Abstract
Radiotherapy is one of the major approaches to cancer treatment. Artificial intelligence in radiotherapy (shortly, Intelligent radiotherapy) mainly involves big data, deep learning, extended reality, digital twin, radiomics, Internet plus and Internet of Things (IoT), which establish an automatic and intelligent network platform consisting of radiotherapy preparation, target volume delineation, treatment planning, radiation delivery, quality assurance (QA) and quality control (QC), prognosis judgment and post-treatment follow-up. Intelligent radiotherapy is an interdisciplinary frontier discipline in infancy. The review aims to summary the important implements of intelligent radiotherapy in various areas and put forward the future of unmanned radiotherapy center.
Introduction
According to the International Agency for Research on Cancer (IARC) of the World Health Organization, 19.3 million new patients and 10 million deaths of cancer are projected to occur in 2020 worldwide (Citation1). Globally, one in five people will develop cancer in their lifetime, and one in eight men and one in 11 women will die from the disease. By 2040, 28.4 million new cancer cases are expected globally, a 47 percent increase from 2020, with the largest increases in low - and moderately developed countries (95 percent and 64 percent, respectively).
As one of the five main treatment options for malignant tumors, radiotherapy uses artificial or natural radiation to treat malignant tumors and/or subclinical sites and is required by up to 70% of cancer patients at different stages (Citation2). The World Health Organization reported that 55% of malignant tumors can be cured by surgery (27%), radiotherapy (22%) or chemotherapy (6%). During the past 120 years, radiotherapy equipment has developed from deep X-ray therapy machines and 60Co machines to linear accelerators and proton and heavy ion accelerators; radiotherapy technology has also evolved from two-dimensional radiotherapy to three-dimensional or even four-dimensional precision radiotherapy (Citation3–7), including three-dimensional conformal radiotherapy (3 D-CRT), intensity modulated radiotherapy (IMRT), Volumetric modulated arc therapy (VMAT), Image-guided radiation therapy (IGRT), etc.
Artificial intelligence (AI) studies and develops the theory, method, technology and application of human intelligence, simulating and extending human intelligence with the actual term of machine intelligence (Citation8). In medical and health fields, AI provides medical image processing, genomics, pathological diagnosis, drug development, cell simulation, telemedicine, health management, wearable development, extended reality and intelligent hospital construction (Citation9–11). Furthermore, AI affords the revolution of radiotherapy process with the automation and intelligence in 3 D-reconstruction, image processing, machine vision, language editing, reality visualization, and so on (Citation12–14). Target contouring and treatment planning are the center of the whole radiotherapy process and the pioneer for computational support. With the improvement of automation and intelligence, radiation oncologist could spare more time to enhance the radiotherapy process, quality assurance (QA) and quality control (QC).
Artificial intelligence in radiotherapy (shortly, Intelligent radiotherapy) is an interdisciplinary frontier discipline in infancy. We have searched the terms of “Artificial intelligence” and “Radiotherapy” in Pubmed, selected the related literatures and filtered the repeat reports in this study. The review aims to summary the important implements of intelligent radiotherapy in various areas and put forward the future of unmanned radiotherapy center, helping radiation oncologist deeply think how to actively adapt and improve themselves in the era of intelligent radiotherapy.
Big data in intelligent radiotherapy
With the high development of Internet and cloud platform, computer equipment is integrated by the network. The frequent data exchange between host and terminal finally promotes the rapid rise of big data (Citation15). Big data is a kind of data set that greatly exceeds the capacity of traditional database software in data acquisition, storage, management and analysis. It has five characteristics: large volume of data content, fast speed of data generation, diversity of data types, low value density and authenticity (Citation16,Citation17). In medical big data, high-dimensional unstructured data such as image data (CT, MRI, PET-CT, ultrasound, etc) is the most important part. These unstructured data needs to be structured, and relevant diseases need to be mined by using knowledge map, support vector machine and neural network (Citation18–22). Source of radiotherapy big data includes radiotherapy image data, radiotherapy process data (tumor diagnosis, medical history, laboratory examination, etc.), simulation positioning data, radiotherapy planning data, treatment delivery data, and QA & QC data. Even, omics big data is very critical, including genomics, metabolomics, proteomics, lipomics, transcriptomics, immunomics, glycomics and imageomics (Citation23–25). All the general view of big data, patient preferences, clinical characteristics and a series of treatment options could be used to make a personal radiotherapy, which comprises the big datasets of radiotherapy technology and clinical information (Citation26). These synthesizing clinical and genomic data improve the decision-making and evidence level in personalized radiotherapy.
Definition of intelligent radiotherapy
The basis of machine intelligence is computing, with the core being machines that can learn. Machine intelligence usually includes natural language processing, computer vision, cognition and reasoning, machine learning and so on. AI has promised to revolutionize radiotherapy. Among the machine intelligence, two main research fields are closely related to radiotherapy, i.e., computer vision and machine learning (Citation27,Citation28).
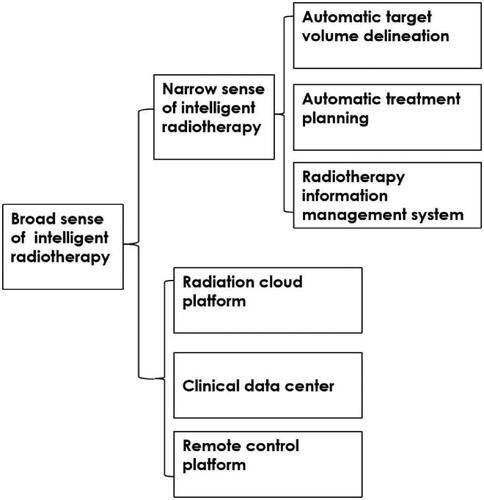
Intelligent radiotherapy could be defined into two scopes. In a narrow sense, intelligent radiotherapy realizes radiotherapy process management mainly based on single-center. It replaces the medical staff's repetitive, labor-intensive, time-consuming radiotherapy-related work, including medical record information management, target volume delineation, treatment plan design, quality control, and tumor control evaluation. In a broad sense, intelligent radiotherapy refers to a multi-center, wide-area intelligent radiotherapy technology based on remote multi-center regional collaborative development. It is based on the construction of the Internet plus radiotherapy cloud platform for intelligent radiotherapy (Citation29). Through the establishment of the block chain radiotherapy system, the application of the edge computing radiotherapy platform, the collection of radiotherapy information of wearable equipment, and the use of 5 G communication with high-speed transmission, an advanced remote network system of intelligent radiotherapy is built to further promote radiotherapy sharing technology ().
