ABSTRACT
Transitions into and out of Daylight Saving Time (DST) can provide insights into how a minor change to a regular sleep–wake cycle can inadvertently affect health. We examined the relationship between DST and missed medical appointments. Using a large dataset, the proportion of missed appointments were examined prior and post spring and autumn clock changes. As predicted, the number of missed medical appointments significantly increased following the spring (forward) clock change and the week of the clock change. This trend was reversed following the transition out of DST. The implications of scheduling appointments around DST to increase attendance are discussed.
More than 1.5 billion men and women are exposed to the transitions involved as the clocks go forward 1 hour in the spring and backward 1 hour in the autumn (Janszky and Ljung Citation2008). Known as Daylight Saving Time (DST), these changes can disrupt chronobiologic rhythms and influence the duration and quality of sleep, with the effect lasting several days after the shifts (Kantermann et al. Citation2007; Lahti et al, Citation2006). The transition into DST in spring can disrupt chronobiologic rhythms and this has numerous adverse biological effects including the predominance of sympathetic activity and an increase in pro-inflammatory cytokine levels (Meier-Ewert et al. Citation2004; Spiegel et al. Citation1999). Conversely, the transition out of DST in autumn has been shown to be less detrimental to the sleep/wake cycle (Tonetti et al. Citation2013).
A wealth of research has examined the impact of the transitions into and out of DST on human behaviour and health, including road traffic accidents (Coren Citation1996), workplace injuries (Barnes & Wagner, Citation2009), and impairments in mood and cognition (Monk and Aplin Citation1980); all of which have been attributed to changes in sleep duration/quality and circadian misalignment. For example, Janszky and Ljung (Citation2008) examined the influence of the forward and backward time transitions on the incidence of acute myocardial infarction. They compared the incidence of acute myocardial infarction during each of the first seven days after the spring or autumn transition and the mean of the incidences on the corresponding weekdays two weeks before and two weeks after the day of the time change. Janszky and Ljung found that the incidence of myocardial infarction was significantly higher for the first three weekdays after the transition to DST in the spring. In contrast, after the transition out of DST in the autumn, only the first weekday was affected significantly. This pattern was more pronounced in those under the age of 65 than for those 65 years or older. Similar results were also found in more recent studies (Kirchberger et al. Citation2015; Janszky et al. Citation2012; Jiddou et al. Citation2013; but see Sipila et al. Citation2016).
In terms of examining the effects that transitions into and out of DST can also have on memory and cognition, Barnes and Wagner (Citation2009) conducted a study examining the impact of DST on workplace injuries. They examined a large dataset spanning more than 20 years of miner data and found that there were more injuries following the change to DST, resulting in nearly 70% more days in work being lost due to these injuries. The effects of the transition into DST have also been found to impact stock market volatility (Berument and Dogan Citation2011; Kamstra et al. Citation2000; but see Pinegar Citation2002) as sleep deprivation may increase risky behaviour and impact human performance and decision-making. For a comprehensive review of DST and its impact on health, memory and cognition, see Harrison (Citation2013).
In general, previous research has focused on health, memory and cognition in isolation. The current study merged these two strands of research by utilising hospital admission data to explore how transitions into and out of DST may impact missed appointments within secondary care. Therefore, the proposed analysis adds to the larger body of evidence that DST effects are tangible and have a measurable impact on individuals and society. Given the negative effects associated with reduced sleep as a result of the spring transition into DST, it was hypothesised that non-attendance would increase in the weeks following the springtime change and that this effect would be reversed following the transition out of DST in autumn. Therefore, the goal of the current study is to examine the impact of DST on medical appointment attendance patterns within a large dataset.
Method
Sample
Information Services Division Scotland provided a complete record of outpatient hospital appointments for the whole of Scotland, from 1 January 2005 to 31 December 2010. The records consisted of 7,531,597 scheduled appointments in total. It should be noted that there were 3,891 instances where patient data was unavailable due to issues of anonymity (i.e. four or less patients scheduled for an appointment). To our knowledge, this is the largest corpus of data for which missed appointment rates have been analysed. Weekend appointments were infrequent (approximately 2% of cases) and were excluded from the analysis. Due to data constraints, only patients over the age of 20 were included in analyses.
