Abstract
We conducted a study to determine current maternal, infant, and young child nutrition (MIYCN) and family planning (FP) practices and how practices can be improved with counseling. The study consisted of qualitative methods. Mothers and couples were able to attempt and adopt new practices after only one counseling visit, except consuming meat daily due to cost, and adopting contraception, which was challenging due to health system constraints. Most appreciated receiving information, reported positive experiences, and said they would continue practices. It is possible to improve these practices through counseling, although some systems factors should be addressed.
Women with children under two years are the most vulnerable to poor health and nutrition. Globally, 45% of child deaths are attributed to poor maternal, infant, and young child nutrition (MIYCN) (Black et al., Citation2013). Short interpregnancy intervals increase the risk of morbidity, malnutrition, and mortality in women and children (Conde-Agudelo, Rosas-Bermudez, Castaño, & Norton, Citation2012; Rutstein, Citation2005). Optimal MIYCN and family planning (FP) practices have mutually beneficial effects on maternal and child health. We designed a study to inform and guide programs in Yemen. For this purpose, we used a methodology, Trials of Improved Practices (TIPs), which is based on market research techniques and is widely applicable across health, nutrition, and other disciplines to design evidence-based programs for their implementation context. In this study, our focus was on interventions to address maternal nutrition, optimal breastfeeding practices in the first 6 months, postpartum return to fecundity, postpartum contraceptive options including the lactational amenorrhea method (LAM), optimal complementary feeding from 6–23 months, and continued breastfeeding through at least 2 years. The study team also explored implications for couple communication and household decision-making. In this paper, the authors present the TIPs study findings and implications for future integrated programing in Yemen and other developing countries.
Background
The investigators conducted this study in two districts of Dhamar, Yemen, which is south of the capital of Yemen, Sana’a city. The study used the TIPs methodology to inform evidence-based, integrated programing to address high rates of malnutrition, short interpregnancy intervals, and low contraceptive prevalence in the country. Our objective was to assess mothers’ and couples’ ability to adopt recommended MIYCN and FP practices after counseling.
Despite deterioration of the economy in the last several decades and political instability recently, there had been some improvements in FP indicators in Yemen at the time of the study. The total fertility rate declined from 6.5 in 1997 to 4.4 in 2013 (Republic of Yemen, Citation2015). Even with this positive change, however, the fertility rate remains high. Only 29% of married women ages 15–49 were using a modern contraceptive method, according to the 2013 Family Health Survey. However, two national surveys found there was little change in proportion of stunted children <5 years between 1997 (48%) and 2013 (47%). (Yemen Demographic Health Surveys, Citation1997 and 2013.) Infant and young child feeding practices remain poor, with only 13% of babies exclusively breastfed in the first 6 months after birth and only 15% of children ages 6–23 months receiving a minimum acceptable diet, as defined by the World Health Organization (WHO, Citation2010).
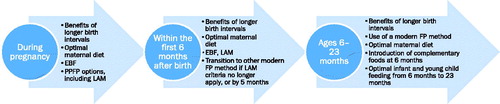
Packaging or integrating MIYCN and FP interventions and counseling together can improve the efficiency of client–provider interactions, performance of doctors, nurses, midwives, and health para-professionals and the comprehensiveness of clients’ exposure to key MIYCN-FP services. In addition, the focus on use of recommended MIYCN and FP practices together has the potential to maximize impact on improved health and nutrition status in mothers and children. shows the similar timing of MIYCN and FP interventions. Although the integration of FP and MIYCN information and services has numerous potential benefits, FP and MIYCN services are generally not offered together. Thus, opportunities for intensive interpersonal counseling for both FP and MIYCN, which has been shown to improve the uptake of health and nutrition practices, are being missed (Kim et al., Citation2016). The researchers sought to use research findings to identify successful strategies for increasing exposure to information about and uptake of optimal practices through integrated MIYCN and FP services, which has not been widely documented in the literature.
Methods
TIPs and research themes
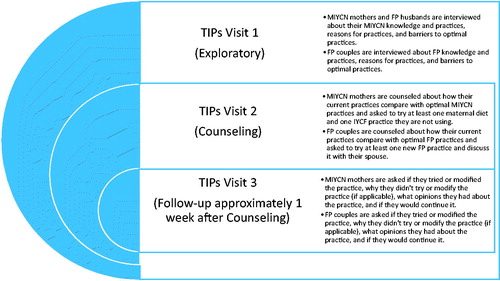
The study was primarily qualitative, using the TIPs methodology (Dickin, Griffiths, & Piwoz, Citation1997), which is used to test practices that a program intends to promote, creating an opportunity to identify barriers and facilitating factors for the uptake of optimal practices based on people’s actual experience with trying new practices. The TIPs process consists of three visits by members of the research team: an exploratory visit; a counseling visit – with tailored counseling, drawing from an iterative counseling guide based on international recommendations (MCHIP, Citation2014, WHO, Citation2010, Citation2016) and based on the findings from the first visit – including identification, with the mother and couples, of a new practice she/they can try; and a follow-up visit to assess changes in practices and discuss challenges. describes the application of the TIPs methodology in this study.