Automatic contouring in radiotherapy
It is of great significance to use artificial intelligence to realize automatic target volume delineation, which is not disturbed by human factors and easy to achieve rapid, accurate and homogenized automatic outline of radiotherapy (Citation30–32). There are three basic techniques of intelligent target volume delineation, including template spectrum library, image segmentation and deep learning. Machine learning is the promising way to realize the automatic recognition and anatomical location of tumors, and complete the automatic segmentation of tumors, non-tumor tissues and regions of interest (Citation33). Radiologists only need to review, fine-tune and modify the images after automatic segmentation. It can be used for clinical treatment, greatly reducing the workload of radiotherapy oncologists. In addition, through intense learning, computers can obtain image details and feature states that may be ignored or imperceptible by human beings. Once machine learning is completed, only one calculation is needed to get the processing results when a new sample arrives. At this time, the processing time is very short, which would exponentially reduce the work time, improve the efficiency of radiotherapy oncologists, and reduce differences in the delineation of radiotherapy target volume among radiotherapy oncologists and radiotherapy units.
On head and neck organs at risk (OARs), Van Dijk et al. (Citation34) proposed a deep learning contouring trained in 589 patients. Compared to atlas-based automatic contouring (ABAS) algorithms currently used clinically, deep learning contouring (DLC) resulted in equal or improved in 19 out of 22 OARs by dice similarity coefficient (DICE), an often used methodology to compare and analyze the similarity coefficient between automatic contour and manual contour. DLC had the DICE 0.74, better than the DICE 0.59 in ABAS. Song Y et al. (Citation35) constructed 2 convolutional neural networks (CNNs) for rectal cancer radiotherapy contouring, ResUNet detects low-level visual features for bladder and femoral head contouring, DeepLabv3+ extracts high-level semantic features with advantages in contouring CTV and the small intestine. As a result, the 2 CNNs displayed high quality delineation and low time consumption based on computation and manual correction.
Automatic planning in radiotherapy
Using big data's intelligent learning of radiotherapy, introducing knowledge-based treatment planning into TPS, and integrating previous treatment experience into the treatment decisions of new patients could significantly improve the efficiency of radiotherapy planning optimization and avoid blind subjectivity of human factors. At present, the main exploration and development directions of intelligent plan design include dose calculation based on artificial intelligence’s neural network and DVH prediction model based on big data's deep learning method (Citation36). Intelligent radiotherapy planning system will analyze the current patient information, such as the location relationship between the target area and OARs, automatically predict the distribution interval of DVH, so that clinical planners can quickly obtain the set value of objective function (such as volume dose relationship, weight factor, etc.). Thus AI can improve the quality of planning and design, improve the efficiency of planning and design, improve the consistency of planning schemes, and reduce the uncertainty caused by human factors (Citation37–40).
It can be expected that after completion and verification of the intelligent delineation of the radiotherapy target and endangered organs, the TPS intelligent plan design will be used to confirm the radiation field distribution design and virtual dose simulation by the radiotherapy physicist according to prescription dose, and carry on the intelligent design and optimization of the radiotherapy plan (Citation41,Citation42). According to the specific conditions of different patients, the optimal solution could be obtained quickly and efficiently.
Intelligent QA & QC in radiotherapy
QA & QC is the guarantee of radiotherapy quality, the basis of tumor control rate and the cornerstone of the development of precision radiotherapy. QA & QC mainly includes radiotherapy scheme, radiotherapy plan, dose verification, radiotherapy equipment, etc., which requires a lot of time and manpower. Intelligent radiotherapy quality control is expected to solve the current difficulties.
With the support of intelligent information system and under the daily quality control rules and regulations, intelligent QA & QC program could automatically start the appropriate instruments at an appropriate time from the planning stage, execution stage, inspection stage to processing stage. It involves the schedule work of radiotherapy physicians, physicists and technicians. All of these results are uploaded to the big data management center to facilitate the automatic quality analysis, problem solution, then ensure the high precision and high efficiency of radiotherapy delivery (Citation43,Citation44).
For the Intelligent QA & QC of radiotherapy equipments, the radiotherapy information system automatically provides the equipment management module to record and query the daily monitoring report, alarm the equipment failure, and remind relevant staff to deal with the problems. Intelligent QA & QC could effectively improve daily, weekly and monthly inspection of radiotherapy equipments, ensure the accuracy of treatment angle and dose distribution, and keep the accelerator to normally operate in good condition.
Extended reality technology in intelligent radiotherapy
Broadly speaking, extended reality technology includes virtual reality (VR), augmented reality (AR) and mixed reality (MR). VR is a human-computer interactive technology that combines a computer system, image display and a sensor (Citation45), in which the user is immersed in an entirely fabricated world. AR and MR, however, do not replace the real world with a virtual one; instead, they are the fusion of computer-generated objects with the real world to generate the effect that the individual is interacting with the visible environment. Extended reality technology can vividly simulate the whole process of radiotherapy, identify problems during the process, and correct them in a timely manner (Citation46–49).
