ABSTRACT
This study identified changes in blood pressure, blood glucose, and cholesterol levels in frail elderly adults who received home health care nursing over 8 years in Korea. Secondary data extracted from nursing records (2010–2018) of a public health center were analyzed using a mixed model of repeated measure. Study participants were elderly people (n = 499) with a mean age of 81.9 ± 5.56 years. Systolic and diastolic blood pressure decreased by 8.97 and 15.78 mmHg, and by 2.92 and 5.01 mmHg, respectively, at 4-year and 8-year monitoring. This demonstrates that home health care nursing is effective and has both short- and long-term benefits.
Introduction
In South Korea, the elderly (aged ≥65 years) account for 15.6% of the total population as of 2020, and this is projected to reach 24.5% in 2030, with the population-aging rate expected to accelerate more rapidly than any other country worldwide, especially in the “old-old” (aged ≥85 years) category (Statistics Korea, Citation2017). This means there will be a particularly rapid increase in the “middle-old” (aged 75–84 years) and “old-old” subgroups of the elderly population, both subgroups with high healthcare needs. The frailty phenotype of Korean elderly individuals described in the Cardiovascular Health Study is as high as 8.3–17.0%, calling for dedicated efforts to provide this population with adequate healthcare (Jang et al., Citation2019).
As a stage in the age-related disabling process before the onset of disease and functional decline in carrying out activities of daily living, frailty has serious implications for the health and quality of life of elderly individuals, who should be identified and managed as early as possible. Although most health problems in elderly individuals date back many years and may be exacerbated by decades-long lifestyle factors, older individuals often avoid seeking active care in health facilities, making it necessary for nurses to visit them at home to monitor their health status and lifestyles to deliver customized interventions (Chung et al., Citation2014). Thus, frailty management in elderly individuals in South Korea mostly began with community-led visiting health nursing programs (Ministry of Health and Welfare, Korea Health Promotion Institute, Citation2019).
In 2018, the prevalence of cerebrovascular and heart disease, which are the second and fourth major causes of death among Koreans aged 65 years and older, respectively, was 360.8 and 260.1 per 100,000 people, respectively (Statistics Korea, Citation2019). Frail elderly individuals tend to have chronic diseases such as hypertension, diabetes mellitus (DM), and hyperlipidemia, and are thus at a high risk of cerebrovascular diseases; they are also more likely to lack systematic health care, including daily exercise and regular visits to healthcare facilities (I. Lee & Jeong, Citation2012). In South Korea, 90% of the elderly population have one or more chronic diseases and 51% have three or more; specifically, 59.0% have hypertension, 29.5% have hyperlipidemia, and 23.2% have DM (Jang et al., Citation2019). The prevalence of cerebrovascular disease is also significantly higher in frail elderly individuals than in their non-frail counterparts (12.2% vs. 5.8%, I. Lee & Jeong, Citation2012).
There are three main types of home health care nursing in South Korea. The first type, home nursing service based on the Medical Service Act (Act No.16555, Article 33.4), is operated as an inpatient alternative service to increase hospital turnover in acute hospitals. This type of nursing is run by home nurse practitioners who have passed the national examination and have more than three years of clinical experience in providing health care services, including performing status checks of patients with early discharge from surgeries, and providing surgical wound treatment, and suture removal, simple treatment, clinical examination, and health education, etc. (Korea Ministry of Government Legislation, Citation2020). The second is home visit nursing as required by the Long-term Care Insurance Act (Act No. 16244, Article 23.1), and generally performed by nurses, home registered nurses (RNs), or aide nurses. These services are intended for elderly people over 65 years of age or those who have senile diseases such as dementia, stroke, and Parkinson’s disease, even if they are less than 65 years of age. The services cover mainly nursing care for the elderly such as checking the health status of subjects, health education, child care, urinary tract catheter change and management, treatment for bedsores, etc. (Korea Ministry of Government Legislation, Citation2019a). The third type is the visiting health care, as required by the Regional Public Health Act (Act No.16262, Article 11.5) (Korea Ministry of Government Legislation, Citation2019b). As a strategy of extending healthy living and improving health equity, the goal of the ‘National Health Promotion Comprehensive Plan’ is to provide health care services through health care teams, including nurses (Ministry of Health and Welfare, Korea Health Promotion Institute, Citation2019). Visiting health care is aimed at providing or linking to health care services by actively identifying the health problems of the vulnerable. These include those who have health problems, low-income families, multi-cultural families, and the elderly, those referred by local children centers, and community organizations (Ministry of Health and Welfare & Korea Health Promotion Institute, Citation2020). This study examines the third type of home health care nursing to evaluate the effectiveness of health care management among elderly people in the community.
