Abstract
Using national register data between 2006–2014, we investigated the relationship between outpatient mental health service use (a proxy for mental disorder) and subsequent marital separation among women in Norway and whether the strength of the association differed for migrant and non-migrant women. Our sample population included 679,928 married women aged 18–60 years. Service use was strongly associated with marital separation among all women. The relationship was stronger for Filipinas but weaker for Somalis and Russians, compared with non-migrant women. Migration-related factors may influence marital separation among migrant women and barriers to care are likely to exist.
Mental disorders are more prevalent among the divorced than among the married (Gutiérrez-Rojas et al., Citation2020). Researchers suggest that divorce can lead to poorer mental health (Recksiedler & Stawski, Citation2019; Tavares & Aassve, Citation2013). However, there is also evidence that mental disorder (Breslau & Chang, Citation2006; Mojtabai et al., Citation2017), distress (Idstad et al., Citation2015) and health service use for mental health problems (Reneflot et al., Citation2020) may be present prior to marital separation. Thus, mental disorder may increase the likelihood of marital separation and simultaneously prevent one reaping the benefits of a stable marriage. Both the causes and ramifications of marital separation and divorce vary, not only for individuals, particularly women, and families concerned, but also according to different social, political and cultural contexts. It is therefore possible that mental health selection out of marriage varies across different groups of migrant women in a society. Shedding light on this currently unexplored topic can improve both our understanding of marital separation among migrant women and contribute to the theoretical literature on mental health selection out of marriage. Given that there are increasing proportions of migrants living in countries all across the world (IOM, Citation2019), examining how mental health is related to their marital and divorce patterns has international relevance.
Divorce rates vary around the world (Ortiz-Ospina & Roser, Citation2020) and also across different migrant groups within a society (Andersson et al., Citation2015; Qian, Citation2013). Migrants may be influenced by divorce laws, norms and attitudes in both the country of origin and the new country (Andersson et al., Citation2015; Furtado et al., Citation2013). In Norway, divorce is easily obtainable, and acceptable, for both women and men. As in the general population, divorced, separated or widowed refugees and migrants are more likely to report depression, anxiety and post-traumatic stress (Chou, Citation2007; Tinghög et al., Citation2017), to consult with a doctor for mental health problems (Straiton et al., Citation2017) and use psychotropic medicine (Hollander et al., Citation2011) than their married counterparts. However, it is not known whether this is due to preexisting problems or a result of the separation process. Further, we do not know if the relationship between mental disorder and subsequent marital separation is the same for migrant and non-migrant women. There are several reasons why it might be different.
The first relates to the disadvantaged position of migrant women in society. With some exceptions, migrant women from outside the European Union (EU), are more likely to have lower education, income and levels of employment than non-migrant women (Bufdir, Citation2020; Gorodzeisky & Semyonov, Citation2017; Vrålstad & Wiggen, Citation2017). They are thus, more likely to experience financial stress than their non-migrant counterparts. Migrant women may also experience a range of other postmigration stress factors such as discrimination, language difficulties and lack of social support (Delara, Citation2016). These factors increase the risk of both mental disorder and marital strain (Fernbrant et al., Citation2013). Since mental disorder can also increase marital strain, migrant women with mental disorder may experience a greater cumulation of strain than non-migrant women, resulting in a stronger relationship between mental disorder and marital separation for migrant than for non-migrant women.
Second, stigma surrounding mental health among migrant groups is well-documented (Henning-Smith et al., Citation2013; Mirza et al., Citation2019; Saechao et al., Citation2012; Straiton et al., Citation2018). Researchers from Australia noted that mental disorder was perceived as one of the few accepted grounds for divorce among Arab speaking migrant communities (Youssef & Deane, Citation2006). Family members may exert pressure on the couple to divorce if a spouse has a mental illness due fear of it reflecting badly upon the family in-law. Similar sentiments have been noted by researchers in South Asia (Sharma et al., Citation2013). Thus, the relationship between mental disorder and marital separation could be stronger for migrant women from collective societies, where marriage is often considered to be between two families rather than two individuals (Bejanyan et al., Citation2015).
Both of the arguments provided above suggest a stronger relationship between mental disorder and marital separation among migrant women. However, another argument points in the opposite direction. The divorce norms and attitudes migrants may take with them when they migrate often differ strongly from those of non-migrant women (Furtado et al., Citation2013). In cultures with patriarchal family structures, such as in South Asia, the Middle East and Turkey, divorced women are often heavily stigmatized and can risk being ostracized from their family and communities (Fernbrant et al., Citation2013; Jennings, Citation2016; Waseem et al., Citation2020). Similar findings are reported among some migrant communities in Europe (Akpinar, Citation2003; Das, Citation2012). Thus, the threshold for marital separation could be higher for groups of women where divorce is more stigmatized and less common, regardless of mental disorder. This could result in a weaker relationship between mental disorder and marital separation among migrant women compared with non-migrant women.
