Abstract
Objective
Monitoring quality of life (QoL) in patients with cancer can provide insight into functional, psychological and social consequences associated with illness and its treatment. The primary objective of this study is to examine the influence of cultural factors on the communication between the patient and the health care provider and the perceived QoL in women with breast cancer in Japan and the Netherlands.
Methods
In Japanese and Dutch women with early breast cancer, the number, content and frequency of QoL-related issues discussed at the medical encounter were studied. Patients completed questionnaires regarding QoL and evaluation of communication with the CareNoteBook.
Results
The total number, frequency and content of QoL-related issues discussed differed between the two countries. Japanese women (n = 134) were significantly more reticent in discussing QoL-issues than the Dutch women (n = 70) (p < .001). Furthermore, Dutch patients perceived the CareNoteBook methodology significantly more positively than the Japanese patients (p < .001). Both groups supported the regular assessment via a CareNoteBook methodology.
Conclusions
Japanese women are more reluctant in expressing their problems with the illness, its treatment and patient-physician communication than Dutch women.
Background
There is increasing recognition of the importance of patient reported outcomes (PROs) in clinical care and research concerning patients with cancer. PROs are defined as ‘any report coming directly from the patient about their health, an illness and/or its treatment using a self-reported measure.Citation1 PROs are essential tools for obtaining insight into patients’ perceptions of treatment consequences and impact of their illness. The use of PROs has evolved from isolated attempts to assess patients’ views, cognitions and emotions regarding their illness and its treatment, into achieving a solid position in guidelines for professionals in oncology care and manuals on assessing and analyzing PRO-data.Citation2–7 Studying PROs demonstrates respect for how persons with cancer make sense of their illness and the associated treatment, which ideally translates into medical professionals incorporating patients’ views into regular medical care. Empirically, our research group and Greenhalgh et al. published papers on how feedback of PRO-data to patients and physicians resulted in facilitating the discussion of quality of life (QoL) issues and heighten physicians’ awareness of patients’ quality of life (QoL).Citation8,Citation9 Major steps in PRO-research have involved studies that show how PRO-data helped to predict patient survival, strongly reinforcing the value of monitoring PROs in the care of patients with cancer.Citation10–14
PROs in cancer care are determined by a wealth of factors, e.g., clinical, sociodemographic, and psychological factors.Citation15 Cross-cultural studies on PROs in patients with cancer have demonstrated that cultural factors can influence patient perceptions and experiences. Work by Dein and by Kleinman and colleagues has shown how the societal meanings attached to illness (any) and cancer (specifically) shape patients’ QoL, their illness behavior, and their interaction with health care providers.Citation16,Citation17
Over the past 20 years, our cross-cultural research group has been studying the illness perceptions and experiences of patients with breast and lung cancer in Japan and the Netherlands. Traditionally, in the Japanese culture much value is placed on being modest and reserved.Citation18 Contrary to Western culture, verbalization of feelings and thoughts is not common. Furthermore, there is respect for the doctor’s status and authority.Citation19 In Japan, the physician–patient relationship is often described as more hierarchical and paternalistic compared to Western countries.Citation20 Western patients are known for more critical assessment of their physicians’ professionalism and communication skills.Citation21
The first publication from our group reported comparable patterns in Japanese and Dutch patients with various diagnostic cancer categories regarding perceived QoL.Citation22 Despite cultural differences, a considerable degree of conceptual equivalence of QoL in Japanese and Dutch patients with cancer was observed.Citation23–26 This indicated a satisfactory structural and cross-cultural equivalence for the use of EORTC-QLQ-C30 with regard to items measuring QoL.Citation21 Subsequently, Japanese cancer researchers developed a methodology to assess QoL in a clinical setting. Kobayashi and colleagues reported on the development of the CareNoteBook: a self-report measure that assesses three dimensions of QoL, i.e. physical well-being, mental well-being, and life well-being. Research from Japanese physicians on PROs in patients with cancer has illustrated the validity of this approach.Citation27,Citation28 Further to our research program on cross-cultural issues in the care of persons with cancer in Japan and the Netherlands, we studied the perceptions of Japanese and Dutch women with early breast cancer about the monitoring of PROs with the use of the CareNotebook.