Sampling
The research team conducted the study in two districts, Wesab Assafel and Maghreb Ans, representing two of the main agro-ecological zones in the governorate (lowlands and highlands) known to influence food supply and, therefore, what people eat. The research team selected one village per district, in consultation with the governorate health team, with the aim of including a highland community in Maghreb Ans and a lowland community in Wesab Assafel. The governorate health team contacted village leaders to request their permission to conduct the study and to identify potential respondents. The research team used a maximum variation sampling approach to select households with children <2 years old, in order to include a variety of socioeconomic strata and geographic locations (e.g., proximity to health facility and road).
Respondents
The study included TIPs visits with 32 mothers and 16 fathers of children <2 years. Eight mothers from each district were interviewed mainly about MIYCN practices (“MIYCN mothers”) but also about their use of FP methods. Eight mothers and their husbands from each district were interviewed about FP practices (“FP couples” or “FP husbands and wives”). Although the study initially intended to assess both MIYCN and FP use among all respondents, the length of the assessments precluded this, and different mothers were identified as MIYCN mothers and FP wives. To respect cultural norms, male research staff interviewed husbands and female research staff interviewed wives. MIYCN mothers were selected to include equal numbers of children from four age groups under 2, and equal numbers in two nutritional status categories (well-nourished or malnourished). The research team also conducted key informant interviews with two grandmothers, two community leaders, and two health workers in each district for a total of 12 key informants. The total sample and respondent characteristics for the study are presented in the results.
Training and dates of field research
Field staff, composed of health and development professionals, received training on optimal MIYCN and FP practices, the protection of human subjects, TIPs methodology, the application of research instruments, and how to weigh and measure length of children to determine their nutritional status so that the sample represented both well and undernourished children. The field research took place in December 2013 and January 2014.
Analysis
Field staff took handwritten notes in Arabic on printed interview guides and began processing and analysis of data in the field, synthesizing majority and minority responses on data review forms that organized results by themes based on ideal practices. They discussed each day’s research with the research team in the evening and supervisors checked forms and asked field staff to address missing information (e.g., answers not recorded). The notes were translated into English so that all the co-investigators could read the responses. Co-investigators and field staff gathered for an analysis workshop after the fieldwork to review the data, address gaps or inconsistencies as needed, and discuss and further synthesize results. The research team conducted all analyses by hand by tallying majority and minority responses and identifying quotes that were representative of the responses. The authors present illustrative responses as quotes in the results.
Human ethics approval
The Johns Hopkins School of Public Health’s institutional review board in the United States approved the study protocol and instruments. The Ministry of Public Health and Population in Yemen also reviewed and approved the study. The research team obtained verbal informed consent from all participants. Consent forms, which were read to participants, explained participation in the study and its purpose (to learn about MIYCN and FP to design an intervention). Due to possible sensitivities, FP couples were required to agree as a couple to participate.
Results
In this section, the description of the study participants, along with findings from the TIPs visits and key informant interviews, are presented. Findings are grouped according to the specific recommendations made to FP couples and MIYCN mothers during the second (counseling) visits based on the observations in the first (exploratory) visits.
The planned number of MIYCN mothers (16) and FP husbands and wives (16 each), a total of 48 respondents, was reached, and all respondents completed the study. includes the gender and ages of children of MIYCN mothers and FP couples.
Table 1. Gender and ages of children of MIYCN mothers and FP couples by district.
There were no ethical concerns or sensitivities detected in or reported by the MIYCN mothers or the FP couples when discussing any of the subject matter.
Characteristics of respondents
All mothers in the sample ranged in age from 19 to 40, with a median age of 28. Fathers ranged in age from 23 to 53, with a median age of 29.5. All mothers had between 1 and 14 children; the median number of children was 3.5. Mothers and fathers in Wesab Assafel had more children than those in Maghreb Ans. Among study respondents, fathers were older and more educated than mothers. All but one of the mothers with some secondary school or above resided in Maghreb Ans. The MIYCN mothers had completed fewer years of education than the FP wives. More than half of the mothers in the study (20 of 32) had not completed any schooling.
More than half of the mothers in the study worked outside the house, either throughout the year or seasonally. Most mothers reported that their husband lived at home, although one mother was a widow and two reported that their husbands lived abroad. Fathers reported having a variety of occupations, with the majority working as either farmers or laborers.
In addition to the 48 TIPs participants, 12 key informants (grandmothers, community leaders, and health workers) completed in-depth interviews. Grandmothers and community leaders were older—all 35 years old or older. All four grandmothers had no formal education while three community leaders had some secondary education.
