Abstract
Objectives
The aim of this work was to co-develop an Acceptance and Commitment Therapy (ACT) intervention to support medication adherence and quality of life in breast cancer survivors (BCSs). The research approach was intervention co-development.
Methods
The sample consisted of BCS focus groups (n = 24), health care provider (HCP) interviews (n = 10), and a co-development workshop (BCSs, n = 12; HCPs, n = 9).We conducted 6 BCS focus groups and 10 HCP interviews to understand the acceptability of ACT. We co-designed the intervention in a workshop.
Results
Participants reported high acceptability of an ACT intervention. BCSs preferred ACT exercises focused on values and self-compassion. Both groups recommended face-to-face intervention delivery, by a clinical psychologist, with a mixture of individual and group sessions. BCSs requested advice on side-effect management.
Conclusions
We effectively used patient and HCP co-design to configure an ACT intervention to support medication adherence and quality of life for BCSs. If feasible and efficacious, this ACT-based intervention could support breast cancer survivorship.
Introduction
Low adherence to adjuvant endocrine therapy (AET) among breast cancer survivors (BCSs) is commonCitation1 and is associated with an increased risk of all-cause mortality and poorer survival.Citation2–8 Women report intolerable side effects as a key reason for nonadherence.Citation9–15 Mood, motivation, and associated factors such as memory are also involved in women’s decisions to use medication.Citation11 Despite this common problem, interventions to support women with breast cancer have not successfully improved adherence.Citation16
Existing interventions have focused on providing information about AETs and targeting contextual factors, such as improving communication between patients and care teams.Citation16 It is therefore perhaps unsurprising that they have been ineffective, when considering the broad range of factors contributing to nonadherence.Citation11,Citation12,Citation17,Citation18 In addition to providing information, interventions that also target emotional and somatic factors may be necessary to improve adherence.
Acceptance and Commitment Therapy (ACT) may provide a suitable framework for such an intervention. ACT aims to help people align their behavior with their overarching goals in life by engendering “psychological flexibility”: the ability to effectively make choices in situations based on one’s values, while experiencing competing psychological demands.Citation19 Therapy involves mindfulness, goal-setting, and perspective-taking exercises and fosters self-compassion. ACT may apply to AET nonadherence because this behavior might involve willingness to tolerate side effects, alongside difficult thoughts and emotions, and to connect medication-taking with longer-term goals and values. There is growing evidence to support the use of ACT in improving functioning with chronic pain and long-term conditions such as cancer.Citation20–24 Preliminary studies and pilot and feasibility randomized controlled trials involving individual and group ACT sessions for patients with breast cancer have reported improvements in psychological distress, quality of life, and psychological flexibility.Citation25,Citation26 While the research evidence base largely comprises preliminary studies, clinicians appear to use ACT frequently in clinical practice with cancer populations, as shown in a recent survey.Citation27
To date, there have been no published ACT interventions supporting medication adherence in women with breast cancer. It is therefore unknown whether these patients or clinicians would find such an approach to managing medications acceptable or suitable. We used a structured patient and health care professional (HCP) co-design approach to develop an ACT intervention for female BCSs. Study 1 used qualitative inquiry to understand women’s experiences of AET, identify patient preferences for an ACT intervention to support women after completing hospital-based treatments, and explore HCPs’ opinions on how the intervention could function within clinical care. Study 1 informed study 2, a structured co-design workshop involving BCSs and HCPs. The workshop aimed to co-design an implementable ACT-based intervention that is acceptable to both BCSs and HCPs.
Study 1: focus groups with BCSs and interviews with HCPs
Method
Design
We recruited women with breast cancer to participate in six semi-structured focus groups (n = 24). We undertook semi-structured telephone interviews with HCPs (n = 10). LHH (PhD, female, research fellow experienced in qualitative methods) conducted the interviews and focus groups. Prior informed written consent was obtained. The Health Research Authority (London Queens Square, England) Research Ethics Committee granted ethical approval (IRAS #242034). The study conforms to the Declaration of Helsinki standards.
