Abstract
This study aimed to investigate the predictive factors of transfer of glioblastoma multiforme (GBM) patients who underwent rehabilitation in acute care hospitals. We retrospectively identified 85 patients with GBM who underwent rehabilitation at our hospital. Multivariable logistic regression analysis showed that age and Barthel index (BI) at rehabilitation initiation significantly influenced the discharge destination. Cut-off values for these factors were 76 years of age and 30 BI points. These findings could help predict the discharge destination and the choice of rehabilitation strategies of newly diagnosed patients with GBM admitted to an acute care hospital.
Introduction
Glioblastoma multiforme (GBM) is a common form of brain cancer and one of the most severe types. The 5-year relative survival rate of patients with GBM is 16%, and median survival times, even after the administration of optimal treatment methods, remain <18 months in Japan (Citation1). The standard treatment for GBM is tumor resection, followed by radiation therapy and systemic treatment with temozolomide (Citation2).
Patients with GBM have central nervous system symptoms which vary depending on the site of the tumor. Typically, patients require rehabilitation to improve and maintain mobility and cognitive function when receiving treatment in acute care hospitals. Generally, GBM inpatients are transferred to hospitals or discharged home after treatment has been initiated. In such cases, rehabilitation and disease management strategies need to be formed while having the patient’s eventual transfer to a hospital or home in mind. However, to the best of our knowledge, no prior studies predicting discharge destination through commonly used indices in rehabilitation and nutrition have been conducted.
In patients with GBM, prognostic factors for survival include age, performance status, the extent of resection and neurological function, and molecular genetics (Citation3). One study has also shown that rehabilitation is associated with survival (Citation4). In addition, several studies have reported improvement in physical and cognitive functioning due to rehabilitation in patients with brain tumors (Citation5–11). To the best of our knowledge, no investigation of factors influencing discharge destination in newly diagnosed patients with GBM after their initial treatment in an acute care hospital has been performed, nor has an associated cut-off value been reported. This study examined factors that influence GBM inpatient transfer in patients who underwent rehabilitation. The primary hypothesis was that indicators of activities of daily living (ADL) and nutrition factors influence transfer in the patients with GBM who had previously undergone rehabilitation. This study aims to analyze factors that influence patient transfer to evaluate rehabilitation strategies used to treat new patients with GBM in acute care hospitals.
Materials and methods
Data collection
We retrospectively reviewed patients consecutively admitted to Yamagata University Hospital between September 1, 2013, and December 31, 2020. The inclusion criteria were all patients diagnosed with GBM, based on pathological or imaging findings (World Health Organization grade IV) (Citation12). Inpatients who died despite receiving treatment in our acute hospital were excluded from the study population. Data including patient age, sex, initial treatment type (surgical, radiation, temozolomide, and radiation plus temozolomide), tumor location, discharge location, length of stay, survival time from the diagnosis, number of family members, Karnofsky performance status (KPS), Barthel index (BI) at the start of rehabilitation and discharge, and serum albumin levels on admission and at discharge were obtained from patients’ clinical records. ΔBI was defined as the difference between the BI at the commencement of the rehabilitation and that at discharge from our hospital. Serum albumin percent change was calculated as serum albumin at discharge divided by serum albumin at admission, then minus one. This study was approved by the Institutional Review Board (The ethical review committee of Yamagata University Faculty of Medicine: approval number 2020-406), and the need for patient consent was waived due to the study’s retrospective nature.
Karnofsky performance status (KPS)
The KPS is commonly used to measure the level of cancer patient activity and medical care requirements. The scale ranges from 0% (dead) to 100% (normal, no complaints, no evidence of disease). KPS has considerable validity as a global indicator of the functional status of patients with cancer (Citation13).
Barthel index
This was developed to determine the ability of patients with neuromuscular or musculoskeletal disorders to care for themselves (Citation14). The BI is assessed based on ADL using the following 10 categories of self-care: feeding, moving from wheelchair to bed and returning, doing personal toilet, getting on and off the toilet, bathing self, walking on a level surface, ascending and descending stairs, dressing and undressing, continence of bowels, and controlling the bladder. Each score is evaluated using a scale of 0–15 points, with a perfect score equaling 100 points.
