ABSTRACT
The present study aimed to investigate the effects of shift work on sleep among pilots and Helicopter Emergency Medical Service crew members (HCM) in the Norwegian Air Ambulance. Sleep was assessed by diaries and actigraphy during a workweek (24 h duty for 7 consecutive days) in the winter season and a workweek during the summer season in pilots and HCM (N = 50). Additionally, differences in sleep were studied between the week before work, the workweek, and the week after work in both seasons. Results indicated that bedtime was later (p <.001) and time spent in bed (p <.05) was shorter during the summer, compared to the winter, season. The workers delayed the sleep period in the workweek, compared to the week before (winter: p <.001, summer: p <.001) and the week after (winter: p <.05-.001, summer: p <.001). They spent more time in bed during the workweek, compared to the week before (winter: p <.001, summer: p <.01) and after (winter: p <.001, summer: p =.37). Further, the workers had longer wake after sleep onset during the workweek, compared to the week before (winter: p <.001, summer: p <.01) and the week after (winter: p <.01, summer: p <.01). Finally, the workers had lower sleep efficiency during the workweek recorded by actigraphy compared to the week before (winter: p <.01, summer: p <.001) and the week after (winter: p <.01, summer: p <.001). According to the sleep diaries the total sleep time was 7:17 h in the winter and 7:03 h in the summer season. Overall, the sleep was somewhat affected during the workweek, with delayed sleep period, longer wake after sleep onset, and lower sleep efficiency compared to when off work. However, the workers spent more time in bed during the workweek compared to the weeks off, and they obtained over 7 h of sleep in both workweeks. Our findings suggest that the pilots and the HCM sleep well during the workweek, although it affected their sleep to some extent.
Introduction
Shift work can be defined as work whereby the workers succeed each other at the workplace following certain patterns, entailing work outside normal daytime, including evenings, nights, and/or weekends (European Directive Citation2003/88/EC 2003). Concerns regarding the negative effects of shift work date back to the 13th century (Bjerner et al. Citation1948). Shift work is associated with acute sleep loss related to early morning and night shifts, with reported reductions of 2–4 h following night shifts (Kecklund and Axelsson Citation2016; Sallinen and Kecklund Citation2010). A characteristic of shift work is extended working hours, often denoted as work beyond 48 h per week (Harrington Citation2001). Such work schedules often imply activity at a time when the internal circadian clock is set at rest and inactivity, and sleep at times when the worker is biologically set to be awake, typically causing sleepiness as well as insomnia (Rosenwasser and Turek Citation2015). Studies indicate that extended working hours are associated with lower sleep efficiency and less total sleep time (Rhéaume and Mullen Citation2018; Swanson et al. Citation2011). Notably, sleep disruption has several well-known detrimental effects related to health, safety, and performance (Folkard and Tucker Citation2003; Medic et al. Citation2017).
Helicopter Emergency Medical Services (HEMS) are increasing becoming a part of the Emergency Medical Service (EMS) throughout the world (Butler et al. Citation2010; Taylor et al. Citation2011). The main indication for HEMS use is severe disease or trauma of patients in need of advanced medical treatment and/or rapid transport to hospital. HEMS is an on-demand medical service, and for the HEMS crew the shift work schedule entails work at irregular hours. Although studies indicate that certain types of accidents, and consequently missions, could be predicted to some extent (Folkard Citation1997; Manfredini et al. Citation2009; Smolensky et al. Citation2015), generally there is low predictability in terms of their quantity, type, and duration. The organization of HEMS varies considerably between countries regarding both work schedules and settings. The work schedules of different HEMS in Europe vary greatly – from 12, 24, and 48 h shifts in Netherland and Finland (Radstaak et al. Citation2014; Sallinen et al. Citation2018), and up to 7 consecutive 24 h shifts in Norway and Austria (Zakariassen et al. Citation2019). Some live on the helicopter base, while others commute every day, and there are also differences regarding the extent to which the crew takes on missions after dark (Radstaak et al. Citation2014; Zakariassen et al. Citation2019).