Methods
Study design
This study was conducted as part of a larger trans-cultural randomized trial in the Netherlands and Japan. The detailed study design has been previously reported.Citation8 In brief, this open-label, multicentre study investigated the effects of introducing a QoL-monitor on aspects of communication, medical care and patient outcomes. The primary objective of this study was to assess the extent to which QoL-topics were discussed. Secondary objectives included the effects of these discussions on patient management; length of consultations; patients’ perceived efficacy to communicate with healthcare providers (HCPs); patients’ satisfaction regarding communication with their HCP; QoL and distress; patients’ perceptions of their illness; and finally patients’ perceptions of the use of the QoL-monitor. Patients were randomly allocated to receive usual care, or usual care with the use of the QoL-monitor before every chemotherapy cycle visit. The study was performed in accordance with the Helsinki Declaration of the World Medical Association. The institutional review boards of each participating institution approved the study protocol.
In this subsample we included the patients who completed a communication checklist before the start of their fourth cycle of chemotherapy, after the consultation with their healthcare provider.
The primary aim of this report is to examine differences in communication between the patient and the healthcare provider and the perceived QoL in women with breast cancer in Japan and the Netherlands.
Patients
Inclusion criteria were female patients with breast cancer stages I–III, performance status 0 (able to carry out all normal activity without restrictions) or 1 (restricted in physically strenuous activity but ambulatory and able to carry out light work),Citation29 scheduled to receive (neo)adjuvant first line intravenous chemotherapy. Eligible patients were invited to participate in this study by their treating physician before the start of chemotherapy. Patients who chose to participate gave written consent.
Chemotherapy
Women in both countries had received one of the following chemotherapy regimens: TAC (75 mg/m2 docetaxel, 50 mg/m2 adriamycin, 500 mg/m2, cyclophosphamide), AC (60 mg/m2 doxorubicin, 600 mg/m2 cyclophosphamide), FEC (500 mg/m2 fluorouracil, 100 mg/m2 epirubicin, 500 mg/m2 cyclophosphamide) or TC (75 mg/m2 docetaxel, 600 mg/m2 cyclophosphamide). The combination of concurrent TAC was used in the Netherlands only.
Questionnaires
On the day of the consultation before the fourth cycle of chemotherapy, participants were asked to complete a communication checklist after the consultation with their healthcare provider (HCP). Women were free to do this at the outpatient clinic or at home, and were asked to return the checklist to the institutional clinical research coordinator. The questionnaires were anonymized, containing only a unique study number. The communication checklist used in the present study was an adapted version of the checklist designed by Hilarius et al.Citation30 and was validated in an investigation by our research team.Citation8 It consists of 19 questions that refer to a specific symptom (e.g. pain, nausea, sleeping problems) or domain of functioning (e.g., physical and emotional functioning). These items are derived from the function and symptoms scales of the cancer generic EORTC QLQ-C30 and breast cancer specific EORTC BR-23 quality of life questionnaires. Patients were asked to indicate for each topic whether it had been discussed (yes/no) with their healthcare provider. The outcome of this self-report checklist is a composite index (the total number of QoL-related topics discussed) together with individual item scores (for each separate QoL topic). Evaluation of the QoL-monitor was carried out with a self-developed questionnaire, consisting of 7 items.Citation8,Citation24 All sociodemographic and clinical characteristics were obtained from patients’ medical records.
Statistical analyses
Descriptive analyses were performed to investigate means and frequencies of the patients’ sociodemographic and breast cancer and treatment characteristics. Differences between the two countries regarding the respondents’ background characteristics and the evaluation of the QoL-monitor were analyzed using t-tests (means) and chi-square tests (frequencies). With regard to the communication content in Japan and the Netherlands, frequencies were calculated for the composite score (total number of QoL-items discussed) and for the separate items. Additionally, percentages per country were calculated for the visits that included discussion of at least one item falling within one of the four clusters of QoL-items (general physical symptoms, locoregional symptoms, role and physical functioning, and psycho-social functioning).