Materials
The authors (clinical psychologists and behavioral scientists) developed separate interview guides for the focus groups and interviews, based on their clinical experience and existing literature on women’s experiences of AETs.Citation12,Citation18 Both guides included a description of ACT and psychological flexibility, including its relevance in this context, questions on the acceptability of ACT in this context, and preferences for the intervention format. The HCP interviews also included an introduction to the problem of nonadherence in AETs and pragmatic questions on how best to implement this intervention within the UK’s existing National Health Service (NHS) services. To ensure sufficient understanding prior to asking about preference, patient focus groups included further descriptions of ACT, along with examples of specific ACT exercises that target each aspect of psychological flexibility (Acceptance, Mindfulness, Values, Committed Action, Flexible Perspective Taking [“Self-as-Context”], and Distancing From Thoughts [“Cognitive Defusion”]). Focus groups also included questions on participants’ experiences of taking AETs, including any barriers to taking them (Supplementary file 1, patient focus group guide).
Participants
BCS focus groups
Adult women were eligible if they had been diagnosed with early stage (1–3) breast cancer, finished their hospital-based treatment, and had been prescribed AET (eg, tamoxifen, aromatase inhibitors). Participants were recruited via a cancer support group’s mailing list and social media. Focus groups were held in community locations across Yorkshire. Participants were offered a voucher to compensate for their time.
HCP interviews
HCPs were breast care nurses, oncologists, surgeons, and clinical psychologists involved in the care of BCSs. They were recruited by approaching NHS hospital sites with breast cancer clinics and clinical psychology services in Yorkshire. Recruitment was increased through snowballing. HCPs were offered monetary compensation for their time.
Measures
Medication adherence
BCSs completed the behavioral domain of the ASK-12 questionnaireCitation28 to assess their adherence to AETs. Participants answered 5 questions on the frequency of various medication-taking behaviors (eg, “taken a medication more or less often than prescribed”), with answer stems: “In the last week,” “In the last month,” “In the last 3 months,” “More than 3 months ago,” “Never.” Scores were out of 20, with higher scores indicating poorer adherence.Citation28
Perceived usefulness and acceptability
BCSs answered questions on their perceived usefulness of ACT for improving well-being, medication decision-making, and managing side effects. They also completed questions on whether specific ACT processes and exercises should be included in the intervention (Supplementary file 2, patient focus group guide).
Analysis
Focus groups and interviews were digitally recorded and transcribed verbatim. We used thematic analysis with a semantic, open-coding approach, from a realist epistemological stance, which reflects that participants’ language is understood as reflecting their reality.Citation29 NVivo plus 12 assisted in organizing codes into themes. LH (a researcher trained in qualitative methods) coded the transcripts and CG and SS checked the quotes and themes for coherence. COREQ guidance was followed.Citation30
Results
Participants
Patient focus groups
All participants were members of local cancer support groups. Average age was 53 years (range 28–70), and half reported being postmenopausal. Average adherence was 8.8 out of 20 (range, 0–18) ().
Table 1. Participant demographics from study 1.
HCP interviews
Ten HCPs from five NHS Trusts participated: four clinical psychologists, three breast care nurses, two surgeons, and one oncologist. Their average number of years experience in breast cancer was 16 (range, 2–35) ().
BCSs’ experience of AETs
Women discussed their experiences of AETs, which grouped into five themes (Appendix B): (1) benefit vs risk: participants questioned whether the risk reduction of AETs were worth the reduced quality of life they caused; (2) control: some participants took their medication to feel they were doing everything they could to prevent a recurrence, and others took them because they did not feel like they had a choice; (3) fluctuating levels of professional support: participants received a lot of support during hospital treatments, but felt this ended upon discharge, leaving many struggling to cope; (4) survivor guilt: feeling guilty they had survived when others had not; and (5) self-identity: AETs made them feel older, and many struggled to accept their post-cancer bodies as their own.
Preferences and opinions on an ACT intervention
Intervention acceptability and suitability
BCSs wanted a supportive intervention after their treatment to help them during the transition from patient to survivor.
… there needs to be something that runs alongside the medication, some talking therapy, somewhere where you can talk about it and be reassured instead of just giving you a prescription and told you are going to take that for 10 years—Lisa, FG2, 53 years
Both BCSs and HCPs were positive about the concept of an ACT-based intervention. All BCSs indicated that an ACT based intervention would be “a little helpful” (33%, 50%) or “very helpful” (66%, 50%) for improving well-being and supporting medication decisions, respectively. BCSs preferred the values and self-compassion exercises (Supplementary file 2, supplementary figure 1).