FP practices
shows the TIPs results for each FP recommendation made during the counseling visit (visit 2) by district. The table is followed by a description of the visit 1 (exploratory) context and the visit 3 (follow-up) results for each recommendation made during the counseling visit.
Table 2. FP results by recommendation and type of respondent.
Discuss FP and reproductive intentions with spouse
Visit 1 Context. FP couples in both districts widely supported using FP, even if they were not using it themselves. No husband expressed opposition to FP, and only one appeared to show ambivalence, indicating, “I do not mind if my wife wants it.” Couples reported that they were comfortable discussing FP with each other. One mother mentioned, “I don’t want more children and when I talk to my husband about FP methods, I feel comfortable.” Two of four grandmothers said they talked to their sons and/or daughters-in-law about using contraception and delaying the birth of another child.
Only half of the couples stated that they wanted another child. Several wives said they were tired of being pregnant and giving birth. Most of those who wanted another child wanted to wait at least 2 years to get pregnant, although two husbands said another pregnancy would depend on Allah’s will. Husbands were concerned about the expense of having too many children. A few husbands were concerned about the safety and reliability of contraceptives, even if they were using a method.
Among couples using FP, all husbands expressed that the decision was made with their wives. However, two-thirds of husbands not using a method and most grandmothers and community leaders reported that husbands have the final say about contraceptive use.
Visit 3 Results. Couples who committed to trying to discuss FP and their intentions with each other succeeded. Although two wives (one from each district) were not asked to try this practice, their husbands approached them to discuss FP. The couples reported that they felt comfortable and satisfied discussing FP together. Several mentioned that they had developed a plan to visit the health facility together or decided which method to use. One husband reported that he was glad to share responsibility for FP decisions. Another said he spoke with his wife about FP and they reached “mutual understanding and sharing opinions between parents.”
Go to the health facility for information about FP
Visit 1 Context. Half of FP wives and more than half of FP husbands stated that health workers were the most common source of information about FP, followed by mass media. Several wives mentioned that they had little or no knowledge about FP or that they had concerns about side effects of contraception. Among the eight couples using FP before the TIPs study, six husbands said they went with their wives to the health facility, and some of these husbands took part in FP counseling. Health workers confirmed that more husbands were coming in to “listen to the advice.” The other two husbands had given their wives permission to go to the health facility alone.
Visit 3 Results. Thirteen FP husbands and 11 wives agreed to go to the health facility for information about FP. These included both current FP users who were interested in switching methods and nonusers who were interested in learning more about FP. Twelve husbands tried and nine succeeded in visiting the health facility. All 11 wives tried and eight succeeded. One husband in Maghreb Ans spontaneously went to the health facility for FP information. Couples were motivated to obtain information about FP because they wanted to delay the next pregnancy. Several husbands wanted either to learn more about FP or to switch methods due to side effects or concerns about efficacy. Couples who sought health services experienced challenges in receiving services, largely due to the lack of female health providers. These challenges were experienced more often in Wesab Assafel than in Maghreb Ans. One wife said, “It is shameful and not acceptable to deal with male staff in such matters in our tradition.” In spite of the obstacles, wives were determined to receive FP services. One wife went back to the health facility daily and another three times in a week, but no female staff were there. Another wife said, “I will keep visiting health services until I find the right service provider.”
One couple from Wesab Assafel tried to go to the health facility for more information about FP options (including potentially switching from pills to an intrauterine device [IUD]), but was unsuccessful due to a lack of provider availability. “I went to the health center and didn’t find anyone to take advice from.” The husband also mentioned that he was aware that IUDs were not available at the local health facility, so if they decided to switch to an IUD, they would have to travel to a health facility in the city, which they could not afford. “There is not enough money to get an IUD at the city and the health center nearby does not provide that.”
A couple with a 4-month-old infant also agreed to visit a health facility for more information about contraception. The wife went to the health facility with female neighbors, but she did not receive the information because there was no female provider there. The husband said he set a date to go, but he did not go because he decided he wanted more children and so changed his mind about using FP.
The husband who spontaneously went to the health facility was concerned about side effects associated with the method his wife was using. Visiting the health facility reassured him to continue FP. He said, “I was against FP methods. However, after visiting health services and listening to the manager’s and midwife’s advice, I was convinced about the advantages of FP methods.”
Start using modern FP method
Visit 1 Context. Respondents generally saw using FP to space births as a means to allow women to rest between pregnancies, improve their physical and mental health, and give them more time to care for their children. However, one husband stated that “there is no benefit from birth spacing … but from Allah [God].” The majority of key informants supported FP use. Modern contraceptive use among respondents was high in Maghreb Ans; all but one of the FP couples were using a method. In Wesab Assafel, only one FP couple used modern contraception. FP use in both districts was low when children were 0–5 months old and increased when children reached 6–11 months. Contraceptive pills were the most common method used, followed by injectables and tubal ligation. Two mothers were using unregistered, high-dose, once-per-month hormonal contraceptive pills from China.