Determining how to achieve fast and accurate positioning is a future development direction of intelligent radiotherapy. The VR system VERT shows great potential in this respect, in which a 360-degree camera can be installed in the accelerator room to capture the actual patient position in a real radiotherapy room for 3 D reconstruction simulation, and radiotherapy workers can manipulate virtual patients as easily as moving a computer mouse. VERT also provides a number of training tools that help doctors explain specific concepts of radiotherapy to patients, such as the isocenter concept and automated placement of skin tattoo marks on virtual patients. Patients and relatives were shown a standard room where radiotherapy is given, a linear accelerator, and how radiotherapy is planned and delivered. Thus VR reduced anxiety in new patients.
Immersive extended reality technology could help optimize treatment planning and provide a better understanding of dose distribution in the body. The spatial relationship is easier to understand when stereoscopic visualization is carried out in a 3 D environment. Johnson K et al. (Citation50) acquired a 360-degree VR video to simulate the delivery of one fraction of image-guided external beam radiation therapy to the pelvis.
Digital twin in intelligent radiotherapy
The digital twin initiative aims to revolutionize healthcare for the benefit of citizens and society through the creation of Digital Twin—computer model of individuals that allow the identification of the best therapy, prevention or health maintenance measure and reflect changes in patients in a virtual space, representing the corresponding life cycle of the subject (Citation51,Citation52). In the future, each device in the radiotherapy center could be compatible with the digital twin approach. The engineer would obtain the operation data of the radiotherapy equipment monitoring system in real time, carry out fault prediction and timely maintenance, and achieve remote assistance, operation and emergency commands (Citation53). In the process of radiotherapy planning, using a digital twin can improve the accuracy of planning, predict the doses patients will require in real life, and effectively control the dose delivery to target regions. In the process of image guidance, the digital twin can be used to accurately predict the radiation dose delivered to organs at risk, which in turn, helps doctors determine whether they need to adjust and modify the plan to effectively protect vital organs, especially in patients whose planned doses are close to the threshold. In the verification of the radiotherapy plan, the digital twin can be used to copy the digital model that is identical to the patient, including the appearance and internal organs, and monitor changes in the functions of various organs. Thus, the patient’s dose can be verified more accurately. Radiation oncologists can evaluate the effect of the radiation dose on patients. In radiotherapy implementation, use of digital twin can improve the accuracy of positioning, predict the actual exposure of patients, and detect in real-time the actual exposure dose patients will receive in the real environment. Coenen A et al. (Citation54) utilized digital twin models for the detection of hemodynamically relevant coronary stenosis, and the diagnostic accuracy reached 85%, increased from the 71% rate achieved by computed tomographic angiography alone.
Intelligent radiotherapy guided by radiomics
Radiomics refers to the high-throughput extraction and analysis of tumor features from medical images obtained by CT, MRI and PET, reflecting the spatial-temporal heterogeneity of tumors in cancer patients and radiotherapy patients (Citation55,Citation56). Its process includes image collection, segmentation of the region of interest, feature extraction, statistical analysis, classification and prediction. The images are mainly collected from CT, MRI and PET, which effectively promotes the precision of radiotherapy for cancers (Citation57,Citation58).
Radiomics can predict the curative effect of stereotactic body radiotherapy (SBRT). Through the analysis of imaging characteristics in patients with lung tumors before and after treatment, researchers found that treatment efficacy is significantly related to changes in imaging features, and the prediction model could have certain guiding significance for patient prognosis (Citation59). Radiomics can predict cancer recurrence and metastasis, with superior accuracy versus traditional prediction indexes (Citation60). Radiomics can also predict adverse reactions to radiotherapy. A report compared and analyzed 20 texture features of CT images in patients with lung cancer before and after radiotherapy and confirmed that the difference in eigenvalues increases gradually with the radiation doses. Combined with image features, the accuracy in predicting radiation pneumonitis could be improved from 0.59 to 0.84 (Citation61).
Internet plus and remote radiotherapy service
The development of the Internet has had a tremendous impact (with revolutionary innovation) on all areas of life, including the medical industry (Citation62,Citation63). The precision cloud radiotherapy platform is the embodiment of the Internet plus and remote radiotherapy service, which can effectively solve the problems of a shortage of radiotherapy professionals and a lack of information (Citation64,Citation65). Through the Internet, big data, cloud computing, cloud services and other technical means, the integration of high-quality radiotherapy resources, research and development of accurate cloud quality control, cloud planning, and other network information systems are possible. Precision cloud radiotherapy technology relies on a strict radiotherapy cloud quality control system and uploads patient information and image data to the cloud platform through the Internet; then, experts designated by higher-level hospitals delineate target volumes and design a radiotherapy plan. After the treatment plan is examined and confirmed according to the quality control requirements of the expert hospital, the data are transmitted back to the treatment planning system of the radiotherapy center of the lower-level hospital. The treatment plan is then re-examined and confirmed by the radiotherapy experts at that hospital; finally, patient treatment is carried out through the network of the treatment system at the radiotherapy center. Through this cooperative work of superior and subordinate hospitals, accurate radiotherapy programs can be provided in primary hospitals. In other words, via the implementation of whole-process guidance, evaluation and monitoring of radiotherapy, patients can obtain high-quality, high-standard, personalized, accurate and safe cancer diagnosis and treatment services locally, minimizing diagnosis and treatment costs and improving patient survival.
Unmaned intelligent radiotherapy center
Currently, due to the sharp imbalance between the huge demand for radiotherapy and the limited supply, it is necessary to realize the automation and intelligence of radiotherapy as soon as possible (Citation66–69). The unmaned intelligent radiotherapy center is a new unattended radiotherapy modality that implements intelligent radiotherapy and Internet of Things (IoT) to provide patients with self-help intelligent radiotherapy.