Analysis
To test for DST trends in non-attendance, we categorised 2,015,078 scheduled appointments based on the week of the clock change, the preceding three weeks of the clock change, and the following three weeks after the clock change (for both transitions into and out of DST). Did Not Attend (DNA) rates (i.e. the percentage of appointments that were missed) were calculated separately for each week. Null hypothesis significance testing (NHST) with a significance level of p < .05 was applied as it is the conventional tool among quantitative researchers. However, practical significance, rather than statistical significance, was of primary concern for this program of research. Thus, the size of the effects are emphasised during the presentation and interpretation of results.
Results
During the spring (forward) clock change, an increase in DNA rate was observed when comparing the week before (9.57%) and immediately after (10.01%) the clock change [χ2 (1, N = 276,819) = 14.87, p < 0.001] (see ). This trend was significant for both men [χ2 (1, N = 109,928) = 12.64, p < 0.001] and women [χ2 (1, N = 166,891) = 4.02, p = 0.045] (see ). No reliable change was observed between the week of change and week following, however, (10.26%) [χ2 (1, N = 252,080) = 2.89, p = 0.089].
Table 1. Demographic information showing similar proportions of appointments allocated based on patient age and gender.
Figure 1. DNA rates by week. Faded lines represent data for each year, solid line is the mean. A: Illustrates an increase in missed appointments following the spring change (forward). B: Illustrates a decrease in missed appointments following the autumn change (backward).
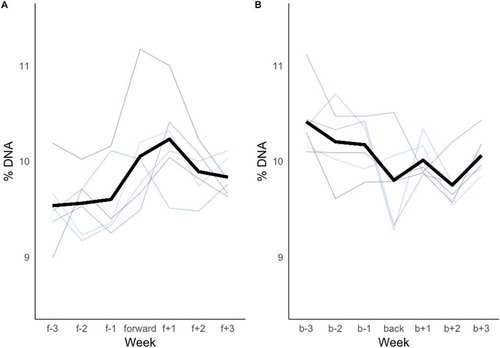
During the autumn (backward) clock change, a reliable decrease in DNA rate was observed before (10.18%) and during (9.79%) the clock change [χ2 (1, N = 306,388) = 12.44, p < 0.001] (see ). This trend was significant for men [χ2 (1, N = 121,601) = 9.69, p = 0.002] but not for women [χ2 (1, N = 184,787) = 3.71, p = 0.05] (see ). A reliable change was also observed between the week of change and one week following (10.01%) [χ2 (1, N = 311,925) = 4.25, p = 0.039], showing an increase in missed appointments.
Finally, it is possible to consider both forward and backward effects in terms of relative risk (Altman Citation1991). Comparing the week immediately following the transition into DST in the spring with the previous week, it was observed that patients were 4.6% more likely to miss an appointment in the week of the change. Conversely, patients were 3.75% more likely to attend in the week following the transition out of DST in the autumn compared to the week prior to the clock change.
Discussion
The goal of the current study was to determine whether there was a reliable change in DNA rates during both the spring and autumn DST changes. In a large dataset, modest but consistent alterations in the number of missed appointments were observed. Specifically, an increase in DNA rates was observed for the spring (forward) clock change and a decrease in DNA rates was observed for the autumn (backward) clock change. A significant effect was observed for both male and female patients (with the exception of female patients for the transition out of DST). Although the study and did not address the causes of the DST effect directly, the observed changes in DNA rates suggests that changes in sleep patterns may have an impact on missed appointments. A similar trend has also been observed when measuring punctuality, with patients arriving earlier for appointments following transitions out of DST (Valax et al. Citation2016).