HEMS operations in Norway are scheduled as 24 h shifts over 7 consecutive d as an around-the-clock operation, with work periods generally being busier during summer compared to winter (Luftambulansetjenesten Citation2020). During the 7 consecutive d shifts the workers engage in on-call work and respond to incoming missions. This implies the crew lives on the base and takes on missions 24/7 for one week. There is large seasonal variation in the duration of daylight in Norway. For example, in the capital Oslo (59.91°N), duration of daylight in November is ~8.5 h and in May it is ~16.0 h, whereas in places north of 67.30°N there is polar night (winter) and midnight sun (summer). Still, there is a dearth of studies investigating what effect the work schedule has on sleep and if this varies by season. HEMS operations add additional risk to patient and crew. Between 1st January 2014 and 30th of May 2020, the Accident Investigation Board Norway (Citation2020) identified 1 accident resulting in 2 fatalities and 1 seriously injured. However, numbers of near-misses are unknown. Given the large potential damage of accidents in HEMS compared to ground-based EMS, this is an area that demands attention. Lack of sleep alters cognitive functions that could affect workers’ ability to perform satisfactorily and may potentially compromise safety (Monk and Folkard Citation1992). This could result in detrimental effects for both crew and patients. Still, we previously found HEMS crew members performed well on a reaction time test throughout the workweek (Flaa et al. Citation2019), suggesting that they were not sleep deprived. More research on the effects of consecutive shifts and long working hours on the sleep of pilots and HEMS crew members (HCM) is deemed essential, and longitudinal and multilevel studies on sleep in a work setting have been called for in order to fill the knowledge gaps in this research area (Litwiller et al. Citation2017).
Accordingly, the aim of the present study was to examine sleep in pilots and HCM on 24 h duty for 7 consecutive d, during two different work periods covering both the winter and summer season. We also examined how total work time and workload affected sleep variables during the workweek. In addition, we studied sleep over three consecutive weeks including the week at home before work, the workweek, and the week at home after work, in both the winter and the summer season. This enabled an examination of potential differences in sleep across the different weeks on and off work across seasons.
Methods
Study setting
In the Norwegian Air Ambulance, shifts are arranged in a 7d duty period followed by 14d off duty, before a new 7d duty period, followed by 21d off duty, period. The shift schedule is identical in all bases involved in the study. The crew lives together on the base during the duty week and conducts on-demand missions around the clock throughout the year. The duty week starts at 10:00 h on Monday morning and ends at 10:00 h following Monday. Workers commute either the same day as the shift starts or the day before. On the base, the crew has access to all the necessary facilities, including a kitchen, exercise room, and living room with TV. Each worker has his/her own separate bedroom with private bathroom, and can control the indoor light using a switch, outdoor light by blackout curtains, and temperature using a radiator. An operating fatigue risk management system (FRMS) includes flight and active work time limitations approved by the Civil Aviation Authority of Norway. The FRMS comprises a human-designed system based on institutional standards for flight- and duty time limitations. Flight time includes missions and training sessions. Active work time includes flight time, administrative duties, technical tasks, and rapid response car missions to locations near the base. The limits for active work time are 14 h over a consecutive 24 h period and 30 h over a 3d period. The maximum flight time is 7 h over a 24 h period, 12 h in a consecutive 48 h period, and 30 h over 7d. If the active work time limit is reached within a 24 h period, the crew (including both the pilot and HCM) must go off flight duty for 8 h. If a crew reaches their limit, the missions are allocated to the nearest base when appropriate. In 2015, the accessibility level was 98% (National Air Ambulance Service of Norway Citation2015).
Procedure
Sleep data were collected over three consecutive weeks (the week before work, the workweek, and the week after work) in two separate periods, one in the winter (October – December) and one in the summer season (May – July). The pilots and HCM completed sleep diaries and wore actigraphs every day throughout the 6 test weeks. On their first duty day, pilots and HCM also completed a questionnaire assessing various sociodemographic variables. The total amount of time the worker would need to complete the daily diaries was 5–10 min, and, therefore, it was not thought to alter their habits and behaviour notably.
Participants
The study took place in fall/winter of 2014 and spring/summer of 2015. All pilots and HCM (n = 70) at the 9 air ambulance bases in Norway operated by the Norwegian Air Ambulance were invited to take part in the study. One of the 9 bases was located in the northern part of Norway, the remaining were located in Trondheim or further south. In all, 61 (87%) workers participated in the fall/winter data collection. Two participants were excluded from the spring/summer data collection, due to changes in their work responsibilities and organizational tasks inconsistent with the remaining sample. Thus, 59 subjects were invited to participate in the spring/summer data collection. A total of 50 (85% of invited/71% of total) pilots and HCM participated in this spring/summer data collection.