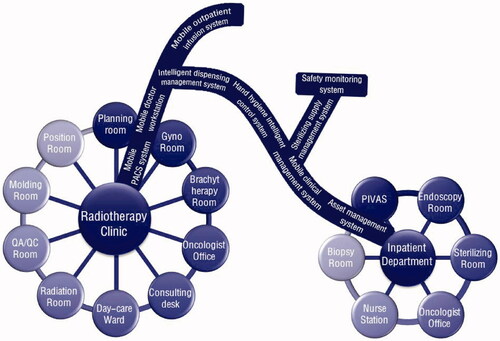
IoT is the Internet connected with things, refers to the technical mode of Internet, which is based on communication sensing technologies such as network radio frequency identification and combines the agreed communication protocol with the Internet to realize the intelligent identification and management of item information, so as to form a network through interconnection (Citation70). The main features are comprehensive sensing, reliable transmission and intelligent processing. Integrating IoT into radiotherapy services can simplify radiotherapy procedures, optimize service mode, and achieve the goal of convenient, fast and safe services. The IoT is architectured by perception layer with kinds of sensors to locate the patients and perceive the life situation, network layer with Wireless Local Area Network (WLAN) to transmit big data, supporting technology layer to ensure the identity authentication and the information security, and application layer to cover the radiotherapy process from pre-treatment to post-treatment periods. The design of IoT in radiotherapy unit integrates various configurations such as radiotherapy clinic, radiotherapy room, day ward and inpatient ward ().
Since the radiotherapy is a complicated process, the essential condition of unmaned intelligent radiotherapy center includes the intelligent communication with patients. Except for extended reality technology, chatbot is other intelligent communication way. AI-assisted chatbot becomes a hotspot for conversational service, education and patient care (Citation71). It’s convenient for the radiotherapy patients to talk with a virtual person based on the platforms of Internet plus and IoT. There is a two-way communication system between the chatbot and user, which help the radiotherapy patients to make their appointments, and solve the problems by crucial information related to their radiotherapy.
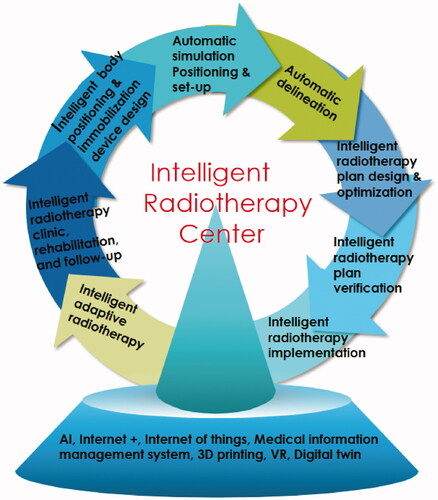
With these approaches, fewer medical staff are required for the whole radiotherapy process. We present the following ideas for the establishment of an unmanned intelligent radiotherapy center ().
First, patient information collection and follow-up are automatically and intelligently processed, which could realize the integration of humans and machines in medical decision-making. Mobile medical products and the IoT can also provide services for patients and their relatives, including whole-process disease management, systematic patient education, customized rehabilitation nutrition program delivery, and timely communication between doctors and patients. Through seamless docking with radiotherapy information management, electronic medical records and hospital information systems, mobile medical products improve the convenience of doctors' clinical and scientific research (Citation72,Citation73).
Second, under the guidance and assistance of an intelligent robot, the patient lies flat on the positioning bed, and the intelligent positioning system scans the body surface and position information through holographic scanning technology. 3 D printing technology is used to generate the patient's personalized immobilization device (Citation74).
Third, after the position of the patient is fixed by the intelligent robot, the automatic laser locator or infrared positioning system accurately locates and automatically uploads the positioning image according to the requirements determined by the radiotherapy doctor, and the intelligent image guidance system is positioned automatically (Citation75).
Fourth, based on an expert medical record database of the radiotherapy plan and AI, the intelligent target volume delineation system can automatically perform accurate and personalized jobs (Citation76).
Fifth, based on the database, the limited conditions and optimized parameters of radiotherapy targets and OARs are automatically generated by machine learning technology, and a high-quality radiotherapy plan is automatically designed and evaluated by automatically importing TPS by script (Citation77,Citation78).
Sixth, before the actual treatment of a patient, a physician uses the extended reality technology and digital twin technique to design a radiotherapy plan that simulates the real human body. After a "rehearsal" on the accelerator, a 3D dose distribution is obtained and compared with the planned output dose (Citation79).
Seventh, with the help of an intelligent robot, a positioning mold is used to accurately fix the patient's position; after intelligently verifying the postural image, an accelerator intelligently approves the patient and implements the radiotherapy plan (Citation13).
Eighth, AI can monitor the radiotherapy process and the target displacement caused by tumor shrinkage or patient weight loss in real time, delineate the target volume, make radiotherapy plans, calculate and optimize the dose, and complete dose verification and quality control, thereby realizing automatic adaptive radiotherapy (Citation80–83).
Intelligent radiotherapy has already widely emerged in the field of radiotherapy recently. However, it has not been perfect yet. There would be a lot of efforts for radiation oncologists to push intelligent radiotherapy forward. We suppose when radiotherapy units are brought into a cloud computing center locally or nationwide in next decade, radiotherapy big data could be input in real time, with image data labeled uniformly and standardized. With the use of intelligent radiotherapy, accurate target positioning and delineation, rigorous treatment planning, appropriate dose control and implementation of radiotherapy could be achieved. Internet plus and IoT could provide a new modality for remote, automatic and intelligent radiotherapy. Therefore, various complications could be handled properly and balanced with the benefits of patients, who can obtain prognosis with best treatment effects.
Conclusion
The revolution of precision radiotherapy based on artificial intelligence is coming. Intelligent radiotherapy is an interdisciplinary frontier discipline, which is still in its infancy and advancing with each passing day. Unmanned radiotherapy center is a lofty ideal, to simplify the medical process, shorten the waiting time, improve work efficiency and realize homogeneous chemotherapy and radiotherapy under remote control. The radiotherapy oncologists shall think deeply: how to actively adapt and improve themselves in the era of intelligent radiotherapy, achieve the best man-machine combination state and make the intelligent radiotherapy shine brilliantly.