The increase in missed appointments observed following the spring (forward) clock change suggest that the potential disruption of chronobiologic rhythms during the transition into DST (e.g. losing an hour of sleep, decreased sleep quality) may translate into patients missing more scheduled appointments and the effect may carry over into the following week (Kantermann et al. Citation2007; Lahti et al., Citation2006). The results also showed that the effect persists beyond the week of change, suggesting that the increase in non-attendance may take longer to settle following a forward clock change. The results of the current study also support previous work by Wagner et al. (Citation2012) who investigated the negative effects of DST in the workplace; specifically on so-called cyberloafing, the time people spend using work hours to check personal emails and browse websites unrelated to work. Using Google search data, the authors were able to demonstrate that shifting into DST resulted in a large increase in cyberloafing. They also carried out an additional experiment, which illustrated a clear relationship between poor quality of sleep and increased levels of cyberloafing. Conversely, the decrease in missed appointments observed after the clock change in autumn suggests that the potential benefits of the transitions out of DST (e.g. extra sleep, improved sleep quality) may translate into improved attendance for scheduled hospital appointments. Such data are consistent with published literature indicating that cognition and health are improved following the autumn clock change (Coren Citation1996; Janszky and Ljung Citation2008). It is worth noting however, that the benefits of increased attendance in the autumn appear to be quite short lived as non-attendance appears to increase quickly in the week following a transition.
It has been postulated that people in Western societies are chronically sleep deprived (Spiegel et al. Citation1999) and it is therefore assumed that changes to sleep quality and/or quantity may underpin the mechanism which changes behaviour during transitions into and out of DST. However, there is comparatively little evidence to suggest that sleep hours are gained following the autumn clock change for example (Harrison Citation2013). One alternative explanation might suggest that, rather than changes to sleeping patterns, the circadian rhythm simply adjusts after the clocks turn back, which may cause people to be early for appointments following the backward clock change and late for appointments when the clocks move forward. However, this is an empirical question that would require additional research.
There are at least two potential limitations associated with the current study. First, the data do not allow us to confirm the exact mechanism of action in terms of what causes the observed effects. That is, people miss appointments for a variety of reasons. However, the effects observed build on the convergence of evidence with effects found in other DST studies examining human behaviour. Second, due to the constraints of the dataset, we are unable to determine exactly what health issues that patients presented at each appointment. It may be the case that patients are missing appointments in relation to health issues such as age related memory deficits. However, older patients are more likely to attend appointments overall (e.g. Ellis and Jenkins Citation2012). This potential limitation appears to be mitigated by the large dataset.
Overall, the current findings represent a large practical significance in terms of the impact on health services. Missed appointments represent a significant financial issue for healthcare systems and have an adverse impact on patient care (Williamson et al. Citation2017). Specifically, small changes in non-attendance for medical appointments could have large implications across the health service. For example, an absolute reduction in DNA rate of just 1.2% could save £60 million per year (Ellis and Jenkins Citation2012). Further, improving attendance rates of medical appointments would also reduce health risk to patients as their conditions are treated promptly reducing health complications of untreated conditions (Gucciardi Citation2008; Murdock et al. Citation2002; Weinger et al. Citation2005).
One possible solution to the observed negative impact on appointment attendance can be observed in previous research which showed that attendance rates could be improved by making some minor modifications to appointment scheduling (Ellis and Jenkins Citation2012). In terms of future research, it would be of interest to examine possible interventions for ameliorating missed appointments, especially during transitions into DST. For example, a simple intervention to reduce non-attendance might involve sending a few additional reminders to patients as spring approaches. Similarly, scheduling more appointments during the week prior to leaving DST would capitalise on higher attendance levels. Therefore, reductions in DNA rates achieved through reminder schemes and through scheduling improvements may be additive, if these very different approaches target separable causes of non-attendance (e.g. forgetting and motivation, respectively). Exploiting these and other patterns within scheduling could help save money and improve patient care.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgement
The authors would like to acknowledge Simon D. Kyle for helpful discussions relating to this work.
Additional information
Funding
References
- Altman DG. 1991. Practical statistics for medical research. London:Chapman and Hall.