Several BCSs felt the intervention could empower them to make decisions, as ACT focuses on taking steps toward individual goals and values.
I think [an intervention to help people make decisions based on values] is really positive. I mean, I’ve actually changed how I’m feeling about this just from what we’ve just said … —Lisa, FG2, 53 years
HCPs agreed that support after hospital treatment would be helpful, and those familiar with ACT felt it would be suited to this population.
[ACT] has much greater relevance than just the medication adherence (…), it’s actually equipping people to deal with so many different impacts of living with … and beyond breast cancer. I think you are hitting lots of birds with one stone. … When you were talking about the education-focused approaches… used previously, they are very specific to medication, whereas this actually has a much greater benefit to people.—Clinical Psychologist 1
Despite the overall positive review of ACT in this context, there was some uncertainty among the BCSs as to how the intervention could help with side effects.
I can’t quite see where it would help with dealing with the pain or the hot flushes … —Unidentified Speaker, FG5
HCPs were cautious about how this intervention could work in practice, given the current limited resources in the NHS health care system:
I read that [funding application] and thought, “Wow, that’s really good. That’s exactly the kind of thing we need.” But … it seems so much harder now we have talked about it. It seemed like such an easy idea before [laughing] but it seems like logistically, it’s actually quite difficult … —Surgeon 1
Format of the intervention
BCSs generally preferred that the intervention was delivered face-to-face, rather than via telephone, on a website, or in a printed leaflet/workbook.
I would agree with face-to-face because I sometimes think there is so much on the internet that you actually scare yourself. [Agreement from two other participants.] —Ellen, FG4, 56 years
They argued that human interaction was necessary to provide appropriate emotional support and help reduce the isolation felt by many patients with cancer during and after treatment.
… being able to come and have human interaction. Because a lot of people who are going through treatment for cancer, you become very isolated, you want to shut your door and shut the world out.—Emily, FG4, 70 years
Participants were also supportive of being able to access supplementary information online. It was felt that a website would make it easier to access key information when women were particularly struggling with side effects or emotions.
… some sort of online access (…). There are times when … I would need help … more in that week than I would in another week. So if you could access … even just exercises or like grounding exercises … remotely when you needed them.—Unidentified Speaker, FG6
Both BCSs and HCPs suggested having a mixture of both individual and group intervention sessions. The group sessions may help reduce isolation by enabling connection with other women in a similar situation.
[Group sessions] offer that opportunity for people to have their experiences normalized and go away with a sense of not being on their own. I think in groups it can have a much more profound impact, people coming together and finding that they have a shared experience.—Clinical Psychologist 1
The individual sessions might allow for deeper personal reflection through having one-on-one time with a therapist.
So I think if you do do it only in a group you are possibly missing out some opportunities to get people to think really, really deeply, which is what you need them to do when you are getting them to think about values.—Cassie, FG2, 58 years
BCSs had a preference for clinical psychologists to deliver the intervention, as it was felt they had more experience delivering group-based therapy.
I think you need a psychologist there because the dynamics of the group may drive different things out of it (…). It’s being able to answer those questions and help people with some really serious stuff that’s close to them. And I think helping them with the right mindset. So I think you have to have somebody who knows that kind of stuff.—Unidentified Speaker, FG5
HCPs agreed that a clinical psychologist is best placed to deliver the intervention. However, they felt that clinical psychologists are a limited resource and considered whether a breast care nurse could be trained to deliver the intervention. This raised concerns regarding training costs and capacity issues elsewhere in the clinical service.
It [ACT] doesn’t say that it has to be a psychologist. But I think there would be benefits to it being a psychologist. So yes, I don’t think it would have to be, but again the ideal world type stuff.—Clinical Psychologist 3
Regarding the number of therapy sessions, BCSs suggested that around 4 would be acceptable. HCPs agreed that a lower number of sessions would increase the likelihood of attendance:
I would say probably 4 is a good number and wouldn’t be off-putting.—Claire, FG3, 57 years
I think the [fewer] sessions for people to attend, the better, because I think they’ll come to more. … So if you’ve got 6 sessions, people probably attend 4…—Clinical Psychologist 3
Feasibility of the intervention
HCPs often reflected on the gap between the ideal intervention and what was feasible given existing resources. A common suggestion was to embed the intervention into existing self-management programs.