Instruments
Questionnaire
The questionnaire contained items assessing background and demographic variables, such as age (y), sex (male/female), marital status (married/cohabiting yes/no), children living at home (yes/no), second job (yes/no), chronotype (1 – pronounced morning type – 5 pronounced evening type), smoking (yes/no), use of sleeping aid (yes/no; which), and physical health (1 very good – 5 very poor). A question regarding sleep need (in h) was also included. All descriptive data were collected during the workweek in the winter season.
Sleep measured with sleep diary
Daily estimates of prior sleep periods were obtained with a modified version of a sleep diary published by Morin (Citation1993). The sleep diary was completed after waking up in the morning for three consecutive weeks in both data collection periods. In all, 50 workers completed a sleep diary in both data collection periods. Based on the diary data, we calculated the crew’s bed time, wake-up time, time in bed, wake after sleep onset, sleep efficiency (total sleep time as a percentage of time in bed), as well as total sleep time.
Sleep measured with actigraphy
Sleep/wake profiles were measured by wrist actigraphy (Actiwatch 2, Respironics Inc.), a device that has the size and appearance of a wristwatch (CamNtech Ltd Citation2008). The actigraph is considered to provide valid and accurate estimates of sleep patterns in normal, healthy adults (Sadeh et al Citation2011; Stone and Ancoli-Israel Citation2011). Further, reliability of the actigraph is found to increase with extended study length (> 5 d; Sadeh et al 2011). It was programmed to record individual sleep/wake profiles continuously in 1-min epochs, using the medium (default) threshold for sleep and wake period detection provided by the software Actiware. For medium threshold, the sensitivity threshold (number of activity counts used to identify wake) was 40 per epoch. Sleep start and sleep end threshold were 10 min of immobility. The workers were instructed to wear the actigraph on the wrist of the non-dominant arm continuously for all three weeks, and to press an event button on the device to indicate bedtime and wake-up time. Scoring was built upon the steps proposed by Chow et al. (Citation2016), including a hierarchical approach emphasizing event markers and then activity levels. For the actigraphs in the present study, the light markers were not set up due to storage limitations. Thus, the scoring was based on sleep diary and activity level in those cases where the event markers were absent (30% of the observations). To avoid overestimation of sleep length, the wake-up time was based on self-reported wake-up time despite low activity level in the absence of an event marker, as workers might stay in bed after awakening. Variables such as bedtime, wake-up time, time in bed, wake after sleep onset, sleep efficiency, and total sleep time were calculated. In total, 50 participants wore the actigraph throughout both data collection periods, but due to technical and user-related issues, data of only 46 out of the 50 actigraphs were eligible for inclusion in the analyzes.
Mission log
The Norwegian Air Ambulance provided a complete overview of the total work time, missions, and training sessions. Total work time represents the actual amount of time spent on missions and training sessions. The work time of a mission was calculated from when an alarm went off to initiate the operation until the helicopter landed after the operation. The work time generated from a training session was calculated from the start of the session to the time of landing back at the base. The total work time variable applied in the analysis was a combination of the two. The workload variable comprised the mean number of missions and training sessions collapsed. Categorical variables were formed for total work time and workload, based on tertiles in order to examine how different levels of work time affect sleep variables. Night work was defined as missions occurring between 24:00 and 07:00 h, including missions that started before, but ended after midnight. However, a mission that started before 07:00 h but end after that clock time, e.g., 05:00 and ended 08:00 h, was not categorized as a night mission.
Data analyzes
Continuous data are summarized as mean (±SD) for symmetric data, median (quartiles) for non-symmetric data, and categorical variables as numbers; n (%). In order to explore the workers’ sleep during the workweeks and the weeks off work, linear-mixed models (LMM) were applied to generate unbiased estimates of variance (West et al. Citation2014). LMM is a generalization of traditional linear regression models, adjusting for the inner correlation structure in the data that results from multiple observations on the same individual. LMM for the four variables of bedtime, wake-up time, time in bed, and total sleep time as dependent variables were fitted. The four sleep variables were examined for both sleep diary and actigraphy data. Analyzes compared both the sleep patterns between the two workweeks in winter versus summer, and over three consecutive weeks (before work, workweek, and after work) during the winter season and the summer season, separately. Total work time and workload were included as fixed factors in the relevant analyzes, and the medium category was set as the reference (based on tertiles). For the analyzes over three weeks, the second week (workweek) was set as the reference. From these analyzes, regression coefficients (unstandardized b-scores) were reported. Due to skewed residuals for the sleep efficiency and wake after sleep onset variables, a Mann-Whitney U test was applied to examine sleep during the two workweeks (winter vs. summer), and a Friedman ANOVA with Wilcoxon post-hoc test was applied for the data analysis over the three weeks, with Bonferroni correction for multiple testing. For the latter analyzes, z-scores were reported. p-values < .05 were considered statistically significant. The statistical analyzes were conducted using SPSS (version 25).
