Abstract
The quality of life (QoL) of women living with metastatic breast cancer and receiving palliative care needs more attention. We reviewed published studies (1992–2019) examining QoL of women receiving palliative care. The findings were interpreted according to the World Health Organization’s (WHO) definition of palliative care. Four themes emerged: (1) the impact of medical treatment on pain relief; (2) the need for psychosocial attention and support; (3) the necessity of an interdisciplinary approach; (4) ambiguous understanding of the term palliative care. A common understanding of the term palliative care and more research is needed to enhance the QoL of women living with metastatic breast cancer.
Background
Metastatic breast cancer (MBC), also referred to as advanced, secondary, or stage IV breast cancer, is an incurable disease, with median overall survival of 2 years. However, survival can range from a few months to many years (Cardoso et al., Citation2018; Chia et al., Citation2020). In most high-income countries, approximately 70% of patients with breast cancer are diagnosed in stages I and II, whereas only 20% to 50% of patients in most low- and middle-income countries are diagnosed in these earlier stages. The 5-year survival rate for breast cancer is much poorer in low-income countries than in high-income countries (Unger-Saldaña, Citation2014). This indicates a need for continuous follow-up and care (Cardoso et al., Citation2018; World Health Organization, Citation2019; Zujewski et al., Citation2018).
Being diagnosed with MBC is a difficult process and needs patient-centered care (Drageset et al., Citation2020; Lee Mortensen et al., Citation2018). In addition to the burden of many possible physical symptoms, women with MBC also face a huge psychological burden with a wide range of psychosocial and spiritual concerns (Drageset et al., Citation2018; Grotmol et al., 2017; Kokkonen et al., Citation2017; Mosher et al., Citation2013; Zhai et al., Citation2019). Improvements in diagnostic techniques and treatment methods, such as hormone-chemotherapy and radiation therapy, can extend the life of these women. However, this may also increase the symptom burden and have an impact on quality of life (QoL) (Cardoso et al., Citation2018; Cherny et al., Citation2018; Tometich et al., Citation2018; Verkissen et al., Citation2019).
QoL is defined as individuals’ perception of their position in life in the context of the culture and value systems in which they live in relation to their goals, expectations, standards and concerns (World Health Organization, Citation2019). It is a broad-ranging concept affected in a complex way by the person's physical health, psychological state, level of independence, social relationships, personal beliefs, and their relationship to salient features of their environment.
Palliative care (PC) is an approach that improves the QoL of patients and their families facing the problems associated with a life-threatening illness, through the prevention and relief of suffering by means of early identification and thorough assessment and treatment of pain and other problems (physical, psychosocial, and spiritual) (World Health Organization, Citation2019). The importance of an interdisciplinary approach is emphasized (Speed, Citation2017; World Health Organization, Citation2019). This definition reflects the core aspects of the modern hospice philosophy founded by Saunders (Citation1978), which emphasizes that pain, in particular, is complex when living with severe illness. Saunders introduced the concept of “total pain,” consisting of physical, mental, social, and spiritual aspects, which are interwoven and cannot be viewed separately. She therefore emphasized an interdisciplinary approach and awareness that includes concern for the family. The philosophy’s main goal is to facilitate patients to live as well as possible until death.
Thus, PC aims to improve the QoL of patients with MBC and their families by relieving symptoms, keeping the disease under control, and achieving a balance between progression of the disease and the discomfort caused by the medical treatment (World Health Organization, Citation2019). Alleviating the painful symptoms and emotional burden that accompany disease progression can allow patients to continue live a good life despite serious illness (Lee Mortensen et al., Citation2018; Sikorskii et al., Citation2020).
Ferrell et al. (2017) and Kokkonen et al. (Citation2019) recommend that PC should start early in the course of disease, also while patients are receiving curative treatment. Thus, this implies patient-centered communication (Back, Citation2020; Farrell & Coleby, Citation2016; Khoshnazar et al., Citation2016) regardless of where the patient is in the course of a disease trajectory, although this approach is particularly important at the end of life (Coyle, Citation2015; Saga et al., Citation2018).
According to Willis et al. (Citation2015) more research is needed to respond appropriately to women’s diverse care needs, particularly those who have lived with MBC for a longer period of time and are receiving different kinds of active or palliative treatment. To our knowledge, no systematic review has been published on this topic. Thus, the aim of this review was to explore the QoL of women living with MBC and receiving PC.
Methods
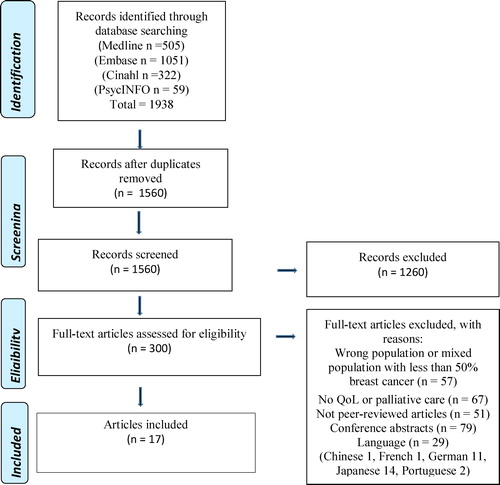
To thoroughly investigate our research aim, we chose to conduct a systematic review according to the PRISMA guidelines and using the PICO framework (Liberati et al., Citation2009). Our review protocol has been registered in PROSPERO (Drageset et al., Citation2016) and outlines the review process. The key criteria for inclusion were adult women with advanced breast cancer receiving PC presented as an approach or as a treatment and measurement or description of QoL. There are many studies with mixed cancer populations. We have chosen to include studies if at least 50% of the population were women with MBC. Studies with no mention of PC, no mention of QoL, or if less than 50% of the study participants were women with MBC, or the paper was not peer-reviewed were excluded.
