?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Objectives
As the aging population increases, it is critical to find ways to sustain older adults’ health and well-being. Mindfulness-Based Stress Reduction (MBSR) may be one approach, but its effects are difficult to discern because few studies have conducted randomized controlled trials with an active control group and blinded examiners. We begin to address these gaps with a pilot study examining the feasibility of conducting an MBSR intervention with an active control condition in healthy older adults.
Methods
Participants were randomly assigned to one of two classes, MBSR or Brain Health education. Classes were matched for time, format, and instructor. The study examined acceptability, practicality, implementation, and preliminary efficacy using a range of participant questionnaires, instructor ratings, cognitive measures assessed by blinded examiners, and attendance.
Results
Both MBSR and the Brain Health class evidenced high rates of recruitment, participant satisfaction, and retention. Implementation procedures were successful, and preliminary results revealed similar levels of efficacy across both classes.
Conclusions
This study demonstrates the feasibility of an MBSR intervention in healthy older adults.
Clinical Implications
MBSR, with its focus on improving stress and self-awareness, has the potential to be an approach that can improve aging adults’ health and coping skills.
The aging population is growing rapidly, as the population of adults 60 years or older is over 50 million and anticipated to double worldwide by 2050 (World Health Organization, Citation2021; U.S. Census Bureau, Citation2020). With an increasing number of adults living into older age, the risk for cognitive impairment, Alzheimer’s disease, and related disorders is also on the rise (Perera et al., Citation2018). Given the cognitive deficits associated with older age and the associated declines in functional abilities and quality of life, a growing emphasis is being placed on facilitating brain health in older adults (Barnes & Yaffe, Citation2011; Krivanek, Gale, McFeeley, Nicastri, & Daffner, Citation2021)
One approach to optimizing brain health in older adults is to reduce factors that are known to be deleterious. For example, chronic stress exposure has been linked to neuronal injury and cognitive decline (Magri et al., Citation2006; Swan et al., Citation1998), suggesting that stress reduction may be particularly important for maintaining and improving cognitive health in older adults. One such potential intervention for reducing stress is Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, Citation1990). MBSR uses mindfulness techniques to teach people how to focus their attention on breathing and other bodily sensations, while observing their thoughts without judgment. This practice has been shown to reduce stress and improve coping and recovery in a variety of populations (Abbott et al., Citation2014; Azulay, Smart, Mott, & Cicerone, Citation2013; Bédard et al., Citation2014; Hofer et al., Citation2014; B. Johansson, Bjuhr, & Rönnbäck, Citation2012; Joo, Lee, Chung, & Shin, Citation2010; Medina & Mead, Citation2021). MBSR could be particularly advantageous for facilitating brain health in older adults, as late life can bring challenges that lead to chronic stress (e.g., loss of loved ones, health declines), which may further increase older adults’ risk for cognitive decline (Gerritsen et al., Citation2017; L. Johansson et al., Citation2013). Teaching MBSR to older adults could thus positively impact their functioning through a low-risk and low-cost intervention.
Previous studies have demonstrated the potential positive effects of mindfulness and MBSR interventions in older adults, including an improvement in overall well-being (Fiocco, Mallya, Farzaneh, & Koszycki, Citation2019; Mallya & Fiocco, Citation2016; Martin & Doswell, Citation2012; Moss et al., Citation2015), reduced depression, anxiety, and stress (Ahmadpanah et al., Citation2017; Foulk, Ingersoll-Dayton, Kavanagh, Robinson, & Kales, Citation2014; Lavretsky et al., Citation2013; M. Williams, Meeten, & Whiting, Citation2018; Mallya & Fiocco, Citation2019; Mathur, Sharma, & Bharath, Citation2016; Meeten, Whiting, & Williams, Citation2015; O’Connor, Piet, & Hougaard, Citation2014; Oken et al., Citation2017; Smith, Graham, & Senthinathan, Citation2007; Wetherell et al., Citation2017), and improved cognition (Berk, van Boxtel, & van Os, Citation2017; Lavretsky et al., Citation2013; Malinowski, Moore, Mead, & Gruber, Citation2017; Sun, Kang, Wang, & Zeng, Citation2013; Yu et al., Citation2021). However, few of these studies included an active control condition to compare to MBSR, and thus the specificity of the effects is unclear (see review by Hazlett-Stevens, Singer, & Chong, Citation2019). For example, Moynihan et al. (Citation2013) delivered MBSR to a community-dwelling sample of 201 adults over the age of 65, and results indicated that MBSR was associated with improvements in a measure of executive function and self-reported mindfulness, relative to controls. However, the control group in this study was passive (i.e., received no intervention), making it challenging to identify whether the basis for gains in cognitive functioning was specific to the MBSR intervention or due to nonspecific factors such as increased social interaction due to the nature of group participation. In another study examining MBSR relative to an active control group where older adults read and engaged in progressive muscle relaxation practices, results suggested that MBSR did not lead to changes on measures of cognition and well-being (Mallya & Fiocco, Citation2016). However, the overlap between the skills learned through MBSR and the active control group make it difficult to parse the benefits of the intervention. Thus, randomized controlled studies of MBSR with a distinct and active control arm are needed in order to understand whether MBSR is an effective tool for improving coping and functioning in healthy older adults.
Another omission in previous mindfulness studies is the lack of blinded examiners. Many studies either reported using a non-blinded examiner or did not state the status of their examiners (e.g., Lavretsky et al., Citation2013; O’Connor et al., Citation2014; Sun et al., Citation2013; Yu et al., Citation2021). Without adequate examiner blinding, results obtained from participants could be influenced by examiner expectancy biases, making it unclear whether mindfulness interventions have a demonstrable effect on cognition and other processes.
The present study aimed to address these gaps in the MBSR literature by conducting a randomized controlled pilot trial of MBSR with blinded examiners and an active control intervention (i.e., Brain Health education class). The two classes were matched with respect to time commitment and social and cognitive engagement. The primary focus of this pilot study was to examine the feasibility of conducting these two interventions with healthy older adults and using these preliminary data to inform a future randomized clinical trial with a larger sample (Arain, Campbell, Cooper, & Lancaster, Citation2010; Leon, Davis, & Kraemer, Citation2011; Thabane et al., Citation2010). We hypothesized that both interventions would be feasible based on the framework described by Bowen et al. (Citation2009): (1) acceptability – based on participant satisfaction and ratings of the intervention; (2) integration – based on whether participants report using intervention skills in their daily life; (3) implementation – based on how well the interventions were executed, including recruitment and the implementation of randomization and blinding; and (4) practicality – based on the ease and efficiency of delivering and participating in the interventions, including measures of attendance, retention, and participant engagement. We also hypothesized that MBSR would demonstrate greater preliminary efficacy compared to the Brain Health education class, as measured by outcome measures of cognition, mood, health, and well-being.