Serum albumin
Serum albumin level is used as an indicator of nutrition and inflammation. Low serum albumin levels after surgery indicate acute inflammation, infection, liver disease, nephrotic syndrome, inadequate nutrition, and extensive burns. Therefore, serum albumin level has been used as a prognostic indicator of mortality and length of stay (Citation15,Citation16). For this reason, we evaluated whether serum albumin level indicated discharge destination.
Inpatient rehabilitation program
At our institute, inpatient rehabilitation is initiated after diagnosis or surgical removal of the tumor. Rehabilitation includes a range of motion exercises, sitting, standing, and walking via physical therapy. In addition, ADL exercises are performed during occupational therapy, while swallowing and speech exercises are performed during speech-language therapy. These were the main contents of the program that each therapist carried out according to the patient’s condition. Each patient participated in a minimum of 20–40 min of therapy, 5 of 7 d per week.
Statistical analysis
Descriptive statistics were analyzed by dividing the participants into a transfer group and a discharge-home group. Categorical variables were assessed using Fisher’s exact test, and continuous variables were analyzed using the Mann–Whitney U test. The Wilcoxon signed rank test compared BI scores determined at the start of rehabilitation and discharge.
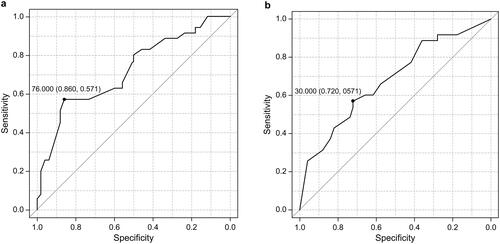
Multivariable logistic regression by forced entry was used to determine factors associated with transfer to a hospital. The independent variables were age, sex, KPS at admission, the BI at the start of rehabilitation, serum albumin level at discharge, and number of family members. Adjusted odds ratios (ORs), 95% confidence intervals (CIs), and corresponding p values were determined. Cut-off values for items determined to be significant via multivariable logistic regression analyses were calculated, receiver-operating characteristic (ROC) curves were obtained, and area under the curve (AUC) sensitivity and specificity values were calculated. Statistical significance was set at p < 0.05. All analyses were performed using EZR version 1.54 (Saitama Medical Center, Jichi Medical University, Saitama, Japan) (Citation17).
Results
A total of 87 newly diagnosed patients with GBM who underwent rehabilitation were included in this study. Two patients who died in our hospital were excluded from the analysis, leaving 50 surviving patients discharged to their homes and 35 transferred to other hospitals. All transferred patients were admitted to the rehabilitation hospital on the same day. The characteristics of the included patients are summarized in . The median age of the patients in the discharge-home and transfer groups was 65 and 77 years, respectively. The Fisher’s exact test showed no significant difference in sex between the discharge-home and transfer groups. The median length of hospital stay and survival time was not significantly different. Although the KPS at admission was not significant, the KPS at discharge was significantly lower in the transfer group than in the discharge-home group (p < 0.01). At the start of rehabilitation (p < 0.01), the discharge BI (p < 0.01) and ΔBI (p < 0.05) were significantly lower in the transfer group than in the discharge-home group (p < 0.01). Admission (p < 0.05) and discharge (p < 0.01) serum albumin levels were significantly lower in the transfer group than in the discharge-home group. Serum albumin percent change was not significantly different between both groups.
Table 1. Patients’ characteristics.