Search strategy
We identified studies by searching major electronic bibliographic databases in the health sciences. Our search was conducted in Medline (OvidSP 1946–present), Embase (OvidSP 1974–present), PsycNFO (OvidSP 1806–present), and Cinahl (Ebscohost 1981–present); all databases were searched for their maximum time span. The final search was performed on December 17, 2019. Our search strategy had three PICO elements: population, intervention, and outcome. First, we searched for the population of patients with advanced breast cancer using the search terms “breast neoplasms” from the thesaurus, and a title/abstract search including “breast” or “mammary” and “cancer” or “neoplasms” or “tumors” or “adenocarcinomas” or “carcinomas.” Then we searched for intervention of PC using the following search terms: “hospice care,” “terminal care,” “palliative care,” and “end of life care.” Lastly, we searched for the outcome “quality of life” as a subject heading and in the title and abstract, using both the full term and the common abbreviations of the expression. The full search strategy is available online on request.
Our search strategy aimed to capture as much of the relevant literature as possible and was therefore performed without limitations on time or language. Our review protocol has been registered in PROSPERO(Drageset, Austrheim, Ellingsen, Citation2016). Nonetheless, we may have missed some studies. Although we found studies in several languages, there were no resources to have these studies translated, and thus 29 articles were excluded during the screening of full text ().
To be able to provide a multifaceted result, both qualitative and quantitative research articles were included, but all the studies finally selected used a quantitative approach. One of these studies also included qualitative data. After eliminating duplicates and irrelevant articles, the search identified 1560 articles. All citations (title and abstracts) were screened independently by the first and last authors using the established eligibility criteria; 1260 articles were excluded by title and abstract. The first and last authors independently assessed the studies for inclusion, and disagreements were resolved by discussion. After screening the titles and abstracts, 300 articles were retrieved to read the full text. Reasons for exclusion after reading the full text were wrong population, mixed population in which women with MBC were less than 50%, no assessment of QoL, no PC, not peer-reviewed articles, conference abstracts, or language. Finally, 17 articles were included ().
Critical appraisal
All the studies were critically appraised by the first and third authors independently and thereafter together, using The Joanna Briggs Institute Critical Appraisal tools (Citation2017), consisting of various checklists for different designs. The checklists contain 9 to 13 criteria. A combination of different checklists was sometimes used when the type of design was unclear. None of the appraised studies were of such low quality that they needed to be excluded.
Overview of selected studies
All studies () reported sample size and inclusion criteria, described the context in which data were collected, and described the type of analysis used.
Table 1. List of studies included.
In the intervention studies (Geels et al., Citation2000; Grabenbauer et al., Citation2016; Karamouzis et al., Citation2007), all the groups were similar at baseline. None of these studies used blinding or concealing.
Eight studies reported small sample size as a limitation (Aboshaiqah et al., Citation2016; Alfano et al., Citation2014; Ben-Arye et al., Citation2014; Karamouzis et al., Citation2007; Lee et al., Citation2017; Puetzler et al., Citation2014; Rugno et al., Citation2014; Slovacek et al., Citation2009). The dropout rate was described in the prevalence and prospective studies (Alfano et al., Citation2014; Ben-Arye et al., Citation2014; Nakamura et al., Citation2018; Reed et al., Citation2012; Rugno et al., Citation2014), and in the intervention studies(Grabenbauer et al., Citation2016; Lee et al., Citation2017). Reasons for a low response rate were reported only in one study (Reed et al., Citation2012). All studies used a questionnaire, but only one study (Nakamura et al., Citation2018) reported lack of validated scales as a limitation.
In the qualitative part of the study of Ben-Arye et al. (Citation2014), congruity between the stated philosophical perspective and the research perspective was not described. The researchers’ cultural and theoretical background and the influence of the researcher on the research and vice versa were not described. However, the overall methodological quality of this study was good because there was congruity between the research questions and method of collecting, analyzing, and interpreting the data.
Data analysis
Thematic analysis was used in our review (Dixon-Woods et al., Citation2005). The process of thematic analysis in the current review involved four steps. First, the authors read the studies separately several times to become fully immersed in the data. In this step, the findings that described the research questions were noted. Second, the findings were organized into descriptive themes by the first and last authors. Third, the main themes were interpreted and described to arrive at a new interpretation that went beyond the original studies. The process of analysis involved continuous discussion and reflection between the first and last authors. At the fourth step, the findings were interpreted primarily in light of the WHO’s definition of PC (World Health Organization, Citation2019).
Findings
A total of 1921 patients were included in this review. In five studies, the participants had various diagnoses, but patients with MBC accounted for more than half of the sample (Aboshaiqah et al., Citation2016; Ben-Arye et al., Citation2014; Grabenbauer et al., Citation2016; Lam et al., Citation2013; Rugno et al., Citation2014). The studies selected for inclusion were from three continents and 23 countries. Ten studies were from Europe, three from America, and four from Asia. One study recruited respondents from several countries (Lam et al., Citation2013). Details of the studies are presented in .
Findings emerging from the studies
Four main findings emerged from the 17 studies that elucidated our aim: (1) the impact of medical treatment on pain relief; (2) the need for psychosocial attention and support; (3) the necessity of an interdisciplinary approach; and (4) ambiguous understanding of the term palliative care.
The impact of medical treatment on pain relief
Treatment of symptoms of physical ailments had a significant impact on QoL (Campora et al., Citation1992; Geels et al., Citation2000; Karamouzis et al., Citation2007; Lam et al., Citation2013; Nakamura et al., Citation2018; Puetzler et al., Citation2014; Veronesi et al., Citation2007). Puetzler et al. (Citation2014) found that pharmacologic pain management among breast cancer outpatients under palliative chemotherapy significantly alleviated pain and improved health-related QoL in several subscales: global QoL, emotional functioning, physical functioning, future perspective, and sleeplessness.