Most studies on home health care nursing conducted in South Korea have examined short-term home health care nursing programs of less than one year, e.g., 8 weeks (Park & Oh, Citation2010; Yang et al., Citation2008) and 8 months (Chin et al., Citation2004). These also addressed blood pressure, blood glucose, depression, quality of life, bone density, obesity, and self-rated health status assessments; however, the results have varied from one study to another. No studies assessing the effects of long-term home care nursing services to check hypertension, DM, and hyperlipidemia status in frail elderly individuals have been carried out to date. A review of 21 non-Korean studies on community-level multifactorial interventions in frail and high-risk seniors revealed that these interventions help reduce risk of declining physical function, depression, falls, and nutritional deficiencies (Lightbody, Citation2002). However, some studies have reported no beneficial effects as regards incontinence, fall risk, depression, physical function, medication costs, hospitalization rate, average length of hospital stay, and number of emergency room visits (Coleman et al., Citation1999).
In this study, we evaluated the effects of long-term home health nursing care among frail elderly individuals in lowering blood pressure, blood glucose, and cholesterol levels. The results would be useful in designing effective health management programs for frail elderly individuals, which is gaining in importance due to the growing aging population globally.
Methods
Study design
We analyzed secondary data to note changes in blood pressure, blood glucose, and total cholesterol levels in participants over a period of 8 years starting from 2010. The sample population was registered in a home health care nursing program, run by a public health center in Seoul, South Korea.
Sample population and setting
We analyzed data from the public health care information system, established and operated by the Ministry of Health and Welfare of the Republic of Korea, for efficient processing of all materials and information necessary by public health centers and for the digitization of healthcare and management records. We were granted permission for only one month (March 2019) by the public health center to retrieve and review anonymized data on the characteristics of frail elderly individuals receiving home health care nursing, details of services delivered, and the effect of home health care nursing.
Participants
In 2010, 5,525 frail elderly individuals were registered for home health care nursing; visiting health nurses (RNs) provided services such as health care monitoring; identification of risky health behaviors and health risk factors; counseling and education for improving health practices; chronic disease management and complication prevention; and provision of information on health and welfare services. A home visit generally lasted 30 minutes to an hour. A total of 599 seniors satisfied the inclusion criteria (frailty score = 4–12 points at the time of registration, minimum period of management = 8 years; Source: Ministry of Health and Welfare, Korea Health Promotion Institute, Citation2019). Among the 599 elderly individuals eligible for the home health care nursing program managed for 8 years or longer, the percentage of high-risk frail elderly adults was 83.3% (n = 499/599). Thus, data from 499 frail elderly adults were analyzed.
A frailty assessment was performed using the 28-item questionnaire proposed in the Guideline for Visiting Health Care (Ministry of Health and Welfare, Korea Health Promotion Institute, Citation2019). The 28 items are grouped under 10 categories: instrumental activities of daily living (5 items: ability to use public transport, shop for small purchases, go to the bank, go out, and attend counseling); motor function (5 items: climbing stairs, standing from a chair, walking for 15 minutes, history of falling, and fear of falling); nutrition (2 items: weight loss and being underweight); oral health (3 items: eating, swallowing, and having a dry mouth), seclusion (2 items: number of outings per week and outing frequency compared to the previous year), cognitive function (3 items: forgetfulness, ability to make phone calls, and ability to recall past events), depression (5 items: in the previous 2 weeks), chronic disease (1 item: presence/absence of eight diseases, including hypertension and DM), sensory function (2 items: vision and hearing impairments), gait evaluation (1 item: timed up and go [TUG] test). One point each was assigned to a negative answer in the items including in the instrumental activities of daily living, motor function, oral health, seclusion, and cognitive function categories; respectively 0 and 2 points were assigned to the absence and presence of a chronic disease; for sensory function, 0 to neither vision nor hearing impairment, 1 to either impairment, and 2 to both impairments; for the TUG test, 0 to walking and returning 2.4 m in less than 8.5 seconds and 2 to 8.5 seconds or longer. Total scores ranged from 0 to 31 points, with higher scores indicating a worse condition (0–3 = healthy, 4–12 = pre-frail, and ≥13 = frail). We could not determine the reliability coefficient (Cronbach’s alpha) of the frailty assessment scale at the time of its development; however, in this study, Cronbach’s alpha was .819 at baseline, .742 at the 4-year monitoring, and .723 at the 8-year monitoring.