… my initial thought would be to try to incorporate it somehow into the Moving Forward program, because you do capture a lot of women and it tends to be at that point they have a lot of questions about the tablets, the side effects … and even if you couldn’t particularly deliver it on the same day … you could at least introduce it and then have a separate day set up potentially for [women using AET].—Breast Care Nurse 3
To improve uptake, recruitment, and feasibility of the intervention, HCPs discussed the need for all staff, and particularly the breast care nurses, to be supportive of the intervention.
I think the key is having someone on the ground … a clinician on the ground who will help you with that rather than sort of coming in externally, and having someone who really believes in the research, is an advocate for it, and I would say someone like a breast care nurse rather than a medical doctor just because they would possibly have a bit more time to talk it through with people.—Clinical Psychologist 2
Study 2: BCS and HCP co-design workshop
Method
Design
We held a 3-hour workshop in a community center to design the intervention format. In 3 mixed and balanced groups of approximately 8 BCSs and HCPs, attendees completed tasks to optimize the configuration of the intervention. This process aimed to bring key stakeholders together to allow consideration of both BCSs’ preferences and HCPs’ perspectives on the feasibility and acceptability of an ACT-based psychological intervention.
Tasks
Participants were provided with an overview of ACT by a clinical psychologist, and a patient provided her experience of using AETs. Then, the groups were asked to design what they considered to be the most optimal and feasible intervention to support medication decision-making in women with breast cancer. Groups were provided with colored cards to represent different idea categories (supplementary file 2, supplementary Table 2). For example, green cards represented the “setting” category such as “hospital,” “support group,” and “remote.” Participants were told they could produce new ideas and were not restricted to the cards. Groups were asked to discuss the options, collectively select their preferred choice for each category, and place the appropriate card(s) onto a flip chart.
The groups were asked to reflect on their choices from several perspectives, to see whether this would lead to changes in choices. We facilitated this by adapting the “Three hats” exercise from the “Thinking differently toolkit.”Citation31,Citation32 Groups were asked to spend 3 minutes on each of the following: negatives/risks; positives/benefits; and new ideas/possibilities. Paper hats colored black (negatives), yellow (positives), and green (possibilities) were placed on each table, to encourage discussions to remain focused. The groups were encouraged to amend their original chart throughout this exercise.
The groups then presented their proposed intervention format to each other, and further amendments were permitted. Each group’s proposal was finalized and recorded for discussion among the research team. Additionally, attendees were invited to provide anonymous suggestions using sticky notes on a chart at the back of the room: BCSs were asked what additional information they would like in an intervention; HCPs were asked to provide examples of questions they often get asked by their patients using AET. Suggestions were collected to inform whether any additional information should be provided within the intervention.
The workshop was exempt from ethical approval according to the Health Research Authority (HRA) screening tool.Citation33
Workshop attendees
Eligibility criteria were identical to study 1. Participants from study 1 who consented to be contacted were recruited by email, and a cancer charity advertised the workshop through their mailing list and Facebook. Posters were put up in community centers to increase group diversity. A snowballing method was used to recruit additional HCPs. Attendees were offered a monetary incentive, a Continued Professional Development certificate, and lunch.
Measures
Attendees provided demographic information on age, sex, profession, AET experience, and ACT experience. BCSs were asked to complete the behavioral domain of the ASK-12.Citation28
Analysis
We examined the groups’ intervention configurations from the workshop in parallel. Where possible, the suggestions from each workshop group were combined by consensus. Where there were discrepancies between groups, we considered how pragmatic each option was and how many groups suggested each option. Similarly, if something was suggested by a single group, we considered its feasibility and potential value to the intervention. We grouped attendees’ suggestions for additional information into common themes.