In the study of Karamouzis et al. (Citation2007), QoL was found to be better among patients receiving chemotherapy than those under only supportive care. The outcomes included physical, emotional, social, and cognitive function; and fatigue, pain, loss of appetite loss, and sexual function. This difference was also evident according to body image, breast/arm symptoms, and systemic therapy side effects. Geels et al. (Citation2000) found a significant association between symptom improvement, such as pain, shortness of breath, mood, tumor regression and QoL with the use of chemotherapy. In contrast, Campora et al. (Citation1992) found that QoL was not improved 3 to 8 months after termination of chemotherapy. Also, the impact of the effect of radiotherapy treatment was highlighted. Better global health status, physical, emotional, and social functioning, and less fatigue, pain, loss of appetite, and constipation in patients with bone metastasis undergoing palliative radiotherapy was emphasized by Lam et al. (Citation2013). Nakamura et al. (Citation2018) reported that bleeding and offensive odor were significantly improved. Surgery also seemed to reveal good symptom palliation (Veronesi et al., Citation2007). However, even if medical treatment of physical symptoms was essential, this could not be viewed separately from the psychological consequences of this condition on QoL.
The need for psychosocial attention and support
Focusing on psychosocial issues and support was emphasized in eight studies (Aboshaiqah et al., Citation2016; Ben-Arye et al., Citation2014; Campora et al., Citation1992; Lee et al., Citation2017; Nuraini et al., Citation2018; Ozanne et al., Citation2009; Reed et al., Citation2012; Slovacek et al., Citation2009). Slovacek et al. (Citation2009) reported a low level of health-related QoL due to depression that affected the psychosocial and emotional aspects of QoL. It was recommended that recognition and management of these symptoms was important. Various programs to alleviate psychosocial concerns were presented. Lee et al. (Citation2017) found that a mindfulness-based stress reduction (MBSR) program alleviated distress and improved enjoyment of life. The patients were satisfied and expressed that MBSR helped them reach a peaceful state and to perceive emotional support from their peer group. They therefore wanted to continue participation in a psychological supportive program. Furthermore, Nuraini et al. (Citation2018) revealed that PC focusing on spirituality improved emotional well-being and comfort in addition to reducing anxiety and depression. Ben-Arye et al. (Citation2014) found that treatment with complementary/integrative medicine (CIM) reduced pre-chemotherapy anxiety. Outcomes revealed feelings of well-being, less fatigue, less depression, and less emotional distress. CIM treatments helped patients to cope with the side effects of chemotherapy, exemplified by quotes from the only study with qualitative data:
When I came to the integrative medicine department, I felt very weak, mentally. After an hour-long treatment session with acupuncture, I felt stronger and safer.
The approach here is aimed at treating the person, not just some patient who is scheduled for chemotherapy.
This was made clear by Aboshaiqah et al. (Citation2016) who reported that an increase in emotional support led to increased general satisfaction. However, Reed et al. (Citation2012) found that QoL, including physical, social, emotional, and functional domains, was low. Women reported reduced social, emotional, and functional well-being and felt that their main source of psychological support was from family and friends, whereas some felt unable to burden those close to them. In addition lack of professional support was also evident when receiving confusing, misleading, or no information about their MCB from their health care professional. Younger women were particularly dissatisfied with the information, advice, care, and support they received. The researchers claimed that the quality of interactions with health care providers influenced how well women coped with their cancer. Those who received professional support felt that it were beneficial, but many did not know how to seek the professional support they needed (Reed et al., Citation2012).
Furthermore, Ozanne et al. (Citation2009) reported that most women had gathered information about MBC and/or had written advance directives themselves. However, this information was seldom shared with health providers (doctors, nurses, and/or social workers). Patients were also more than three times more likely to talk to and share written plans with family and friends (Ozanne et al., Citation2009). Furthermore, Campora et al. (Citation1992) found that family support was good in most cases, but that some patients with severe anxiety needed further pharmacologic and/or psychological interventions. In contrast to Reed et al. (Citation2012), Campora et al. (Citation1992) found that information regarding disease and treatment given by health professionals was considered satisfactory by most of the patients.
The necessity of an interdisciplinary approach
The impact of an interdisciplinary approach was emphasized in several studies (Aboshaiqah et al., Citation2016; Alfano et al., Citation2014; Grabenbauer et al., Citation2016; Reed et al., Citation2012; Rugno et al., Citation2014; Veronesi et al., Citation2007). Aboshaiqah et al. (Citation2016) emphasized that PC should provide adequate psychosocial support and that interdisciplinary and collaborative approaches should be integrated in PC of cancer patients. Furthermore, when patients were followed up concurrently by PC and clinical oncology teams, they reported better QoL and less depression, received less chemotherapy, and achieved longer survival overall than those followed up under a traditional care model (Rugno et al., Citation2014). However, Reed et al. (Citation2012) also found that women’s interactions with health care professionals were typically limited to the specialist oncologist within the hospital setting, with little involvement of their general practitioner and PC services (Reed et al., Citation2012). The women reported a high symptom burden and dissatisfaction with elements of their care, indicating that alternative models of service delivery should be explored. Veronesi et al. (Citation2007) concluded that good symptom palliation should be considered more often by an interdisciplinary care provider. Supervised exercise programs and complementary and alternative medicine (CAM) were used to treat symptoms. Grabenbauer et al. (Citation2016) found that a supervised exercise program during and after radiation and chemotherapy not only improved oxygen consumption and body composition, but also QoL and fatigue. Alfano et al. (Citation2014) reported that CAM was frequently used to treat breast cancer and/or its symptoms. Art therapy, psychotherapy, and prayer were identified as activities that had the potential to improve QoL.