Results
Seventy Dutch and 134 Japanese women with breast cancer were eligible for the analyses in this study sample of the trial between October 2012 and April 2016. Demographic and clinical variables are summarized in . Whereas age and breast cancer characteristics were mostly similar in Japan and the Netherlands, treatment details were different. Compared with Japan, respondents in the Netherlands more often received neoadjuvant chemotherapy, were prescribed different chemotherapy regimens, and had undergone radiotherapy before their chemotherapy treatment more often.
Table 1. Sociodemographic and clinical characteristics.
QoL-related topics discussed
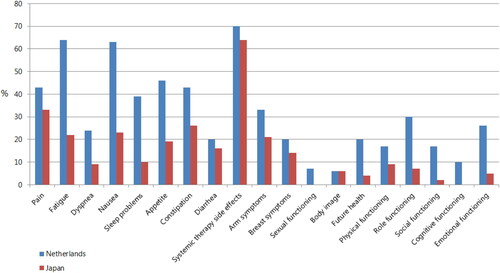
The total number of QoL-related topics that were discussed during the visit are summarized in and . These self-reports indicate that on average more QoL-related items had been discussed during the visit in the Netherlands compared with Japan (5.97 versus 2.90, t(203) = 6.83, p < 0.001). More than 25% of Japanese women indicated that no QoL-related item had been discussed during the visit.
Figure 1. Total number of QoL-related items discussed during medical visit (consultation before fourth cycle of chemotherapy).
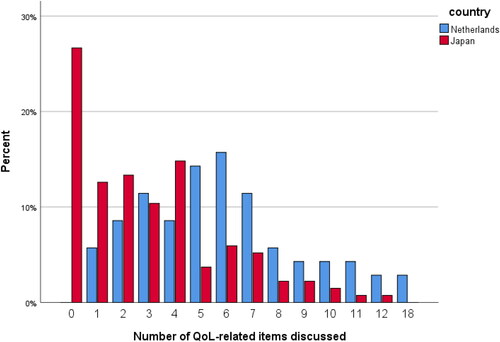
Table 2. Total number of QoL-related items discussed during visit.
According to the Japanese women, items that had been discussed most frequently during the visit were common side effects of chemotherapy (e.g. feeling ill, taste differences, hair loss, hot flushes; 64%), pain (33%) and constipation (26%). Dutch women indicated that side effects of chemotherapy (70%), fatigue (64%) and nausea (63%) had been discussed most frequently (see and ).
Table 3. Discussion of QoL-related items in the Netherlands and Japan.
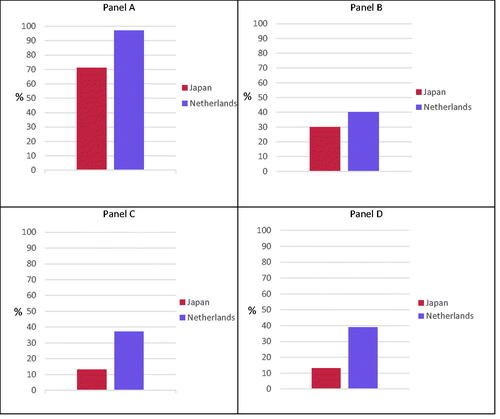
Overall, the majority of Dutch (97%) and Japanese (71%) women remembered discussing one or more general physical complaint (see ). According to Dutch women, items relating to locoregional symptoms (reported complaints by patients about the breast or the arm), role and physical functioning, and psycho-social functioning had been discussed in 37-40% of the visits. For Japanese women these three domains of QoL had been discussed in only 13-30% of the visits.
Figure 3. Proportion of visits that included discussion (at least 1 item per domain) about: general physical symptoms (Panel A), locoregional symptoms (Panel B), physical and role functioning (Panel C) and psycho-social functioning (Panel D).
shows the evaluation of the QoL-monitor by the patients of this study sample who were randomized to the interventional study arm (63 Japanese and 28 Dutch patients). Patients in both countries appear to evaluate the QoL-monitor overall positively, with the Dutch patients reporting a higher perceived usefulness and a lower perceived burden.
Table 4. Evaluation of QoL-monitor use.