Ethical considerations
We received written consent from the relevant public health center to use the dataset; analyses were performed on the relevant data, which were entered into an Excel worksheet (MicroSoft, Redmond, WA, USA); no personal identifiers were used (name, ID number, address, telephone number, etc.). This study conformed to recognized standards of the Declaration of Helsinki (IRB no. 1041566–201903-HR-004-01).
Sample size and power
To determine whether the sample size was sufficiently large to have adequate power, we used sample size calculation software PASS 12 (NCSS; Kaysville, UT, USA; www.ncss.com). The minimum detectable time-dependent difference in measurements (three repetitions at the significance level of .05) was set to 0.29 – the regression coefficient of the time-dependent frailty score. Study power was 80% when the variance of the residuals of the fitted model was set to 2.25, and the autocorrelation coefficient at 0.6; the required sample size was 499.
Statistical analysis
A mixed model of repeated measures analysis was performed on the 8-year data. Dependent variables were systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), and total cholesterol levels. Each variable was adjusted for age, sex, income level, number of family members living in the household, and number of comorbidities. Model fitting was performed using the correlation matrix for AR(1) and the least square mean, and 95% confidence intervals were calculated from the fitted model for a period of up to 8 years from registration. Statistical analyses were performed using the R program version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Home health care nursing program for frail elderly individuals
The home health care nursing program provides public health education and counseling (e.g., promotion of physical activities, dietary management, oral management, urinary incontinence management, depression prevention, cognitive function improvement, fall prevention, etc.); oral gymnastics to improve oral functions such as mastication, swallowing, articulation, and saliva secretion; dementia-related healthcare; hobbies, support, and encouragement for social participation such as participation in religious activities; education about fostering a safe environment; and health education and emotional support for the registrants’ families or referrals to appropriate services.
The average number of annual home health care nursing visits by nursing staff per participant ranged between 4.72 and 8.75 times over 8 years. The visit cycle is determined based on the health status of the elderly and the ability to self-care. As visits are used in conjunction with other health services, it is difficult to determine whether the health status was related to the number of visits. The intervention provision rates in 2018 were as follows: 100% (every visit) for medication instructions, exercise therapy, nutritional instructions, emotional support, fall prevention education, and abstinence and hypertension education; 85.7% for hypertension management and complication prevention; 36.4% for DM management and complication prevention; and 24.2% for smoking cessation advice.
Results
Participants’ general characteristics
Participants’ demographic characteristics are shown in . The study population comprised 499 elderly persons with a mean age of 81.9 ± 5.56 years in 2018. Most participants were women (76.25); 48.6% of participants had an income less than the minimum cost of living, the mean number of family members was 1.41 ± 0.65, and the mean number of comorbidities was 3.88 ± 1.26.
Table 1. Participants’ general characteristics (n = 499)
Changes in blood pressure, blood glucose, and total cholesterol levels
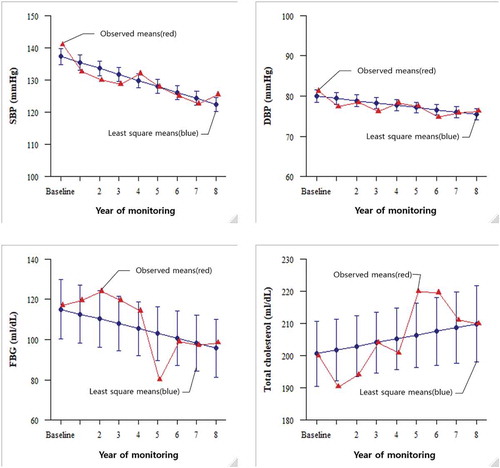
Measures of blood pressure, blood glucose, and total cholesterol levels were taken three times: at baseline, at the 4-year monitoring, and at the 8-year monitoring; these were compared to calculate changes between the three time points; sex, age, number of family members living in the household, number of comorbidities, and economic status were treated as covariates. SBP and DBP were significantly reduced at the 4- and 8-year monitoring. No significant changes in FBG or total cholesterol levels were noted at either follow-up ().