Ambiguous understanding of the term palliative care
The term palliative was understood as a stage of illness (Ozanne et al., Citation2009; Reed et al., Citation2012). Reed et al. (Citation2012) pointed out that patients were not referred to PC early in the disease trajectory; patients themselves were reluctant to access PC services because they associated this with end-of-life care. Ozanne et al. (Citation2009) found that discussion of advance directives and patient’s preferences were often lacking, because they were equated with end-of-life care. The term was also understood as a purpose of treatment (Grabenbauer et al., Citation2016; Lam et al., Citation2013; Puetzler et al., Citation2014). Furthermore, a variety of complementary therapies or approaches, such as supportive care and biologically based therapies, were used to alleviate suffering and improve QoL. These were not labeled as PC (Alfano et al., Citation2014; Ben-Arye et al., Citation2014; Grabenbauer et al., Citation2016; Karamouzis et al., Citation2007; Lee et al., Citation2017; Nuraini et al., Citation2018).
Discussion
This review shows that women with MBC need PC, but this was only partly offered. Typically, only life-prolonging treatment and relief from physical symptoms were offered. However, a holistic approach also includes an interdisciplinary focus on psychological, social, and spiritual aspects of their suffering. According to World Health Organization (Citation2019), PC reflects a “whole-person” philosophy of care implemented across the life span and across diverse health care settings, where the goal is to improve the QoL. A current trend is that PC is appropriate at any age and at any stage of serious illness and can be provided together with curative treatment (Coyle, Citation2015; World Health Organization, Citation2019). This is in line with Kokkonen et al. (Citation2019) and Ferrell et al. (Citation2017) who emphasized the need to integrate PC early in the disease course to improve QoL. However, this is challenging when this approach is associated with end-of-life care (Ozanne et al., Citation2009; Reed et al., Citation2012).
Karamouzis et al. (Citation2007) found that QoL was better among patients receiving chemotherapy than those under only supportive care. However, the point of PC is not either/or, but to integrate both physical and psychosocial/spiritual aspects. The term “total pain” as described by Saunders (Citation1978) shows the complexity of the patients’ suffering when living with severe, life-threatening illness.
To relieve suffering when living with MBC, medical treatment and various forms of medical pain relief in addition to supportive care are essential. This review revealed that adequate symptom treatment such as pharmacologic pain management, chemotherapy, and radiation or surgery had a significant impact on overall QoL. These findings correlate with several other studies (Dano et al., Citation2019; Kai et al., Citation2019; Kumar et al., Citation2019) in which surgery, radiation, and chemotherapy were reported to have a positive influence on QoL. However, the suffering or pain these patients experience is complex (Campora et al., Citation1992). Saunders (Citation1978) emphasized that health care providers should systematically assess the patient's symptoms and address the patient’s concerns through the illness trajectory. Furthermore, listening to patients' own descriptions of their symptom burden may ensure that treatment is consistent with their values and goals (Tometich et al., Citation2018; World Health Organization, Citation2019).
Moreover, the findings also revealed that the women needed psychosocial attention and support from family and friends, as well as from health care professionals. These challenges can be alleviated by support from health care professionals and family (Cardoso et al., Citation2018; Kristanti et al., Citation2017; Lee Mortensen et al., Citation2018; Zujewski et al., Citation2018). Reed et al. (Citation2012) found that the main source of psychological support was from family and friends, although some women felt unable to burden those close to them. In addition, many did not know how to seek the professional support they needed. This was also pointed out by Drageset et al. (Citation2018, Citation2020) who emphasized that the way women with breast cancer were seen and met had an impact. Saunders (Citation1978) emphasized that the patients and the family should be a “unit of care.” The patients’ condition and suffering has an impact on the people close to them, which means that the patients’ suffering is also the families’ suffering (Baudry et al., Citation2019; Fjose et al., Citation2016; Krug et al., Citation2016). Therefore, the PC approach includes concerns and involvement of the family and vice versa (Cardoso et al., Citation2018; Wang, Molassiotis, & Tan, 2018; World Health Organization, Citation2019).
The need to integrate the psychological and spiritual aspects of patient care is emphasized by World Health Organization (Citation2019). Our review revealed that different forms of life-giving treatments such as MBSR programs, CIM, and exercise programs helped to alleviate distress. This was also emphasized by Cardoso et al. (Citation2018) and (Sasaki et al., Citation2019) who found that found CAM could be helpful for treating specific symptoms.
As emphasized by Back (Citation2020) and Khoshnazar et al. (Citation2016), we found that good communication, especially person-centered information, affects the quality of life of women with MBC. Patients wanted adequate information from health care professionals. In general, cancer treatment involves a great deal of information about the treatment and adverse effects (Wang et al., Citation2018; Zøylner et al., Citation2019; Zujewski et al., Citation2018). When patients receive early PC, both patients and family members become better informed about disease symptoms, severity, and treatment directives. They are also given more time for life decisions, promoting the experience of higher self-efficacy and individual value decisions (McClain et al., Citation2003). However, Reed et al. (Citation2012) found that the needs of some patients were not met, especially related to information, advice, care, and support. This raises the question of how health care professionals provide information and support when the illness trajectory is increasingly unpredictable. To support patient-centered care means starting the information based on the patient's own understanding of their situation (Drageset et al., Citation2020). A good interpersonal relationship between patient and doctor is important for the patient’s acceptance of illness and participation in deciding the treatment options (Back, Citation2020; Fong Ha & Longnecker, Citation2010). However, Ozanne et al. (Citation2009) found that even when patients had gathered information about advance directives and made written plans, few discussed this plan with their providers.