Married migrant women are a diverse group in terms of the type of marriage they enter and their reasons for migration. This may further complicate the picture. Due to restrictive migration policies for those outside of the EU, entering a transnational marriage may be a viable route to migration to Europe for some women (Aalandslid & Tronstad, Citation2010; Beck-Gernsheim, Citation2011). This can increase spousal dependency and disempowerment which can impact mental health (Flemmen & Lotherington, Citation2012; Straiton et al., Citation2018). Yet, when suffering from mental disorder, they may be particularly reliant on their spouse for social support as well as help in navigating the health services in order to seek treatment. The relationship between mental disorder and subsequent marital separation could therefore be weaker than for non-migrant women. Furthermore, migrant women origininating from countries that often enter exogamous marriages (marriages outside of their social group) may experience other challenges in their marriage such as cultural differences and other people’s suspicions about the legitimacy of such unions (Adserà & Ferrer, Citation2015; Flemmen & Lotherington, Citation2012). Indeed, exogamous marriages are more likely to end in divorce than endogamous marriages (marriages within their social group) (Adserà & Ferrer, Citation2015; Andersson et al., Citation2015; Sandnes & Østby, Citation2015). Thus, there may be many more important factors that increase the risk of marital separation for migrant women in exogamous marriages, regardless of mental disorder. This could mean that the relationship between mental disorder and marital separation is weaker for groups of migrant women who tend to enter exogamous marriages compared with groups of migrant women who tend to enter endogamous marriages.
Aims of the study
In this study, we aim to determine the association between mental disorder (measured by use of outpatient mental health services (OPMH)) and subsequent marital separation among non-EU migrant and non-migrant women living in Norway. Additionally, we explore whether the relationship differs by country of origin. We use longitudinal register data and control for marital history, age, dependent children, education and income, variables that are associated with marital separation and/or mental health (Bufdir, Citation2020; Gorodzeisky & Semyonov, Citation2017; Lyngstad & Jalovaara, Citation2010; Vrålstad & Wiggen, Citation2017). Our focus is on non-EU migrant women, since they may experience bigger shifts in cultural roles, values and expectations post-migration than EU migrant women. We select the six biggest groups of married migrant women from countries outside of the EU, living in Norway, during the study period (2006–2014) together with all non-migrant women. These groups include women from Thailand, The Philippines, Russia, Pakistan, Iraq and Somalia. The former three groups often enter exogamous marriages with non-migrant men, while the latter three most often enter endogamous marriages with a partner, or a descendent of someone, from the same country of origin (Aalandslid & Tronstad, Citation2010; Molstad, Citation2020). Notably, workforce participation rates for Russian, Thai and Filipino women are far higher than for the other three groups (Statistics Norway, Citation2020), which could also increase the feasibility of marital separation, yet at the same time, be protective of mental health. Thus, due to heterogeneity in the acceptability of divorce, the type of marriage entered and available resources across these six groups, it is of interest to investigate if the relationship between OPMH use and subsequent marital separation varies across these six migrant groups compared with non-migrant women. However, due to the competing reasons outlined above, it is unclear whether the relationship may be stronger or weaker for migrant women than for non-migrant women.
Method
Data sources
In this study, we use data from four Norwegian national registries, linked at an individual level through a non-identifiable version of a personal number. All Norwegian born individuals and registered residents with at least six months of residence are assigned this personal number. The Central Population Registry contains demographic information and the Education database contains education level. Information on child-benefit comes from FD-Trygd and annual income comes from the National Income registry. Finally, the National Database for the Reimbursement of Health Expenses (KUHR) contains information on patient contacts, including outpatient mental health care service contacts.
Ethical approval for this study was granted by the Regional Committee for Medical and Health Research Ethics, South East Norway (REK 2014/1970) and both registry owners approved the use of their data. Consent to participate was not required since this study uses already existing administrative data.
Study population
We used a dynamic study design, including all long-term resident women, aged 18–60 years who were living in Norway for at least two years and registered as married at some point between 2006 and 2013. Information on marital status was extracted for each year of the study. Women were followed until they experienced marital separation or were censored at the end of 2014, the year they turned 60, died, or emigrated or were widowed, whichever came first. Sixty years of age was the upper age limit since there were very few migrant women over 60 in our selected migrant groups. We excluded women who were widowed prior to baseline.
Variables
Outcome: Marital separation was defined as a change in registered status from married to separated. This is more accurate indicator of marital dissolution than divorce, since some couples can be separated for years before finalizing their divorce.
Exposure: Use of outpatient mental health care services was used as a proxy for mental disorder. We defined this as at least one contact with outpatient mental health care services. This exposure was time varying, recorded for each year of inclusion. However, once exposed, individuals were always coded as exposed.
Covariates
Marital history: Women who had no record of a previous marriage were coded being in their first marriage, while women with a previous marriage record were coded being in a remarriage.
Country of origin: Migrants were defined as women born abroad with two foreign-born parents and non-migrants as all others. We only selected migrants from the following countries: Thailand, The Philippines, Pakistan, Russia, Iraq and Somalia. These were the six biggest groups of migrant women from non-EU countries living in Norway during the study period.
Age group (time varying): Age was grouped into 4 categories: <30 (reference group), 30–39, 40–49, 50+ years.
Dependent children (time-varying): Receipt of child benefit, which is automatically paid to mothers whose children are under the age of 18 years and live in the same household (yes/no).
Education (time-varying): We grouped education into two categories: Less than higher education or unknown education level (reference group) and higher education.
Income level (time-varying): Low or medium/high (reference group). Based on personal income of the women (the sum of work and business-related income), we defined the threshold for low income as less than 50% of the median income for all women in our study, per year.
