Abstract
A research-to-action collaboration sought to understand and respond to barriers to female genital fistula treatment in Nigeria and Uganda. This was guided by appreciative inquiry, a participatory approach for transformative programing with four phases: (1) inquire, (2) imagine, (3) innovate, and (4) implement. Through this process, partners designed and refined a treatment barrier reduction intervention using multiple communication channels to disseminate a consistent fistula screening algorithm and provide transportation vouchers to those screening positive. Partnership between an implementation organization, a research institution, and local community partners enabled data-driven design and patient-centered implementation to address specific barriers experienced by women.
A genital fistula is an abnormal opening in the female genital tract that causes uncontrollable, constant leakage of urine and/or feces. Common causes include obstructed Labor without timely medical intervention, surgical error, most often during cesarean section or gynecological surgery, and injury, such as sexual violence or traumatic injury. In low-income countries, particularly in sub-Saharan Africa and South Asia, obstetric fistula is the most common type, although the proportion of iatrogenic cases appears to be increasing (EngenderHealth, Fistula Care Plus, 2016; Raassen, Ngongo, & Mahendeka, 2014). Ministries of Health, public and private donors, and nongovernmental organizations have invested in establishing surgical fistula treatment services in many countries with an identified fistula burden. However, there are many women with fistula who have not yet reached fistula care and are not well-served by current outreach and/or service delivery models. Comparing estimates of the fistula burden, whether obtained from community surveys or estimation models, with the number of women served annually at fistula treatment sites (http://globalfistulamap.org) suggests a persistent backlog of untreated fistula cases (Dolea & AbouZahr, 2003; Tunçalp, Isa, Landry, & Stanton, 2014). However, because measuring the prevalence and incidence of fistula is challenging and it can be difficult to locate or sample untreated women who have not sought care, there has been limited information on the profile of unserved women living with fistula (Adler, Ronsmans, Calvert, Filippi, 2013; Tunçalp, Tripathi, Landry, Stanton, & Ahmed, 2015). Collaborators at EngenderHealth and the Population Council implemented a research to action partnership in order to understand:
Who and where are these women?
What barriers do they face in seeking, reaching, and receiving fistula care?
What interventions would address these barriers?
Research to action through appreciative inquiry
Background
The USAID-supported Fistula Care Plus (FC+) Project is a five-year initiative managed by EngenderHealth. The Population Council is a research partner under the FC + Project. As part of FC+, EngenderHealth and the Population Council are collaborating to increase knowledge on access barriers and test responsive program intervention.
Following a literature review, Population Council staff developed a conceptual framework illustrating nine key barriers to accessing fistula treatment, adapted from the three delays model for maternal mortality (Baker, Bellows, Bach, Warren, 2017). The literature review also identified the limited implementation or evaluation of interventions to respond to barriers to accessing fistula treatment.
In 2015, the Population Council team conducted formative qualitative research in Nigeria and Uganda, to understand barriers to and enablers of fistula care, particularly from the perspective of women with fistula, family members and other community stakeholders. In-depth interviews and focus group discussions were conducted with purposively sampled respondents in Ebonyi and Kano States in Nigeria and Hoima and Masaka Districts in Uganda (Keya, Sripad, Nwala, & Warren, Citation2018; Sripad & Warren, Citation2016; Warren, Agbonkhese, & Ishaku, 2016). Informed by the findings of this formative research, EngenderHealth, Population Council, and local partners collaborated to design an intervention aimed at improving access to fistula treatment. The fistula treatment barrier reduction intervention was implemented in the catchment areas of two fistula treatment facilities in Nigeria – National Obstetric Fistula Center (NOFIC) in Abakaliki, Ebonyi State and NOFIC in Babbar Ruga, Katsina State – and one facility in Uganda – Fistula Clinic at Kitovu Mission Hospital in Masaka District.