Results
Workshop attendees
Twelve BCSs and nine HCPs attended the workshop. The majority of participants had not taken part in study 1. BCSs’ mean age was 53 (range, 33–67), and average adherence score was 8.5 out of 20 (range, 5–14). Most BCSs were postmenopausal (10/12), with 11 of 12 having experience of taking aromatase inhibitors and 4 of 12 with experience of taking tamoxifen. Four clinical psychologists, four breast care nurses, and one trainee surgeon attended. Attendees were split into 3 groups containing a mixture of BCSs and HCPs. A researcher facilitated each group.
Findings
Compromises were made regarding the number of sessions between BCSs’ preferences and HCPs’ thoughts on feasibility (many/unlimited sessions vs fewer, respectively). The “three hats” exercise successfully elicited BCSs’ perspectives during the “positive” section and potential limitations from HCPs during the “negatives” section. All groups amended their ideas as a result of this task and the feedback round.
The suggestions for additional information requested by BCSs and common questions received by HCPs were grouped into themes (supplementary file 2, Supplementary Table 2). The most common questions related to treatment side effects and coping with emotional issues. Some suggestions reflected the discussions during the focus groups: for example, low levels of understanding regarding the risk reduction afforded by AETs and low awareness of typical symptoms were mentioned. This information was used to inform the content of a website that will supplement the ACT sessions.
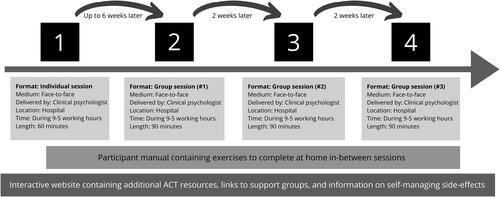
There was consensus between workshop groups in the final intervention configurations (), particularly with regard to medium (primarily face-to-face, with option of video call), day (during the working week), and additional resources (website). There were discrepancies between groups on the suggested setting and intervention deliverer. Findings from study 1 were therefore used to inform final configuration decisions.
Table 2. Final configuration suggestions from each workshop group (n = 21).
Agreeing to a final configuration
The findings from both studies were discussed within the core research team and at a multidisciplinary Trial Management Group meeting. The findings from both studies were mostly consistent, especially with regard to the medium of face-to-face (). The proposed intervention was presented to the Trial Management Group, who agreed to this configuration (). More detail on the content and therapeutic methods used in the ACTION intervention, including the specific aims of each session, are detailed in Supplementary File 2, supplementary table 4. The one-to-one session (session 1) involves a conversational assessment between the therapist and the participant on psychological flexibility to see where this could be enhanced in the participant’s day-to-day life. This includes conversations about their salient experiences of treatment (hospital and AETs) and how they approach concomitant thoughts and feelings, alongside a conversation about what is important to them. This culminates in a very brief individualized formulation suggesting some possibilities for enhancing psychological flexibility in order to enhance well-being. The following 3 group sessions give participants the opportunity to engage in group discussion, self-reflection, and experiential exercises designed to enhance different aspects of psychological flexibility. In group session 1, the focus is on enhancing contact with values and then the possibility for defusion to enable effective actions. This session includes established ACT exercises, such as Workability and Verbal Distancing.Citation34,Citation35 Group session 2 focuses on values and committed action in more detail, with exercises such as the Values Compass used to help participants clarify what’s personally meaningful then the Smallest Possible Step exercise suggested as a homework to initiate new enriching activity. In this session, participants are offered the opportunity to specifically reflect on HT decisions and side-effect management from within the framework of their own personal values. This session also gives participants the opportunity to see the possibilities for well-being within acceptance-based approaches to experiences, using established metaphors, such as Passengers on the Bus.Citation34 The final session outlines ways of stepping back from unhelpful self-stories, via exercises such as Notice Who Is NoticingCitation34 and Letting Go of Unhelpful Labels.Citation36 It also invites participants to notice whether anything experienced or learned in ACTION has been helpful.
Table 3. Comparison of results from studies 1 and 2.
Discussion
We used a co-design approach to develop an ACT-based intervention to support AET medication decisions and quality of life in BCSs. The methodology enabled us to incorporate the perspectives of both BCSs who would be eligible to participate in the group and HCPs who could be involved in delivering it.