Table 2. Hypertension, diabetes mellitus (DM), and total cholesterol changes since registration
Factors associated with changes in blood pressure, blood glucose, and cholesterol levels in frail elderly individuals receiving home health care nursing
We analyzed the factors contributing to changes in participants’ biomarkers; the final measurements of blood pressure, blood glucose, and total cholesterol levels were set as dependent variables. Both SBP and DBP decreased significantly over time. SBP was higher in individuals in their 80s (vs. 70s) and in individuals with three or more comorbidities (vs. one). FBG levels significantly decreased as care continued. Total cholesterol levels were higher in women than in men ( and ).
Table 3. Factors associated with changes in blood pressure, blood glucose, and total cholesterol levels
Figure 1. Changes in blood pressure, blood glucose, and total cholesterol levels in participants during the monitoring period
Discussion
A paradigm shift from home health care nursing is underway, and it is necessary to verify the efficacy of the management of frail elderly individuals by visiting public health nurses (RNs). In our study, the longer the duration of home health care, the better managed was the blood pressure. It was particularly well-managed compared to DM or hyperlipidemia. Less efficacy is expected for DM and hyperlipidemia because these are heavily dependent on exercise and dietary interventions in addition to medication. It is necessary to develop and implement community-led programs to ensure exercise adherence and dietary management in recipients of hypertension, DM, and hyperlipidemia management services. Our study findings confirm the long-term effects of home health care nursing by visiting public health nurses in frail elderly adults. Visiting health nurses are key personnel for providing community-based, cost-effective health management in the elderly. Home health care nursing by visiting nurses had both short-term as well as long-term benefits; this study confirms that home health care nursing is a sustainable form of health care, especially due to the increase in the elderly population and the number of chronic diseases.
Geriatric frailty has been identified to be a major cause of sarcopenia (muscle loss with aging), overall physical and cognitive functional decline (Clegg et al., Citation2013), increased mortality (Morley, Citation2016), higher risk of falling (Kojima et al., Citation2015), and increased hospitalization and admission into long-term rehabilitation facilities (Clegg et al., Citation2013; Kojima et al., Citation2015). The awareness of the importance of timely frailty care is gaining traction since the earlier the onset of frailty care, the more efficient it is in preventing exacerbations. In this study, SBP and DBP significantly decreased at the 4- and 8-year follow-up visits compared to baseline, demonstrating that frailty care is increasingly effective over time. Better care outcomes were obtained in individuals in their 70s (vs. 80s) and in persons with one comorbidity (vs. three or more). When compared with two earlier studies, in which visiting healthcare was provided for 8 years, SBP and DBP decreased by 9.8 mmHg (P< .01) and 4.3 mmHg (P< .01), respectively (Chin et al., Citation2004), and by 26.7 mmHg (P< .01) and 11.2 mmHg (P< .01), respectively (Yang et al., 2008); the outcome measurements in our study indicate similar or slightly lower effects. However, compared with the mean age of participants in the earlier studies (67.7 and 70.0 years, respectively), the mean age in our study at baseline was slightly higher, and the fact that blood pressure was consistently reduced over the following eight years indicates that the intervention was highly effective.
While previous studies have dealt with short- and mid-term intervention periods of less than one year, this study is significant in that the frail old adults included were selected from among those registered in a home health care nursing program spanning 8 years. To date, only the degree of frailty had been monitored in this population (D. O. Lee & Chin, Citation2019). No other study had examined changes in blood pressure, blood glucose, and total cholesterol levels. In our study, non-significant changes were found in FBG levels at both follow-up visits. This was less effective than that reported in the two earlier studies, in which FBG levels decreased by 7.6 mg/dl (P< .01) (Chin et al., Citation2004) and 35.8 mg/dl (P< .01) (Yang et al., Citation2008) after an 8-week visiting healthcare follow-up. Nevertheless, the fact that FBG levels gradually decreased over time, without worsening after eight years, is an encouraging result.