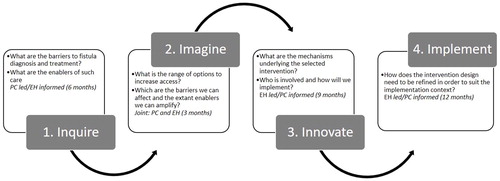
In this research-to-action partnership, collaborators relied on the adapted appreciative inquiry model as a conceptual guide. Appreciative inquiry is a participatory action-research approach that focuses on positive practices and aspirations within a social system, accounts for values and perspectives of stakeholders, and leads to transformative programing (Ludema, Cooperrider, & Barrett, 2001). In adapting this model, the collaborators drew on appreciative inquiry’s use in project development and evaluation; where each phase informs the next (Coghlan, Preskill, & Tzavaras Catsambas, 2003). illustrates this adapted model, which includes the process phases of inquire, imagine, innovate and implement, as well as the key questions and lead actor at each stage. The process of designing, refining, and initiating implementation of the fistula treatment barrier reduction intervention is described below, according to each phase of the appreciative inquiry model.
Inquire phase – research findings on treatment barriers and enablers
By employing formative qualitative research, the research-to-action partners uncovered numerous barriers to fistula treatment, but also an array of enablers, primarily created by communities themselves, to help women with fistula. First, the researchers documented widespread lack of awareness about fistula’s causes and treatment among women with fistula, their family members, and the general public, despite years of outreach and communication about fistula by EngenderHealth and other actors. The findings indicated that stigma prevents women from participating in community events where fistula and other women’s health issues are discussed and hinders open discussion of symptoms with peers in their social networks and even with community-based health workers.
Through the qualitative research, collaborators also identified a number of enablers that support women in becoming aware of, seeking, and receiving fistula treatment services. Community members indicated that mass media (e.g., radio) may improve fistula knowledge and treatment by directly reaching women not well-served by community-based, in-person approaches. Other identified enablers to improve access to fistula care include financial assistance for transportation and psychosocial support.
The findings also suggested that care-seeking decisions are not made exclusively or even primarily by women with fistula. Numerous “gatekeepers” influence whether, when, and how women with fistula symptoms seek services. Marital partners or in-laws, frequently serve as barriers to accessing care and may even ostracize or abandon women, further isolating some women living with fistula. Conversely, family members, particularly parents, can also have a positive, enabling role in care-seeking behaviors, providing financial and/or social support.
Through the qualitative research, the collaborators learned that barriers to appropriate treatment exist within the health system as well. Respondents suggested that inadequate knowledge among primary health care (PHC) workers can keep women from reaching appropriate fistula care. Many health workers are not well-informed about fistula or the existence of fistula treatment centers, and therefore are unable to provide correct referrals. In some cases, health workers may even attempt to provide treatment at lower-level facilities without adequate training or knowledge. The findings also illustrated the notable degree to which fistula information and services have been organized around the needs or perceptions of health system stakeholders, as opposed to affected women.
Through qualitative research, the research-to-action collaborators identified a number of sources of variation between research sites. For instance, in Ebonyi State (Southeastern Nigeria), the “standout” barriers appeared to be severe stigma about fistula and lack of awareness or correct information about fistula treatment. In Kano State (Northern Nigeria), the most important barrier appeared to be costs related to transportation; care for the patient; and having an accompanying person, as traveling alone is socially unacceptable for women. In Uganda, drivers were more likely to express concerns about transporting women who may be leaking feces or urine than in the Nigeria sites. Additionally, in Uganda, mobile phone-based payment appeared a feasible option for reimbursing transportation costs, whereas such networks and infrastructure were not as well-developed and adopted in the parts of Nigeria where the qualitative research was conducted.
provides a list of barriers to and enablers of fistula treatment identified in the qualitative research.
Table 1. Barriers to and enablers of fistula treatment identified through qualitative research.