Disclosure statement
The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA A Cancer J Clin. 2020;70(1):7–30. doi:https://doi.org/10.3322/caac.21590.
- Allen C, Her S, Jaffray DA. Radiotherapy for cancer: present and future. Adv Drug Deliv Rev. 2017;109:1–2. doi:https://doi.org/10.1016/j.addr.2017.01.004.
- Chhabra A, Langen K, Mehta MP. An overview of modern proton therapy. Chin Clin Oncol. 2016;5(4):48 doi:https://doi.org/10.21037/cco.2016.05.06.
- Mohan R, Grosshans D. Proton therapy - Present and future. Adv Drug Deliv Rev. 2017;109:26–44. doi:https://doi.org/10.1016/j.addr.2016.11.006.
- Sokol O, Scifoni E, Tinganelli W, Kraft-Weyrather W, Wiedemann J, Maier A, et al. Oxygen beams for therapy: advanced biological treatment planning and experimental verification. Phys Med Biol. 2017;62(19):7798–813. doi:https://doi.org/10.1088/1361-6560/aa88a0.
- Senthilkumar K, Maria Das KJ. Comparison of biological-based and dose volume-based intensity-modulated radiotherapy plans generated using the same treatment planning system. J Cancer Res Ther. 2019;15(Supplement):S33–S38. doi:https://doi.org/10.4103/jcrt.JCRT_956_16.
- Mavroidis P, Komisopoulos G, Buckey C, Mavroeidi M, Swanson GP, Baltas D, et al. Radiobiological evaluation of prostate cancer IMRT and conformal-RT plans using different treatment protocols. Phys Med. 2017;40:33–41. doi:https://doi.org/10.1016/j.ejmp.2017.07.003.
- Chouard T, Venema L. Machine intelligence. Nature. 2015;521(7553):435 doi:https://doi.org/10.1038/521435a.
- Yu KH, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng. 2018;2(10):719–31. doi:https://doi.org/10.1038/s41551-018-0305-z.
- Chen M, Decary M. Artificial intelligence in healthcare: an essential guide for health leaders. Healthc Manage Forum. 2020;33(1):10–8. doi:https://doi.org/10.1177/0840470419873123.
- Siddique S, Chow JCL. Machine learning in healthcare communication. Encyclopedia. 2021;1(1):220–39. doi:https://doi.org/10.3390/encyclopedia1010021.
- Zheng D, Hong JC, Wang C, Zhu X. Radiotherapy treatment planning in the age of AI: are we ready yet? Technol Cancer Res Treat. 2019;18:1533033819894577 doi:https://doi.org/10.1177/1533033819894577.
- Wang C, Zhu X, Hong JC, Zheng D. Artificial intelligence in radiotherapy treatment planning: present and future. Technol Cancer Res Treat. 2019;18:1533033819873922 doi:https://doi.org/10.1177/1533033819873922.
- Wang M, Zhang Q, Lam S, Cai J, Yang R. A review on application of deep learning algorithms in external beam radiotherapy automated treatment planning. Front Oncol. 2020;10:580919. doi:https://doi.org/10.3389/fonc.2020.580919.
- Sherer MV, Lin D, Elguindi S, Duke S, Tan LT, Cacicedo J, et al. Metrics to evaluate the performance of auto-segmentation for radiation treatment planning: a critical review. Radiother Oncol. 2021;160:185–91. doi:https://doi.org/10.1016/j.radonc.2021.05.003.
- Arina A, Gutiontov SI, Weichselbaum RR. Radiotherapy and immunotherapy for cancer: from "Systemic" to "Multisite". Clin Cancer Res. 2020;26(12):2777–82. doi:https://doi.org/10.1158/1078-0432.CCR-19-2034.
- Lee SH, Han P, Hales RK, Voong KR, Noro K, Sugiyama S, Haller JW, et al. Multi-view radiomics and dosiomics analysis with machine learning for predicting acute-phase weight loss in lung cancer patients treated with radiotherapy. Phys Med Biol. 2020;65(19):195015. doi:https://doi.org/10.1088/1361-6560/ab8531.
- Isaksson LJ, Pepa M, Zaffaroni M, Marvaso G, Alterio D, Volpe S, et al. Machine learning-based models for prediction of toxicity outcomes in radiotherapy. Front Oncol. 2020;10:790. doi:https://doi.org/10.3389/fonc.2020.00790.
- Grovik E, Yi D, Iv M, Tong E, Rubin D, Zaharchuk G. Deep learning enables automatic detection and segmentation of brain metastases on multisequence MRI. J Magn Reson Imaging. 2020;51(1):175–82. doi:https://doi.org/10.1002/jmri.26766.
- Hegi-Johnson F, de Ruysscher D, Keall P, Hendriks L, Vinogradskiy Y, Yamamoto T, et al. Imaging of regional ventilation: Is CT ventilation imaging the answer? A systematic review of the validation data. Radiother Oncol. 2019;137:175–85. doi:https://doi.org/10.1016/j.radonc.2019.03.010.
- He QE, Tong YF, Ye Z, Gao LX, Zhang YZ, Wang L, Song K. A multiple genomic data fused SF2 prediction model, signature identification, and gene regulatory network inference for personalized radiotherapy. Technol Cancer Res Treat. 2020;19:1533033820909112. doi:https://doi.org/10.1177/1533033820909112.
- Defourny N, Monten C, Grau C, Lievens Y, Perrier L. Critical review and quality-assessment of cost analyses in radiotherapy: How reliable are the data? Radiother Oncol. 2019;141:14–26. doi:https://doi.org/10.1016/j.radonc.2019.09.020.