Statistical analyses
For the main analyses, we used discrete-time event history analyses (Allison, Citation1984) with logistic regression to investigate the odds of marital separation among women who have and have not used OPMH services and among both non-migrant and migrant women. We organized our data in person-period format, where each separate record represents each year an individual is at risk. Since marital changes are only recorded once per calendar year, we lagged the exposure variable by one year (use of OPMH) to ensure that OPMH occurred before the change in civil status. We also lagged all other time-varying covariates (dependent children, education and income) for the same reason. First, we conducted analyses with OPMH use and country of origin, while controlling for age. In the second model, we also controlled for marital history and dependent children, while in the third model we added in income level and education. To determine whether country of origin moderated the relationship between mental disorder (defined as OPMH use) and marital separation, we included an interaction term between OMPH use and country of origin in model 4, while controlling for all other predictors. We used STATA version 16 to analyze the data.
Findings
Population sample
Our population sample included 679,928 married women and a total of 4,732,433 observations. Women were in the study on average 6.96 years (range 2–9 years). However, due to our use of lag variables, the first year in the dataset (baseline) was redundant in the main analyses, resulting in 4,052,505 observations in the analyses. shows differences in the study variables by country of origin. Age is shown at the start of the study period while dependent child/ren, education and income level are shown for the last lagged year of the study period. Around 7% of non-migrant married women used OPMH services in the follow-up period, compared with 11% of Iraqi women. OPMH use was the least common among Somali, Thai and Filipino women (2%). Marital separation was least common among Pakistanis (8%) and most common among Somalis (25%).
Table 1. Characteristics of study population by country of origin.
Is mental disorder associated with marital separation?
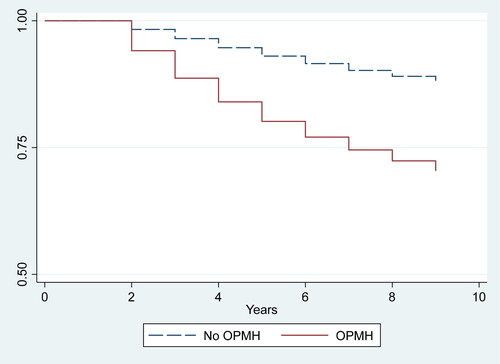
provides a visual overview of the association between mental disorder (OPMH use) and remaining married using Kaplan-Meier estimates. As expected, the decline in those remaining married was steeper among those who had used OPMH services compared with those who had not used OPMH services. The risk of separation continued to increase over time for those who had used OPMH services compared to those who had not. In this figure, we have not accounted for the time-varying nature of the exposure (when OPMH services were first used) or for covariates.
Event history analysis
shows the odds ratio (OR) for marital separation according to the different demographic variables. In model 1, having had an outpatient mental health consultation was associated with higher yearly odds of marital separation compared to those with no consultation during the follow-up period. While the yearly odds ratio for marital separation did not differ between non-migrant women and Filipinas, it was higher for Thai, Russian and Somali women and lower for Iraqi and Pakistani women.
Table 2. Discrete time analysis for the association between use of outpatient mental healthcare services (OPMH) and martial separation^.
In model 2, we included age, use of outpatient mental health services, country and previous marriage. We also ran analyses with dependent children but this was not significantly related to marital separation and we therefore excluded it from further analyses. The odds ratio for OPMH on marital separation decreased slightly from 2.68 to 2.46. Adding in education and income in model 3 reduced the odds of marital separation for those who used outpatient mental health services further (OR = 2.26) compared with those who did not. In this model, Iraqi women also had lower odds of marital separation compared with non-migrants. Russian and Somali women had at least twice the yearly odds, while Pakistani women, had around half the yearly odds of non-migrant women.
Finally, we introduced an interaction term between country of origin and use of OPMH while controlling for all covariates (model 4). The interaction term was significant for women from Russia, Somalia and The Philippines. Odds ratios indicated that the relationship between OPMH and marital separation was weaker for Russian and Somali women compared with non-migrant women but stronger for Filipinas.
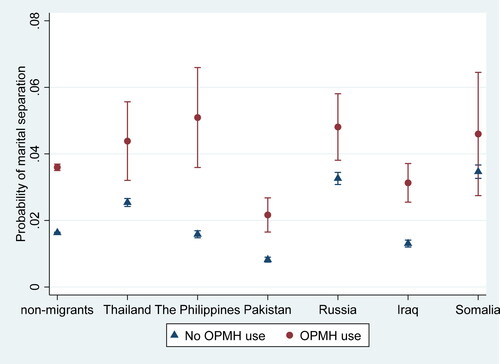
To investigate these relationships further, we plotted predicted yearly probabilities of marital separation. shows that for all groups, the yearly probability of marital separation was higher among those who had used OPMH than among those who had not. However, this difference was not significant for Somali women. The confidence interval for exposed Somali women was very wide (due to the small number using OPMH), indicating some uncertainty in this finding. The difference in the yearly probability of marital separation among Filipinas who had and had not used OPMH services, on the other hand, was considerably larger than for non-migrants.
Discussion
In this study, we found that overall, women who had attended outpatient mental health services had higher yearly odds of marital separation than women who had not attended OPMH services. This confirms previous research (Breslau et al., Citation2011; Mojtabai et al., Citation2017) and adds to the literature by showing that mental disorder is also associated with marital separation among migrant women. One explanation is that mental disorder can impair the ability to maintain a relationship (Breslau et al., Citation2011). Individuals with mental disorders may experience more relationship problems, which leads to marital breakdown.