Discussion
There are two key findings from this study. First, Japanese breast cancer patients were more cautious and reluctant in reporting physical, psychological, and social consequences and problems associated with the illness and its medical treatment than their Dutch counterparts. Second, compared with the Japanese women with breast cancer, the Dutch women with breast cancer in our study had a significantly more favorable attitude to monitoring and discussing their quality of life during the medical treatment. They perceived the CareNoteBook methodology more helpful in encouraging them to report problems, to formulate questions, and to communicate about this with their physician. Also, they perceived the CareNoteBook less burdensome or difficult to complete. Nevertheless, the large majority of Dutch and Japanese women in this study endorsed introducing the monitoring of QoL during chemotherapy treatment. Earlier research findings are in line with our current work. Women with breast cancer welcomed physicians’ requests to report their responses to the illness and its treatment.Citation21,Citation28 In 2017 we reported the differences in QoL between Japanese and Dutch women after one cycle of chemotherapy in this randomized trial.Citation23 Japanese patients reported higher scores on several domains of QoL compared with the Dutch patients. If Japanese patients perceive fewer problems affecting their QoL, they may feel less need to discuss QoL-related issues with their physician.
Responses to inquiring about the impact of breast cancer were generally viewed positively by the patients concerned.Citation24,Citation31 Previous research showed a similar reticence in reporting problems with the medical treatment of breast cancer in Japanese patients. For example, Matsui et al. uncovered a fairly large set of problems in four domains (psychological and existential; physical; social relations; social living) in Japanese patients with cancer.Citation32 Okuyama et al. reported similar findings, and also a reluctance among Japanese patients with cancer to disclose their emotional distress to their physicians.Citation18 These findings were reinforced in the study by Sakai et al. who identified differences in perceptions of breast cancer treatments between patients, physicians and nurses regarding unmet information needs in Japanese settings.Citation33–35
Our study results are in line for the greater part with the body-of-knowledge on how women with breast cancer perceive their illness and its medical treatment. Nevertheless, a limitation of our current work pertains to possible selection effects. The women who participated in the study may be more positive and less critical about the medical care they received than “the average patient with breast cancer”- which would imply that our findings reflect too much of a positive result overall of monitoring QoL. On the other hand, one may argue that particularly women who have strong opinions are more willing to participate in a trial with focus on communication. Furthermore, it should be taken into account that the reported results have been obtained from the checklists, filled in by patients after their consultation with their healthcare provider (HCP). Not all discussed QoL-issues may have been remembered or possibly interpreted differently. We have previously shown in this trial that there were some small differences in reporting the items that were discussed between observers that evaluated the content of audio-recordings of consultations and patients who completed the questionnaires.Citation8
Regarding clinical practice implications, this study shows that despite the small differences in reporting psychosocial aspects of their disease and patient-physician communication, Japanese and Dutch patients are committed to participate in QoL-research. Modern oncology care in Japan is moving in the direction of what applies in Western societies, namely a focus on shared-decision making, QoL, self-management, patient-reported outcomes and patient-physician communication. For example, Fujimori et al. reported effects of a communication skills training for Japanese oncologist which led to a decreased level of distress in patients.Citation36 Sakai et al. showed that Japanese patients have mainly nonphysical concerns during cancer treatment.Citation36 Incorporating assessments of functional, psychological and social problems associated with living with breast cancer into regular medical care, allows clinical interventions aimed at improving QoL.Citation9,Citation37–40
As we outlined in a previous publication, we suggest a number of recommendations for daily clinical practice:Citation41
Incorporate assessing QoL into clinical care, similar to incorporating laboratory values into diagnostic and therapeutic policy.
Sensitize health care providers about the importance of QoL in patients with cancer.
Introduce regular collection of PRO’s for patients with cancer during their treatment. This can help identify symptoms and concerns that otherwise would stay undetected.
Very recently, similar results were reported by Jabbarian and colleagues.Citation42 Negative illness perceptions (IP) were associated with worse QoL in patients with advanced cancer. Targeting specific symptoms like anxiety and depression, through modification of IPs, may improve QoL in these patients.