Methods
Participants
Sixty-two healthy research volunteers were enrolled at VA Northern California Health Care System. Participants were defined as healthy if they met study inclusion and exclusion criteria. Inclusion criteria for the study were 60–80 years of age and native English proficiency. Exclusion criteria were substantial visual/hearing impairment; score of <19 on the Mini-Mental State Examination (MMSE; Johansson et al., Citation2012); history of neurological illness (e.g., dementia, stroke, Parkinson’s disease, moderate/severe TBI); history of severe psychiatric illness (e.g., schizophrenia, bipolar disorder); recent substance abuse/dependence disorder (within 1 year); acutely suicidal; and concurrent involvement in another rehabilitation program. Participants’ medical history was attained through clinical interview and review of computerized medical records. Current active medications were recorded but were not used as an exclusionary factor.
Study participants were recruited through fliers posted at our VA medical center, review of VA medical records, and personal outreach using prior participant pools from our research group. Participants included Veterans who received care at our VA and older adults (non-Veterans) in the local community. A starting pool of approximately 750 VA records/participants were reviewed. Of these, approximately 65% were excluded due to having a neurological illness, severe psychiatric illness, acute suicidality, or recent substance use; 15% due to being outside the age range; and 10% due to lack of interest. In terms of ethnicity, the MBSR class included three Asian American participants, three Black participants, and 17 White participants, while the Brain Health class included six Black participants and 20 White participants (see for demographic data).
Table 1. Participant demographics.
Power analyses were derived from repeated sampling simulations based on planned linear-mixed models with our main efficacy outcome variables entered as dependent variables in the same model. With three assessments per person, alpha set at 0.05, and a 2-tailed test, a sample size of 24 participants per group was required to detect a small effect size (d = 0.04) with 85% power, assuming equal group sizes.
Procedures
Our study was approved by the VA Northern California Health Care System (VANCHCS) Institutional Review Board, which ensures that all procedures were conducted in concordance with the 1964 Helsinki Declaration. All participants provided written informed consent before completing the intervention at VANCHCS. Once enrolled, participants were randomized into one of the two 8-week classes (MBSR or Brain Health). In addition to participation in the class, participants also completed: 1) a pre-intervention test session, which occurred within two-weeks prior to the start of the class; 2) a post-intervention test session, which occurred within two weeks after the end of the class; and 3) a three-month follow-up session. The pre- and post-intervention test sessions included a neuropsychological battery and a set of questionnaires. The pre- and post-intervention test sessions were conducted by four clinical neuropsychologists who were blinded to participant assignment (MBSR vs. Brain Health). Participants were assessed by the same examiner across test sessions. During the post-intervention test session, an anonymous questionnaire assessing study acceptability was also included. At the three-month follow-up, only the questionnaires were completed (i.e., no neuropsychological tests) because the follow-up was conducted via mail. Participants were compensated for test sessions at the rate of $20/hour.
Randomization
Participants were randomly assigned to either the MBSR class or the Brain Health class. Randomization was completed by our study statistician, with age and gender as blocking factors (male vs. female and < 65 vs. ≥ 65). These randomized assignments were then marked and placed in sealed and numbered envelopes. Once participants provided consent (but before the start of any assessments or interventions), these envelopes were opened sequentially by study staff to assign participants to one of the classes.
Blinding
Participants were informed during the consent process that the study aim was to examine the effectiveness of two different Brain Health and Wellness classes being taught at VA and that they would be randomly assigned to one of these classes. A true double-blind trial was not possible because once participants attended their first class, the content of the intervention was apparent. However, in an effort to maintain blinding where possible, participants were asked not to share or discuss class content with others outside of their class or with their test examiners. To minimize potential examiner bias, the clinicians who conducted pre- and post-intervention testing sessions had no involvement in recruitment, class assignment, or the intervention. Potential examiner bias was assessed by having examiners guess which class each participant had attended, using a forced-choice survey. During post-intervention testing, participants also completed a survey that asked whether they knew about the content of the other class, which provided a check for potential participant bias.
Treatment interventions
The treatment intervention was an 8-week MBSR class, and the active control condition was an 8-week Brain Health education class. provides details on the weekly class topics for both classes. There were three rounds of both classes that occurred six months apart, resulting in a total of three MBSR and three Brain Health classes in this pilot study. The MBSR and Brain Health classes were matched for instructor (i.e., all participants had the same instructor), level of interaction with the instructor, social interaction with class participants, physical movement, class schedule, and inclusion of homework activities. The instructor was a health educator with a Master’s degree in Education with an emphasis on instruction. She obtained training and holds MBSR certification through the University of Massachusetts MBSR program and has over 10 years of experience facilitating MBSR classes and teaching health education courses. The instructor made an effort to minimize cross-contamination of material across the classes (e.g., avoiding discussion of meditation in the Brain Health class and redirecting such discussions). Participants could miss a maximum of three classes during the 8-week schedule and still be included in the study. Participants completed homework logs every week to track the number of hours they spent doing homework at home, and study staff collected these logs every week.
Table 2. Weekly topics for MBSR and brain health classes.
MBSR class
The standardized 8-week MBSR class (Kabat-Zinn, Citation1990) met weekly for 2.5 hours, with a day-long retreat in the 6th week. Participants were taught the practice of mindfulness, including sitting meditation, mindful movement, informal mindfulness practices of daily life (e.g., eating, communicating, working, coping), body awareness, and yoga. During the retreat, participants reviewed class material, were led in longer meditation and yoga practices, and ate lunch together. In between the classes, participants were given assignments they could complete at their own pace throughout the week at home, where they engaged in the practice of mindfulness with meditation CDs, mindful movement, and readings.
Brain Health class
Like the MBSR class, the 8-week Brain Health class also met weekly for 2.5 hours, with a day-long retreat in the 5th week. The curriculum was adapted from a VA class designed for people with brain injuries. Participants were instructed on brain-behavior relationships, the impact of brain injuries on cognitive abilities (e.g., attention, learning, and memory), the impact of nutrition and sleep on cognition, and strategies for successful aging. Participants also performed simple physical exercises and stretches in order to match the yoga/movement aspect of the MBSR class. Each class consisted of a lecture using slides and video clips (~1.5 hours), followed by a discussion where participants shared their experiences and insights (~1 hour). During the day-long retreat, participants in the Brain Health class reviewed class material, watched documentaries on brain-related topics, and ate lunch together. In between the classes, participants were given assignments they could complete at their own pace at home throughout the week, including readings and brief homework exercises related to each week’s topic.
Outcome measures
Acceptability and integration
To assess acceptability and integration, participants completed an anonymous survey at the end of the post-intervention testing session. This survey included nine items about their satisfaction with the class rated on a scale from 1–5 (very unlikely to very likely; see ). Five additional open-ended questions were asked to measure integration (e.g., “Have you made any changes in your lifestyle? If so, please describe.”). The survey was created through team consensus, by drawing from class satisfaction surveys used in published MBSR studies (Aherne et al., Citation2016; e.g., Ruijgrok-Lupton, Crane, & Dorjee, Citation2018). The surveys were completed by participants in a private room out of view of the instructor, examiner, and other participants. The participants placed their surveys into an envelope to ensure anonymity.