Different understanding and use of the term PC was also found. A major challenge is that PC is associated with a late disease stage or end-of-life care, which is why health providers, patients, and families want to avoid this approach as long as possible (Adler et al., Citation2019; Beernaert et al., Citation2015). To support these women and their families, it is essential to change the focus from “living longer” to include “living better”, which also includes concerns for the family. PC should be integrated early in the course of the disease (Saunders, Citation1978; World Health Organization, Citation2019).
Strengths and limitations
This review focused on QoL among women with MBC receiving PC. Despite a broad literature search and comprehensive search strategy, intended to include both qualitative and quantitative studies to provide a more multifaceted result, only 17 quantitative studies were included. Only one of these (Ben-Arye et al., Citation2014) also included qualitative data. Even though we attempted to include evidence of QoL among patients living with MBC receiving PC worldwide, 8 of the 17 studies were from Europe. Probably some studies were not included because of limited resources to get foreign language studies translated. A more culturally diverse study population could have strengthened the findings. Furthermore, the exclusion of studies with less than 50% of women with MBC in the population meant that several studies were not included. In addition, because PC is a diagnosis-independent approach, the diagnosis is not always reported, which means that many studies including women with MBC were probably lost. However, a major limitation is that it is difficult to measure the effects of PC when the term palliative care is attributed to various meanings.
We found The Joanna Briggs Institute Critical Appraisal tools (Citation2017) appropriate to assess the methodological quality of the studies in this review. There was variation in the overall methodological quality of the studies, and the most prominent was a small sample size. Because of the limited number of studies and the variations in sample size, the results should be interpreted with caution. Nevertheless, the findings in the current review highlight that women with MBC need PC to attain the best possible QoL for themselves and their families, but further research is needed.
Conclusion
PC is not a stage of illness and is more than treatment. A PC approach is fundamentally important to alleviate pain and distress among patient with MBC. PC that includes person-centered information should be integrated as part of standard care and not limited to the end-of-life phase. There is a need for common understanding of the concept of PC.
Longitudinal data exploring QoL through the disease trajectory are needed to get a more detailed picture of the challenges of living with MCB. In addition, intervention studies to investigate the effect of early integration of a palliative approach among patients with breast cancer and their relatives are needed.
Relevance to clinical practice
Efforts to gain a common understanding of the term of palliative care are important. Tailored PC is helpful and should be offered to women with MBC at all stages of the disease. The importance of early integration of palliative care should be promoted.
Disclosure statement
No conflict of interest has been declared by the authors.
References
- Aboshaiqah, A., Al-Saedi, T. S., Abu-Al-Ruyhaylah, M. M., Aloufi, A. A., Alharbi, M. O., Alharbi, S. S., … Al-Erwi, A. F. (2016). Quality of life and satisfaction with care among palliative cancer patients in Saudi Arabia. Palliative & Supportive Care, 14, 1–7. https://doi.org/https://doi.org/10.1017/S1478951516000432
- Adler, S. R., Coulter, Y. Z., Stone, K., Glaser, J., Duerr, M., & Enochty, S. (2019). End-of-life concerns and experiences of living with advanced breast cancer among medically underserved women. Journal of Pain and Symptom Management, 58(6), 959–967. https://doi.org/https://doi.org/10.1016/j.jpainsymman.2019.08.006
- Alfano, A. C., Paiva, C. E., Rugno, F. C., da Silva, R. H., & Paiva, B. S. (2014). Biologically based therapies are commonly self-prescribed by Brazilian women for the treatment of advanced breast cancer or its symptoms. Supportive Care in Cancer : official Journal of the Multinational Association of Supportive Care in Cancer, 22(5), 1303–1311. https://doi.org/https://doi.org/10.1007/s00520-013-2087-x
- Back, A. L. (2020). Patient-clinician communication issues in palliative care for patients with advanced cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 38(9), 866–876. https://doi.org/https://doi.org/10.1200/jco.19.00128
- Baudry, A.-S., Vanlemmens, L., Anota, A., Cortot, A., Piessen, G., & Christophe, V. (2019). Profiles of caregivers most at risk of having unmet supportive care needs: Recommendations for healthcare professionals in oncology. European Journal of Oncology Nursing: The Official Journal of European Oncology Nursing Society, 43, 101669. https://doi.org/https://doi.org/10.1016/j.ejon.2019.09.010
- Beernaert, K., Deliens, L., Pardon, K., Van den Block, L., Devroey, D., Chambaere, K., & Cohen, J. (2015). What are physicians' reasons for not referring people with life-limiting illnesses to specialist palliative care services? A nationwide survey. PloS One, 10(9), e0137251. https://doi.org/https://doi.org/10.1371/journal.pone.0137251
- Ben-Arye, E., Israely, P., Baruch, E., & Dagash, J. (2014). Integrating family medicine and complementary medicine in cancer care: A cross-cultural perspective. Patient Educ Couns, 97(1), 135–139. https://doi.org/https://doi.org/10.1016/j.pec.2014.06.006
- Campora, E., Naso, C., Vitullo, M. T., Giudici, S., Camoirano, A., Repetto, L., & Rosso, R. (1992). The impact of chemotherapy on the quality of life of breast cancer patients. Journal of Chemotherapy (Florence, Italy)), 4(1), 59–63. https://doi.org/https://doi.org/10.1080/1120009x.1992.11739141
- Cardoso, F., Senkus, E., Costa, A., Papadopoulos, E., Aapro, M., André, F., Harbeck, N., Aguilar Lopez, B., Barrios, C. H., Bergh, J., Biganzoli, L., Boers-Doets, C. B., Cardoso, M. J., Carey, L. A., Cortés, J., Curigliano, G., Diéras, V., El Saghir, N. S., Eniu, A., … Winer, E. P. (2018). 4th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 4)†. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 29(8), 1634–1657. https://doi.org/https://doi.org/10.1093/annonc/mdy192
- Cherny, N. I., Paluch-Shimon, S., & Berner-Wygoda, Y. (2018). Palliative care: Needs of advanced breast cancer patients. Breast Cancer (Dove Medical Press)), 10, 231–243. https://doi.org/https://doi.org/10.2147/BCTT.S160462
- Chia, S., Burstein, H., & Vora, R. S. (2020). Prognostic and predictive factors in metastatic breast cancer. In UpToDate. Stephen Chia.