- Morrison JJ, Hostetter J, Wang K, Siegel EL. Data-driven decision support for radiologists: re-using the National Lung Screening Trial dataset for pulmonary nodule management. J Digit Imaging. 2015;28(1):18–23. doi:https://doi.org/10.1007/s10278-014-9720-1.
- Chen RC, Gabriel PE, Kavanagh BD, McNutt TR. How will big data impact clinical decision making and precision medicine in radiation therapy? Int J Radiat Oncol Biol Phys. 2016;95(3):880–4. doi:https://doi.org/10.1016/j.ijrobp.2015.10.052.
- Sahiner B, Pezeshk A, Hadjiiski LM, Wang X, Drukker K, Cha KH, et al. Deep learning in medical imaging and radiation therapy. Med Phys. 2019;46(1):e1–e36. doi:https://doi.org/10.1002/mp.13264.
- Yao JJ, Zhang F, Gao TS, Zhang WJ, Lawrence WR, Zhu BT, et al. Survival impact of radiotherapy interruption in nasopharyngeal carcinoma in the intensity-modulated radiotherapy era: A big-data intelligence platform-based analysis. Radiother Oncol. 2019;132:178–87. doi:https://doi.org/10.1016/j.radonc.2018.10.018.
- Mintz Y, Brodie R. Introduction to artificial intelligence in medicine. Minim Invasive Ther Allied Technol. 2019;28(2):73–81. doi:https://doi.org/10.1080/13645706.2019.1575882.
- Amisha Malik P, Pathania M, Rathaur VK. Overview of artificial intelligence in medicine. J Family Med Prim Care. 2019;8(7):2328–2331. doi:https://doi.org/10.4103/jfmpc.jfmpc_440_19.
- Thompson RF, Valdes G, Fuller CD, Carpenter CM, Morin O, Aneja S Jr., et al. Artificial intelligence in radiation oncology: A specialty-wide disruptive transformation? Radiother Oncol. 2018;129(3):421–6. doi:https://doi.org/10.1016/j.radonc.2018.05.030.
- Chow JCL. Internet-based computer technology on radiotherapy. Rep Pract Oncol Radiother. 2017;22(6):455–62. doi:https://doi.org/10.1016/j.rpor.2017.08.005.
- Li Q, Kim J, Balagurunathan Y, Liu Y, Latifi K, Stringfield O, et al. Imaging features from pretreatment CT scans are associated with clinical outcomes in nonsmall-cell lung cancer patients treated with stereotactic body radiotherapy. Med Phys. 2017;44(8):4341–9. doi:https://doi.org/10.1002/mp.12309.
- Huynh E, Coroller TP, Narayan V, Agrawal V, Hou Y, Romano J, et al. CT-based radiomic analysis of stereotactic body radiation therapy patients with lung cancer. Radiother Oncol. 2016;120(2):258–66. doi:https://doi.org/10.1016/j.radonc.2016.05.024.
- Siddique S, Chow JCL. Artificial intelligence in radiotherapy. Rep Pract Oncol Radiother. 2020;25(4):656–66. doi:https://doi.org/10.1016/j.rpor.2020.03.015.
- van Dijk LV, Van den Bosch L, Aljabar P, Peressutti D, Both S, Jhms R, et al. Improving automatic delineation for head and neck organs at risk by Deep Learning Contouring. Radiother Oncol. 2020;142:115–23. doi:https://doi.org/10.1016/j.radonc.2019.09.022.
- Song Y, Hu J, Wu Q, Xu F, Nie S, Zhao Y, et al. Automatic delineation of the clinical target volume and organs at risk by deep learning for rectal cancer postoperative radiotherapy. Radiother Oncol. 2020;145:186–92. doi:https://doi.org/10.1016/j.radonc.2020.01.020.
- Ng F, Jiang R, Chow JCL. Predicting radiation treatment planning evaluation parameter using artificial intelligence and machine learning[J]. IOPSciNotes. 2020;1(1):014003. doi:https://doi.org/10.1088/2633-1357/ab805d.
- Yamada T, Watanabe S, Nagaoka T, Nemoto M, Hanaoka K, Kaida H, et al. Automatic delineation algorithm of reference region for amyloid imaging based on kinetics. Ann Nucl Med. 2020;34(2):102–7. doi:https://doi.org/10.1007/s12149-019-01419-9.
- Fung NTC, Hung WM, Sze CK, Lee MCH, Ng WT. Automatic segmentation for adaptive planning in nasopharyngeal carcinoma IMRT: Time, geometrical, and dosimetric analysis. Med Dosim. 2020;45(1):60–5. doi:https://doi.org/10.1016/j.meddos.2019.06.002.
- Cunha CE, Fernandes R, Santos CX, Boccaletti KW, Pellizzon ACA, Barbosa JHO. Viability of mobile applications for remote support of radiotherapy patients. Rev Assoc Med Bras. 2019;65(10):1321–6. doi:https://doi.org/10.1590/1806-9282.65.10.1321.
- Maguire R, Ream E, Richardson A, Connaghan J, Johnston B, Kotronoulas G, et al. Development of a novel remote patient monitoring system: the advanced symptom management system for radiotherapy to improve the symptom experience of patients with lung cancer receiving radiotherapy. Cancer Nurs. 2015;38(2):E37–47. doi:https://doi.org/10.1097/NCC.0000000000000150.
- Han EY, Kim GY, Rebueno N, Yeboa DN, Briere TM. End-to-end testing of automatic plan optimization using RayStation scripting for hypofractionated multimetastatic brain stereotactic radiosurgery. Med Dosim. 2019;44(4):e44–e50. doi:https://doi.org/10.1016/j.meddos.2018.12.006.
- Mason SA, White IM, Lalondrelle S, Bamber JC, Harris EJ. The stacked-ellipse algorithm: an ultrasound-based 3-D uterine segmentation tool for enabling adaptive radiotherapy for uterine cervix cancer. Ultrasound Med Biol. 2020;46(4):1040–52. doi:https://doi.org/10.1016/j.ultrasmedbio.2019.09.001.