The main reasons respondents gave for not using FP were concerns about side effects, the perception that they were not at risk of pregnancy, costs associated with obtaining contraception, and partner opposition. When asked what could increase their FP use, respondents cited education about methods, making FP available and affordable, making female health workers available, agreement from husbands to use FP, and sharing success stories about FP. One woman reported that a health worker had told her to come back for FP after her menses returned, putting her at risk of a pregnancy before her menses returned.
Visit 3 Results. Eight couples not using FP agreed to start using a modern method. However, only one couple, from Maghreb Ans, was successful in adopting this practice. After receiving counseling from the midwife, the wife agreed to take pills until her menses became more regular and then consider switching to an IUD.
One couple not using FP had 14 children (the youngest was 15 months). They agreed to visit the health facility, motivated by the TIPs counseling. They succeeded in going to the health facility, but during the screening, they found out that the wife was pregnant.
Couples encountered a lack of female providers. In addition, contraceptive methods were in short supply from public providers and too expensive from private providers. One couple mentioned that they were turned away for an IUD by a private provider who encouraged them to return once the wife’s menstruation finished. Another wife was advised against using contraception due to poor health.
Consider using LAM
Visit 1 Context. LAM is a modern, temporary contraceptive method based on the suppression of ovulatory activity through breastfeeding. With correct use, it is more than 98% effective in preventing pregnancy. To use LAM, women must meet three simple criteria: they must practice exclusive breastfeeding (EBF), they must not have resumed menstruation after childbirth, and they must have an infant <6 months old. Promotion and use of LAM as an option for postpartum women has the potential to increase both the duration of EBF and the continued use of FP at 1 year postpartum (Ahmed et al.,2015; Bongiovanni et al.,2005). None of the TIPs participants with babies <6 months old were using LAM, although half had heard of using breastfeeding for FP (not LAM, per se). No one knew all three LAM criteria, and none of the women with infants <6 months old were exclusively breastfeeding. Half of the wives knew that they could get pregnant before menstruation returned. However, others thought that they could get pregnant only after their menses began again. Most women reported wanting to breastfeed for 2 years to prevent another pregnancy. Many mothers reported thinking that they were protected from pregnancy for as long as they breastfed, regardless of exclusivity or duration.
Visit 3 Results. The wife with a 4-month-old infant was advised to exclusively breastfeed, which she tried. She reported that her baby had no diarrhea, cried less, and slept better. However, she felt that she did not have enough breast milk to continue the practice, so she introduced food to her baby. One of the other two couples with a baby <6 months had an infant who was close to reaching 6 months; the wife in the other couple had experienced a return of menstruation.
Discuss benefits of FP with others in the community
Visit 1 Context. When asked about their main sources of information on FP, several women mentioned friends, neighbors, and female relatives. Several husbands mentioned the importance of sharing stories of successful and satisfied users. Couples had strong opinions about why they wanted to limit their family size or delay their next pregnancy and the benefits of FP methods in helping them to do so.
Visit 3 Results. All four wives trying this recommendation were successful in carrying it out. The husband of one of these wives spontaneously spoke with others about the benefits of FP. All respondents said they felt satisfied when speaking with and motivating others. One wife said, “I liked talking to women about the importance of FP methods. They responded to my advice and decided to go to health services to choose a suitable method for them.”
All four wives said that they would continue to speak with others about FP. One said, “I will sit with our village women in social gatherings to advise them about how to breastfeed, bring up their children, stay healthy… . I would recommend all women use FP and tell them how it made me comfortable and gave me more time to care for my children, husband, and house.”
MIYCN practices
Ten of the 16 children in the sample were malnourished (stunted, wasted, or underweight; ≤ −2 standard deviations from the median for the reference population for each indicator) (WHO, Citation2016). Five of the six children who were considered well-nourished were above but close to the cutoff for malnutrition (≤ −2 standard deviations), suggesting that they were vulnerable to becoming malnourished in the future.
shows the MIYCN TIPs results for breastfeeding practices, and shows the MIYCN TIPs results for food intake for mothers and children 6–23 months old. There were no obvious differences between districts, so these results are not disaggregated by district.
Table 3. MIYCN results: breastfeeding practices for infants and children.
Table 4. MIYCN results: dietary practices in mothers of children <2 years and feeding for children 6–23 months.
Breastfeeding for infants 0–5 months
Visit 1 Context. Through interviews and observations, mothers revealed that they valued breastfeeding, but they were not exclusively breastfeeding. No babies under 6 months were being exclusively breastfed, and only one child 6–23 months old had been exclusively breastfed. In the first hours after birth, the majority of babies were given colostrum, but half also were given prelacteal feeds. Based on the observations, practices were not optimal: Babies were incorrectly positioned and were breastfeeding infrequently, for short durations, or from only one breast. Half the mothers complained that they did not have “adequate breast milk,” which they equated with babies crying after breastfeeding or all the time. This problem triggered the introduction of food and liquids. Grandmothers and health workers also reported that insufficient breast milk was a problem.
