpe, M. (2010). Who is referred to neurology clinics? - The diagnoses made in 3781 new patients. Clinical Neurology and Neurosurgery, 112(9), 747–751. doi:10.1016/j.clineuro.2010.05.011
- Tavares, L., Vagos, P., & Xavier, A. (2020). The role of self-compassion in the psychological (mal)adjustment of older adults: A scoping review. International Psychogeriatrics, 1-14. doi:10.1017/S1041610220001222
- Tolin, D. F. (2016). Doing CBT: A comprehensive guide to working with behaviors, thoughts, and emotions. New York: Guilford Press.
- Walzl, D., Solomon, A. J., & Stone, J. (2022). Functional neurological disorder and multiple sclerosis: A systematic review of misdiagnosis and clinical overlap. Journal of Neurology, 269(2), Springer Science and Business Media Deutschland GmbH, 654–663. doi:10.1007/s00415-021-10436-6
- Zarotti, N., Eccles, F., Broyd, A., Longinotti, C., Mobley, A., & Simpson, J. (2022). Third wave cognitive behavioural therapies for people with multiple sclerosis: A scoping review. Disability and Rehabilitation, 1–16. doi:10.1080/09638288.2022.2069292
- Zigmond, A. S., & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi:10.1111/j.1600-0447.1983.tb09716.x