- McNutt TR, Moore KL, Wu B, Wright JL. Use of big data for quality assurance in radiation therapy. Semin Radiat Oncol. 2019;29(4):326–32. doi:https://doi.org/10.1016/j.semradonc.2019.05.006.
- Kalet AM, Luk S, Phillips MH. Radiation therapy quality assurance tasks and tools: the many roles of machine learning. Med Phys. 2020;47(5):e168–e177. doi:https://doi.org/10.1002/mp.13445.
- Sun X-S, Li X-Y, Chen Q-Y, Tang L-Q, Mai H-Q. Future of radiotherapy in nasopharyngeal carcinoma. Br J Radiol. 2019;92(1102):20190209. doi:https://doi.org/10.1259/bjr.20190209.
- Zhao ZQ, Zheng P, Xu ST, Wu X. Object detection with deep learning: a review. IEEE Trans Neural Netw Learn Syst. 2019;30(11):3212–32. doi:https://doi.org/10.1109/TNNLS.2018.2876865.
- Chamunyonga C, Burbery J, Caldwell P, Rutledge P, Fielding A, Crowe S. Utilising the virtual environment for radiotherapy training system to support undergraduate teaching of IMRT, VMAT, DCAT treatment planning, and QA concepts. J Med Imaging Radiat Sci. 2018;49(1):31–8. doi:https://doi.org/10.1016/j.jmir.2017.11.002.
- Bachmann D, Weichert F, Rinkenauer G. Review of three-dimensional human-computer interaction with focus on the leap motion controller. Sensors. 2018;18(7):2194. doi:https://doi.org/10.3390/s18072194.
- Kang M, Kim J, Jang B, Chae Y, Kim JH, Ahn JH. Graphene-based three-dimensional capacitive touch sensor for wearable electronics. ACS Nano. 2017;11(8):7950–7. doi:https://doi.org/10.1021/acsnano.7b02474.
- Johnson K, Liszewski B, Dawdy K, Lai Y, McGuffin M. Learning in 360 degrees: a pilot study on the use of virtual reality for radiation therapy patient education. J Med Imaging Radiat Sci. 2020;51(2):221–6. doi:https://doi.org/10.1016/j.jmir.2019.12.008.
- Bjornsson B, Borrebaeck C, Elander N, Gasslander T, Gawel DR, Gustafsson M, et al.; Swedish Digital Twin Consortium. Swedish digital twin C. Digital twins to personalize medicine. Genome Med. 2019;12(1):4. doi:https://doi.org/10.1186/s13073-019-0701-3.
- He R, Chen G, Dong C, Sun S, Shen X. Data-driven digital twin technology for optimized control in process systems. ISA Trans. 2019;95:221–34. doi:https://doi.org/10.1016/j.isatra.2019.05.011.
- Zheng Y, Yang S, Cheng H. An application framework of digital twin and its case study. J Ambient Intell Human Comput. 2019;10(3):1141–53. doi:https://doi.org/10.1007/s12652-018-0911-3.
- Coenen A, Kim YH, Kruk M, Tesche C, De Geer J, Kurata A, et al. Diagnostic accuracy of a machine-learning approach to coronary computed tomographic angiography-based fractional flow reserve: result from the MACHINE consortium. Circ Cardiovasc Imaging. 2018;11(6):e007217. doi:https://doi.org/10.1161/CIRCIMAGING.117.007217.
- Parekh V, Jacobs MA. Radiomics: a new application from established techniques. Expert Rev Precis Med Drug Dev. 2016;1(2):207–26. doi:https://doi.org/10.1080/23808993.2016.1164013.
- Wu J, Tha KK, Xing L, Li R. Radiomics and radiogenomics for precision radiotherapy. J Radiat Res. 2018;59(suppl_1):i25–i31. doi:https://doi.org/10.1093/jrr/rrx102.
- Jang BS, Chang JH, Park AJ, Wu HG. Generation of virtual lung single-photon emission computed tomography/CT fusion images for functional avoidance radiotherapy planning using machine learning algorithms. J Med Imaging Radiat Oncol. 2019;63(2):229–35. doi:https://doi.org/10.1111/1754-9485.12868.
- Liney GP, Whelan B, Oborn B, Barton M, Keall P. MRI-linear accelerator radiotherapy systems. Clin Oncol. 2018;30(11):686–91. doi:https://doi.org/10.1016/j.clon.2018.08.003.
- Lee G, Lee HY, Park H, Schiebler ML, van Beek EJR, Ohno Y, et al. Radiomics and its emerging role in lung cancer research, imaging biomarkers and clinical management: State of the art. Eur J Radiol. 2017;86:297–307. doi:https://doi.org/10.1016/j.ejrad.2016.09.005.
- Keek S, Sanduleanu S, Wesseling F, de Roest R, van den Brekel M, van der Heijden M, et al. Computed tomography-derived radiomic signature of head and neck squamous cell carcinoma (peri)tumoral tissue for the prediction of locoregional recurrence and distant metastasis after concurrent chemo-radiotherapy. Plos One. 2020; 15(5):e232639. doi:https://doi.org/10.1371/journal.pone.0232639.
- Cunliffe A, Armato SG, Castillo R, Pham N, Guerrero T, Al-Hallaq HA. Lung texture in serial thoracic computed tomography scans: correlation of radiomics-based features with radiation therapy dose and radiation pneumonitis development. Int J Radiat Oncol Biol Phys. 2015;91(5):1048–56. doi:https://doi.org/10.1016/j.ijrobp.2014.11.030.
- Bertucci F, Le Corroller-Soriano AG, Monneur A, Fluzin S, Viens P, Maraninchi D, Goncalves A. [E-health and "Cancer outside the hospital walls", Big Data and artificial intelligence]. Bull Cancer. 2020;107(1):102–12. doi:https://doi.org/10.1016/j.bulcan.2019.07.006.