Visit 3 Results. Three mothers with infants 2 months old or younger succeeded in EBF. They liked this practice, were supported in using it by their families, and said they would continue EBF and recommend it to others because they had more breast milk, their baby was healthier, and EBF would prevent another pregnancy. One mother also repositioned her baby to ensure proper attachment while breastfeeding. The mothers commented that they had never heard that babies <6 months old only needed breast milk. One mother commented, “The more breast milk I have, the more my baby breastfeeds.” Another mother described herself as “more relaxed about breastfeeding because my breast milk increased” with EBF.
The fourth mother’s baby was 5 months old and had been introduced to foods (e.g., sugary biscuits, potatoes, bananas) starting at the second month. While this mother tried to exclusively breastfeed and tried to breastfeed on each breast for 15 minutes, she could not continue because her baby was crying. She felt her breast milk was not adequate and the baby was not getting sufficient nutrition. She commented that mothers need to give biscuits to children who cry because biscuits make them “quiet and comfortable.” Although the mother could not continue EBF, her husband felt that their baby would be healthier if she could.
Breastfeeding for children 6–23 months
Visit 1 Context. All but one child 6–23 months old were still breastfeeding. One mother was advised by her doctor to stop breastfeeding because of the medication she was taking. Many mothers were breastfeeding only once in 24 hours. Inadequate breastfeeding practices observed included incorrect positioning, not breastfeeding from both breasts, and breastfeeding for short durations.
Visit 3 Results. Four of five mothers tried and succeeded at breastfeeding from and emptying both breasts and at breastfeeding at least six to eight times in 24 hours. All of these mothers reported that they liked the practice because “breast milk increased,” “my baby is not hungry, and is sleeping in a normal way,” and “it will make him grow.” One mother reported that breastfeeding more often “makes me feel relaxed and happy.” Mothers said they would continue better breastfeeding practice(s) and recommend them to others because “it is healthy for our children.” One mother said she would continue these practice(s) for at least 2 years; another said she would continue them until “my baby grows up.”
Families encouraged mothers to use the practices because they thought the practices would benefit the child and the mother. Three of the mothers agreed to try some additional practices to improve breastfeeding. One agreed to try breastfeeding during the night and succeeded in doing so. She reported that she was supported by her family and would continue the practice for 2 years and would recommend it to other mothers because her baby was more satisfied.
Two mothers were asked to reposition their baby while sitting, presumably because they were holding the baby awkwardly. Both mothers tried and succeeded with the new position. They felt positive, happy, and relaxed with the new position and would continue to use it and recommend it to others because it was “beneficial to my own health and the health of the infant.” One mother who tried this practice modified it by lying down, which she found more comfortable.
Increase the number of meals per day
Visit 1 Context. Three-quarters of MIYCN mothers were consuming at least three meals a day, but less than half of their children were consuming the minimum number of meals per day. Mothers identified problems with feeding their children, such as the child not wanting to eat or being sick. Half of mothers had strategies to entice children to eat, such as playing with or breastfeeding the child. Other mothers said they would try again at the next meal.
Visit 3 Results. Mothers’ Results. One mother was successful in increasing the meals she consumed. Another mother did not try because she became sick, but she agreed to try the practice in the future. The mother who succeeded in using the practice daily said she liked the practice, which her family encouraged her to use, because she felt healthier and thought she had more breast milk. She said she would continue eating more food for at least 6 months and would recommend it to others because it was beneficial to her and “important for breastfeeding.”
Children’s Results. Three mothers succeeded in increasing the meals they provided to their children; two received the recommendation to increase meals for their children and the third decided on her own to use the practice. Mothers reported that feeding more to their children improved their child’s sleep, made the child more active while awake, caused the child to demand even more food, and resulted in better nutrition. Mothers reported that they felt “relaxed and happy” about providing more food to their children. They said they would continue doing so and would recommend the practice to others because “I feel my child is eating in a better way.” Two mothers were supported by their families in using this practice, and one mother received no feedback from her family about it.
Vary the diet
Visit 1 Context. Mothers were asked what foods they had consumed and fed to their children ages 6–23 months on the day before the interview. Some mothers and most children ages 6–23 months were consuming diets with a limited number of food groups. Lack of dietary diversity was a greater problem among the children, particularly those 6–8 months old, than among their mothers. Dietary diversity improved as children grew older. One-quarter of children received sugary foods daily and nearly half received sugary foods two to three times per week.
Visit 3 Results. Mothers’ Results. Twelve out of 13 mothers tried the practice and nine were successful in using the practice daily. These mothers liked the practice because they felt either that they had more breast milk or that they were healthier. Two mothers had better appetites and another mother felt calmer because she had more breast milk. All mothers said they would continue the practice and recommend it to others, but one mother stated that she could continue the practice only when she had enough money to buy all the foods.