Table 3. Anonymous post-intervention questionnaire items with mean scores (SDs).
Treatment implementation
Randomization was assessed by examining whether the two intervention groups were comparable with respect to sociodemographic variables, including age, education, ethnicity, and gender. Successful blinding was evaluated by having the examiners complete a forced-choice post-intervention survey as to which class they believed the participant had just completed. Participants were also asked to report what they believed was taught in the other intervention arm, in order to evaluate whether participants were blind as to the content of the other class. Regarding treatment fidelity, two experts were asked to rate the class instructor on adherence to the class manuals on a scale from 1–5 (low adherence to high adherence), based on a 20-minute video clip of the instructor.
Practicality
Practicality was measured in part based on participant retention rates and class attendance rates. Also, at the end of the class, the instructor rated participants on their level of engagement and understanding of the class material using a 10-point scale, with higher numbers indicating greater engagement and understanding. Because the rating forms changed between the second and third round of classes, the first set of ratings used a scale from 1–10 and the latter ratings used a scale from 1–7. For both forms, higher numbers indicated better comprehension/participation. Engagement was also measured by examining the number of hours participants reported spending on homework assignments, as well as participant responses on a post-intervention questionnaire to gauge how much they learned about certain topics (e.g., mindfulness, brain-behavior relationships) during the class.
Efficacy testing
Mood
The Geriatric Depression Scale-Short Form (GDS; Yesavage et al., Citation1982) and the State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, Citation1983) measured self-reported symptoms of depression and anxiety, respectively. The GDS was selected because the study participants were older adults (ages 60–80). The STAI Form Y-1 was chosen for its focus on current symptoms of anxiety. Both measures have been shown to have strong reliability and validity (L. L. Barnes, Harp, & Jung, Citation2002; Dennis, Boddington, & Funnell, Citation2007; Sheikh & Yesavage, Citation1986; Stanley, Novy, Bourland, Beck, & Averill, Citation2001). Higher scores on both measures reflect greater symptom severity.
Cognition
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS; Randolph et al., Citation1998) was utilized to compare cognition before and after intervention. The RBANS has been shown to have strong psychometric properties (Duff et al., Citation2004). The RBANS has multiple versions with a scoring system that accounts for practice effects from pre- to post-intervention testing. The RBANS yields a total scale score for overall cognition as well as five index scores for attention, language, visuospatial/constructional abilities, immediate memory, and delayed memory. The domains of attention and immediate memory were the primary variables of interest because MBSR has been shown to enhance focus and reduce distractibility in other groups (Tang, Hölzel, & Posner, Citation2015).
The Cognitive Failures Questionnaire (CFQ; Broadbent et al., Citation1982) includes 25 questions about the frequency of making minor and common cognitive mistakes (e.g., “Do you find you forget people’s names?”) rated on a 0–4 scale (never to very often). Higher scores indicate a greater frequency of making cognitive mistakes.
Health and functioning
The RAND 36-Item Short Form Health Survey (RAND SF-36 v. 1.0; Hays & Morales, Citation2001) was used to measure current health and daily functioning. The RAND SF-36 includes self-ratings across eight health domains: Physical functioning, bodily pain, limitations due to physical health problems, limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health. This measure was administered to evaluate changes in daily functioning, and higher scores indicate better health and functioning.
Mindfulness and well-being
Two measures of self-reported mindfulness and well-being were administered. The Mindful Attention Awareness Scale (MAAS; Brown & Ryan, Citation2003) includes 15 items related to the frequency of occurrence of everyday experiences of awareness/attention (e.g., “I find it difficult to stay focused on what’s happening in the present”) rated on a 1–6 scale (almost always to almost never). The Satisfaction with Life Scale (Diener, Emmons, Larsen, & Griffin, Citation1985) includes 5 statements of general life satisfaction rated on a 1–7 scale (strongly agree to strongly disagree).
Data analytic approach
For measures collected at one timepoint (i.e., acceptability, integration, implementation, practicality), analyses were conducted using a multivariate ANOVA (MANOVA) as an omnibus test for measures with multiple dependent variables. If post-hoc analyses were completed, Bonferroni adjusted p-values were applied. Pairwise comparisons were examined with independent t-tests for continuous variables and Chi-square analyses for binary variables. For measures collected at multiple timepoints (i.e., preliminary efficacy), separate linear mixed effects models (“lme4” package v. 1.1–21 in “R” v. 3.6.3) were used to examine each outcome. Class (MBSR, Brain Health) and timepoint (pre-intervention, post-intervention, and three-month follow-up) were entered as fixed effects, participants were entered as a random effect, and the outcome variable was entered as a dependent variable. Main effects of class and timepoint, as well as the class x timepoint interaction (reflecting intervention effects) were examined. For measures of cognition and health, which included multiple sub-scales, Bonferroni adjusted p-values were applied.
Results
Acceptability and integration
A MANOVA was used determine whether there were differences in patient acceptability and integration between MBSR and the Brain Health control group (for specific items and means, see ). Results indicated significant class differences F(1,43) = 5.07, p < .001, so separate post-hoc ANOVAs were utilized to examine each of the nine measures (Bonferroni adjusted p = .006).
Results from the anonymous survey revealed that participation in MBSR was associated with better stress coping skills F(1,43) = 45.61, p < .001. All other items from the anonymous survey did not reveal class differences (ps >.009). Open-ended questions (e.g., What was your most significant insight during the class?) elicited many responses indicating satisfaction with both the MBSR and Brain Health class (see for sample responses).
Table 4. Responses to open-ended items on the anonymous questionnaire.
Two survey items were used to measure integration. Participants in the MBSR class were more likely than participants in the Brain Health class to report practicing the skills they learned (67% vs. 41% reporting “very likely”), t(39) = −2.42, p = .020. MBSR participants were also more likely to respond yes to the question, Have you made any changes in your lifestyle? (90% vs. 58%), relative to Brain Health participants, (1, N = 49) = 4.71, p = .030.
Treatment implementation
Randomization efforts were successful, as the MBSR and Brain Health groups did not differ with respect to gender balance, (1, N = 49) = 0.01, p = .921, or age t(46) = 0.99, p = .329. Participants in classes also did not differ in terms of years of education t(47) = 0.99, p = .329 or ethnicity F(1,47) = 0.10, p = .76. Study implementation was also successful, as the instructor received a mean rating of 5 out of 5 for the Brain Health class and 5 out of 5 for the MBSR class, with higher scores reflecting greater adherence to class manuals. Blinding procedures for examiners were also successful. First, forced-choice tests completed by examiners after the post-intervention test session revealed that examiners were at chance levels (40% accurate) at guessing which class each participant had taken. Additionally, examiners reported no instances of being informed of a participant’s class membership, either by a participant or a member of the research team. Participant blinding was also successful, as responses from post-testing questionnaires revealed that participants were unaware of what was being taught in the other class.