Study 1 identified women’s difficulties with AET, their challenging experiences with the transition between treatment and survivorship, and their reports of debilitating side effects and perceived low levels of support. This is consistent with literature from the UK and the US, highlighting that BCSs desire supportive interventions at this stage in treatment.Citation12,Citation18 ACT was considered acceptable for supporting BCSs, with particular enthusiasm for exercises focused on understanding their individual values and goals and fostering self-compassion. BCSs reported skepticism around ACT’s use in relation to side effects, suggesting that this may need to be addressed when communicating with patients about this therapy. Commensurate with data showing that psychological therapists in cancer contexts favor ACT approaches,Citation27 HCPs’ feedback was similar. However, concerns were raised regarding NHS capacity to deliver such an intervention.
Study 2 involved a co-design workshop and effectively consolidated and refined the suggestions from study 1. Three mixed groups of BCSs and HCPs proposed similar intervention configurations. This workshop highlighted the perceived usefulness of providing online resources for reference between and after the sessions. Suggestions for website content were made, such as the inclusion of patient stories and practical strategies for managing side effects. Such narrative information may help women adjust to their illness and treatment.Citation37 Our data support that using patient narratives in this setting is acceptable to BCSs.
Clinical implications
We identified the period immediately following hospital-based treatment as the optimal period for delivering psychological support and information on AET. This supports epidemiological data demonstrating that the first months are likely to be key for supporting medication side effects and adherence.Citation38 There is a therapeutic opportunity for greater discussion and shared decision-making regarding AETs at this stage.Citation39 Furthermore, ensuring that consultations are patient-centered may improve patient satisfaction with informationCitation40 and increase long-term adherence to AETs.Citation12 Our intervention has been designed to be implemented rapidly within the breast cancer care pathway; however, feasibility and efficacy trials are needed prior to implementation.
Study limitations
Participants in the focus groups and workshop were similar in age and ethnicity. Therefore, key issues that may be relevant to underrepresented groups, including specific religious or cultural ideals, may be missed within the content of the intervention. The majority of BCS participants were members of breast cancer support groups, which may reduce generalizability and may have resulted in selection bias toward those who favor group-based support services. ACT is a complex psychological theory, and explaining it to a lay audience in a limited timeframe may have led to misunderstanding. This work was undertaken prior to the COVID-19 pandemic; therefore acceptability of remote interventions (eg, video calls) is likely to be underestimated. Encouragingly, in study 2, 2 of the 3 groups indicated that they would consider the option of attending the therapy sessions remotely. Understanding the acceptability of ACT in the future pilot trial will be key to confirming the data reported here.
Conclusions
Using a co-design approach, we developed an ACT-based intervention that was considered to be acceptable and feasible to both potential intervention users and deliverers. Incorporating views and preferences of both BCSs and HCPs involved in their care, a consensus was reached on the configuration of the intervention. Further research is needed to examine the actual acceptability, feasibility, and efficacy of this co-designed intervention.
Supplemental Material
Download Zip (138.4 KB)Acknowledgements
The authors acknowledge the contribution of the ACTION investigators (in alphabetical order): Rachael EllisonCitation1, Michelle CollinsonCitation1, Amanda FarrinCitation1, Robbie FoyCitation2, Suzanne HartleyCitation1, Ellen MasonCitation1, Jamie MetherellCitation1, Rebecca MottramCitation1, Richard NealCitation2, Duncan PettyCitation3, Julie SaritagCitation4, Galina VelikovaCitation1,Citation5, and Michael WolfCitation6.
1Clinical Trials Research Unit, University of Leeds, UK.
2Leeds Institute of Health Sciences, University of Leeds, UK.
3School of Pharmacy and Medical Sciences, University of Bradford, UK.
4Patient representative.
5St James’s University Hospital, Leeds & Faculty of Medicine and Health, University of Leeds, UK.
6Department of Medicine, Northwestern University, USA.
The authors would like to thank Jill Long at Yorkshire Cancer Community for her support with recruitment for both studies and all the people who participated in this project.
Disclosure statement
All authors declare they have no conflicts of interest.
Data sharing
Raw data, beyond those displayed in this article, are not shared.