Values of BI at the start of rehabilitation and at discharge were compared, and the findings are shown in a box plot ( and ). The BI values of patients in the discharge-home and transfer groups were significantly higher at discharge than at the start of rehabilitation (p < 0.01). There was no significant difference observed when the tumor location in the two groups was compared, and patients in both groups tended to have frontal tumors more frequently than tumors at other locations. The initial treatment of GBM was significantly different between the two groups (p < 0.01); most treatments were surgery, radiation, and chemotherapy (). The choice of chemotherapy contents (Temozolomide, Bevacizumab, or Nivolumab) and radiation dose was based on the patient’s general condition. BI comparison at the start of rehabilitation for each initial treatment () showed no significant difference in BI values between the two groups. BI comparison at discharge for each initial treatment () shows that BI values of the received resection, radiation, and chemotherapy group in the initial treatment were significantly higher in the discharge-home group than transfer group (p < 0.01). BI comparison at the start of rehabilitation and at discharge for each initial treatment () shows that BI values of the received resection, radiation, and chemotherapy group at initial treatment were significantly higher at discharge than at the start of rehabilitation (p < 0.01).
Figure 1. (a) Comparison of BI values of patients in the discharge-home group at the start of rehabilitation and at discharge; (b) Comparison of BI values of patients in the hospital transfer group at the start of rehabilitation and at discharge. BI: Barthel index.
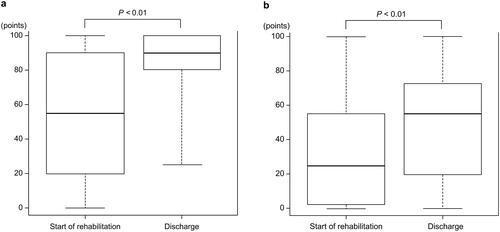
Table 2. Location of the tumor and initial treatment type in included patients with glioblastoma.
Table 3. BI comparison at the start of rehabilitation for each initial treatment.
Table 4. BI comparison at discharge for each initial treatment.
Table 5. BI comparison at the start of rehabilitation and at discharge for each initial treatment.
A multivariable logistic regression analysis of associations between transfer to a hospital and factors assessed is presented in . As a result, age (OR = 1.06; 95% CI, 1.020–1.110; p < 0.01), and BI at the start of rehabilitation (OR = 0.98; 95% CI, 0.966–0.998; p < 0.05) were determined to impact transfer to a hospital ().
Table 6. Analysis of factors influencing discharge destination.
We analyzed cut-off values for age and BI at the start of rehabilitation and obtained a ROC curve ( and ). The cut-off value for age was 76, and that for BI at the start of rehabilitation was 30.
Figure 2. (a) ROC curve for age. The cut-off value was 76 years of age, specificity was 0.860, sensitivity was 0.571, and AUC was 0.72; (b) ROC curve for BI at the start of rehabilitation. The cut-off value was 30 points, specificity was 0.720, sensitivity was 0.571, and AUC was 0.68. ROC: receiver operating characteristic; AUC: area under the curve.
Discussion
This study investigated factors affecting discharge destinations (discharge-home or transfer to another hospital) and calculated the cut-off values for each by obtaining a ROC curve using data from newly diagnosed patients with GBM who underwent rehabilitation. The results showed that age and BI significantly affected transfer, and cut-off values were 76 years and 30 points. In addition, patients with newly diagnosed GBM who underwent rehabilitation had improved BI scores.
Previous studies mainly focused on prognostic indicators of GBM survival. For example, the Radiation Therapy Oncology Group (RTOG) (Citation18) reported that the prognostic factors for survival were age, KPS, extent of resection, and neurologic function. Similarly, other studies have shown that factors such as sex and radiotherapy are associated with survival (Citation19). As GBM is commonly the most malignant brain tumor, identifying indicators of survival might be highly important. However, to the best of our knowledge, no discharge factor or cut-off value in patients that underwent rehabilitation in acute care hospitals has been identified so far. Our most important finding was that predictors of transfer in patients with GBM were age and BI. Moreover, BI may be useful in an acute care hospital setting for predicting GBM patient outcomes. This suggests that it may be useful to predict discharge destination as soon as possible. Therefore, it is important to consider at the start of rehabilitation, age, BI, and other factors that can affect transfer.
This study showed that the transfer group had significantly lower BI values at the start of rehabilitation and discharge than the discharge-home group. This result suggests that lower functioning patients require more rehabilitation therapy, caregiver management, care services, and other environmental improvements after being transferred. Cut-off values of significant variables (age and BI) were 76 years and 30 points, respectively. Patients with GBM who were older than 65 (Citation20) or 55 (Citation21) years of age were previously determined to have poorer outcomes; therefore, patients with advanced age and low BI scores should be managed early by social workers.