- Coyle, N. (2015). Introduction to palliative nursing care. In B. R. Ferrell, N. Coyle, & J. A. Paice (Eds.), Oxford textbook of palliative nursing (pp. 4–5). Oxford University Press.
- Dano, D., Hénon, C., Sarr, O., Ka, K., Ba, M., Badiane, A., Thiam, I., Diene, P., Diop, M., Dem, A., Marino, P., Mancini, J., Annede, P., Gonçalves, A., Diouf, D., & Monneur, A. (2019). Quality of life during chemotherapy for breast cancer in a West African Population in Dakar, Senegal: A prospective study. Journal of Global Oncology, (5), 1–9. https://doi.org/https://doi.org/10.1200/JGO.19.00106
- Dixon-Woods, M., Agarwal, S., Jones, D., Young, B., & Sutton, A. (2005). Synthesising qualitative and quantitative evidence: A review of possible methods. Journal of Health Services Research & Policy, 10(1), 45–53. https://doi.org/https://doi.org/10.1177/135581960501000110
- Drageset, S., Austrheim, G., & Ellingsen, S. (2016). Quality of life of women living with metastatic breast cancer and receiving palliative care: A systematic review. Prospero: A Journal of New Thinking in Philosophy for Education. ISSN 13458-6785.
- Drageset, S., Lindstrom, T. C., & Ellingsen, S. (2018). “I Have Both Lost and Gained.” Norwegian survivors' experiences of coping 9 years after primary breast cancer surgery. Cancer Nursing, 43(1), E30–E37. https://doi.org/https://doi.org/10.1097/NCC.0000000000000656
- Drageset, S., Lindstrom, T. C., & Ellingsen, S. (2020). “Cancer changed my life.” Women's experiences 1 and 9 years after primary breast cancer surgery. Nordisk Sygeplejeforskning, 10(01), 20–33. https://doi.org/https://doi.org/10.18261/issn.1892-2686-2020-01-03
- Farrell, C., & Coleby, T. (2016). An integrated model for breast cancer and palliative care. Cancer Nursing Practice, 15(7), 28–31. https://doi.org/https://doi.org/10.7748/cnp.2016.e1346
- Ferrell, B. R., Temel, J. S., Temin, S., Alesi, E. R., Balboni, T. A., Basch, E. M., Firn, J. I., Paice, J. A., Peppercorn, J. M., Phillips, T., Stovall, E. L., Zimmermann, C., & Smith, T. J. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology : official Journal of the American Society of Clinical Oncology, 35(1), 96–112. https://doi.org/https://doi.org/10.1200/JCO.2016.70.1474
- Fjose, M., Eilertsen, G., Kirkevold, M., & Grov, E. K. (2016). A valuable but demanding time family life during advanced cancer in an elderly family member. ANS. Advances in Nursing Science, 39(4), 358–373. https://doi.org/https://doi.org/10.1097/ANS.0000000000000145
- Fong Ha, J., & Longnecker, N. (2010). Doctor-patient communication: A review. The Ochsner Journal, 10, 38–43.
- Geels, P., Eisenhauer, E., Bezjak, A., Zee, B., & Day, A. (2000). Palliative effect of chemotherapy: Objective tumor response is associated with symptom improvement in patients with metastatic breast cancer. Journal of Clinical Oncology : official Journal of the American Society of Clinical Oncology, 18(12), 2395–2405. https://doi.org/https://doi.org/10.1200/JCO.2000.18.12.2395
- Grabenbauer, A., Grabenbauer, A. J., Lengenfelder, R., Grabenbauer, G. G., & Distel, L. V. (2016). Feasibility of a 12-month-exercise intervention during and after radiation and chemotherapy in cancer patients: Impact on quality of life, peak oxygen consumption, and body composition. Radiation Oncology (London, England)), 11 (1), 42. https://doi.org/https://doi.org/10.1186/s13014-016-0619-5
- Grotmol, K. S., Lie, H. C., Hjermstad, M. J., Aass, N., Currow, D., Kaasa, S., Moum, T. Å., Pigni, A., Loge, J. H., … European Palliative Care Research Collaborative. (2017). Depression–a major contributor to poor quality of life in patients with advanced cancer. Journal of Pain and Symptom Management, 54(6), 889–897. https://doi.org/https://doi.org/10.1016/j.jpainsymman.2017.04.010
- Kai, M., Kubo, M., Kawaji, H., Kurata, K., Mori, H., Yamada, M., & Nakamura, M. (2019). QOL-enhancing surgery for patients with HER2-positive metastatic breast cancer. BMJ Support Palliat Care, 9(2), 151–154. https://doi.org/https://doi.org/10.1136/bmjspcare-2018-001622
- Karamouzis, M. V., Ioannidis, G., & Rigatos, G. (2007). Quality of life in metastatic breast cancer patients under chemotherapy or supportive care: A single-institution comparative study. European Journal of Cancer Care, 16(5), 433–438. https://doi.org/https://doi.org/10.1111/j.1365-2354.2006.00771.x
- Khoshnazar, T. A., Rassouli, M., Akbari, M. E., Lotfi-Kashani, F., Momenzadeh, S., Rejeh, N., & Mohseny, M. (2016). Communication needs of patients with breast cancer: A qualitative study. Indian Journal of Palliative Care, 22(4), 402–409. https://doi.org/https://doi.org/10.4103/0973-1075.191763
- Kokkonen, K., Saarto, T., Makinen, T., Pohjola, L., Kautio, H., Jarvenpaa, S., & Puustjarvi-Sunabacka, K. (2017). The functional capacity and quality of life of women with advanced breast cancer. Breast Cancer, 24(1), 128–136. https://doi.org/https://doi.org/10.1007/s12282-016-0687-2
- Kokkonen, K., Tasmuth, T., Lehto, J. T., Kautiainen, H., Elme, A., Jaaskelainen, A. S., & Saarto, T. (2019). Cancer patients' symptom burden and health-related quality of life (HRQoL) at Tertiary Cancer Center from 2006 to 2013: A cross-sectional study. Anticancer Research, 39(1), 271–277. https://doi.org/https://doi.org/10.21873/anticanres.13107