However, marital problems are also associated with increased mental distress (Recksiedler & Stawski, Citation2019; Tavares & Aassve, Citation2013). Thus, it is also possible that those with relationship problems are at higher risk of developing a mental disorder, implying that OPMH, in this study, may be a symptom, rather than a cause, of marital separation. According to Reneflot et al. (Citation2020) help-seeing from a general practitioner for mental health problems is highest in the year of separation but is also elevated the year before and after. In this study, we lagged our analyses by one year, to ensure that the mental disorder occurred before the breakup. We also conducted a sensitivity analysis where we lagged OPMH by two years instead of one. Although the relationship between OPMH and marital separation was slightly reduced, the findings were remarkably similar to those shown above, despite including fewer individuals (see Appendix 1). Additionally, there is likely to be a delay between the onset of a mental disorder and our measure of onset (OPMH use). Many may not seek professional help right away and a general practitioner may try to treat the disorder at the primary care level. There is often a considerable time lapse between a referral to secondary care (which is usually required in Norway) and the first contact with OPMH. This also increases the time lag between onset of disorder and marital separation, making it likely that mental disorder, to some extent, is driving selection out of marriage.
Notably, in this explorative study, we found a difference in the strength of the association between OPMH and marital separation for some groups of migrant women. None of our proposed theoretical arguments appeared to be consistent with the observed differences in the relationship between OPMH use and marital separation across groups. Instead, the association between mental disorder and marital separation appeared to be weaker, the more common marital separation. To confirm this, however, investigation of the association between mental disorder and marital separation in a larger number of groups of migrant women, including those with fewer differences in cultural roles and values regarding marital separation (for example, EU migrant women), is required.
Somali women stood out most in this study; OPMH service use was not significantly associated with subsequent marital separation, while it was for all other groups. Somalis appear to be one of the most disadvantaged groups of migrants in Norway (Tronstad et al., Citation2018), so if our social disadvantage argument was correct, there would have been a stronger relationship between OPMH and marital separation. We also proposed that higher levels of stigma around divorce could result in a weaker relationship. Yet, we found that Somalis had the highest odds of separation and, while there are no official divorce statistics in Somalia, marital disruption in sub-Saharan Africa is considered common and divorce appears to be sanctioned (Clark & Brauner-Otto, Citation2015; Landinfo, Citation2018). Similarly, Somali and other African migrants have been observed to be at elevated risk of divorce in other studies (Andersson et al., Citation2015; Sandnes & Østby, Citation2015). For these groups, other factors, such as changes in gender norms and access to resources could play a larger role in decisions to separate than mental disorder (Al-Sharmani, Citation2017).
An alternative explanation for the lack of association between OPMH service use and marital separation among Somali women could be that there are many women with a mental disorder who have not used OPMH services. Use of mental health care services, both primary and secondary, is low among Somalis (Abebe et al., Citation2018; Straiton et al., Citation2017). In the current study, less than 2% of married Somali women had used OPMH services compared with 7% of non-migrant women. In addition to barriers such as language and ability to navigate the health care system (Gele et al., Citation2016), stigma surrounding mental disorder is a well-documented barrier among Somali migrants (Henning-Smith et al., Citation2013; Piwowarczyk et al., Citation2014). OPMH use may therefore be a poorer approximation of mental disorder than for non-migrants. In other words, there may be a high proportion of unidentified mental disorder among Somali women in this study. Although Somalis tend to report lower levels of mental health problems than many other migrant groups in surveys, and not higher than the general population (Rask et al., Citation2016; Vrålstad & Wiggen, Citation2017), the Hopkins Symptom Checklist scale, used in these studies, may not be culturally validated for Somalis. British researchers found that one third of Somali refugees had a mental disorder when applying a culturally adapted interview (Bhui et al., Citation2006). Thus, researchers need to consider if there is gap, and how to bridge it, between use of mental health care services and actual mental disorders among Somali migrants. Russian women also stood out in the findings. The relationship between OPMH service use and separation was weaker than for non-migrant women. This is in line with our suggestion that women in transnational marriages may experience disempowerment relative to non-migrant women (Eggebø, Citation2010; Flemmen & Lotherington, Citation2012; Straiton et al., Citation2018). They may be more reliant on their spouse when faced with mental disorder. Alternatively, since transnational couples may also experience many challenges in their marriage, including cultural conflict, distrust from others about their intentions with the marriage and a mismatch in age and education level (Adserà & Ferrer, Citation2015; Flemmen & Lotherington, Citation2012), there may be many other factors, that play a stronger role in the decision to separate than mental disorder.
Yet, among Filipino women, another group who often enter exogamous marriages, the association between use of OPMH and marital separation was somewhat stronger. We can only speculate as to the reasons for this. This group had similar odds of marital separation as non-migrant women. Many Filipinas move abroad to improve their family’s economic conditions (Mcdonald & Valenzuela, Citation2012). They send remittances home to pay for health care, education, food or shelter for their families in The Philippines. At the same time, many are married to non-migrants and may fear being unable to support their family if their marriage ends. Thus, it is possible that Filipinas are motivated to stay in unsatisfactory marriages unless it negatively affects their health. However, one might have expected the same pattern among Thai women, since they also tend to marry non-migrants, send remittances and are motivated to put their family’s wellbeing before their own (Straiton et al., Citation2019). Yet, the relationship between OPMH and marital separation was not significantly different for Thai women compared with non-migrant women. Perhaps this difference is because Thai women are more likely to enter a marriage with a non-migrant prior to moving to Norway than Filipino women (Sandnes & Østby, Citation2015) and may therefore experience greater dependency on their spouse when faced with mental disorder.