Three mothers tried and liked the practice but modified it because not all the recommended foods were available or affordable every day—particularly fruits, vegetables, and meat. One mother liked the idea of varying her diet and said she would recommend the practice to other mothers who had sufficient food, but she was unable to try the practice herself because she felt she needed to prioritize feeding her eight children.
Half of the mothers using the practice daily, even those who modified it, said their families had encouraged them to use the practice because it would benefit the mother and child. The other half said that no family members gave their opinion about the practice or encouraged the mother to use it. When mothers were probed about why family members did not give their opinion or encouragement about using the new practices, mothers reported their family were not aware that they were trying it.
Children’s Results. Seven of eight mothers were successful in varying their child’s diet. Four mothers succeeded in using the practice daily. One mother was asked to stop giving her baby sugary biscuits and to vary the child’s diet, which she was able to do. Mothers felt positively about the practice because it was “suitable for my child and will help my baby grow” and improved appetites. Two out of four mothers said they would continue to use the practice without modifying it. Two mothers said they would not be able give all of these foods every day in the future, but they would give the foods when they were available. “Meat is expensive and not available every day but [when] we have it, my baby will receive some.” All mothers said they would recommend the practice.
Three mothers modified the practice because not all the foods were available. Giving meat daily was not possible. Mothers believed in and would recommend the practice even if they could not practice it or had to substitute foods. They appreciated the benefits of dietary diversity for their child’s health, including prevention of diarrhea, more satisfied appetite, enhanced mood, and better sleep.
One mother did not try varying her child’s diet because she became sick and also could not afford all the foods daily. She liked the idea of the practice and said she would use it in the future and would recommend it to others. Almost all mothers received encouragement from their family to use the practice.
Do not give a feeding bottle
Visit 1 Context. One mother reported using a bottle, not to give milk or formula, but to feed a thin porridge. Research staff reported that this was a common practice in many areas of Yemen.
Visit 3 Results. The mother who was using a feeding bottle stopped using it and used a spoon and glass instead when feeding her baby. She liked the practice because her baby’s diarrhea stopped and her baby “slept more and played more.” She said she would not use the feeding bottle in the future and would recommend this to others as a way to decrease diarrhea. While family members were supportive of the new practice, they also commented that “most babies are fed with a bottle” which may imply some resistance to change.
Do not give tea; give milk instead
Visit 1 Context. One-third of children were receiving tea daily and more than half were given tea two to three times per week.
Visit 3 Results. Two mothers tried this practice and succeeded. They liked the practice and said they would continue using it because they felt their children were healthier and “eating in a better way” without tea. Their families supported the practice.
Discussion
In this study, we found that mothers and couples were able to attempt and adopt new practices after only one counseling visit. All FP wives and all but two FP husbands tried the practices they accepted. Most practices were successfully adopted by respondents. One exception was starting a method of contraception, which was generally not adopted due to challenges related to the health system.
The MIYCN mothers succeeded in adopting one or more new breastfeeding practices. Both MIYCN mothers and FP wives had trouble returning to exclusive breastfeeding when their babies were older (4-5 months). Two MIYCN mothers with babies two months of age or younger succeeded in returning to exclusive breastfeeding. Most who accepted the recommendation to increase the number of meals they consumed and/or the diversity of their diets or to adopt one or more new infant and young child feeding practice(s) succeeded in doing so. In many cases, trying optimal practices facilitated continued use because the practices resulted in positive outcomes for the mother and child (e.g., the child crying less and sleeping more), which created a positive feedback loop. Respondents generally indicated a lack of knowledge and a dearth of opportunities in their communities to learn about MIYCN and FP. They were appreciative of the opportunity to learn more about optimal practices and receive motivational support during the counseling session.
The authors are not advocating for just one counseling contact in FP and MIYCN programs. Mothers and couples need ongoing counseling to reinforce continued use of new practices and the adoption of other new practices as they and their children reach new milestones. Nutrition outcomes have improved as exposure to counseling messages increased in community-based nutrition programs (BASICS, Citation2008; Kim et al., Citation2016).
Findings from our study are consistent with other studies that have demonstrated the value of the TIPs methodology in giving mothers and couples new information about optimal practices and empowering them to select and try new practices (Government of Malawi, Citation2011; Kavle et al., Citation2015). This study makes a unique contribution in using the TIPs methodology for evidence-based, integrated FP and MIYCN programming. The study team was interested in exploring these two themes together because MIYCN and FP practices during pregnancy and the first 2 years of life reinforce one another and the timing of milestones is similar. The ability of TIPS methodology to inform multi-disciplinary counseling and programing suggests it could also be valuable for other disciplines within the social sciences. Results from this study also add to the limited literature on use of qualitative methods to explore determinants of MIYCN and FP practices in Yemen specifically.