No significant changes were found in total cholesterol levels at either follow-up visit compared to baseline; however, total cholesterol level was higher in women than in men. This result is similar to that of a previous study (Yang et al., 2008), in which no significant changes were obtained after an 8-week visiting healthcare follow-up. The reason that home nursing care was more effective in managing hypertension was because it is relatively easy to ensure drug adherence in hypertension as compared to DM or hyperlipidemia due to the greater dependence on medication. The nationwide hypertension medication adherence rate increased from 24.4% in 2000 to 71.6% in 2016 (H. Lee et al., Citation2019), which is an effect of long-term home health care nursing coupled with hypertension management by medical clinics. A non-Korean meta-analysis reported that a self-directed intervention program led by community nurses contributed to reductions in SBP and DBP by 3.04 mmHg and 1.42 mmHg, respectively, along with a reduction in glycated hemoglobin of 0.15 mg/ml (Massimi et al., Citation2017). Face-to-face interventions proved more effective than telephone interventions (Bosworth et al., Citation2005).
However, DM and hyperlipidemia require stricter dietary adherence than does hypertension. Frail elderly adults are at risk of malnutrition, especially those with lower education levels (Miettinen et al., Citation2017). In South Korea, 58.7% of elderly individuals require dietary guidance or improvement, and 51.9% are affected by a lack of exercise (Yang et al., Citation2011). Consequently, DM or hyperlipidemia management involving dietary control is more likely to be problematic compared to hypertension. Poor nutrition and lack of exercise are related to various factors such as economic capacity, ability to cook and exercise, and having social relationships with others who share and support these activities. Among older Koreans (aged 65 and older), the proportions of those who can independently shop and cook were 87.4% and 87.8%, respectively, which implies that 12–13% of all Korean seniors are in need of support for grocery shopping and meal preparation. Further, the proportion of those who had asked for free meals or lunchbox deliveries were 33.8% and 35.0%, respectively; whereas only 3.8% and 1.4% actually received such services, with demand by far surpassing supply (Chung et al., Citation2014). Such routine support is needed for community-dwelling older adults. In some areas, local women’s associations run social kitchens, growing vegetables themselves, and delivering cooked means to frail elderly adults. In fact, gathering together to grow vegetables and walking to a community eating place come with added health benefits (e.g., exercise and muscle strengthening), apart from improved nutritional status and fewer depressive symptoms (I. S. Lee et al., Citation2018). The widespread use of these could lead to better fragility management and care efficacy.
According to the 2014 National Survey of Older Koreans (Chung et al., Citation2014), the health status of elderly Koreans undergoes an abrupt downturn at around age 85 years, with rapid decline of physical activities; this appears as an inverted U-shaped relationship between age and safety accident rate on the graph; many are unable to sustain themselves independently when admitted to facilities due to an abrupt decline in public transfer income.
This study analyzed data collected over eight years by well-trained visiting health nurses, and its strength lies in the fact that it covers older individuals living in the community, that is, it was not limited to vulnerable groups. However, some study limitations should be noted. First, since we analyzed secondary health center data, there were no control groups; therefore, causation cannot be inferred. Long-term research is needed to compare communities with varied programs. Second, we analyzed data from those areas of Seoul with relatively high socioeconomic status. It is necessary to systematically analyze the data from all of Korea, including rural areas. Third, the community health center database did not include information on educational attainment, which has been identified as a high-risk factor for frailty (Hoogendijk et al., Citation2014). In our study, economic status was taken as a proxy and treated as a covariate. Given the impact of educational level on health status through the mediating effect of health literacy, it is necessary to include educational level in the community health center database. Finally, in addition to hypertension, DM, and hyperlipidemia, other indicators known to be associated with frailty in old age – such as depression, nutritional intake, and weight – should be included in any future analysis of the long-term effects of visiting healthcare.
