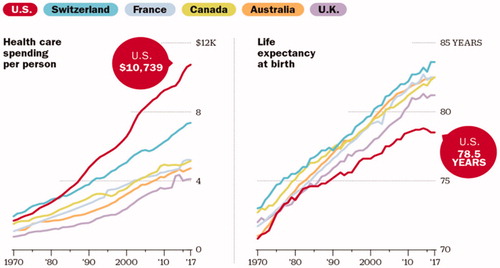
Over that last couple of decades, we have seen an explosive increase in healthcare costs in the United States including the cost of cancer drugs, testing/imaging, and hospitalization with vast amounts for administration. Almost no aspect of the healthcare system has failed to be directly or indirectly impacted by the increase in costs which have far exceeded the more gradual rise in the Gross Domestic Product. As many of us have pointed out, the US healthcare system is perhaps the ‘poster child’ for such runaway increases in healthcare expenditures most notably with skyrocketing cancer drug prices (Citation1). Healthcare costs in the United States clearly represents an outlier compared to healthcare costs in other developed industrialized nations and continues to lag behind most industrialized countries in life expectancy at birth representing the only developed country where life expectancy has actually been decreasing in the most recent years () (Citation2). The concerning decline in life-expectancy in the US, when other major Western nations have demonstrate a continued rise, suggests that millions of lives are being cut short with current efforts.
Figure 1 . Health care spending and life expectancy in US and other developed countries (Citation2).
Financial Burden: The US healthcare system has absolutely failed to tackle the steep increases in costs and continues to rely on the dictum of pricing healthcare ‘to the extent that the market will bear’ ignoring entirely, what individuals including patients and families ‘can bear’. This has reached crisis proportions in the US as insurers have passed on an increasing proportion of healthcare costs to patients through rising copays, lowering caps, frequent denials of coverage and overall policies that fail to address the high costs associated with many devastating healthcare conditions such as cancer. Various stop-gaps approaches have and are being implemented to try to stem the tide of these increasing costs and their impact on patients including: 1) the development of generic medications, biosimilars of the exciting but extraordinarily expensive novel biologic therapies, 2) greater price transparency for drugs, tests and hospitalization, 3) inventive but unproven payment and reimbursement models among many others and 4) frequent calls for value-based pricing including Value Frameworks from both the American Society of Clinical Oncology (ASCO) and the European Society of Medical Oncology (ESMO) all of which remain conceptual and in limbo (Citation3,Citation4). There have even been calls from major thought leaders for patient-driven initiatives including petitions to lower the high price of cancer drugs (Citation5). However, these are but band aids placed on large gaping wounds in the healthcare system that are hemorrhaging, threatening and sometimes killing patients who are the most vulnerable.
Financial Toxicity: In recent years, it has become popular and appropriate to refer to this increasingly impactful and often toxic exposure to rising healthcare costs and the financial burden placed on patients and their families as ‘financial toxicity’ (Citation6,Citation7). This places the impact of costs squarely on the level of other major adverse effects and toxicities that patients experience with serious life-threatening diseases like cancer and treatments such as chemotherapy, radiation therapy and surgery. It also begs for a discussion of financial adverse effects with patients and families similar to discussions about other treatment-related toxicities along with the overall benefits and harms of treatment. Cancer is one of the most expensive medical settings generally including diagnosis, staging, treatment, supportive care, emergency care and hospitalizations, survivorship care, and end-of-life costs. The National Cancer Institute defines financial toxicity as a term to describe “problems a patient has related to the cost of medical care such as not having health insurance or having a lot of costs for medical care not covered by health insurance can cause financial problems and may lead to debt and bankruptcy. Financial toxicity can also affect a patient’s quality of life and access to medical care. For example, a patient may not take a prescription medicine or may avoid going to the doctor to save money.”