Generally, patients concurrently undergo rehabilitation and GBM treatment in acute care hospitals. A previous study showed that rehabilitation improved the physical and cognitive functions of 78 patients with GBM (Citation5). Another study revealed that a high level of functional improvement was a predictor of longer survival in patients who underwent rehabilitation (Citation4). Similar to prior findings, patients with GBM assessed in this study may have shown improved functional levels via initial treatment and rehabilitation. GBM is a rapidly progressive disease; many patients experience decreased physical activity during inpatient care, leading to disuse syndromes, such as generalized muscle weakness and cognitive decline. The improved effectiveness of treatment may be due to the early implementation of sit-to-stand and joint mobilization exercises training in activities of daily living (ADL) to develop compensatory movements among patients on bed rest for acute body management after tumor resection and GBM diagnosis. These results suggest that rehabilitation performed in conjunction with initial treatments likely improves physical functioning.
Serum albumin is a good indicator of malnutrition, inflammation, and liver and renal diseases. In addition, patients with malignancies, chronic heart failure, and benign lung diseases require special attention due to the high prevalence of malnutrition and low serum albumin levels (Citation22). Although serum albumin levels at admission were significantly lower in the transfer group than those in the discharge-home group, no significant effect on transfer was observed in the patients that were included in the study. This may be because most patients with GBM have low levels of inflammation and a good nutritional status on admission.
This study has several limitations. It was an observational, non-randomized study, the sample size was small, and patients from a single acute care hospital were examined. Therefore, it was difficult to assess all variables via multivariate analysis, and the effect of confounding factors could not be eliminated. Hence, the results of this study may not be generalizable. In the future, a multicenter study with larger sample size is needed. Additionally, no precise timepoint for BI assessment at the start of rehabilitation and before discharge by a therapist was used. Rehabilitation was ordered at different times postoperatively (or admission) for each patient with GBM. We should consider assessing BI at an optimal time point. There are no set discharge criteria scores, including standard BI and KPS, at discharge in our hospital. This makes it difficult to examine the appropriate timing of rehabilitation using the criteria and compare the effects of rehabilitation. We would like to make efforts to set standards for these scores in the future. Finally, we did not assess family caregiving skills or the psychological state of patients and their families; we would like to include these factors in future research to examine how they might affect outcomes. Furthermore, to cope with psychological and social problems, we believe it is necessary to share information among multiple professions and establish a support system to help patients receive better treatment and discharge support.
In conclusion, a multivariable logistic regression analysis using data of patients newly diagnosed with GBM who underwent rehabilitation in an acute care hospital identified factors that influenced transfer and calculated cut-off values for each factor. Age and BI at the time of initiation of rehabilitation were factors that influenced transfer, with cut-off values of 76 years of age and 30 points, respectively. Furthermore, these results suggest that rehabilitation likely improves physical functioning. This study suggests a rehabilitation strategy for patients with GBM, which encourages management to be performed along with plans (from the beginning of treatment) to transfer patients receiving treatment in an acute care hospital to another hospital.
Acknowledgments
The authors thank all members of the Rehabilitation Unit, Yamagata University, Faculty of Medicine, for their help in conducting this study.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Additional information
Funding
References
- Brain tumor registry of Japan (2005–2008). Neurol Med Chir (Tokyo). 2017;57(1):9–102. doi:10.2176/nmc.sup.2017-0001.
- Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJB, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi:10.1056/NEJMoa043330.
- Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–820. doi:10.1007/s00401-016-1545-1.
- Roberts PS, Nuño M, Sherman D, Asher A, Wertheimer J, Riggs RV, Patil CG. The impact of inpatient rehabilitation on function and survival of newly diagnosed patients with glioblastoma. Pm R. 2014;6(6):514–521. doi:10.1016/j.pmrj.2013.12.007.
- Tang V, Rathbone M, Park Dorsay J, Jiang S, Harvey D. Rehabilitation in primary and metastatic brain tumours: impact of functional outcomes on survival. J Neurol. 2008;255(6):820–827. doi:10.1007/s00415-008-0695-z.