Practicality
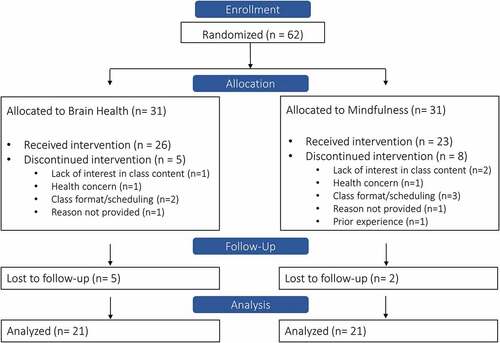
We examined practicality by measuring retention (i.e., the number of recruited participants who completed the program) and participant engagement in the class. Of the 62 individuals who were interested in participating and randomized to one of the two interventions, 23 out of 28 participants (82%) completed the MBSR class, and 26 out of 34 participants (76%) completed the Brain Health class. Our study thus had a high retention rate, particularly for a study that required eight weeks of continuous engagement, in addition to pre- and post-intervention assessments (Cramer et al., Citation2016). A total of 13 participants chose to withdraw (see ). Eight of these participants withdrew from the MBSR intervention, including one due to having previously taught MBSR herself, three due to scheduling difficulties, two due to lack of interest in the class, one who later reported a health condition, and one who did not provide a reason. Five participants withdrew from the Brain Health intervention, one due to lack of time, one because the classes were too long, one due to a lack of interest in the class content, one later reported a health condition, and one did not provide a reason. Of the 49 individuals who completed the 8-week interventions, 42 (86%) completed the 3-month follow-up (91% of MBSR participants and 81% of Brain Health participants).
Participant engagement was measured by examining attendance rates and the number of hours participants spent doing homework. Attendance was high in both interventions (MBSR: 87%, Brain Health: 84%), as only one participant in each group missed more than three classes. The mean number of hours of homework completed (e.g., meditation, yoga, body scan) by MBSR participants per week was higher (M = 2.1, SD = 1.3) than the number of hours of homework completed by Brain Health participants (e.g., reading, videos; M = 1.2, SD = 1.3, t(49) = −2.33, p = .024).
With respect to comprehension of class material, the instructor’s mean rating of participants in the first two rounds was 8.7 out of 10 (SD = 1.3) for MBSR participants and 9.2 out of 10 (SD = 1.4) for Brain Health participants. With respect to class participation, the instructor’s mean rating for participants in the first two rounds was 9.9 out of 10 (SD = 3.9) for MBSR participants and 9.0 out of 10 (SD = 1.9) for Brain Health participants. In the third round of classes, the instructor’s mean rating of class comprehension was 6.8 out of 7 (SD = 0.3) for participants in the MBSR class and 6.8 (SD = 0.5) for participants in the Brain Health class. With respect to class participation in the third round, the instructor’s mean rating was 7.0 out of 7 (SD = 0) for participants in the MBSR class and 6.8 out of 7 (SD = 0.6) for participants in the Brain Health class.
Efficacy testing
Mood
Anxiety as measured by the STAI was not associated with class, timepoint, or their interaction effect (ps>.169). On the depression outcome measure, results indicated a significant class main effect that was evident at baseline, such that the MBSR group had lower (i.e., better) GDS scores than the Brain Health group (B = −2.43, SE = 1.01, t(130) = −2.38, p = .019, 95% CI = [−4.41, −0.45]). There was also a significant timepoint main effect, such that scores across all participants improved over time (B = −0.60, SE = 0.28, t(87) = −2.10, p = .038, 95% CI = [−1.16, −0.04]). The class x timepoint interaction was not significant (B = 0.43, SE = 0.41, t(88) = 1.03, p = .307, 95% CI = [−0.38, 1.24]).
Cognition
Cognitive efficacy, as measured by the RBANS, was analyzed by examining the overall RBANS score and its different subscale scores (i.e., working memory, visuospatial ability, attention, delayed memory) separately. Given the number of subscales examined, the significance threshold was adjusted to p < .01. Results indicated a significant timepoint main effect, such that all participants had improved delayed memory scores (B = 8.23, SE = 2.71, t(47) = 3.04, p = .004, 95% CI = [2.94, 13.56]) and overall RBANS scores over time (B = 5.38, SE = 1.82, t(47) = 2.96, p = .005, 95% CI = [1.82, 8.95]). At a less stringent threshold, a significant class main effect indicated that MBSR participants had higher delayed memory scores than the Brain Health participants across timepoints (B = 14.16, SE = 7.06, t(81) = 2.01, p = .048, 95% CI = [0.46, 27.85]). No other significant class, timepoint, or interaction effects were indicated for any of the remaining RBANS outcomes (ps>.069).
On the Cognitive Failures Questionnaire, results indicated a significant class main effect that was evident at baseline, such that Brain Health participants reported higher scores than MBSR participants (B = −9.40, SE = 3.63, t(90) = −2.59, p = .011, 95% CI = [−16.47, −2.33]); as well as a timepoint main effect, as participants across both interventions reported better scores over time (B = −1.94, SE = 0.76, t(85) = −2.55, p = .013, 95% CI = [−3.43, −0.45]). The intervention x timepoint interaction was not significant (B = 0.28, SE = 1.07, t(85) = 0.26, p = .794, 95% CI = [−1.82, 2.38]).
Health and functioning
Preliminary efficacy on health and functioning was evaluated with the RAND SF-36 subscales (i.e., physical functioning, role limitations due to physical health, role limitations due to emotional problems, energy/fatigue, emotional well-being, social functioning, pain, and general health; see for means). Given the number of subscales examined, the significance threshold was adjusted to p < .006. Results revealed a significant class x timepoint interaction for role limitations due to physical health (B = 14.03, SE = 4.65, t(86) = 3.02, p = .003, 95% CI = [4.89, 23.13]), as MBSR participants reported fewer limitations due to their physical health over time. At a less stringent significance threshold of p < .05, the general health subscale also showed a significant class x timepoint interaction (B = 3.46, SE = 1.67, t(88) =2.07, p = .041, 95% CI = [0.19, 6.75]), as participants in the MBSR class reported higher levels of general health over time. All other comparisons were not significant (ps>.071).
Table 5. Mean (SD) preliminary efficacy scores by timepoint and intervention.
Mindfulness and well-being
On the Mindfulness Attention Awareness Scale and the Satisfaction with Life Scale, results indicated no class, timepoint, or interaction effects (ps>.382).
Discussion
The current study examined the feasibility of conducting a randomized controlled trial of MBSR in a sample of healthy aging adults, using a Brain Health education class as an active control condition. While a number of studies have examined the effectiveness of MBSR in older adults, few have conducted randomized controlled trials that included strong blinding procedures and an active control group, making it difficult to determine whether benefits attributed to MBSR were derived from class content, or due to more general benefits of taking part in a class with social interaction and cognitive stimulation. Findings from our current pilot study demonstrated that a randomized controlled trial of MBSR in healthy aging adults is feasible and moreover, that the MBSR intervention may lead to specific benefits even when compared to an active control intervention.