Interestingly, there was no significant difference in the association between use of OPMH services and marital separation for Iraqi and Pakistani women compared with non-migrants. These groups, especially Pakistanis, had overall lower odds of marital separation, which is in line with previous research (Adserà & Ferrer, Citation2015; Andersson et al., Citation2015; Sandnes & Østby, Citation2015). It could be that our competing theoretical arguments of social disadvantage and stigma around divorce and mental disorder cancel each other out, resulting in a similar association between OPMH use and marital separation as for non-migrants.
It should be noted that our measure of mental disorder only includes those who have used OPMH services. There is a large proportion of untreated, or inadequately treated mental disorders in the general population (Thornicroft et al., Citation2017; Torvik et al., Citation2018). Additionally, common mild to moderate disorders are mostly treated at the primary care level (Mykletun et al., Citation2010) so only those with more severe and enduring difficulties are identified in this study. Since migrants may experience greater barriers to care than non-migrants (Debesay et al., Citation2019; Satinsky et al., Citation2019; Thomson et al., Citation2015) there could be a greater proportion of migrant women who have a mental disorder but have not sought care, resulting in an underestimation of the association between mental disorder on marital separation for all our migrant groups. Researchers should investigate the size of the gap between need for, and use of, mental health services among different groups of migrants in the future. Nonetheless, this register study has national coverage and does not suffer from the associated difficulties of including migrants in surveys, such as selection bias (Norwegian Institute of Public Health, Citation2019; Reichel & Morales, Citation2017).
Another limitation in this study is that we may be slightly overestimating the proportion of migrants in their first marriage, compared with those in their second. This was because we were not able to identify migrants who had been married prior to coming to Norway if they were remarried before, or upon, arrival (within the same calendar year) in Norway. However, this variable did not explain much of the relationship between OPMH use and marital separation, so a slight overestimation is unlikely to have significantly affected the strength of the relationship between OPMH use and marital separation. We were also unable to control for some important predictors of marital separation, such as length of marriage and age upon marriage (Lyngstad & Jalovaara, Citation2010). Our information on marital status was obtained from the Central Population Register, which is updated once per year. The year of marriage (and therefore age upon marriage) was not available for migrants who were married before coming to Norway. Neither were we able to discriminate between those who married prior to arrival and those who married within the first year of arrival. Thus, length of, and age at, marriage was unknown for the majority of migrants included in this study. Adjusting for these variables would probably slightly weaken the association between OPMH use and marital separation, as it does in the non-migrant population. However, researchers from the US suggest that the relationship between age of marriage and risk of separation may not be the same across all ethnicities (Lehrer & Son, Citation2017). Finally, we lacked information on spouses, such as their age, education level, income level, migrant status and history of mental disorder. Future research should consider these factors, since they may influence both their spouses’ mental health and the risk of marital separation.
Our study findings add to a body of research looking at the relationship between mental disorder and marital separation using longitudinal data and suggest that mental disorder may have an adverse impact on relationships. Uniquely, we provide insight into marital breakdown among different groups of migrant women in Norway, and the role of mental disorder. It appears that the relationship may be weaker among migrant groups where separation is more common. While it is assumed that marital separation is a viable option for those who are in unhappy marriages in Norway, it is important to recognize that the obstacles may be larger for some groups of migrant women. Further, mental disorder may also affect educational attainment and future earnings (López-López et al., Citation2020). This coupled with reduced household income as a result of separation and potential reduction in social support due to associated stigma around separation and divorce, can have further ramifications for mental health of migrant women. Thus, it is important to identify and treat mental disorder early. General practitioners and other health care providers should be aware of the significance of mental disorder on life events such as marital separation and the subsequent implications on mental health. Further, in marital separation processes, or marital discord, it may be important to ask about mental health status and encourage or, particularly for migrant women, facilitate, help-seeking if deemed necessary. Finally, we also need more research to understand why the relationship between OPMH use and marital separation may be stronger for some groups of migrant women and weaker for others, compared with non-migrant women.
Appendix_1___final.docx
Download MS Word (29.9 KB)Additional information
Funding
References
- Aalandslid, V., & Tronstad, K. R. (2010). Family reunification, gender and employment [Norwegian] (23/2010; p. 56). Statistics Norway. https://www.ssb.no/a/publikasjoner/pdf/rapp_201023/rapp_201023.pdf
- Abebe, D. S., Elstad, J. I., & Lien, L. (2018). Utilization of somatic specialist services among psychiatric immigrant patients: The Norwegian Patient Registry Study. BMC Health Services Research, 18(1), 852. https://doi.org/10.1186/s12913-018-3672-y
- Adserà, A., & Ferrer, A. (2015). Immigrants and demography. In B. R. Chiswick & P. W. Miller (Eds.), Handbook of the economics of international migration (Vol. 1, pp. 315–374). Elsevier. https://doi.org/10.1016/B978-0-444-53764-5.00007-4
- Akpinar, A. (2003). The honour/shame complex revisited: Violence against women in the migration context. Women’s Studies International Forum, 26(5), 425–442. https://doi.org/10.1016/j.wsif.2003.08.001
- Allison, P. D. (1984). Event history analysis: Regression for longitudinal event data. SAGE Publications.