Additional information
Funding
References
- Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134(2):459–478. doi:https://doi.org/10.1007/s10549-012-2114-5
- Chirgwin JH, Giobbie-Hurder A, Coates AS, et al. Treatment adherence and its impact on disease-free survival in the Breast International Group 1-98 Trial of tamoxifen and letrozole, alone and in sequence. J Clin Oncol. 2016;34(21):2452–2459. doi:https://doi.org/10.1200/JCO.2015.63.8619
- Dezentje VO, van Blijderveen NJ, Gelderblom H, et al. Effect of concomitant CYP2D6 inhibitor use and tamoxifen adherence on breast cancer recurrence in early-stage breast cancer. J Clin Oncol. 2010;28(14):2423–2429. doi:https://doi.org/10.1200/JCO.2009.25.0894
- Gabrys L, Jordan S, Schlaud M . Prevalence and temporal trends of physical activity counselling in primary health care in Germany from 1997-1999 to 2008-2011. Int J Behav Nutr Phys Act. 2015;12(1):136. doi:https://doi.org/10.1186/s12966-015-0299-9
- Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C. Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer. 2013;108(7):1515–1524. doi:https://doi.org/10.1038/bjc.2013.116
- McCowan C, Shearer J, Donnan PT, et al. Cohort study examining tamoxifen adherence and its relationship to mortality in women with breast cancer. Br J Cancer. 2008;99(11):1763–1768. doi:https://doi.org/10.1038/sj.bjc.6604758
- Winn AN, Dusetzina SB. The association between trajectories of endocrine therapy adherence and mortality among women with breast cancer. Pharmacoepidemiol Drug Saf. 2016;25(8):953–959. doi:https://doi.org/10.1002/pds.4012
- Yood MU, Owusu C, Buist DS, et al. Mortality impact of less-than-standard therapy in older breast cancer patients. J Am Coll Surg. 2008;206(1):66–75. doi:https://doi.org/10.1016/j.jamcollsurg.2007.07.015
- Bluethmann SM, Murphy CC, Tiro JA, Mollica MA, Vernon SW, Bartholomew LK. Deconstructing decisions to initiate, maintain, or discontinue adjuvant endocrine therapy in breast cancer survivors: a mixed-methods study. Oncol Nurs Forum. 2017;44(3):E101–E111. doi:https://doi.org/10.1188/17.ONF.E101-E110
- Brett J, Boulton M, Fenlon D, et al. Adjuvant endocrine therapy after breast cancer: a qualitative study of factors associated with adherence. Patient Prefer Adherence. 2018;12:291–300. doi:https://doi.org/10.2147/PPA.S145784
- Cahir C, Dombrowski SU, Kelly CM, Kennedy MJ, Bennett K, Sharp LJ . Women’s experiences of hormonal therapy for breast cancer: exploring influences on medication-taking behaviour. Support Care Cancer. 2015;23(11):3115–3130. doi:https://doi.org/10.1007/s00520-015-2685-x
- Kahn KL, Schneider EC, Malin JL, Adams JL, Epstein AMJ. Patient centered experiences in breast cancer: predicting long-term adherence to tamoxifen use. Med Care. 2007;45(5):431–439. doi:https://doi.org/10.1097/01.mlr.0000257193.10760.7f
- Coombes RC, Hall E, Gibson LJ, et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med. 2004;350(11):1081–1092. doi:https://doi.org/10.1056/NEJMoa040331
- Cuzick J. Aromatase inhibitors for breast cancer prevention. J Clin Oncol. 2005;23(8):1636–1643. doi:https://doi.org/10.1200/JCO.2005.11.027
- Howell A, Cuzick J, Baum M, et al . Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365(9453):60–62. doi:https://doi.org/10.1016/S0140-6736(04)17666-6
- Heiney SP, Parker PD, Felder TM, Adams SA, Omofuma OO, Hulett JM. A systematic review of interventions to improve adherence to endocrine therapy. Breast Cancer Res Treat. 2019;173(3):499–510. doi:https://doi.org/10.1007/s10549-018-5012-7
- Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol. 2013;4:91. doi:https://doi.org/10.3389/fphar.2013.00091
- Harrow A, Dryden R, McCowan C, et al. A hard pill to swallow: a qualitative study of women’s experiences of adjuvant endocrine therapy for breast cancer. BMJ Open. 2014;4(6):e005285. doi:https://doi.org/10.1136/bmjopen-2014-005285
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and Commitment Therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25. doi:https://doi.org/10.1016/j.brat.2005.06.006
- Graham CD, Gouick J, Krahé C, Gillanders D. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev. 2016;46:46–58. doi:https://doi.org/10.1016/j.cpr.2016.04.009
- Hann KEJ, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain. J Context Behav Sci. 2014;3(4):217–227. doi:https://doi.org/10.1016/j.jcbs.2014.10.001
- A-Tjak JG, Davis ML, Morina N, Powers MB, Smits JA, Emmelkamp PMJP. A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychother Psychosom. 2015;84(1):30–36. doi:https://doi.org/10.1159/000365764
- Feros DL, Lane L, Ciarrochi J, Blackledge J. Acceptance and Commitment Therapy (ACT) for improving the lives of cancer patients: a preliminary study. Psycho-Oncol. 2013;22(2):459–464.