Fathers and mothers were open to discussing their FP and reproductive intentions together, and several participants were able to speak about the benefits of FP with others in their community. In spite of respondents’ willingness to try new practices, however, numerous barriers, including a lack of female providers at the health facility, contraceptive stock-outs, and the prohibitively high cost of contraceptive methods from private providers, hindered FP uptake. These barriers need to be addressed in future programing.
Breast milk is a valued food for babies, and all mothers in the study breastfed. However, breastfeeding practices need to be improved to ensure that breast milk supply is adequate and to meet the three LAM criteria if mothers choose to use this FP method. In this context, it is clear that babies need to be fed more frequently, from both breasts, and for longer durations. Counseling about optimal breastfeeding practices and strategies for addressing common breastfeeding challenges are needed during pregnancy, immediately after and in the first week after birth, and during the first 6 months after birth. Although most families had access to a diverse diet, children were not receiving many of the foods that other family members were eating because mothers and fathers thought these foods were appropriate only for older children. In addition, some foods, such as meat, were not available on a daily basis due to cost. It is important to ensure that mothers and families prioritize meat and other animal foods to children when they have them and have opportunities to learn how to prepare foods that children can eat (e.g., via recipes and demonstrations on grinding, mashing foods). When meat and other animal foods are not available, parents should know what to substitute for meat, for example, when it is not available (e.g., legumes, eggs), and how to responsively feed children—based on their hunger and satiety cues and nutrition needs—to meet their energy and nutrient requirements.
Ministries of livestock and agriculture might need to implement programs to increase families’ access to animals. Food and micronutrient supplements might be needed for certain families.
Through an analysis of national surveys, Rutstein found that as interpregnancy intervals increase, stunting and underweight in children <5 years decrease (Rutstein, Citation2005). Informing parents about the role of FP, along with optimal infant and child feeding, in preventing malnutrition can reinforce the use of modern contraception. Based on this TIPs research, the study team revised the iterative counseling guide and developed an integrated MIYCN-FP counseling guide with MIYCN-FP counseling cues and tailored messages for each contact with couples and mothers (Assabri et al, Citation2016). Project staff disseminated study results and the counseling guide to the Ministry of Public Health and Population (MOPHP) and stakeholders in a national workshop in Yemen before the current political conflict. Donor agencies continue to assist the MOPHP to use the results of the study.
Limitations of the study
Several deviations from the original study plan occurred. For the FP TIPs, the original plan was to allow 10–14 days between the counseling visit and the follow-up visit. However, due to challenges with aligning site visit schedules across the two districts, the follow-up visits to MIYCN mothers and FP couples occurred only 7 days after the counseling visit. More couples might have started an FP method if there had been more time between the visits.
In several cases, research team members deviated from recommendations that were included in the counseling guide, adjusting the recommendation or adding recommendations that were not included in the guide.
The research team decided not to record the interviews, as they deemed it culturally inappropriate at the time of the fieldwork. The quotes used in the results are, therefore, taken from what the field staff wrote on the intake forms and are not direct quotes from respondents.
It would have been useful to future TIPs studies if mothers had tried to add specific foods or amounts of foods and then commented on why they were or were not able to add the specific foods and amounts. Other studies have shown that increasing the amount of foods added to children’s diets is problematic for mothers, either because this process needs to be gradual or because mothers do not believe children can consume as much food as is recommended (Government of Malawi, Citation2011).
Although study results identified barriers to optimal practices, the study methodology was not designed to allow for determination of the underlying causes of health systems constraints—for example, why female health staff or FP commodities were not available at the public health service sites. These barriers affected the results for couples who agreed to go to the health facility for FP services and/or to obtain a modern contraceptive method.
The penetration of unregulated commercial FP commodities and foods of low nutritional value (“junk foods”) is a risk to health and nutrition. However, the study team did not explore how to address this problem. Authors of recent studies have found significant use of such foods among young children in the Middle East (Kavle et al., Citation2015) and this appears to be a problem in Yemen as well.
Conclusions
Opportunities exist to address perceptions and promote optimal practices related to fecundity after childbirth, postpartum contraceptive uptake, and MIYCN. With counseling and accurate information about optimal practices, which was not widely available, mothers and couples can make changes in their MIYCN and FP practices, even in a resource-constrained country like Yemen. Results underscore the importance of gender, couple communication, and household decision-making in influencing nutrition and family planning practices. Support from family members played an important role in the uptake and continuation of these practices. Although there are barriers that reduce the use of optimal practices, many of these barriers can be overcome by working with the public and private sectors to address health workforce constraints and increase the availability of modern contraceptives and certain foods. Designers of programs in any context worldwide can apply the TIPs methodology for formative research with program beneficiaries to ground their work in evidence. Findings from this study can be used to inform future efforts to provide integrated MIYCN and FP counseling and programing at each contact with mothers and families (from antenatal care through child health contacts) and to address these health and nutrition needs to improve maternal and child health outcomes in Yemen.