- Al-Sharmani, M. (2017). Divorce among transnational Finnish Somalis: Gender, religion, and agency. Religion and Gender, 7(1), 70–87. https://doi.org/10.18352/rg.10207
- Andersson, G., Obućina, O., & Scott, K. (2015). Marriage and divorce of immigrants and descendants of immigrants in Sweden. Demographic Research, 33, 31–64. https://doi.org/10.4054/DemRes.2015.33.2
- Beck-Gernsheim, E. (2011). The marriage route to migration: Of border artistes, transnational matchmaking and imported spouses. Nordic Journal of Migration Research, 1(2), 60–68. https://doi.org/10.2478/v10202-011-0008-y
- Bejanyan, K., Marshall, T. C., & Ferenczi, N. (2015). Associations of collectivism with relationship commitment, passion, and mate preferences: Opposing roles of parental influence and family allocentrism. PLoS One, 10(2), e0117374. https://doi.org/10.1371/journal.pone.0117374
- Bhui, K., Craig, T., Mohamud, S., Warfa, N., Stansfeld, S. A., Thornicroft, G., Curtis, S., & McCrone, P. (2006). Mental disorders among Somali refugees. Social Psychiatry and Psychiatric Epidemiology, 41(5), 400–408. https://doi.org/10.1007/s00127-006-0043-5
- Breslau, J., & Chang, D. (2006). Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Social Psychiatry and Psychiatric Epidemiology, 41(12), 943–950. https://doi.org/10.1007/s00127-006-0119-2
- Breslau, J., Miller, E., Jin, R., Sampson, N. A., Alonso, J., Andrade, L. H., Bromet, E. J., de Girolamo, G., Demyttenaere, K., Fayyad, J., Fukao, A., Gălăon, M., Gureje, O., He, Y., Hinkov, H. R., Hu, C., Kovess-Masfety, V., Matschinger, H., Medina-Mora, M. E., … Kessler, R. C. (2011). A multinational study of mental disorders, marriage, and divorce. Acta Psychiatrica Scandinavica, 124(6), 474–486. https://doi.org/10.1111/j.1600-0447.2011.01712.x
- Bufdir. (2020). Lavinntekt og økonomiske vansker blant personer med innvandrerbakgrunn. bufdir.no | Barne-, ungdoms- og familiedirektoratet. https://bufdir.no/Statistikk_og_analyse/Etnisitet/okonomi/lavinntekt_og_okonomiske_vansker/
- Chou, K.-L. (2007). Psychological distress in migrants in Australia over 50 years old: A longitudinal investigation. Journal of Affective Disorders, 98(1–2), 99–108. https://doi.org/10.1016/j.jad.2006.07.002
- Clark, S., & Brauner-Otto, S. (2015). Divorce in sub-Saharan Africa: Are unions becoming less stable? Population and Development Review, 41(4), 583–605. https://doi.org/10.1111/j.1728-4457.2015.00086.x
- Das, C. (2012). Barriers and supports to divorce for victimised British-Indian Mothers and consequences of divorce: Narratives of British-Indian adult children of divorce. Child Care in Practice, 18(2), 147–164. https://doi.org/10.1080/13575279.2011.646953
- Debesay, J., Arora, S., & Bergland, A. (2019). Migrants’ Consumption of Healthcare Services in Norway: Inclusionary and Exclusionary Structures and Practices. https://doi.org/10.18261/9788215031699-2019-04
- Delara, M. (2016). Social determinants of immigrant women’s mental health. Advances in Public Health, 2016, 9730162. https://doi.org/10.1155/2016/9730162
- Eggebø, H. (2010). The problem of dependency: Immigration, gender, and the welfare state. Social Politics: International Studies in Gender, State & Society, 17(3), 295–322. https://doi.org/10.1093/sp/jxq013
- Fernbrant, C., Essén, B., Östergren, P.-O., & Cantor-Graae, E. (2013). Navigating between control and autonomy: Recently arrived Iraqi refugees’ perceptions regarding honor, well-being, and risk for intimate partner violence. Journal of Immigrant & Refugee Studies, 11(2), 178–197. https://doi.org/10.1080/15562948.2013.776473
- Flemmen, A., & Lotherington, A. (2012). Transnational marriages: Politics and desire (pp. 127–137). Routledge.