Conclusions
Analyses of the 8-year data showed that hypertension management by visiting public health nurses was effective, DM was maintained at baseline levels (without exacerbation), although hyperlipidemia management did not improve. Given that the mean age of participants in this study was 72 years at baseline and that outcome measurements were taken eight years later, hypertension and DM care using visiting health nurses can be considered effective. However, it is necessary to integrate the visiting healthcare scheme into more systematic and comprehensive programs to ensure adequate nutritional intake and sufficient muscle strength via community collaboration such as social kitchens and strength training exercise adherence. Our study results have the following practical implications: 1) as blood pressure was significantly lowered and blood glucose levels were maintained, we believe that it is necessary to continue and expand the home health care nursing program. 2) Since blood glucose management becomes more effective over time, it is necessary to continue to provide these services and monitor their effects. 3) It is necessary to promote dietary control and lifestyle adjustment to enhance the effectiveness of home DM and hyperlipidemia nursing care. 4) Given that most frail elderly individuals live alone or with a spouse (who may also be old and frail), it is necessary to strengthen community-level cooperation for better health management.
Additional information
Funding
References
- Bosworth, H. B., Olsen, M. K., Gentry, P., Orr, M., Dudley, T., McCant, F., & Oddone, E. Z. (2005). Nurse administered telephone intervention for blood pressure control: A patient-tailored multifactorial intervention. Patient Education and Counseling, 57(1), 5–14. PMID: 15797147. https://doi.org/10.1016/j.pec.2004.03.011
- Chin, Y. R., Lee, I., & Chang, H. S. (2004). Analysis of the effects and nursing intervention of home health care in public health centers. Journal of KoreanAcademy of Community Nursing, 15(3), 353. https://jkachn.org/search.php?where=aview&id=10.12799/jkcn.2004.15.3.353&code=1200JKCN&vmode=FULL
- Chung, K. H., Oh, Y. H., Kang, E. N., Kim, J. H., Sunwoo, D., & Oh, M. A. (2014). A survey of the Korean older individuals in 2014. Sejong: Ministry of Health and Welfare, Korean Institute of Health and Social Welfare. https://www.kihasa.re.kr/web/publication/research/view.do?menuId=45&tid=71&bid=12&division=002&keyField=title&searchStat=2018&key=2014%EB%85%84%EB%8F%84+%EB%85%B8%EC%9D%B8%EC%8B%A4%ED%83%9C%EC%A1%B0%EC%82%AC&ano=1879.
- Clegg, A., Young, J., Iliffe, S., Rikkert, M. O., & Rockwood, K. (2013). Frailty in older people. The Lancet, 381(9868), 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
- Coleman, E. A., Grothaus, L. C., Sandhu, N., & Wagner, E. H. (1999). Chronic care clinics: A randomized controlled trial of a new model of primary care for frail older adults. Journal of the American Geriatrics Society, 47(7), 775–783. https://doi.org/10.1111/j.1532-5415.1999.tb03832.x
- Hoogendijk, E. O., van Hout, H. P. J., Heymans, M. W., van der Horst, H. E., Frijters, D. H. M., Broese van Groenou, M. I., … Huisman, M. (2014). Explaining the association between educational level and frailty in older adults: Results from a 13-year longitudinal study in the Netherlands. Annals of Epidemiology, 24(7), 538–544.e2. https://doi.org/10.1016/j.annepidem.2014.05.002
- Jang, I.-Y., Lee, H. Y., & Lee, E. (2019). Geriatrics fact sheet in Korea 2018 from National Statistics. Annals of Geriatric Medicine and Research, 23(2), 50–53. https://doi.org/10.4235/agmr.19.0013
- Kojima, G., Kendrick, D., Skelton, D. A., Morris, R. W., Gawler, S., & Iliffe, S. (2015). Frailty predicts short-term 320 incidence of future falls among British community-dwelling older people: A prospective cohort study nested within a randomised controlled trial. BMC Geriatrics, 15(1), 155. https://doi.org/10.1186/s12877-015-0152-7
- Korea Ministry of Government Legislation (2019a). Long-term care insurance act. Seoul. The Government of the Republic of Korea. http://www.law.go.kr/engLsSc.do?tabMenuId=tab45#.