- Kim SC, Shaw BR, Shah DV, Hawkins RP, Pingree S, McTavish FM, Gustafson DH. Interactivity, presence, and targeted patient care: mapping e-health intervention effects over time for cancer patients with depression. Health Commun. 2019;34(2):162–71. doi:https://doi.org/10.1080/10410236.2017.1399504.
- Gurbani S, Weinberg B, Cooper L, Mellon E, Schreibmann E, Sheriff S, et al. The brain imaging collaboration suite (BrICS): a cloud platform for integrating whole-brain spectroscopic MRI into the radiation therapy planning workflow. Tomography. 2019;5(1):184–91. doi:https://doi.org/10.18383/j.tom.2018.00028.
- Miras H, Jiménez R, Perales Á, Terrón JA, Bertolet A, Ortiz A, Macías J. Monte Carlo verification of radiotherapy treatments with CloudMC. Radiat Oncol. 2018;13(1):99. doi:https://doi.org/10.1186/s13014-018-1051-9.
- Alleyne-Mike K, Sylvester P, Henderson-Suite V, Mohoyodeen T. Radiotherapy in the Caribbean: a spotlight on the human resource and equipment challenges among CARICOM nations. Hum Resour Health. 2020;18(1):49 doi:https://doi.org/10.1186/s12960-020-00489-5.
- Numasaki H, Teshima T, Okuda Y, Ogawa K, Japanese Society for Radiation Oncology Database Committee. Japanese Society for Radiation Oncology Database C. Japanese structure survey of radiation oncology in 2013. J Radiat Res. 2020;61(5):799–816. doi:https://doi.org/10.1093/jrr/rraa047.
- Pan Y, Yang R, Zhang S, Li J, Dai J, Wang J, Cai J. National survey of patient specific IMRT quality assurance in China. Radiat Oncol. 2019;14(1):69 doi:https://doi.org/10.1186/s13014-019-1273-5.
- Hamidi M, Mahendran P, Denecke K. Towards a digital lean hospital: concept for a digital patient board and its integration with a hospital information system. Stud Health Technol Inform. 2019;264:606–10. doi:https://doi.org/10.3233/SHTI190294.
- Pearse J, Chow JCL. An Internet of Things app for monitor unit calculation in superficial and orthovoltage skin therapy[J]. IOPSciNotes. 2020;1(1):014002. doi:https://doi.org/10.1088/2633-1357/ab8be0.
- Chow JCL. Artificial intelligence in radiotherapy and patient care. Artif Intell Med. 2021;18:1533033819873922. doi:https://doi.org/10.1007/978-3-030-58080-3_143-1.
- Lurie JD, Merrens EJ, Lee J, Splaine ME. An approach to hospital quality improvement. Med Clin North Am. 2002;86(4):825–45. doi:https://doi.org/10.1016/S0025-7125(02)00021-4.
- Pettersson N, Simpson D, Atwood T, Hattangadi-Gluth J, Murphy J, Cervino L. Automatic patient positioning and gating window settings in respiratory-gated stereotactic body radiation therapy for pancreatic cancer using fluoroscopic imaging. J Appl Clin Med Phys. 2018;19(2):74–82. doi:https://doi.org/10.1002/acm2.12258.
- Cardenas CE, Yang J, Anderson BM, Court LE, Brock KB. Advances in auto-segmentation. Semin Radiat Oncol. 2019;29(3):185–97. doi:https://doi.org/10.1016/j.semradonc.2019.02.001.
- Beaton L, Bandula S, Gaze MN, Sharma RA. How rapid advances in imaging are defining the future of precision radiation oncology. Br J Cancer. 2019;120(8):779–90. doi:https://doi.org/10.1038/s41416-019-0412-y.
- Fan J, Wang J, Chen Z, Hu C, Zhang Z, Hu W. Automatic treatment planning based on three-dimensional dose distribution predicted from deep learning technique. Med Phys. 2019;46(1):370–81. doi:https://doi.org/10.1002/mp.13271.
- Mattiucci GC, Boldrini L, Chiloiro G, D'Agostino GR, Chiesa S, De Rose F, et al. Automatic delineation for replanning in nasopharynx radiotherapy: what is the agreement among experts to be considered as benchmark? Acta Oncol. 2013;52(7):1417–22. doi:https://doi.org/10.3109/0284186X.2013.813069.
- Sharma P, Suehling M, Flohr T, Comaniciu D. Artificial intelligence in diagnostic imaging: status quo, challenges, and future opportunities. J Thorac Imaging. 2020;35(Suppl 1):S11–S16. doi:https://doi.org/10.1097/RTI.0000000000000499.
- Pacelli R, Caroprese M, Palma G, Oliviero C, Clemente S, Cella L, Conson M. Technological evolution of radiation treatment: implications for clinical applications. Semin Oncol. 2019;46(3):193–201. doi:https://doi.org/10.1053/j.seminoncol.2019.07.004.
- Brock KK. Adaptive radiotherapy: moving into the future. Semin Radiat Oncol. 2019;29(3):181–4. doi:https://doi.org/10.1016/j.semradonc.2019.02.011.
- Morgan HE, Sher DJ. Adaptive radiotherapy for head and neck cancer. Cancers Head Neck. 2020;5:1 doi:https://doi.org/10.1186/s41199-019-0046-z.
- Witt JS, Rosenberg SA, Bassetti MF. MRI-guided adaptive radiotherapy for liver tumours: visualising the future. Lancet Oncol. 2020;21(2):e74–e82. doi:https://doi.org/10.1016/S1470-2045(20)30034-6.
- Sakanaka K, Fujii K, Mizowaki T. Adaptive radiotherapy in locally advanced esophageal cancer with atelectasis: a case report. BMC Cancer. 2020;20(1):21. doi:https://doi.org/10.1186/s12885-019-6505-4.