Imagine phase – collaborative process of identifying potential intervention
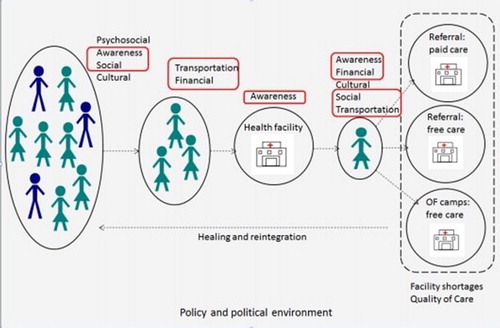
EngenderHealth and Population Council partners discussed the formative research findings and identified potential strategies for an intervention to empower women with fistula symptoms and promote direct access to fistula treatment. The findings demonstrated numerous points at which women can ‘fall through the cracks’ as they move through the stages of care seeking, due to awareness, socio-cultural, financial, transportation, and health system barriers. The Population Council team developed a diagram illustrating this attrition process (see ), which helped the collaborators imagine different points of intervention (Warren et al., Citation2018). While many extant strategies such as community outreach or free medical care address a single barrier to fistula treatment, the research-to-action partners sought to design a comprehensive intervention that reflects awareness of and response to the full array of barriers in , which an individual woman might encounter across the care seeking process. The enablers identified through the qualitative research also helped guide the partners in intervention strategies, providing examples of potential solutions that are already acceptable to women and present in their communities to a limited extent. The findings indicated that existing enablers and coping mechanisms help some women access treatment, but that they require amplification, linkage, and consistent provision to reach all women facing barriers to fistula treatment and prevent the attrition illustrated in .
Considering the barriers and enablers identified during the inquiry phase, during the imagine phase the partners were guided by several key principles:
Centering the intervention on women who have not been well-served by existing strategies.
Ensuring accurate and consistent fistula information and screening messages.
Deploying multiple communication channels.
Minimizing gatekeepers and wasted time.
Facilitating social support to fistula clients.
Innovate phase – Intervention design
Through this collaborative process, the EngenderHealth team designed an intervention with the following elements:
Three channels for fistula messages and screening: mass media and a free phone hotline, community agents, and primary health facility workers.
One consistent screening algorithm across these channels.
One referral enabler for all positively-screened women: a voucher for free transportation with a companion to and from an accredited fistula treatment facility.
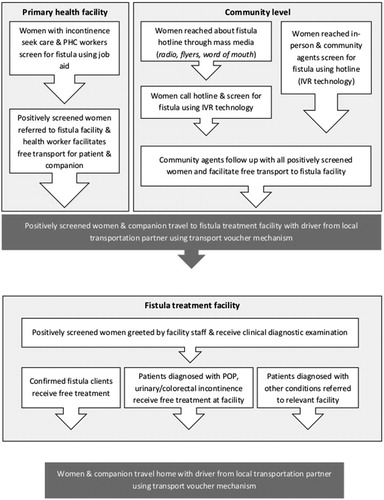
The intervention strengthens screening and referral mechanisms at primary health facilities and within communities through phone-based communication and community agents. summarizes the actors in the intervention, including key local partners and numbers trained to implement the intervention.
Table 2. Intervention partners.
The EngenderHealth team trained health care workers (doctors, midwives, nurses, and community health care workers) at primary health facilities across the catchment areas to identify and screen potential fistula clients, using a paper-based job aid, and refer these women for treatment. Additionally, community agents and PHC workers follow up with positively screened women and facilitate their free transport to the fistula treatment facility using a transportation voucher designed for the intervention. Community agents also follow-up with women who call into the hotline on their own and facilitate their free transport to the facility with a transportation voucher. Individuals across all three screening channels – community agents, health workers, and the hotline staff – collect the same data, using the same screening algorithm. The key fistula symptom question within this algorithm is, “Do you currently experience constant leakage of urine or feces from your vagina during the day and night even when you are not urinating or trying to urinate?”
Key components of the intervention include:
Local partnerships: The EngenderHealth team identified appropriate local partners in each of the intervention areas to fulfill the different implementation roles and provide feedback and learning on the implementation process. These local partners, listed in , included the staff of primary health facilities, fistula treatment facilities, existing community outreach networks, and transportation providers.