Acknowledgments
This study was made possible by the generous support of the American people through the United States Agency for International Development (USAID), under the terms of the Leader with Associates Cooperative Agreement GHS-A-00-08-00002-00 and Cooperative Agreement AID-OAA-A-14-00028. The contents are the responsibility of The Maternal and Child Health Integrated Program (MCHIP) and The Maternal and Child Survival Program (MCSP), and do not necessarily reflect the views of USAID or the United States Government.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ahmed, S., Ahmed, S., McKaig, C., Begum, N., Mungia, J., Norton, M., & Baqui, A. (2015). Effect of integrating family planning with a maternal and newborn health program on postpartum contraceptive use and optimal birth spacing in rural Bangladesh. Studies in Family Planning, 46(3), 297–312.
- Assabri, A., Cooper, C., Al-Gendari, K. A., Pfitzer, A., & Galloway, R. (2016). The power of counseling: Changing maternal, infant, and young child nutrition and family planning practices in Dhamar, Yemen. Washington, DC: The Maternal and Child Survival Program. Retrieved from: https://www.mchip.net/sites/default/files/Yemen%20MIYCN-FP%20TIPs%20Report.pdf
- BASICS (2008). Evaluation of the AIN-C program in Honduras. Arlington, VA: BASICS and USAID.
- Black, R. E., Victora, C. G., Walker, S. P., Bhutta, Z. A., Christian, P., de Onis, M., … Uauy, R. … Maternal and Child Nutrition Study Group. (2013). Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet, 382(9890), 427–431. doi:10.1016/S0140-6736(13)60937-X
- Bongiovanni, A., Samam’h, M., Al’Sarabi, R., Masri, S., Zehner, E., & Huffman, S. (2005). Promoting the Lactational Amenorrhea Method (LAM) in Jordan increases modern contraception use in the extended postpartum period: LINKAGES’ final report of its LAM research in Jordan. Retrieved from: http://pdf.usaid.gov/pdf_docs/Pnadh002.pdf
- Conde-Agudelo, A., Rosas-Bermudez, A., Castaño, F., & Norton, M. H. (2012). Effects of birth spacing on maternal, perinatal, infant, and child health: A systematic review of causal mechanisms. Studies in Family Planning, 43(2), 93–114. doi:10.1111/j.1728-4465.2012.00308.x
- Dickin, K., Griffiths, M., & Piwoz, E. (1997). Designing by dialogue: A program planners’ guide to consultative research for improving young child feeding. Washington, DC: The Manoff Group and Academy for Educational Development/Sara Project.
- Government of Malawi. (2011). Consulting with caregivers: Formative research to determine the barriers and facilitators to optimal and young child feeding in three regions of Malawi. Washington, DC: Government of Malawi, the World Bank, USAID, and USAID’s Infant and Young Child Nutrition Project.
- Kavle, J. A., Mehanna, S., Saleh, G., Fouad, M. A., Ramzy, M., Hamed, D., … Galloway, R. (2015). Exploring why junk foods are “essential” foods and how culturally tailored recommendations improved feeding in Egyptian children. Maternal & Child Nutrition, 11(3), 346–370. doi:10.1111/mcn.12165
- Kim, S. S., Rawat, R., Mwangi, E. M., Tesfaye, R., Abebe, Y., Baker, J., … Menon, P. (2016). Exposure to large-scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLoS One, 11(10), e0164800. doi:10.1371/journal.pone.0164800
- Maternal and Child Health Integrated Program (2014). A guide for planning and implementing social and behavior change communication activities for postpartum family planning. Baltimore: Jhpiego.
- Republic of Yemen. (1997). Yemen demographic and maternal and child health survey. Sana’a, Yemen: Demographic and Health Surveys. Central Statistical Organization.
- Republic of Yemen. (2015). Yemen National Health and Demographic Survey 2013. Rockville, MD: Republic of Yemen, Ministry of Public Health and Population and the Central Statistical Organization, Pan Arab Program for Family Health, Egypt, and Measure DHS, ICF International.
- Rutstein, S. O. (2005). Effects of preceding birth intervals on neonatal, infant and under-five mortality and nutritional status in developing countries: Evidence from the Demographic and Health Surveys. International Journal of Gynecology & Obstetrics, 89, S7–S24. doi:10.1016/j.ijgo.2004.11.012
- World Health Organization. (2010). Indicators for assessing infant and young child feeding practices: Part III; country profiles. Geneva, Switzerland: World Health Organization Press.
- World Health Organization. (2013). Programming Strategies of Postpartum Family Planning. Retrieved from: http://www.who.int/reproductivehealth/publications/family_planning/ppfp_strategies/en/
- World Health Organization. (2016). WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva, Switzerland: World Health Organization Press.