In addition to the multiple costs associated with cancer care, the extent and depth of financial toxicity experienced will depend on individual and family wealth, income, debt, ability to work, health and disability insurance coverage. Surveys suggest that at least a quarter or more of cancer patients experience what they consider to be financial toxicity (Citation8). Various measurement instruments have been developed and validated in an effort to better quantitate and track drivers of financial toxicity and its consequences. There include the Comprehensive Score for Financial Toxicity (COST), the Breast Cancer Finances Survey (BCFS) inventory and the Socioeconomic Wellbeing Scale (Citation9). Unfortunately, these often fail to capture the most devasting predictors of financial toxicity and are not routinely included in clinical trials or observation data repositories. Greater risk of financial toxicity is seen in patients with more advanced or recurrent cancer and those with multiple cancers or other major medical conditions. Greater financial toxicity appears to be experienced by minorities, the economically disadvantaged, un- or under-employed individuals, the less formally educated, younger cancer patients and survivors of childhood cancer and is almost always accompanied by considerable emotional distress (Citation10,Citation11). In a study of 1202 adult cancer survivors identified in the Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Questionnaire, material or psychological financial hardship were reported in 40% of surveyed individuals under 65 (Citation12). More recently, a longitudinal study of the Health Retirement Study evaluated financial toxicity in 9.5 million newly diagnosed cancer patients over 50 years of age between 2000 and 2012 (Citation13). By year 2, over 42% had depleted their entire life’s assets with greater loss among women and those retired, of older age and either uninsured or on Medicaid along with individuals with progressive cancer and/or multiple major comorbidities. By year 4 following diagnosis, nearly 40% remained financially insolvent with significantly greater risk among the same demographic, socioeconomic and clinical factors in multivariable analysis (Citation13).
Increasingly, authors and professional organizations have called for full disclosure and routine discussion of treatment costs with patients as an essential element of cancer care leading to truly informed consent and shared decision making after all potential benefits and harms have been disclosed and discussed. At the same time, providers have been challenged to fully understand the financial impact of their clinical recommendations due to the complexity of the US healthcare system and the enormous variation in insurance coverage associated with different policies, plans, caps, co-payments, deductibles, co-insurance and a variety of limitations often placed in the fine print. While there has been increasing reliance by practitioners on administrative staff including trained financial counselors, these discussions are often generic and unable to accurately pinpoint the individual patient’s ultimate financial responsibility due to the complexity and uncertainty of current healthcare financing. Finally, the impact of financial toxicity on cancer survivors and families is multifaceted and often profound including the ability to receive or continue expensive treatments, further debt and bankruptcy, lower length and quality of life associated with poor physical and emotion health, poor social engagement, anxiety and depression including fear of cancer recurrence, and suicidal ideation (Citation11).
Financial Abuse: In oncology, we are now faced with a system where the optimal effective therapy is a novel biologic agent that at the time of approval is priced somewhere north of $10,000/month which is several fold higher than the median family household income in the US which has remained essentiallyflat over the last few decades (Citation14). At the same time, the price of these novel therapies at the time of approval only represents the starting price point for launching further startling increases to levels several fold higher often amounting to hundreds of thousands of dollars for a typical course of therapy. As a result, patients are being severely blind-sided by enormous surprise medical bills later in their disease course. When they are unable to meet these financial responsibilities, as is often the case, patients are increasingly being threatened or actively sued by the health system charged with their care. It is essential that we bring the enormous financial burden being inflicted on our patients out of the shadows and into the light. This amounts to nothing less than financial abuse that our healthcare system is inflicting on our most vulnerable populations including women and virtually all minorities in our society. Financial abuse is being perpetrated on those unable to work due to family obligations, childcare, or overt employer bias or, if employed, are being systematically under-payed, offered little or no health benefits including benefits that are most needed by these vulnerable populations. We have been rightfully appalled at the physical and emotional abuse in the work place and elsewhere that has been present but only recent brought to the surface often years after it occurred, and yet have largely ignored the financial abuse that our healthcare system has inflicted on patient and families due with limited or no ability to pay and mounting physical, emotional and economic challenges. Like other forms of abuse, the abuse of individuals due to exploding healthcare costs and expanding financial burden placed on patients, societal tolerance of these abusive practices should not and cannot be tolerated any modern health system or society. Women, minorities, and all afflicted populations need protection and care that is commensurate with our obligation as healthcare providers, institutions, payers and compassionate people.
Financial Torture: As discussed above, we have come to recognize that the financial burden that modern cancer care and our health system imposes on our patients is akin to other forms of both physical and emotional toxicity and abusive behavior that we have increasing called out in other modern social interactions. At the same time, it is essential that we now consider more thoroughly the most egregious, sustained, and harmful effects of financial toxicity and abuse nearly always inflicted by anonymous, shadowy individuals without any transparency, disclosure or consent. It is not at all an exaggeration, that the result of a patient’s inability to meet an extraordinary, unexpected and rapidly increasing financial burden often leads to verbal or written threats, intimidation, and even coercion from the very institutions and forces charged with caring, healing and comforting patients. Coercion may start with being required to sign a virtually unlimited financial obligation for a costly but urgent and potentially life-saving procedure or wait for preapprovals that may take days, weeks or may never come. Coercion becomes even more sinister when patients with limited or no ability to pay for exorbitant treatments costs are forced to choose between refusing or stopping effective treatment early or the agonizing choice of placing their family in dire financial straits including loss of home, livelihood, financial security, malnutrition, or even life itself (Citation13). Studies have clearly demonstrated increased rates of home mortgages, bankruptcy, and mortality including suicide by those with extreme financial threats (Citation15). We can think of no term that better equates with such experiences of extreme financial, emotional and even physical injury than the term torture. Similar perspectives have been taken by the courts when incarcerated individuals have been refused health care and the torture inflicted on our patients deprived of proper cancer care cannot be viewed as anything less.