PHC workers: PHC workers are essential to identifying suspected fistula cases, as primary health facilities are often the first point of contact for women with fistula symptoms. EngenderHealth supported the training of PHC workers (doctors, midwives, nurses, and community health care workers) across health facilities in each of the three intervention areas. The three-day PHC worker training was designed to increase knowledge of genital fistula; strengthen capacity to screen for fistula; and build skills for the provision of quality emergency obstetric and newborn care, with a focus on fistula prevention. The training also enabled PHC workers to review key messages for fistula prevention and treatment, including the importance of sending potential fistula cases to accredited fistula treatment centers, rather than attempting treatment at primary health centers. Finally, trainees received guidance on how to participate in the intervention (e.g., screen patients using a standardized job aid and provide the transport voucher).
Fistula screening hotline: Through the fistula hotline, women are screened for fistula using interactive voice response (IVR) technology and the delivery of prerecorded messages to callers about how and where to get fistula treatment. Advertisements for the hotline are disseminated through radio announcements, community agents’ outreach activities, and culturally appropriate graphic flyers designed for audiences with limited literacy. Callers “flash” into the toll-free number and receive a prompt call back. Callers are instructed to select their preferred language. In Nigeria, the hotline is available in Igbo, Hausa, Pidgin, and English, and in Uganda, the hotline is available in Luganda. Callers are asked their age, followed by the key fistula symptom question noted above. For women who answer “yes,” questions are asked using the IVR technology to collect data on demographics, fistula etiology, and experienced barriers to treatment. Women who screen positively within the intervention catchment areas hear a recorded message that a community agent will follow up with them via phone within four days. Positively screened callers outside the catchment area receive a follow-up SMS and voice message with referral information about the nearest fistula treatment center. Box 1 describes the innovative nature of this intervention element.
Community agents: Community agents serve multiple roles in strengthening fistula screening and referral systems at the community level and providing in-person support to socially isolated women living with fistulas. Community agents participated in a two-day training that aimed to equip them with the knowledge and skills to screen women for fistula using the IVR hotline and refer them for treatment, as well as to promote healthy practices before, during, and after childbirth and monitor maternal health care-seeking and pregnancy outcomes in their communities.
Transportation voucher: The collaborators partnered with three local transportation providers, one in each intervention site – the National Union of Road Transport Workers (NURTW) in Ebonyi, Aba Jamil Car Hire Services in Katsina, and Lukaya Taxi Operator Cooperative Society Limited (LUTOCs) in Kalungu. In Nigeria, each positively screened woman and a companion of her choosing are entitled to a free round-trip to and from the fistula treatment facility. However, if there is a backlog of patients waiting for surgery at either of the fistula facilities in Nigeria, then the diagnosed fistula client and her companion are entitled to two free round trips to and from the facility, so they can return later for treatment. In Uganda, each positively screened woman and a companion of her choosing are entitled to two free round-trips to and from the fistula facility – one for diagnosis and another for treatment during a scheduled fistula treatment camp – due to the service model used for fistula treatment at the Uganda treatment facility. Each transportation voucher has a unique identifier and multiple copies to enable close monitoring of how it is utilized.
Through the intervention, the research-to-action partners seek to cover all women living with fistula, avoiding assumptions that a single channel of information or referral is feasible or acceptable for every client. illustrates the pathways in which women with fistula symptoms are identified, screened, and referred for fistula care within the community and at PHCs. Abiding by the principles outlined during the imagine phase, the partners seek, through the intervention, to make fistula diagnosis and treatment more woman-centered, thereby improving access. In this context, woman-centered means approaches to services that are:
Informed by, realistic about, and responsive to gender-related barriers.
Holistic, working within the community and inside the health facility.
Attentive to the ways that women ‘fall through the cracks’ as they seek effective care.
For example, through formative research in Nigeria, particularly in Kano, the research-to-action collaborators learned that social norms and long distances to care make it difficult for women to travel to fistula care sites alone. Therefore, the transportation voucher automatically includes an accompanying person. Similarly, the emphasis on a consistent screening algorithm and immediate referral to the fistula center is a response to findings in the formative research that women can get ‘stuck’ at the primary health facility level, unable to reach health workers who have accurate knowledge of fistula diagnosis, evaluation, and management.