- Marín FM, Soriano MCL. Acceptance of relapse fears in breast cancer patients: effects of an ACT-based abridged intervention. Psicooncología: investigación y Clínica Biopsicosocial en Oncología. 2016;13(1):7–21.
- Johns SA, Stutz PV, Talib TL, et al. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: a 3‐arm pilot randomized controlled trial. Cancer. 2020;126(1):211–218. doi:https://doi.org/10.1002/cncr.32518
- Chunxiao Z, Lizu L, Lin Z, et al. The effects of acceptance and commitment therapy on the psychological and physical outcomes among cancer patients: a meta-analysis with trial sequential analysis. J Psychos Res. 2020;140:110304.
- Thewes B, Brebach R, Dzidowska M, Rhodes P, Sharpe L, Butow P. Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psychooncology. 2014;23(4):390–396. doi:https://doi.org/10.1002/pon.3423
- Matza LS, Park J, Coyne KS, Skinner EP, Malley KG, Wolever R. Derivation and validation of the ASK-12 adherence barrier survey. Ann Pharmacother. 2009;43(10):1621–1630. doi:https://doi.org/10.1345/aph.1M174
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:https://doi.org/10.1191/1478088706qp063oa
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:https://doi.org/10.1093/intqhc/mzm042
- De Bono E. Six Thinking Hats. UK: Penguin; 2017.
- NHS Institute for Innovation and Improvement. Thinking differently. 2007.
- NHS Health Research Authority. http://www.hra-decisiontools.org.uk/research/
- Harris R. 2019. ACT Made Simple: An Easy-to-Read Primer on Acceptance and Commitment Therapy. New Harbinger Publications.
- Hayes SC, Hofmann SG, eds. 2018. Process-Based CBT: The Science and Core Clinical Competencies of Cognitive Behavioral Therapy. Oakland, CA: New Harbinger Publications.
- Rose MR, Norton S, Vari C, et al. Acceptance and Commitment Therapy for muscle disease (ACTMus): protocol for a two-arm randomised controlled trial of a brief guided self-help ACT programme for improving quality of life in people with muscle diseases. BMJ Open. 2018;8(10):e022083. doi:https://doi.org/10.1136/bmjopen-2018-022083
- Entwistle VA, France EF, Wyke S, et al. How information about other people’s personal experiences can help with healthcare decision-making: a qualitative study. Patient Educ Couns. 2011;85(3):e291–e8. doi:https://doi.org/10.1016/j.pec.2011.05.014
- Smith SG, Sestak I, Howell A, Forbes J, Cuzick J. Participant-reported symptoms and their effect on long-term adherence in the International Breast Cancer Intervention Study I (IBIS I). J Clin Oncol. 2017;35(23):2666–2673. doi:https://doi.org/10.1200/JCO.2016.71.7439
- Barry MJ, Edgman-Levitan S . Shared decision making-pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi:https://doi.org/10.1056/NEJMp1109283
- Mallinger JB, Griggs JJ, Shields CG . Patient-centered care and breast cancer survivors’ satisfaction with information. Patient Educ Couns. 2005;57(3):342–349. doi:https://doi.org/10.1016/j.pec.2004.09.009