In terms of feasibility, our pilot study was successfully implemented. Our randomization procedures adequately balanced demographic factors, as there were no significant group differences with respect to age, gender, ethnicity, and education. There was also no evidence of cross-contamination between interventions (i.e., no participants indicated that they had learned about the contents of the other intervention), and our instructor received high scores for course adherence (i.e., treatment fidelity). Additionally, clinician blinding procedures were successful as examiners administering pre- and post-intervention assessments were at chance levels in guessing which class participants had taken part in (MBSR vs. Brain Health).
Both classes also demonstrated high practicality, as participant attendance and retention was near or above 80% across both classes. The class instructor also provided high mean ratings of class participants when asked to report individual participants’ comprehension of course material and class participation. Regarding acceptability, participants’ satisfaction ratings for both the class and the instructor were high across both interventions. Importantly, these scores were obtained anonymously, in order to minimize bias and social pressure. With respect to integration, participants in both classes reported a high likelihood of continuing to use the skills they had gained in the interventions. Notably, MBSR participants were more likely than Brain Health participants to report having made lifestyle changes during the course of the intervention and a desire to continue practicing skills and concepts that they had learned.
In terms of preliminary efficacy, results across most outcome measures were similar across MBSR and Brain Health control groups (i.e., measures of anxiety, health functioning, mindfulness, and well-being). While preliminary, our results did indicate group differences in two of the eight domains measured by the SF-36. Specifically, relative to Brain Health participants, MBSR participants reported fewer role limitations due to physical health over time, and at less stringent statistical levels, MBSR participants also reported greater improvements in their general health over time, which was not seen in Brain Health participants. With the focus on stress reduction in the MBSR intervention, MBSR participants also reported better stress coping abilities. These findings support prior studies that have begun to illuminate how MBSR, with its focus on improving stress and self-awareness, has positive effects on cardiovascular health (DeCarli et al., Citation2001; Loucks et al., Citation2015; Scott-Sheldon et al., Citation2020) and physical health (Alsubaie et al., Citation2017; Grossman, Niemann, Schmidt, & Walach, Citation2004). Our findings thus suggest that MBSR can contribute to improvements in participants’ reported physical health, but replication of our findings are needed to establish efficacy.
Notably, participants in the Brain Health class also showed a greater change (MDiff = 8.2) in their delayed memory scores over time relative to MBSR participants (MDiff = 3.2). While this finding is preliminary and was not significant in our sample, it does support an extant study that found improved verbal memory scores in healthy aging adults after the completion of a 6-week education program focused on cognitive skills, exercise, stress reduction, and diet (Miller et al., Citation2012). This preliminary result also aligns with prior studies examining brain psychoeducation (Norrie et al., Citation2011; Reijnders, Geusgens, Ponds, & van Boxtel, Citation2017) and cognitive training programs more broadly, (Butler et al., Citation2018; Chapman et al., Citation2016; Nguyen, Murphy, & Andrews, Citation2019; Shah, Weinborn, Verdile, Sohrabi, & Martins, Citation2017) which have indicated that many older adults benefit from programs that focus on increasing their knowledge and skills related to cognitive functioning. This suggests that like MBSR, brain health psychoeducation may also serve as an important and effective intervention for improving health and cognition in aging adults. These results also highlight how critical it is to include an active control condition in MBSR trials, as doing so can help elucidate whether specific interventions lead to specific benefits.
Prior studies have indicated that MBSR can have positive benefits on mood and stress (Ahmadpanah et al., Citation2017; Foulk et al., Citation2014; Lavretsky et al., Citation2013; M. Williams et al., Citation2018; Mallya & Fiocco, Citation2019; Mathur et al., Citation2016; Meeten et al., Citation2015; O’Connor et al., Citation2014; Oken et al., Citation2017; Smith et al., Citation2007; Wetherell et al., Citation2017), but studies examining MBSR often lack an active control condition, making it unclear whether benefits were specific to the intervention. In the current study, our findings did not reveal group differences that resulted from participating in either MBSR or the active control group on measures of self-reported depression, anxiety, well-being, and socio-emotional functioning. This may be due to our sample being under-powered at the time of the follow-up period (3-months post intervention). Future studies with larger sample sizes and longer follow-up periods will be critical for determining the specific benefits that MBSR provides relative to an active control intervention.
Limitations and future research
The present study had a number of strengths, as we conducted a successful randomized controlled pilot study of MBSR with an active control condition. Our findings also have ecological validity, as our study was conducted with a community-dwelling sample of healthy older adults. Our findings demonstrate the trial’s feasibility and provide a preliminary test of the effectiveness of MBSR, as our study design revealed that certain gains associated with MBSR were specific to the intervention and not due to general benefits of taking part in a group intervention. Finally, we also administered a comprehensive battery of measures using blinded examiners, allowing us to better understand how MBSR may influence both mental and physical health.
The study also has important limitations. First, our findings are preliminary, as our small sample size (particularly at the 3-month follow-up period) was under-powered for detecting small effect sizes, which in turn can lead to statistical bias and under-detection of small group differences. This limitation and the need to replicate this study’s preliminary results would be best addressed in future randomized clinical trials with larger sample sizes. Another limitation is that our outcome measures relied heavily on participants’ responses, which could have been biased due to concerns with social desirability (Podsakoff, MacKenzie, Lee, & Podsakoff, Citation2003). This limitation was somewhat mitigated by obtaining measures from multiple sources (e.g., feasibility scores from both participants and instructors; implementation success based on reports from blinded examiners and participants) and multiple methods (e.g., objective cognitive scores plus subjective mood scores; anonymous and expert ratings). Also, the critical comparison in the current study was between the MBSR and Brain Health class, and there was no reason to believe that participants in the MBSR class were more impacted by social desirability factors. Another limitation is that some measures, such as coping with stress and instructor’s treatment fidelity, were only measured with a single item. While single-item self-report measures can demonstrate good reliability and validity (e.g., McDowell, Citation2010; Robins, Hendin, & Trzesniewski, Citation2001; Zimmerman et al., Citation2006), future studies would also benefit from utilizing multi-item stress and coping questionnaires to better assess outcomes and a wider sampling of class sessions to measure treatment fidelity.
Another issue highlighted in the current pilot study was a discrepancy between the number of hours spent on homework, with MBSR participants spending more time doing homework than Brain Health participants. Trials ongoing at our site now include additional readings and homework for the Brain Health class in order to reduce this discrepancy. Also, although the two groups were matched on several demographic variables, future trials might also benefit from balancing intervention and control groups with respect to baseline levels of functioning related to the outcomes of interest (e.g., baseline mood, health, and cognition scores).