Box 1. Interactive voice response: Using digital health innovation to address barriers faced by women.
A central innovation of the intervention is the use of interactive voice response (IVR) technology to mitigate key barriers faced by women: stigma, gatekeeping by family members and/or PHC workers, distance from health service points and related transportation challenges, and low literacy levels among both community members and community agents. The EngenderHealth team collaborated with VOTO Mobile, now Viamo, to design a free fistula hotline that screens callers for fistula and collects data on positively screened callers. Digital health tools have frequently been used to “push out” health information in the region, however using such platforms for screening and referral is novel. The IVR approach tackles the barriers discussed above in specific ways. For women reluctant to seek face-to-face services to discuss their fistula symptoms, IVR provides a way to report these symptoms and receive accurate information directly without in-person interaction. Further, most partners employing digital health approaches have relied on SMS and other text-based platforms out of reach to community members who cannot read or write – IVR eliminated this barrier. The IVR hotline was field-tested to ensure that community members viewed the voice actors as credible and nonthreatening, that important terms were appropriately translated for local dialects, and that the process of using the hotline felt clear and simple. The EngenderHealth team also trained community agents to screen women for fistula using the hotline, so that limited literacy among this cadre does not hinder the ability to screen and refer women who do feel comfortable interacting with community peers. Finally, as using the hotline eliminates the requirement for travel to a specific health service site for initial screening and referral, the partners aimed to address challenges related to family and health worker gatekeeping, transport, and costs faced by some women with fistula. The IVR approach may address barriers to screening, referral, and treatment for other health issues faced primarily by geographic isolated, low-literacy, and otherwise marginalized populations.
Implement phase – Adapting and delivering in the community
As the intervention was developed and launched, EngenderHealth headquarters and in-country staff identified areas needing revision and refinement to better match community realities and needs. The EngenderHealth team sought advice and input from local partners and other organizational resource persons to refine and adjust aspects of the intervention. This was a highly iterative and collaborative process, largely informed by feedback from in-country community mobilization specialists, who are attune to the realities on the ground. Examples of issues for refinement include:
Density of and existing structures of community agents
EngenderHealth staff identified existing community structures in both countries to implement the community outreach activities under this intervention. In Nigeria, community-based organization (CBO) partners selected volunteers to serve as community agents in the catchment areas. In Uganda, community agents for the intervention were selected from the existing network of Village Health Team members (VHTs), a mechanism supported by the Ugandan Ministry of Health. Leveraging these existing structures ensures that the selected community agents have the capacity to do the work and promotes sustainability. Despite these advantages, the ratio of community agents to community members differs across the countries, posing challenges to program fidelity. In Uganda, there are roughly five VHTs assigned to one village, whereas in Nigeria, the selected CBOs assign one community agent to roughly 30 villages. In response, EngenderHealth selected one VHT per village in Uganda in order to reduce the density of community agents, but at the same time, not disrupt the geographic assignments of the VHTs. Thus, the density of community agents remains greater in Uganda than in Nigeria, which may result in greater saturation of outreach activities in Uganda than in Nigeria.
Variation in transportation coverage across the two countries
In addition to the density of community agents, differences in radio coverage between the two countries also posed a challenge to program fidelity. In Uganda, radio messages advertising the fistula screening hotline can be restricted to the catchment area of the intervention (i.e., district-level); however, in Nigeria, radio messages cannot be restricted to the intervention’s catchment areas (i.e., LGA). Instead, radio messages air throughout an entire state. Since the hotline advertises free transport, the EngenderHealth team modified its approach in Nigeria to ensure the intervention adheres to ethical standards. In Nigeria, community agents provide follow up to positively screened women calling from anywhere in Ebonyi or Katsina States, not just the intervention’s LGAs, and facilitate free transportation to and from the treatment facilities.