Further research would allow the use of methods that assess more specifically and more in depth the functional, psychological, and social issues associated with the medical treatment for patients with breast cancer. Various medical professional organizations appear to support this suggestion.Citation7,Citation43 Review papers on self-management in patients with cancer offer the scientific context for this development. These suggestions support the work by various research groups on the importance of monitoring PROs in patients with cancer, with its potential of improving overall survival.Citation44–46
Declarations
Funding: This study was supported by a grant of the Dutch Pink Ribbon Foundation (110078) and from Pfizer, Japan. The authors have no financial relationship with the organizations that sponsored this research.
Conflict of Interest: All authors declare that they have no conflicts of interest
Availability of data and material: available upon reasonable request
Authors contributions: all authors contributed to the design, data collection and analysis, and writing of the manuscript.
References
- FDA U.S. Food and Drug Administration (FDA). Patient-reported outcome measures: use in medical product development to support labeling claims. 2006. Rockville: Food and Drug Administration. www.fda.gov/cber/gdlns/problbl.html.
- Basch E, Wilfong L, Schrag D. Adding patient-reported outcomes to medicaredical product development to supmodel. Jama. 2020;323(3):213–214. doi:https://doi.org/10.1001/jama.2019.19970
- Basch E, Barbera L, Kerrigan CL, Velikova G. Implementation of patient-reported outcomes in routine medical care. Am Soc Clin Oncol Educ Book. 2018;38:122–134. doi:https://doi.org/10.1200/EDBK_200383
- Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. Jama. 2017;318(2):197–198. doi:https://doi.org/10.1001/jama.2017.7156
- Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol . 2016;34(6):557–565. doi:https://doi.org/10.1200/JCO.2015.63.0830
- Bottomley A, Reijneveld JC, Koller M, et al. Current state of quality of life and patient-reported outcomes research. Eur J Cancer. 2019;121:55–63. doi:https://doi.org/10.1016/j.ejca.2019.08.016
- Coens C, Pe M, Dueck AC, et al. International standards for the analysis of quality-of-life and patient-reported outcome endpoints in cancer randomised controlled trials: recommendations of the SISAQOL Consortium. Lancet Oncol. 2020;21(2):e83–e96. doi:https://doi.org/10.1016/S1470-2045(19)30790-9
- Lugtenberg RT, Fischer MJ, de Jongh F, et al. Using a Quality of Life (QoL)-monitor: preliminary results of a randomized trial in Dutch patients with early breast cancer. Qual Life Res. 2020;29(11):2961–2975. doi:https://doi.org/10.1007/s11136-020-02549-8
- Greenhalgh J, Long AF, Flynn R. The use of patient reported outcome measures in routine clinical practice: lack of impact or lack of theory? Soc Sci Med. 2005;60(4):833–843. doi:https://doi.org/10.1016/j.socscimed.2004.06.022
- Ambroggi M, Biasini C, Toscani I, et al. Can early palliative care with anticancer treatment improve overall survival and patient-related outcomes in advanced lung cancer patients? A review of the literature. Support Care Cancer. 2018;26(9):2945–2953. doi:https://doi.org/10.1007/s00520-018-4184-3
- Mierzynska J, Piccinin C, Pe M, et al. Prognostic value of patient-reported outcomes from international randomised clinical trials on cancer: a systematic review. Lancet Oncol. 2019;20(12):e685–e698. doi:https://doi.org/10.1016/S1470-2045(19)30656-4
- Sullivan DR, Forsberg CW, Ganzini L, et al. Longitudinal changes in depression symptoms and survival among patients with lung cancer: a national cohort assessment. J Clin Oncol. 2016;34(33):3984–3991. doi:https://doi.org/10.1200/JCO.2016.66.8459
- Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol. 2017;35(8):834–841. doi:https://doi.org/10.1200/JCO.2016.70.5046