- Korea Ministry of Government Legislation (2019b). Regional public health act. Seoul. The Government of the Republic of Korea. http://www.law.go.kr/engLsSc.do?tabMenuId=tab45#.
- Korea Ministry of Government Legislation (2020). Medical service act. Seoul. The Government of the Republic of Korea. http://www.law.go.kr/engLsSc.do?tabMenuId=tab45#liBgcolor17.
- Lee, D. O., & Chin, Y. R. (2019). The follow-up study of changes in frailty in elderly receiving home health care of the public health center. Journal of Korean Academy of Community Health Nursing, 30(4), 528. https://doi.org/10.12799/jkachn.2019.30.4.528
- Lee, H., Park, S., & Kim, H. C. (2019). Temporal and geospatial trends of hypertension management in Korea: A nationwide study 2002–2016. Korean Circulation Journal, 49(6), 514–527. https://doi.org/10.4070/kcj.2018.0358
- Lee, I., & Jeong, I. S. (2012). Frailty level and health-related characteristics among participants of a tailored home visiting service. Journal of the Korean Geriatrics Society, 16(2), 74–83. https://doi.org/10.4235/jkgs.2012.16.2.74
- Lee, I. S., Lee, Y. J., Lim, E. S., Chin, Y. R., Lee, K. U., & Hong, H. J. (2018). The community empowerment program plan for vitalizing city. Seoul National University.
- Lightbody, E. (2002). Evaluation of a nurse-led falls prevention programme versus usual care: A randomized controlled trial. Age and Ageing, 31(3), 203–210. https://doi.org/10.1093/ageing/31.3.203
- Massimi, A., De Vito, C., Brufola, I., Corsaro, A., Marzuillo, C., Migliara, G., … Damiani, G. (2017). Are community-based nurse-led self-management support interventions effective in chronic patients? Results of a systematic review and meta-analysis. PLoS One, 12(3), e0173617. https://doi.org/10.1371/journal.pone.0173617
- Miettinen, M., Tiihonen, M., Hartikainen, S., & Nykänen, I. (2017). Prevalence and risk factors of frailty among home care clients. BMC Geriatrics, 17(1), 266. https://doi.org/10.1186/s12877-017-0660-8
- Ministry of Health and Welfare & Korea Health Promotion Institute (2020). Integrated community health promotion project guidelines: Home health care. Sejong. Seoul. Korea Health Promotion Institute. https://www.khealth.or.kr/kps/publish/view?menuId=MENU00890&page_no=B2017003&pageNum=1&siteId=&srch_text=&srch_cate=&srch_type=&str_clft_cd_list=&str_clft_cd_type_list=&board_idx=10348.
- Ministry of Health and Welfare, Korea Health Promotion Institute. (2019). Guideline for visiting health care. Korea Health Promotion Institute.
- Morley, J. E. (2016). Frailty and sarcopenia: The new geriatric giants. Revista De Investigacion Clinica, 68(2), 59–67. https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=65968
- Park, J. S., & Oh, Y. J. (2010). The effect of case management for clients with hypertension. DM registered in customized home visiting health care services. Journal of Korean Public Health Nursing, 24(1), 135–150. http://dx.doi.org/10.5932/JKPHN.2010.24.1.135
- Statistics Korea. (2017, December 7). Estimation of future population. The Government of the Republic of Korea. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA401&conn_path=I2
- Statistics Korea. (2019). Older individuals statistics. Daejeon. The Government of the Republic of Korea. https://www.kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=377701.
- Yang, S.-O., Kwon, M. S., Choi, Y.-J., & Lee, S.-H. (2011). The effects of a case management program of customized home visiting health service for clients with arthritis. Journal of Korean Academy of Community Health Nursing, 22(2), 151. https://doi.org/10.12799/jkachn.2011.22.2.151
- Yang, S.-O., Ahn, S. Y., Yim, E. S., & Kwon, M. S. (2008). The effects of customized home visiting health service in Gangwon-do - Focused on hypertension and DM Clients. Journal of Korean Academy of Community Health Nursing, 19 (1), 88. https://jkachn.org/search.php?where=aview&id=10.12799/jkachn.2008.19.1.88&code=0200JKACHN&vmode=FULL