Literacy level of community agents
Initially, the EngenderHealth team planned to utilize a paper-based job aid for the community agents, similar to the one provided to the PHC workers. This would enable assessment of differences in women’s experience of barriers to fistula care between women reached in person by a community agent and women who learn about the hotline through mass media and are presumably more socially isolated. However, shortly after the community agents were selected, EngenderHealth country staff learned that many are nonliterate. Through consultations with partners, the community-based screening approach was modified, with the community agents using the IVR hotline to conduct facilitated screenings.
Multiple users per mobile phone and maintaining confidentiality when following up via phone
During the implementation phase, the partners discussed how best to follow-up with positively-screened callers. In some cases, multiple people may be using the same mobile phone, resulting in potential confidentiality breaches when community agents follow up with the phones numbers of positively screened callers. In order to ensure confidentiality and not disclose information to the wrong person during follow-up, the EngenderHealth and Population Council team consulted VOTO Mobile (now Viamo) staff and established a protocol whereby a CBO/VHT coordinator would make the initial follow-up call to the positively screened phone number and ask the person answering whether they recently completed a mobile-based survey asking medical questions. If the respondent answers positively, this would confirm that the person on the phone is the hotline caller. If the person is unaware of the survey, then the CBO/VHT coordinator would inquire to see whether there are any other users of the phone and ask to speak with them.
As the refined intervention is implemented in the three catchment areas, the research-to-action collaborators are conducting a quasi-experimental process and effectiveness evaluation, triangulating qualitative and quantitative data from community and health system sources as well as IVR hotline data to understand whether and how the intervention has promoted access to fistula treatment.
Feasibility and replication considerations
The research-to-action partnership adapting the appreciative inquiry model enabled the collaborators to design and implement a data-driven, client-centered approach responding to barriers experienced by women living with fistula. Collaboration also facilitated innovation and refinement throughout the process, by drawing on diverse perspectives and areas of expertise during design and implementation. Such partnerships may enable other actors to create health information and service delivery interventions for a variety of other public health concerns that primarily affect vulnerable and marginalized populations.
As with other iterative and participatory design models and implementation processes (e.g., human-centered design), concerns may be raised about feasibility, particularly logistics, cost, and timeframe requirements of the appreciative inquiry approach. In assessing whether this approach is suitable for specific health issues or contexts, partners should determine whether existing program or service delivery approaches are working effectively. For instance, if resources are already being expended on training and service provision models that do not successfully reach their target audiences or reduce the mortality or morbidity burden, then the added inputs and resources required for an iterative program revision or design cycle may lead to net savings for the health system. In the case of fistula screening in low-resource settings, the long durations of living with the condition reported by many patients, the gap between the estimated burden and numbers treated, as well as the findings of qualitative research that there are barriers that reduce the effectiveness of existing education and case-finding approaches, all suggest that new approaches are necessary to ensure that women with fistula are able to connect to care (Baker et al., Citation2017; Landry et al., Citation2013; Tunçalp et al., 2014).
It is recommended that partners applying this approach incorporate sustainability planning from the start. This may include evaluation or research components to generate evidence regarding the efficacy or cost-effectiveness of the intervention or service delivery models resulting from application of appreciative inquiry. Because existing, ‘indigenous’ actors in a community or health system may not have the resources to add the logistical, coordination, or supervisory layer that may be available during the pilot or externally funded program phases, it is also important to assess the value and effort required for each component of a complex intervention separately, to understand whether separately sustained or scaled-up elements can still address the challenges identified through the appreciative inquiry stages.
In the case of the fistula research-to-action partnership described here, the collaborators are conducting an effectiveness evaluation and will disseminate the findings to community-based stakeholders and national policymakers in each implementation country, to promote the sustainability and adoption of relevant intervention components.
Conclusion
Collaboration between actors from an implementation organization, a research institution, and local community partners enabled data-driven design and patient-centered implementation to address specific barriers experienced by women with fistula. Applying the appreciative inquiry approach strengthened this collaboration and ensured responsive program implementation in a dynamic community and service delivery context.