Conclusion
This randomized controlled pilot study established the feasibility of conducting MBSR in a healthy aging population, with an active control condition and blinded cognitive test examiners. Our preliminary efficacy measures suggest that while both interventions may be beneficial for mood and cognition, MBSR may have specific benefits for self-reported physical health. This study provides the groundwork for a larger randomized controlled clinical trial to evaluate the efficacy of MBSR with respect to improvements in cognition, health, and mood, and provides additional evidence that MBSR can serve as a cost-effective and potentially powerful alternative intervention for improving health and well-being in older adults.
Clinical implications
Both MBSR and Brain Health education interventions may be beneficial for older adults’ mood and cognition, but MBSR may have specific benefits for self-reported physical health.
Our pilot study suggests that MBSR, with its focus on improving stress and self-awareness, has the potential to improve aging adults’ health and coping skills. However, future randomized controlled trials studies with larger sample sizes and longer follow-up periods will be critical for determining the specific benefits that MBSR provides relative to an active control intervention.
Authors’ contributions
JB designed and oversaw the execution of the study, KS collaborated on the design and execution of the study, as well as assisted with data management; SL assisted with data management, conducted data analyses and drafted the manuscript; TH assisted with data analysis; DD taught the class interventions and assisted with design and execution of the study; SP assisted with manuscript preparation; and BC assisted with design and execution of the study. All authors reviewed and approved the final version of the manuscript for submission.
Acknowledgments
Profound gratitude goes to the research participants who took part in this study, and to Drs. Michael Cole, Ori Elis, Fred Loya, and James Muir for their assistance with this project.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this manuscript are not readily available due to Department of Veteran Affairs privacy regulations. Requests to access the datasets should be directed to JB at [email protected].
Additional information
Funding
References
- Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A., Coon, J. T., Kuyken, W., … Dickens, C. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351. doi:10.1016/j.jpsychores.2014.02.012
- Aherne, D., Farrant, K., Hickey, L., Hickey, E., McGrath, L., & McGrath, D. (2016). Mindfulness based stress reduction for medical students: Optimising student satisfaction and engagement. BMC Medical Education, 16(1), 1–11. doi:10.1186/s12909-016-0728-8
- Ahmadpanah, M., Akbari, T., Akhondi, A., Haghighi, M., Jahangard, L., Bahmani, D. S., … Brand, S. (2017). Detached mindfulness reduced both depression and anxiety in elderly women with major depressive disorders. Psychiatry Research, 257, 87–94. doi:10.1016/j.psychres.2017.07.030
- Alsubaie, M., Abbott, R., Dunn, B., Dickens, C., Keil, T. F., Henley, W., & Kuyken, W. (2017). Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: A systematic review. Clinical Psychology Review, 55, 74–91. doi:10.1016/j.cpr.2017.04.008
- Arain, M., Campbell, M. J., Cooper, C. L., & Lancaster, G. A. (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology, 10(1), 1–7. doi:10.1186/1471-2288-10-67
- Azulay, J., Smart, C. M., Mott, T., & Cicerone, K. D. (2013). A pilot study examining the effect of mindfulness-based stress reduction on symptoms of chronic mild traumatic brain injury/postconcussive syndrome. The Journal of Head Trauma Rehabilitation, 28(4), 323–331. doi:10.1097/HTR.0b013e318250ebda
- Barnes, L. L., Harp, D., & Jung, W. S. (2002). Reliability generalization of scores on the Spielberger State-Trait Anxiety Inventory. Educational and Psychological Measurement, 62(4), 603–618. doi:10.1177/0013164402062004005
- Barnes, D. E., & Yaffe, K. (2011). The projected effect of risk factor reduction on Alzheimer’s disease prevalence. The Lancet Neurology, 10(9), 819–828. doi:10.1016/S1474-4422(11)70072-2
- Bédard, M., Felteau, M., Marshall, S., Cullen, N., Gibbons, C., Dubois, S., … Rees, L. (2014). Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: Results from a randomized controlled trial. The Journal of Head Trauma Rehabilitation, 29(4), E13–E22. doi:10.1097/HTR.0b013e3182a615a0
- Berk, L., van Boxtel, M., & van Os, J. (2017). Can mindfulness-based interventions influence cognitive functioning in older adults? A review and considerations for future research. Aging & Mental Health, 21(11), 1113–1120. doi:10.1080/13607863.2016.1247423
- Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., … Fabrizio, C. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. doi:10.1016/j.amepre.2009.02.002
- Broadbent, D. E., Cooper, P. F., FitzGerald, P., & Parkes, K. R. (1982). The cognitive failures questionnaire (CFQ) and its correlates. British Journal of Clinical Psychology, 21(1), 1–16.
- Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. doi:10.1037/0022-3514.84.4.822
- Butler, M., McCreedy, E., Nelson, V. A., Desai, P., Ratner, E., Fink, H. A., … Brasure, M. (2018). Does cognitive training prevent cognitive decline? A systematic review. Annals of Internal Medicine, 168(1), 63–68. doi:10.7326/M17-1531
- Chapman, S. B., Aslan, S., Spence, J. S., Keebler, M. W., DeFina, L. F., Didehbani, N., … D’Esposito, M. (2016). Distinct brain and behavioral benefits from cognitive vs. physical training: A randomized trial in aging adults. Frontiers in Human Neuroscience, 10, 338. doi:10.3389/fnhum.2016.00338
- Cramer, H., Haller, H., Dobos, G., & Lauche, R. (2016). A systematic review and meta-analysis estimating the expected dropout rates in randomized controlled trials on yoga interventions. Evidence-Based Complementary and Alternative Medicine, 2016.