- Barnes CM, Wagner DT. 2009. Changing daylight saving time cuts into sleep and increases workplace injuries. J Appl Psychol 94:1305–17.
- Berument H, Dogan N. 2011. Effects of daylight saving time changes on stock market volatility: A reply. Psychol Rep 109:863–78.
- Coren S. 1996. Daylight savings time and traffic accidents. N Engl J Med 334:924–25.
- Ellis DA, Jenkins R. 2012. Weekday affects attendance rate for medical appointments: Large-scale data analysis and implications. PLoS One 12:e51365.
- Gucciardi E. 2008. A systematic review of attrition from diabetes education services: Strategies to improve attrition and retention research. Can J Diabetes Care 32:53–65.
- Harrison Y. 2013. The impact of daylight saving time on sleep and related behaviours. Sleep Med Rev 17:285–92.
- Janszky I, Ahnve S, Ljung R, Mukamal KJ, Gautam S, Wallentin L, Stenestrand U. 2012. Daylight saving time shifts and incidence of acute myocardial infarction – Swedish register of information and knowledge about Swedish heart intensive care admissions (RIKS-HIA). Sleep Med 13:237–42.
- Janszky I, Ljung R. 2008. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med 359:1966–68.
- Jiddou MR, Pica M, Boura J, Qu L, Franklin BA. 2013. Incidence of myocardial infarction with shifts to and from daylight savings time. Am J Cardiol 111:631–35.
- Kamstra MJ, Kramer LA, Levi MD. 2000. Losing sleep at the market: The daylight saving anomaly. Am Econ Rev 90:1005–11.
- Kantermann T, Juda M, Merrow M, Roenneberg T. 2007. The human circadian clock’s seasonal adjustment is disrupted by daylight saving time. Curr Biol 17:1996–2000.
- Kirchberger I, Wolf K, Heier M, Kuch B, Von Scheidt W, Peters A, Meisinger C. 2015. BMC Public Health 15:778–86.
- Lahti TA, Leppamaki S, Lonnqvist J, Partonen T. 2006. Transition to daylight saving time reduces sleep duration plus sleep efficiency of deprived sleep. Neurosci Lett 406:174–77.
- Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, Mullington JM. 2004. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43:678–83.
- Monk TH, Aplin LC. 1980. Spring and autumn daylight saving time changes: Studies of adjustment in sleep timings, mood, and efficiency. Ergonomics 23:167–78.
- Murdock A, Rogers C, Lindsay H, Tham T. 2002. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J Roy Soc Med 95:284–86.
- Pinegar JM. 2002. Losing sleep at the market: Comment. Am Econ Rev 92:1251–56.
- Sipila JOT, Rautava P, Kyto V. 2016. Association of daylight saving time transitions with incidence and in-hospital mortality of myocardial infarction in Finland. Ann Med 48:10–16.
- Spiegel K, Leproult R, Van Cauter E. 1999. Impact of sleep debt on metabolic and endocrine function. The Lancet 354:1435–39.
- Tonetti L, Erbacci A, Fabbri M, Martoni M, Natale, V. 2013. Effects of transitions into and out of daylight saving time on the quality of the sleep/wake cycle: An actigraphic study in healthy university students. Chronobiol Int 30:1218–22.
- Valax MF, Rattat AC, Baracat B, Cegarra J. 2016. Effect of daylight saving time on Punctuality for Medical Appointments. Applied Cognitive Psychology 30:911–16.
- Wagner DT, Barnes CM, Lim VKG, Ferris DL. 2012. Lost sleep and cyberloafing: Evidence from the laboratory and a daylight saving time quasi-experiment. J Appl Psychol 97:1068–76.
- Weinger K, McMurrich S, Yi J, Lin S, Rodriguez M. 2005. Psychological characteristics of frequent short-notice cancellers of diabetes medical and education appointments. Diabetes Care 28:1791–93.
- Williamson A, Ellis DA, Wilson P, McQueenie R, McConnachie A. 2017. Understanding repeated non-attendance in health services: Pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ Open 7:e014120.