Torture has been defined as an act by which severe pain or suffering, whether physical or mental, is intentionally inflicted on a person for any reason including intimidation or coercion, or for any reason based on discrimination of any kind. The World Medical Association defines torture as the deliberate, systematic or wanton infliction of physical or mental suffering by one or more persons acting alone or on the orders of any authority, to force another person to yield information or for any other reason. It further states that a physician shall not countenance, condone or participate in the practice of torture or other forms of cruel, inhuman or degrading activities. It is no surprise that survivors of torture of any kind often suffer from physical and psychological symptoms and ongoing disabilities. No aspect of this can ever be considered necessary or acceptable. Clinicians should not be complicit with this ongoing crisisby failing to understand the financial consequences of our treatment recommendations, properly informing vulnerable patients of the financial risks in addition to physical ones, and supporting patients emotionally as well as by providing guidance toward resources that may partially mitigate the financial trauma that awaits them. At the same time, we must urgently and rapidly act to bring the American healthcare system in all of its complexities into alignment with our moral, ethical and social understanding of fairness, compassion, and justice and eliminate the injustice, abuse and, yes, even torture, that is being inflicted routinely on many of the most vulnerable members of our society.
References
- Ramsey SD, Lyman GH, Bangs R. Addressing skyrocketing cancer drug prices comes with tradeoffs: pick your poison. JAMA Oncol. 2016;2(4):425–426. doi:10.1001/jamaoncol.2015.5813.
- Case A, Deaton A. How healthcare costs hurt American workers and benefit the wealthy. Time. 2020.
- Schnipper LE, Davidson NE, Wollins DS, Blayney DW, Dicker AP, Ganz PA, et al. Updating the American Society of Clinical Oncology value framework: revisions and reflections in response to comments received. JCO. 2016;34(24):2925–2934. doi:10.1200/JCO.2016.68.2518.
- Schnipper LE, Davidson NE, Wollins DS, Tyne C, Blayney DW, Blum D, et al. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. JCO. 2015;33(23):2563–2577. doi:10.1200/JCO.2015.61.6706.
- Tefferi A, Kantarjian H, Rajkumar SV, Baker LH, Abkowitz JL, Adamson JW, et al. In support of a patient-driven initiative and petition to lower the high price of cancer drugs. Mayo Clin Proc. 2015;90(8):996–1000. doi:10.1016/j.mayocp.2015.06.001.
- Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153–165. doi:10.3322/caac.21443.
- Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109:djw205.
- Knight TG, Deal AM, Dusetzina SB, Muss HB, Choi SK, Bensen JT, et al. Financial toxicity in adults with cancer: adverse outcomes and noncompliance. JOP. 2018;14(11):e665–e673. doi:10.1200/JOP.18.00120.
- Witte J, Mehlis K, Surmann B, Lingnau R, Damm O, Greiner W, et al. Methods for measuring financial toxicity after cancer diagnosis and treatment: a systematic review and its implications. Ann Oncol. 2019;30(7):1061–1070. doi:10.1093/annonc/mdz140.
- de Souza JA, Yap BJ, Wroblewski K, Blinder V, Araújo FS, Hlubocky FJ, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer. 2017;123(3):476–484. doi:10.1002/cncr.30369.
- Huang I-C, Bhakta N, Brinkman TM, Klosky JL, Krull KR, Srivastava D, et al. Determinants and consequences of financial hardship among adult survivors of childhood cancer: a report from the St. Jude Lifetime Cohort Study. J Natl Cancer Inst. 2019;111(2):189–200. doi:10.1093/jnci/djy120.
- Yabroff KR, Dowling EC, Guy GP, Banegas MP, Davidoff A, Han X, Jr, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–267. doi:10.1200/JCO.2015.62.0468.
- Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or debt? National estimates of financial toxicity in persons with newly-diagnosed cancer. Am J Med. 2018;131(10):1187–1199 e5. doi:10.1016/j.amjmed.2018.05.020.
- Prasad V, De Jesus K, Mailankody S. The high price of anticancer drugs: origins, implications, barriers, solutions. Nat Rev Clin Oncol. 2017;14(6):381–390. doi:10.1038/nrclinonc.2017.31.
- Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. JCO. 2016;34(9):980–986. doi:10.1200/JCO.2015.64.6620.