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi:https://doi.org/10.1056/NEJMoa1000678
- Haslam A, Herrera FromOnliD, Gill J, Prasad V. Patient experience captured by quality-of-life measurement in oncology clinical trials. JAMA Netw Open. 2020;3(3):e200363–19. doi:https://doi.org/10.1001/jamanetworkopen.2020.0363
- Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5(2):119–124. doi:https://doi.org/10.1016/S1470-2045(04)01386-5
- Kleinman A, Eisenberg L, Good B. Culture, illness, and care. Ann Intern Med. 1978;88(2):251–258. doi:https://doi.org/10.7326/0003-4819-88-2-251
- Okuyama T, Endo C, Seto T, et al. Cancer patients' reluctance to disclose their emotional distress to their physicians: a study of Japanese patients with lung cancer. Psychooncology. 2008;17(5):460–465. doi:https://doi.org/10.1002/pon.1255
- Ashing-Giwa KT, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology. 2004;13(6):408–428. doi:https://doi.org/10.1002/pon.750
- Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata N, Aoki Y. The interaction between physician and patient communication behaviors in Japanese cancer consultations and the influence of personal and consultation characteristics. Patient Educ Couns. 2002;46(4):277–285. doi:https://doi.org/10.1016/S0738-3991(01)00164-1
- Aelbrecht K, Hanssens L, Detollenaere J, Willems S, Deveugele M, Pype P. Determinants of physician-patient communication: the role of language, education and ethnicity. Patient Educ Couns. 2019;102(4):776–781. doi:https://doi.org/10.1016/j.pec.2018.11.006
- Kleijn WC, Ogoshi K, Yamaoka K, et al. Conceptual equivalence and health-related quality of life: an exploratory study in Japanese and Dutch cancer patients. Qual Life Res. 2006;15(6):1091–1101. doi:https://doi.org/10.1007/s11136-006-0049-1
- Fischer MJ, Krol er FromOnlinEMM, Ranke GMC, et al. Routine monitoring of quality of life for patients with breast cancer: an acceptability and field test. J Psychosoc Oncol. 2012;30(2):239–259. doi:https://doi.org/10.1080/07347332.2011.644398
- Fischer MJ, Inoue K, Matsuda A, et al. Cross-cultural comparison of breast cancer patients.644398" er: ancer: ry study in Japanese and D. Breast Cancer Res Treat. 2017;166(2):459–471. doi:https://doi.org/10.1007/s10549-017-4417-z
- Kaptein AA, Yamaoka K, Snoei L, et al. Illness perceptions and quality of life in Japanese and Dutch patients with non-small-cell lung cancer. Lung Cancer. 2011;72(3):384–390. doi:https://doi.org/10.1016/j.lungcan.2010.09.010
- Kaptein AA, Yamaoka K, Snoei L, et al. Illness perceptions and quality of life in Japanese and Dutch women with breast cancer. J Psychosoc Oncol. 2013;31(1):83–102. doi:https://doi.org/10.1080/07347332.2012.741092
- Kobayashi K, Green J, Shimonagayoshi M, et al. Validation of the care notebook for measuring physical, mental and life well-being of patients with cancer. Qual Life Res. 2005;14(4):1035–1043. doi:https://doi.org/10.1007/s11136-004-2958-1
- Matsuda A, Yamada Y, Ishizuka N, et al. Effectiveness of a self-monitoring quality of life intervention for patients with cancer receiving palliative care: a randomized controlled clinical trial. Asian Pac J Cancer Prev. 2019;20(9):2795–2802. doi:https://doi.org/10.31557/APJCP.2019.20.9.2795
- Young J, Badgery-Parker T, Dobbins T, Jorgensen M, Gibbs P, Faragher I, Jones I, Currow D. Comparison of ECOG/WHO performance status and ASA score as a measure of functional status. J Pain Symptom Manage. 2015;49(2):258–64.
- Hilarius DL, Kloeg PH, Gundy CM, Aaronson NK. Use of health-related quality-of-life assessments in daily clinical oncology nursing practice. Cancer. 2008;113(3):628–637. doi:https://doi.org/10.1002/cncr.23623
- van der Kloot WA, Uchida Y, Inoue K, et al. The effects of illness beliefs and chemotherapy impact on quality of life in Japanese and Dutch patients with breast or lung cancer. Chin Clin Oncol. 2016;5:3.