- Kristanti, S. M., Setiyarini, S., & Effendy, C. (2017). Enhancing the quality of life for palliative cancer patients in Indonesia through family caregivers: A pilot study of basic skills training. BMC Palliativ Care, 16(4). https://doi.org/https://doi.org/10.1186/s12904-016-0178-4
- Krug, K., Miksch, A., Peters-Klimm, F., Engeser, P., & Szecsenyi, J. (2016). Correlation between patient quality of life in palliative care and burden of their family caregivers: A prospective observational cohort study. BMC Palliative Care, 15, 4 https://doi.org/https://doi.org/10.1186/s12904-016-0082-y
- Kumar, A., Mukundan, H., Bhatnagar, S., Sarin, A., Taneja, S., & Sahoo, S. (2019). Radiation for palliation: Role of palliative radiotherapy in allevieating pain/symptoms in a prospective observational study at two tertiary care centers. Indian Journal of Palliative Care, 25(3), 391–397. https://doi.org/https://doi.org/10.4103/IJPC.IJPC_35_19
- Lam, K., Chow, E., Zhang, L., Wong, E., Bedard, G., Fairchild, A., Vassiliou, V., El-Din, M. A., Jesus-Garcia, R., Kumar, A., Forges, F., Tseng, L.-M., Hou, M.-F., Chie, W.-C., & Bottomley, A. (2013). Determinants of quality of life in advanced cancer patients with bone metastases undergoing palliative radiation treatment. Supportive Care in Cancer, 21(11), 3021–3030. https://doi.org/https://doi.org/10.1007/s00520-013-1876-6
- Lee Mortensen, G., Madsen, I. B., Krogsgaard, R., & Ejlertsen, B. (2018). Quality of life and care needs in women with estrogen positive metastatic breast cancer: A qualitative study. Acta Oncologica (Stockholm, Sweden)), 57(1), 146–151. https://doi.org/https://doi.org/10.1080/0284186x.2017.1406141
- Lee, C. E., Kim, S., Kim, S., Joo, H. M., & Lee, S. (2017). Effects of a mindfulness-based stress reduction program on the physical and psychological status and quality of life in patients with metastatic breast cancer. Holist Nurs Pract, 31(4), 260–269. https://doi.org/https://doi.org/10.1097/HNP.0000000000000220
- Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. A., Clarke, M., Devereaux, P. J., Kleijnen, J., & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine, 6(7), e1000100. https://doi.org/https://doi.org/10.1371/journal.pmed.1000100
- McClain, C., Rosenfeld, B., & Breitbart, W. (2003). Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. The Lancet, 361(9369), 1603–1607. doi: VOLUME 361, ISSUE 9369, P1603-1607, https://doi.org/https://doi.org/10.1016/S0140-6736(03)13310-7
- Mosher, C. E., Johnson, C., Dickler, M., Norton, L., Massie, M. J., & DuHamel, K. (2013). Living with metastatic breast cancer: A qualitative analysis of physical, psychological, and social sequelae. The Breast Journal, 19(3), 285–292. https://doi.org/https://doi.org/10.1111/tbj.12107
- Nakamura, N., Kawamori, J., Takahashi, O., Shikama, N., Sekiguchi, K., Takahashi, T., Kato, S., Ogita, M., Motegi, A., & Akimoto, T. (2018). Palliative radiotherapy for breast cancer patients with skin invasion: A multi-institutional prospective observational study. Japanese Journal of Clinical Oncology, 48(6), 555–558. https://doi.org/https://doi.org/10.1093/jjco/hyy054
- Nuraini, T., Andrijono, A., Irawaty, D., Umar, J., & Gayatri, D. (2018). Spirituality-focused palliative care to improve Indonesian breast cancer patient comfort. Indian Journal of Palliative Care, 24(2), 196–201. https://doi.org/https://doi.org/10.4103/IJPC.IJPC_5_18
- Ozanne, E. M., Partridge, A., Moy, B., Ellis, K. J., & Sepucha, K. R. (2009). Doctor-patient communication about advance directives in metastatic breast cancer. Journal of Palliative Medicine, 12(6), 547–553. https://doi.org/https://doi.org/10.1089/jpm.2008.0254
- Puetzler, J., Feldmann, R. E., Jr., Brascher, A. K., Gerhardt, A., & Benrath, J. (2014). Improvements in health-related quality of life by comprehensive cancer pain therapy: A pilot study with breast cancer outpatients under palliative chemotherapy. Oncology Research and Treatment, 37(9), 456–462. https://doi.org/https://doi.org/10.1159/000365537
- Reed, E., Simmonds, P., Haviland, J., & Corner, J. (2012). Quality of life and experience of care in women with metastatic breast cancer: A cross-sectional survey. Journal of Pain and Symptom Management, 43(4), 747–758. https://doi.org/https://doi.org/10.1016/j.jpainsymman.2011.05.005
- Rugno, F. C., Paiva, B. S. R., & Paiva, C. E. (2014). Early integration of palliative care facilitates the discontinuation of anticancer treatment in women with advanced breast or gynecologic cancers. Gynecologic Oncology, 135(2), 249–254. https://doi.org/https://doi.org/10.1016/j.ygyno.2014.08.030
- Saga, Y., Enokido, M., Iwata, Y., & Ogawa, A. (2018). Transitions in palliative care: Conceptual diversification and the integration of palliative care into standard oncology care. Chinese Clinical Oncology, 7(3), 32 https://doi.org/https://doi.org/10.21037/cco.2018.06.02
- Sasaki, Y., Cheon, C., Motoo, Y., Jang, S., Park, S., Ko, S.-G., Jang, B.-H., & Hwang, D.-S. (2019). Complementary and alternative medicine for breast cancer patients: An overview of systematic reviews. Yakugaku Zasshi : Journal of the Pharmaceutical Society of Japan, 139(7), 1027–1046. https://doi.org/https://doi.org/10.1248/yakushi.18-00215
- Saunders, C. M. (1978). The philosophy of terminal care. (C. M. Saunders Ed.). Edward Arnold.