Disclosure statement
The authors declare that we have no competing interests.
Additional information
Funding
References
- Adler, A. J., Ronsmans, C., Calvert, C., & Filippi, V. (2013). Estimating the prevalence of obstetric fistula: A systematic review and meta-analysis. BMC Pregnancy and Childbirth, 13(1), 246.doi:10.1186/1471-2393-13-246
- Baker, Z., Bellows, B., Bach, R., & Warren, C. (2017). Barriers to obstetric fistula treatment in low-income countries: A systematic review. Tropical Medicine & International Health, 22(8), 938–959. doi:10.1111/tmi.12893
- Coghlan, A. T., Preskill, H., & Tzavaras Catsambas, T. (2003). An overview of appreciative inquiry in evaluation. New Directions for Evaluation, 2003(100), 5–22. doi:10.1002/ev.96
- Dolea, C., & AbouZahr, C. (2003). Global burden of obstructed labour in the year 2000. Geneva: World Health Organization.
- EngenderHealth, Fistula Care Plus (2016). Iatrogenic fistula: An urgent quality of care challenge (Technical Brief). New York, NY: V. Tripathi & K. Levin. Retrieved from Fistula Care Plus website: https://fistulacare.org/wp-fcp/wp-content/uploads/2015/10/Iatrogenic-fistula-technical-brief_2016-1.pdf
- Keya, T. K., Sripad, P., Nwala, E., & Warren, C. (2018). “Poverty is the big thing”: exploring financial, transportation, and opportunity costs associated with fistula management and repair in Nigeria and Uganda. International Journal of Equity in Health, 1(1), 1770.
- Landry, E., Frajzyngier, V., Ruminjo, J., Asiimwe, F., Barry, T. H., Bello, A., … Barone, M. A. (2013). Profiles and experiences of women undergoing genital fistula repair: Findings from five countries. Global Public Health, 8(8), 926–942. doi:10.1080/17441692.2013.824018
- Ludema, J. D., Cooperrider, D. L., & Barrett, F. J. (2001). Appreciative inquiry: The power of the unconditional positive question. In P. Reason & H. Bradbury (Eds.), Handbook of action research (pp. 189–199). London: SAGE Publications Ltd.
- Raassen, T. J., Ngongo, C. J., & Mahendeka, M. M. (2014). Iatrogenic genitourinary fistula: An 18-year retrospective review of 805 injuries. International Urogynecology Journal, 25(12), 1699–1706. doi:10.1007/s00192-014-2445-3
- Sripad, P., & Warren, C. (2016). Formative research on factors influencing access to fistula care and reatment in Uganda. (Research report). Retrieved from the Population Council website: https://www.popcouncil.org/uploads/pdfs/2016RH_FistulaCare_Uganda.pdf
- Tunçalp, Ö., Isah, A., Landry, E., & Stanton, C. K. (2014). Community-based screening for obstetric fistula in Nigeria: A novel approach. BMC Pregnancy and Childbirth, 14(1), 44. doi:10.1186/1471-2393-14-44
- Tunçalp, Ö., Tripathi, V., Landry, E., Stanton, C. K., & Ahmed, S. (2015). Measuring the incidence and prevalence of obstetric fistula: Approaches, needs and recommendations. Bulletin of the World Health Organization, 93(1), 60–62. doi:10.2471/BLT.14.141473
- Warren, C. E., Sripad, P., Mwangi, A., Ndwiga, C., Liambila, W., & Bellows, B. (2018). “Sickness of Shame”: Investigating challenges and resilience among women living with obstetric fistula in Kenya. In S. Choudhury, J. T. Erausquin, & M. Withers (Eds.), Global perspectives on women’s sexual and reproductive health across the lifecourse (pp. 91–109). Cham: Springer.
- Warren, C., Agbonkhese, R., & Ishaku, S. (2016). Formative research on assessing barriers to fistula care and treatment in Nigeria (Research report). Retrieved from the Population Council website: https://www.popcouncil.org/uploads/pdfs/2016RH_FistulaCare_Nigeria.pdf