- Matsui T, Hirai K, Shokoji M, et al. Problems, goals and solutions reported by cancer patients participating in group problem-solving therapy. Jpn J Clin Oncol. 2019;49(3):245–256. doi:https://doi.org/10.1093/jjco/hyy191
- Sakai H, Umeda M, Okuyama H, Nakamura S. Differences in perception of breast cancer treatment between patients, physicians, and nurses and unmet information needs in Japan. Support Care Cancer. 2020;28(5):2331–2338.
- Kasahara - Kiritani M, Matoba T, Kikuzawa S, et al. Public perceptions toward mental illness in Japan. Asian J Psychiatr. 2018;35:55–60. doi:https://doi.org/10.1016/j.ajp.2018.05.021
- Uchida M, Sugie C, Yoshimura M, et al. Factors associated with a preference for disclosure of life expectancy information from physicians: a cross-sectional survey of cancer patients undergoing radiation therapy. Support Care Cancer. 2019;27(12):4487–4495. doi:https://doi.org/10.1007/s00520-019-04716-1
- Fujimori M, Shirai Y, Asai M, Kubota K, Katsumata N, Uchitomi Y. Effect of communication skills training program for oncologists based on patient preferences for communication when receiving bad news: a randomized controlled trial. J Clin Oncol. 2014;32(20):2166–2172. doi:https://doi.org/10.1200/JCO.2013.51.2756
- Sasaki H, Tamura K, Naito Y, et al. Patient perceptions of symptoms and concerns during cancer chemotherapy: 'affects my family' is the most important. Int J Clin Oncol. 2017;22(4):793–800. doi:https://doi.org/10.1007/s10147-017-1117-y
- Atema V, van Leeuwen M, Kieffer JM, et al. Efficacy of internet-based cognitive behavioral therapy for treatment-induced menopausal symptoms in breast cancer survivors: Results of a randomized controlled trial. J Clin Oncol. 2019;37(10):809–822. doi:https://doi.org/10.1200/JCO.18.00655
- Compen F, Bisseling E, Schellekens M, et al. Face-to-face and internet-based mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2018;36(23):2413–2421. doi:https://doi.org/10.1200/JCO.2017.76.5669
- Farthmann J, Hanjalic omOnliA, Veit J, et al. The impact of chemotherapy for breast cancer on sexual function and health-related quality of life. Support Care Cancer. 2016;24(6):2603–2609. doi:https://doi.org/10.1007/s00520-015-3073-2
- Kaptein AA, Schoones JW, Fischer MJ, Thong MSY, Kroep JR, van der Hoeven KJM. Illness perceptions in women with breast cancer -3073-2" nction and health-relat. Curr Breast Cancer Rep. 2015;7(3):117–126. doi:https://doi.org/10.1007/s12609-015-0187-y
- Jabbarian LJ, Rietjens JAC, Mols F, Oude Groeniger J, Heide A, Korfage IJ. Untangling the relationship between negative illness perceptions and worse quality of life in patients with advanced cancer lth-relath treatment as usual in reducing psychologic. Support Care Cancer. 2021. Online ahead of print
- Lyman GH, Greenlee H, Bohlke K, et al. Integrative therapies during and after breast cancer treatment: ASCO endorsement of the SIO clinical practice guideline. J Clin Oncol. 2018;36(25):2647–2655. doi:https://doi.org/10.1200/JCO.2018.79.2721
- Matsuda A, Yamaoka K, Tango T, Matsuda T, Nishimoto H. Effectiveness of psychoeducational support on quality of life in early - stage breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2014;23(1):21–30. doi:https://doi.org/10.1007/s11136-013-0460-3
- Rodin G, An E, Shnall J, Malfitano C. Psychological interventions for patients with advanced disease: implications for oncology and palliative care. J Clin Oncol. 2020;38(9):885–904. doi:https://doi.org/10.1200/JCO.19.00058
- Kaptein AA, Kobayashi K, Matsuda A, et al. We alda i omOnlineneMalfpatients’, caregivers’ and health care providers’ illness perceptions about non-small-cell lung cancer (NSCLC). Lung Cancer. 2015;90(3):575–581. doi:https://doi.org/10.1016/j.lungcan.2015.10.017