- DeCarli, C., Miller, B. L., Swan, G. E., Reed, T., Wolf, P. A., & Carmelli, D. (2001). Cerebrovascular and brain morphologic correlates of mild cognitive impairment in the National Heart, Lung, and Blood Institute Twin Study. Archives of Neurology, 58(4), 643–647. doi:10.1001/archneur.58.4.643
- Dennis, R. E., Boddington, S. J. A., & Funnell, N. J. (2007). Self-report measures of anxiety: Are they suitable for older adults? Aging & Mental Health, 11(6), 668–677. doi:10.1080/13607860701529916
- Diener, E. D., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. doi:10.1207/s15327752jpa4901_13
- Duff, K., Schoenberg, M. R., Patton, D., Mold, J., Scott, J. G., & Adams, R. L. (2004). Predicting change with the RBANS in a community dwelling elderly sample. Journal of the International Neuropsychological Society, 10(6), 828–834. doi:10.1017/S1355617704106048
- Fiocco, A. J., Mallya, S., Farzaneh, M., & Koszycki, D. (2019). Exploring the benefits of mindfulness training in healthy community-dwelling older adults: A randomized controlled study using a mixed methods approach. Mindfulness, 10(4), 737–748. doi:10.1007/s12671-018-1041-x
- Foulk, M. A., Ingersoll-Dayton, B., Kavanagh, J., Robinson, E., & Kales, H. C. (2014). Mindfulness-based cognitive therapy with older adults: An exploratory study. Journal of Gerontological Social Work, 57(5), 498–520. doi:10.1080/01634372.2013.869787
- Gerritsen, L., Wang, H.-X., Reynolds, C. A., Fratiglioni, L., Gatz, M., & Pedersen, N. L. (2017). Influence of negative life events and widowhood on risk for dementia. The American Journal of Geriatric Psychiatry, 25(7), 766–778. doi:10.1016/j.jagp.2017.02.009
- Grossman, P., Niemann, L., Schmidt, S., & Walach, H. (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. doi:10.1016/S0022-3999(03)00573-7
- Hays, R. D., & Morales, L. S. (2001). The RAND-36 measure of health-related quality of life. Annals of Medicine, 33(5), 350–357. doi:10.3109/07853890109002089
- Hazlett-Stevens, H., Singer, J., & Chong, A. (2019). Mindfulness-based stress reduction and mindfulness-based cognitive therapy with older adults: A qualitative review of randomized controlled outcome research. Clinical Gerontologist, 42(4), 347–358. doi:10.1080/07317115.2018.1518282
- Hofer, H., Holtforth, M. G., Lüthy, F., Frischknecht, E., Znoj, H., & Müri, R. M. (2014). The potential of a mindfulness-enhanced, integrative neuro-psychotherapy program for treating fatigue following stroke: A preliminary study. Mindfulness, 5(2), 192–199. doi:10.1007/s12671-012-0167-5
- Johansson, B., Bjuhr, H., & Rönnbäck, L. (2012). Mindfulness-based stress reduction (MBSR) improves long-term mental fatigue after stroke or traumatic brain injury. Brain Injury, 26(13–14), 1621–1628. doi:10.3109/02699052.2012.700082
- Johansson, L., Guo, X., Hällström, T., Norton, M. C., Waern, M., Östling, S., … Skoog, I. (2013). Common psychosocial stressors in middle-aged women related to longstanding distress and increased risk of Alzheimer’s disease: A 38-year longitudinal population study. BMJ Open, 3(9), e003142. doi:10.1136/bmjopen-2013-003142
- Joo, H. M., Lee, S. J., Chung, Y. G., & Shin, I. Y. (2010). Effects of mindfulness based stress reduction program on depression, anxiety and stress in patients with aneurysmal subarachnoid hemorrhage. Journal of Korean Neurosurgical Society, 47(5), 345–351. doi:10.3340/jkns.2010.47.5.345
- Kabat-Zinn, J. (1990). Full catastrophe living: The program of the stress reduction clinic at the University of Massachusetts Medical Center. New York, NY: Delacorte Press.
- Krivanek, T. J., Gale, S. A., McFeeley, B. M., Nicastri, C. M., & Daffner, K. R. (2021). Promoting successful cognitive aging: A ten-year update. Journal of Alzheimer’s Disease, 81(3), 871–920. doi:10.3233/JAD-201462
- Lavretsky, H., Epel, E. S., Siddarth, P., Nazarian, N., Cyr, N. S., Khalsa, D. S., … Irwin, M. R. (2013). A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: Effects on mental health, cognition, and telomerase activity. International Journal of Geriatric Psychiatry, 28(1), 57–65. doi:10.1002/gps.3790
- Leon, A. C., Davis, L. L., & Kraemer, H. C. (2011). The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research, 45(5), 626–629. doi:10.1016/j.jpsychires.2010.10.008
- Loucks, E. B., Schuman-Olivier, Z., Britton, W. B., Fresco, D. M., Desbordes, G., Brewer, J. A., & Fulwiler, C. (2015). Mindfulness and cardiovascular disease risk: State of the evidence, plausible mechanisms, and theoretical framework. Current Cardiology Reports, 17(12), 1–11. doi:10.1007/s11886-015-0668-7
- Magri, F., Cravello, L., Barili, L., Sarra, S., Cinchetti, W., Salmoiraghi, F., … Ferrari, E. (2006). Stress and dementia: The role of the hypothalamic-pituitary-adrenal axis. Aging Clinical and Experimental Research, 18(2), 167–170. doi:10.1007/BF03327435
- Malinowski, P., Moore, A. W., Mead, B. R., & Gruber, T. (2017). Mindful aging: The effects of regular brief mindfulness practice on electrophysiological markers of cognitive and affective processing in older adults. Mindfulness, 8(1), 78–94. doi:10.1007/s12671-015-0482-8
- Mallya, S., & Fiocco, A. J. (2016). Effects of mindfulness training on cognition and well-being in healthy older adults. Mindfulness, 7(2), 453–465. doi:10.1007/s12671-015-0468-6
- Mallya, S., & Fiocco, A. J. (2019). The effects of mindfulness training on cognitive and psychosocial well-being among family caregivers of persons with neurodegenerative disease. Mindfulness, 10(10), 2026–2037. doi:10.1007/s12671-019-01155-1
- Martin, M., & Doswell, S. (2012). Mindfulness and older people: A small study. British Journal of Occupational Therapy, 75(1), 36–41. doi:10.4276/030802212X13261082051454
- Mathur, S., Sharma, M. P., & Bharath, S. (2016). Mindfulness-based cognitive therapy in patients with late-life depression: A case series. International Journal of Yoga, 9(2), 168. doi:10.4103/0973-6131.183711
- McDowell, I. (2010). Measures of self-perceived well-being. Journal of Psychosomatic Research, 69(1), 69–79. doi:10.1016/j.jpsychores.2009.07.002
- Medina, A. M., & Mead, J. S. (2021). An exploration of mindfulness in speech-language pathology. Communication Disorders Quarterly, 42(4), 257–265. doi:10.1177/1525740120942141
- Meeten, F., Whiting, S., & Williams, C. M. (2015). An exploratory study of group mindfulness-based cognitive therapy for older people with depression. Mindfulness, 6(3), 467–474. doi:10.1007/s12671-014-0279-1
- Miller, K. J., Siddarth, P., Gaines, J. M., Parrish, J. M., Ercoli, L. M., Marx, K., … Barczak, N. (2012). The memory fitness program: Cognitive effects of a healthy aging intervention. The American Journal of Geriatric Psychiatry, 20(6), 514–523. doi:10.1097/JGP.0b013e318227f821
- Moss, A. S., Reibel, D. K., Greeson, J. M., Thapar, A., Bubb, R., Salmon, J., & Newberg, A. B. (2015). An adapted mindfulness-based stress reduction program for elders in a continuing care retirement community: Quantitative and qualitative results from a pilot randomized controlled trial. Journal of Applied Gerontology, 34(4), 518–538. doi:10.1177/0733464814559411
- Moynihan, J. A., Chapman, B. P., Klorman, R., Krasner, M. S., Duberstein, P. R., Brown, K. W., & Talbot, N. L. (2013). Mindfulness-based stress reduction for older adults: Effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology, 68(1), 34–43. doi:10.1159/000350949
- Nguyen, L., Murphy, K., & Andrews, G. (2019). Immediate and long-term efficacy of executive functions cognitive training in older adults: A systematic review and meta-analysis. Psychological Bulletin, 145(7), 698–733. doi:10.1037/bul0000196
- Norrie, L. M., Diamond, K., Hickie, I. B., Rogers, N. L., Fearns, S., & Naismith, S. L. (2011). Can older “at risk” adults benefit from psychoeducation targeting healthy brain aging? International Psychogeriatrics, 23(3), 413–424. doi:10.1017/S1041610210001109
- O’Connor, M., Piet, J., & Hougaard, E. (2014). The effects of mindfulness-based cognitive therapy on depressive symptoms in elderly bereaved people with loss-related distress: A controlled pilot study. Mindfulness, 5(4), 400–409. doi:10.1007/s12671-013-0194-x
- Oken, B. S., Wahbeh, H., Goodrich, E., Klee, D., Memmott, T., Miller, M., & Fu, R. (2017). Meditation in stressed older adults: Improvements in self-rated mental health not paralleled by improvements in cognitive function or physiological measures. Mindfulness, 8(3), 627. doi:10.1007/s12671-016-0640-7
- Perera, G., Pedersen, L., Ansel, D., Alexander, M., Arrighi, H. M., Avillach, P., … Gungabissoon, U. (2018). Dementia prevalence and incidence in a federation of European electronic health record databases: The European medical informatics framework resource. Alzheimer’s & Dementia, 14(2), 130–139. doi:10.1016/j.jalz.2017.06.2270
- Podsakoff, P. M., MacKenzie, S. B., Lee, J.-Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903. doi:10.1037/0021-9010.88.5.879
- Randolph, C. (1998). Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). Psychological Corporation.