- Geler-Kulcu D, Gulsen G, Buyukbaba E, Ozkan D. Functional recovery of patients with brain tumor of acute stroke after rehabilitation: a comparative study. J Clin Neurosci. 2009;16(1):74–78. doi:10.1016/j.jocn.2008.04.014.
- Greenberg E, Treger I, Ring H. Rehabilitation outcomes in patients with brain tumors and acute stroke. Am J Phys Med. 2006;85(7):568–573. doi:10.1097/01.phm.0000223218.38152.53.
- Mukand JA, Blackinton DD, Crincoli MG, Lee JJ, Santos BB. Incidence of neurologic deficits and rehabilitation of patients with brain tumors. Am J Phys Med Rehabil. 2001;80(5):346–350. doi:10.1097/00002060-200105000-00005.
- Marciniak CM, Sliwa JA, Heinemann AW, Semik PE. Functional outcomes of persons with brain tumors after inpatient rehabilitation. Arch Phys Med Rehabil. 2001;82(4):457–463. doi:10.1053/apmr.2001.21862.
- Bartolo M, Zucchella C, Pace A, Lanzetta G, Vecchione C, Bartolo M, et al. Early rehabilitation after surgery improves functional outcome in inpatients with brain tumours. J Neurooncol. 2012;107(3):537–544. doi:10.1007/s11060-011-0772-5.
- Zucchella C, Capone A, Codella V, De Nunzio AM, Vecchione C, Sandrini G, et al. Cognitive rehabilitation for early post-surgery inpatients affected by primary brain tumor: a randomized, controlled trial. J Neurooncol. 2013;114(1):93–100. doi:10.1007/s11060-013-1153-z.
- Gupta A, Dwivedi T. A simplified overview of world health organization classification update of central nervous system tumors 2016. J Neurosci Rural Pract. 2017;8(4):629–641. doi:10.4103/jnrp.jnrp_168_17.
- Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer. 1980;45(8):2220–2224. doi:10.1002/1097-0142(19800415)45:8.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65.
- De Luis DA, Terroba MC, Cuellar L, Terroba MC, Cabezas G, Rojo S, et al. Nutritional assessment: predictive variables at hospital admission related with length of stay. Ann Nutr Metab. 2006;50(4):394–398. doi:10.1159/000094362.
- de Luis DA, Terroba MC, Cuellar L, Izaola O, de la Fuente B, Martin T, Cabezas G. Association of anthropometric and biochemical markers with length of stay and mortality in the hospital. Eur Rev Med Pharmacol Sci. 2013;17(10):1321–1325.
- Kanda Y. Investigation of feely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi:10.1038/bmt.2012.244.
- Li J, Wang M, Won M, Shaw EG, Coughlin C, Curran WJ, Jr, Mehta MP. Validation and simplification of the Radiation Therapy Oncology Group recursive partitioning analysis classification for glioblastoma. Int J Radiat Oncol Biol Phys. 2011;81(3):623–630. doi:10.1016/j.ijrobp.2010.06.012.
- Tugcu B, Postalci LS, Gunaldi O, Tanriverdi O, Akdemir H. Efficacy of clinical prognostic factors on survival in patients with glioblastoma. Turk Neurosurg. 2010;20(2):117–125. doi:10.5137/1019-5149.JTN.2461-09.4.
- Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95(2):190–198. doi:10.3171/jns.2001.95.2.0190.
- Jeremic B, Milicic B, Grujicic D, Dagovic A, Aleksandrovic J. Multivariate analysis of clinical prognostic factors in patients with glioblastoma multiforme treated with a combined modality approach. J Cancer Res Clin Oncol. 2003;129(8):477–484. doi:10.1007/s00432-003-0471-5.
- Pirlich M, Schütz T, Kemps M, Luhman N, Burmester GR, Baumann G, et al. Prevalence of malnutrition in hospitalized medical patients: impact of underlying disease. Dig Dis. 2003;21(3):245–251. doi:10.1159/000073342.