- Sikorskii, A., Niyogi, P. G., Victorson, D., Tamkus, D., & Wyatt, G. (2020). Symptom response analysis of a randomized controlled trial of reflexology for symptom management among women with advanced breast cancer. Support Care Cancer, 28(3), 1395–1404. https://doi.org/https://doi.org/10.1007/s00520-019-04959-y
- Slovacek, L., Slovackova, B., Slanska, I., Petera, J., Priester, P., Filip, S., & Kopecky, J. (2009). Depression symptoms and health-related quality of life among patients with metastatic breast cancer in programme of palliative cancer care. Neoplasma, 56(6), 467–472. https://doi.org/https://doi.org/10.4149/neo_2009_06_467
- Speed, L. (2017). Non-surgical management of musculoskeletal malignancy. Orthopaedics and Trauma, 31(3), 195–203. https://doi.org/https://doi.org/10.1016/j.mporth.2017.03.011
- The Joanna Briggs Institute Critical Appraisal tools. (2017). http://joannabriggs.org/research/critical-appraisal-tools.html
- Tometich, D. B., Mosher, C. E., Hirsh, A. T., Rand, K. L., Johns, S. A., Matthias, M. S., Outcalt, S. D., Schneider, B. P., Mina, L., Storniolo, A. M. V., Newton, E. V., & Miller, K. D. (2018). Metastatic breast cancer patients' expectations and priorities for symptom improvement. Supportive Care in Cancer : official Journal of the Multinational Association of Supportive Care in Cancer, 26(11), 3781–3788. https://doi.org/https://doi.org/10.1007/s00520-018-4244-8
- Unger-Saldaña, K. (2014). Challenges to the early diagnosis and treatment of breast cancer in developing countries. World Journal of Clinical Oncology, 5(3), 465–477. https://doi.org/https://doi.org/10.5306/wjco.v5.i3.465
- Verkissen, M. N., Hjermstad, M. J., Van Belle, S., Kaasa, S., Deliens, L., & Pardon, K. (2019). Quality of life and symptom intensity over time in people with cancer receiving palliative care: Results from the international European Palliative Care Cancer Symptom study. PloS One, 14(10), e0222988. https://doi.org/https://doi.org/10.1371/journal.pone.0222988
- Veronesi, G., Scanagatta, P., Goldhirsch, A., Rietjens, M., Colleoni, M., Pelosi, G., & Spaggiari, L. (2007). Results of chest wall resection for recurrent or locally advanced breast malignancies. The Breast, 16(3), 297–302. https://doi.org/https://doi.org/10.1016/j.breast.2006.12.008
- Wang, T., Molassiotis, A., Chung, B. P. M., & Tan, J. (2018). Unmet care needs of advanced cancer patients and their informal caregivers: A systematic review. BMC Palliat Care, 17(1), 96. https://doi.org/https://doi.org/10.1186/s12904-018-0346-9
- Willis, K., Lewis, S., Ng, F., & Wilson, L. (2015). The experience of living with metastatic breast cancer-a review of the literature. Health Care Women Int, 36(5), 514–542. https://doi.org/https://doi.org/10.1080/07399332.2014.896364
- World Health Organization. (2019). WHO definition of palliative care. http://www.who.int/cancer/palliative/definition/en/
- Zhai, J., Newton, J., & Copnell, B. (2019). Posttraumatic growth experiences and its contextual factors in women with breast cancer: An integrative review. Health Care for Women International, 40(5), 554–580. https://doi.org/https://doi.org/10.1080/07399332.2019.1578360
- Zøylner, I. A., Lomborg, K., Christiansen, P. M., & Kirkegaard, P. (2019). Surgical breast cancer patient pathway: Experiences of patients and relatives and their unmet needs. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy, 22(2), 262–272. https://doi.org/https://doi.org/10.1111/hex.12869
- Zujewski, J. A., Dvaladze, A. L., Ilbawi, A., Anderson, B. O., Luciani, S., Stevens, L., & Torode, J. (2018). Knowledge summaries for comprehensive breast cancer control. Journal of Global Oncology, (4), 1–7. https://doi.org/https://doi.org/10.1200/jgo.17.00141