- Furtado, D., Marcén, M., & Sevilla, A. (2013). Does culture affect divorce? Evidence from European immigrants in the United States. Demography, 50(3), 1013–1038. https://doi.org/10.1007/s13524-012-0180-2
- Gele, A. A., Pettersen, K. S., Torheim, L. E., & Kumar, B. (2016). Health literacy: The missing link in improving the health of Somali immigrant women in Oslo. BMC Public Health, 16(1), 1134. https://doi.org/10.1186/s12889-016-3790-6
- Gorodzeisky, A., & Semyonov, M. (2017). Labor force participation, unemployment and occupational attainment among immigrants in West European countries. PLOS One, 12(5), e0176856. https://doi.org/10.1371/journal.pone.0176856
- Gutiérrez-Rojas, L., Porras-Segovia, A., Dunne, H., Andrade-González, N., & Cervilla, J. A. (2020). Prevalence and correlates of major depressive disorder: A systematic review. Brazilian Journal of Psychiatry, 42(6), 657–672. https://doi.org/10.1590/1516-4446-2020-0650
- Henning-Smith, C., Shippee, T. P., McAlpine, D., Hardeman, R., & Farah, F. (2013). Stigma, discrimination, or symptomatology differences in self-reported mental health between US-born and Somalia-born Black Americans. American Journal of Public Health, 103(5), 861–867. https://doi.org/10.2105/AJPH.2012.301184
- Hollander, A.-C., Bruce, D., Burström, B., & Ekblad, S. (2011). Gender-related mental health differences between refugees and non-refugee immigrants-a cross-sectional register-based study. BMC Public Health, 11(1), 180. https://doi.org/10.1186/1471-2458-11-180
- Idstad, M., Torvik, F. A., Borren, I., Rognmo, K., Røysamb, E., & Tambs, K. (2015). Mental distress predicts divorce over 16 years: The HUNT study. BMC Public Health, 15(1), 320. https://doi.org/10.1186/s12889-015-1662-0
- IOM. (2019). The World Migration Report 2020. International Organization for Migration. https://worldmigrationreport.iom.int/wmr-2020-interactive/
- Jennings, E. A. (2016). Predictors of marital dissolution during a period of rapid social change: Evidence from South Asia. Demography, 53(5), 1351–1375. https://doi.org/10.1007/s13524-016-0504-8
- Landinfo. (2018). Somalia: Marriage and divorce. Landinfo.
- Lehrer, E., & Son, Y. (2017). Women’s age at first marriage and marital instability in the United States: Differences by race and ethnicity. Demographic Research, 37, 229–250. https://doi.org/10.4054/DemRes.2017.37.9
- López-López, J. A., Kwong, A. S. F., Washbrook, E., Pearson, R. M., Tilling, K., Fazel, M. S., Kidger, J., & Hammerton, G. (2020). Trajectories of depressive symptoms and adult educational and employment outcomes. BJPsych Open, 6(1), E6. https://doi.org/10.1192/bjo.2019.90
- Lyngstad, T. H., & Jalovaara, M. (2010). A review of the antecedents of union dissolution. Demographic Research, 23, 257–292. https://doi.org/10.4054/DemRes.2010.23.10
- Mcdonald, T., & Valenzuela, M. R. (2012). Why Filipino migrants remit? Evidence from a home-host country matched sample. Monash Economics Working Papers 09-12, Monash University, Department of Economics.
- Mirza, A., Birtel, M. D., Pyle, M., & Morrison, A. P. (2019). Cultural differences in psychosis: The role of causal beliefs and stigma in White British and South Asians. Journal of Cross-Cultural Psychology, 50(3), 441–459. https://doi.org/10.1177/0022022118820168
- Mojtabai, R., Stuart, E. A., Hwang, I., Eaton, W. W., Sampson, N., & Kessler, R. C. (2017). Long-term effects of mental disorders on marital outcomes in the National Comorbidity Survey ten-year follow-up. Social Psychiatry and Psychiatric Epidemiology, 52(10), 1217–1226. https://doi.org/10.1007/s00127-017-1373-1
- Molstad, C. S. (2020). Family migration and marriage patterns 1990-2018 (2020/5; p. 70). Statistics Norway. https://www.ssb.no/befolkning/artikler-og-publikasjoner/_attachment/411225?_ts=16ffbcb2098
- Mykletun, A., Knudsen, A. K., Tangen, T., & Overland, S. (2010). General practitioners’ opinions on how to improve treatment of mental disorders in primary health care. Interviews with one hundred Norwegian general practitioners. BMC Health Services Research, 10, 35. https://doi.org/10.1186/1472-6963-10-35
- Norwegian Institute of Public Health. (2019). Health among immigrants in Norway: Living conditions survey among immigrants in Norway 2016 (p. 167). Norwegian Institute of Public Health. https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2019/levekarsundersokelsen-blant-innvandrere-i-norge-2016-rapport-2019-v2.pdf
- Ortiz-Ospina, E., & Roser, M. (2020, July 25). Marriages and divorces. Our World in Data. https://ourworldindata.org/marriages-and-divorces
- Piwowarczyk, L., Bishop, H., Yusuf, A., Mudymba, F., & Raj, A. (2014). Congolese and Somali beliefs about mental health services. Journal of Nervous and Mental Disease, 202(3), 209–216.