- Reijnders, J. S. A. M., Geusgens, C. A. V., Ponds, R. W. H. M., & van Boxtel, M. P. J. (2017). “Keep your brain fit!” Effectiveness of a psychoeducational intervention on cognitive functioning in healthy adults: A randomised controlled trial. Neuropsychological Rehabilitation, 27(4), 455–471. doi:10.1080/09602011.2015.1090458
- Robins, R. W., Hendin, H. M., & Trzesniewski, K. H. (2001). Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg self-esteem scale. Personality and Social Psychology Bulletin, 27(2), 151–161. doi:10.1177/0146167201272002
- Ruijgrok-Lupton, P. E., Crane, R. S., & Dorjee, D. (2018). Impact of mindfulness-based teacher training on MBSR participant well-being outcomes and course satisfaction. Mindfulness, 9(1), 117–128. doi:10.1007/s12671-017-0750-x
- Scott-Sheldon, L. A. J., Gathright, E. C., Donahue, M. L., Balletto, B., Feulner, M. M., DeCosta, J., … Salmoirago-Blotcher, E. (2020). Mindfulness-based interventions for adults with cardiovascular disease: A systematic review and meta-analysis. Annals of Behavioral Medicine, 54(1), 67–73. doi:10.1093/abm/kaz020
- Shah, T. M., Weinborn, M., Verdile, G., Sohrabi, H. R., & Martins, R. N. (2017). Enhancing cognitive functioning in healthly older adults: A systematic review of the clinical significance of commercially available computerized cognitive training in preventing cognitive decline. Neuropsychology Review, 27(1), 62–80. doi:10.1007/s11065-016-9338-9
- Sheikh, J. I., & Yesavage, J. A. (1986). Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health, 5(1–2), 165–173. doi:10.1300/J018v05n01_09
- Smith, A., Graham, L., & Senthinathan, S. (2007). Mindfulness-based cognitive therapy for recurring depression in older people: A qualitative study. Aging and Mental Health, 11(3), 346–357. doi:10.1080/13607860601086256
- Spielberger, C. D., Gorsuch, R. L., Lushene, R. E., Vagg, P. R., & Jacobs, G. A. (1983). State-trait anxiety inventory. Palo Alto. Palo Alto, CA: Consulting Psychologists Press Inc.
- Stanley, M. A., Novy, D. M., Bourland, S. L., Beck, J. G., & Averill, P. M. (2001). Assessing older adults with generalized anxiety: A replication and extension. Behaviour Research and Therapy, 39(2), 221–235. doi:10.1016/S0005-7967(00)00030-9
- Sun, J., Kang, J., Wang, P., & Zeng, H. (2013). Self‐relaxation training can improve sleep quality and cognitive functions in the older: A one‐year randomised controlled trial. Journal of Clinical Nursing, 22(9–10), 1270–1280. doi:10.1111/jocn.12096
- Swan, G. E., DeCarli, C., Miller, B. L., Reed, T., Wolf, P. A., Jack, L. M., & Carmelli, D. (1998). Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology, 51(4), 986–993. doi:10.1212/WNL.51.4.986
- Tang, -Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16(4), 213–225. doi:10.1038/nrn3916
- Thabane, L., Ma, J., Chu, R., Cheng, J., Ismaila, A., Rios, L. P., … Goldsmith, C. H. (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10(1), 1–10. doi:10.1186/1471-2288-10-1
- U.S. Census Bureau. (2020). 2020 demographic analysis estimated by components of change. Retrieved from https://www.census.gov/data/tables/2020/demo/popest/2020-demographic-analysis-tables.html
- Wetherell, J. L., Hershey, T., Hickman, S., Tate, S. R., Dixon, D., Bower, E. S., & Lenze, E. J. (2017). Mindfulness-based stress reduction for older adults with stress disorders and neurocognitive difficulties: A randomized controlled trial. The Journal of Clinical Psychiatry, 78(7), 11977. doi:10.4088/JCP.16m10947
- Williams, C. M., Meeten, F., & Whiting, S. (2018). ‘I had a sort of epiphany!’An exploratory study of group mindfulness-based cognitive therapy for older people with depression. Aging and Mental Health, 22(2), 208–217. doi:10.1080/13607863.2016.1247415
- World Health Organization. (2021). Ageing and Health. World Health Organization Fact Sheets. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Retrieved 2 February 2021.
- Yesavage, J. A., Brink, T. L., Rose, T. L., Lum, O., Huang, V., Adey, M., & Leirer, V. O. (1982). Geriatric depression scale. Journal of Psychiatric Research, 17(1), 37–49. doi:10.1016/0022-3956(82)90033-4
- Yu, J., Rawtaer, I., Feng, L., Fam, J., Kumar, A. P., Cheah, I. K.-M., … Tan, E. C. (2021). Mindfulness intervention for mild cognitive impairment led to attention-related improvements and neuroplastic changes: Results from a 9-month randomized control trial. Journal of Psychiatric Research, 135, 203–211. doi:10.1016/j.jpsychires.2021.01.032
- Zimmerman, M., Ruggero, C. J., Chelminski, I., Young, D., Posternak, M. A., Friedman, M., … Attiullah, N. (2006). Developing brief scales for use in clinical practice: The reliability and validity of single-item self-report measures of depression symptom severity, psychosocial impairment due to depression, and quality of life. Journal of Clinical Psychiatry, 67(10), 1536–1541. doi:10.4088/JCP.v67n1007