- Qian, Z. (2013). Divergent paths of American families. https://s4.ad.brown.edu/Projects/Diversity/Data/Report/report09112013.pdf
- Rask, S., Suvisaari, J., Koskinen, S., Koponen, P., Mölsä, M., Lehtisalo, R., Schubert, C., Pakaslahti, A., & Castaneda, A. E. (2016). The ethnic gap in mental health: A population-based study of Russian, Somali and Kurdish origin migrants in Finland. Scandinavian Journal of Public Health, 44(3), 281–290. https://doi.org/10.1177/1403494815619256
- Recksiedler, C., & Stawski, R. S. (2019). Marital transitions and depressive symptoms among older adults: Examining educational differences. Gerontology, 65(4), 407–418. https://doi.org/10.1159/000493681
- Reichel, D., & Morales, L. (2017). Surveying immigrants without sampling frames – Evaluating the success of alternative field methods. Comparative Migration Studies, 5(1), 1. https://doi.org/10.1186/s40878-016-0044-9
- Reneflot, A., Øien-Ødegaard, C., & Hauge, L. J. (2020). Marital separation and contact with primary healthcare services for mental health problems: A register-based study. BMC Psychology, 8(1), 124. https://doi.org/10.1186/s40359-020-00488-0
- Saechao, F., Sharrock, S., Reicherter, D., Livingston, J. D., Aylward, A., Whisnant, J., Koopman, C., & Kohli, S. (2012). Stressors and barriers to using mental health services among diverse groups of first-generation immigrants to the United States [Health & Mental Health Services]. Community Mental Health Journal, 48(1), 98–106. [ https://doi.org/10.1007/s10597-011-9419-4
- Sandnes, T., & Østby, L. (2015). Family migration and marriage patterns 1990–2013 [Norwegian] (2015/23). Statistics Norway. http://www.ssb.no/befolkning/artikler-og-publikasjoner/_attachment/228459?_ts=14d70308ab8
- Satinsky, E., Fuhr, D. C., Woodward, A., Sondorp, E., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy (Amsterdam, Netherlands), 123(9), 851–863. https://doi.org/10.1016/j.healthpol.2019.02.007
- Sharma, I., Pandit, B., Pathak, A., & Sharma, R. (2013). Hinduism, marriage and mental illness. Indian Journal of Psychiatry, 55(Suppl 2), S243–S249. https://doi.org/10.4103/0019-5545.105544
- Statistics Norway. (2020, March). Employment among immigrants, register-based. Ssb.No. https://www.ssb.no/en/arbeid-og-lonn/statistikker/innvregsys/aar/2020-03-02
- Straiton, M. L., Ansnes, T., & Tschirhart, N. (2019). Transnational marriages and the health and well-being of Thai migrant women living in Norway. International Journal of Migration, Health and Social Care, 15(1), 107–119. https://doi.org/10.1108/IJMHSC-01-2018-0002
- Straiton, M. L., Heloise, M. L., & Donnelly, T. T. (2018). It has not occurred to me to see a doctor for that kind of feeling” Filipina immigrants’ perceptions of help-seeking for mental health problems. BMC Women’s Health, 18, 73.
- Straiton, M. L., Reneflot, A., & Diaz, E. (2017). Mental health of refugees and non-refugees from war-conflict countries: Data from Primary healthcare services and the Norwegian prescription database. Journal of Immigrant and Minority Health, 19(3), 582–589. https://doi.org/10.1007/s10903-016-0450-y
- Tavares, L. P., & Aassve, A. (2013). Psychological distress of marital and cohabitation breakups. Social Science Research, 42(6), 1599–1611. https://doi.org/10.1016/j.ssresearch.2013.07.008
- Thomson, M. S., Chaze, F., George, U., & Guruge, S. (2015). Improving immigrant populations’ access to mental health services in Canada: A review of barriers and recommendations. Journal of Immigrant and Minority Health, 17(6), 1895–1905. https://doi.org/10.1007/s10903-015-0175-3
- Thornicroft, G., Chatterji, S., Evans-Lacko, S., Gruber, M., Sampson, N., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Andrade, L., Borges, G., Bruffaerts, R., Bunting, B., de Almeida, J. M. C., Florescu, S., de Girolamo, G., Gureje, O., Haro, J. M., He, Y., Hinkov, H., … Kessler, R. C. (2017). Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry: The Journal of Mental Science, 210(2), 119–124. https://doi.org/10.1192/bjp.bp.116.188078
- Tinghög, P., Malm, A., Arwidson, C., Sigvardsdotter, E., Lundin, A., & Saboonchi, F. (2017). Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: A population-based survey. BMJ Open, 7(12), e018899. https://doi.org/10.1136/bmjopen-2017-018899
- Torvik, F. A., Ystrom, E., Gustavson, K., Rosenström, T. H., Bramness, J. G., Gillespie, N., Aggen, S. H., Kendler, K. S., & Reichborn-Kjennerud, T. (2018). Diagnostic and genetic overlap of three common mental disorders in structured interviews and health registries. Acta Psychiatrica Scandinavica, 137(1), 54–64. https://doi.org/10.1111/acps.12829
- Tronstad, K. R., Nygaard, M., & Bask, M. (2018). Accumulation of welfare problems among immigrants in Norway (2018:8; NIBR Report). Norwegian Institute for Urban and Regional Research.
- Vrålstad, S., & Wiggen, K. S. (2017). Living conditions among imigrants in Norway 2016 (2017/13). Statistics Norway. http://www.ssb.no/308564/living-conditions-among-imigrants-in-norway-2016
- Waseem, J., Muneer, R., Hoor-Ul-Ain, S., Tariq, R., & Minhas, A. (2020). Psychosocial determinants of divorce and their effects on women in Pakistan: A national review. International Journal of Human Rights in Healthcare, 13(4), 299–315. https://doi.org/10.1108/IJHRH-09-2018-0059
- Youssef, J., & Deane, F. P. (2006). Factors influencing mental-health help-seeking in Arabic-speaking communities in Sydney, Australia. Mental Health, Religion & Culture, 9(1), 43–66. https://doi.org/10.1080/13674670512331335686