Missing data
Missing data on the sleep items comprised between 0.0% and 11.9% for the sleep diary, and between 2.4 and 12.5% for actigraphy. Data were marked as missing in the sleep diaries if the workers had forgot to fill out certain columns. Data were marked as missing in the actigraph recordings if the worker had removed the actigraph, or due to technical issues related to the actigraph. Missing data were only calculated for the sleep periods. Complete case analysis with more than 5% missing data introduces bias of unknown direction and magnitude (Dong and Peng Citation2013), and multiple imputation was conducted in order to perform Friedman ANOVA. Ten imputed datasets were generated based on the distribution of the existing data, and results averaged to one value. This was conducted individually per worker for the relevant weeks (workweek for workweek, etc.). Dependent variables included in the imputation were wake after sleep onset and sleep efficiency.
Ethics
The study was conducted in line with the Declaration of Helsinki and was approved by the Regional Committee for Medical and Health Research Ethics of Western Norway (REK-Vest; project no. 2014/593), as well as the Norwegian Social Data Service (NSD). It also followed the ethical standards and methods outlined by Portaluppi et al. (Citation2010). All participants provided written informed consent before participating.
Results
Descriptive statistics
A total of 25 pilots and 25 HCM took part in the study, median (quartiles) age was 43 y (38–48 y), and all, but one, participants were men (98%). The mean (SD) work experience in the HEMS occupation was 9.4 (7.9) y. Forty-five (90%) of the workers reported cohabitation or marriage, and 39 (78%) had children living at home. In all, 20 workers (40%) had a second job with the percentage of full-time employment ranging from 2 to 50%. On the chronotype 14 workers (28%) reported being neither morning nor evening type, 13 (26%) were more morning than evening type, 13 (26%) were more evening than morning type, 4 (8%) were morning type, and 4 (8%) evening type. None of the workers were smokers, while 1 worker (2%) used melatonin as a sleeping aid. In all, 43 workers (90%) rated their physical health as good or very good. The mean (SD) self-reported sleep need (h:min) was 7:12 (0:45).
Workload and total work time
The mean (SD) workload in terms of number of missions during the workweek was 14.5 (7.3), ranging from 4 to 32, in the winter season, and 17.6 (6.3), ranging from 5 to 30, in the summer season. Of these, night work made up 1.8 (1.6) in the winter season, and 1.6 (1.1) in the summer season. A total of 16% (winter season) and 6% (summer season) of the workers performed ≥ 3 nighttime missions. Overall, the mean (SD) total work time spent on missions and trainings sessions during the workweek was 18:41 h (08:41 h) during the winter season, and 25:22 h (09:05 h) during the summer season. The difference between the winter- and summer season was statistically significant for both total work time and workload (both p < .001).
Sleep during the workweek in the winter season compared with the workweek in the summer season
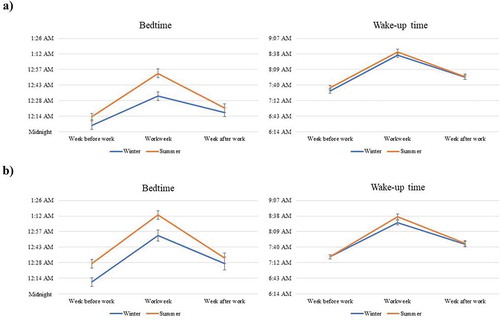
Summary measures for sleep variables derived from the sleep diary and actigraphy are presented in and . Bedtime was significantly later during the workweek in the summer season than in the winter season (sleep diary: p < .001, actigraphy: p < .01; ). Those with higher amount of total work time had later bedtime in the summer season as compared to those with medium amount (sleep diary: b = 0.59, p < .001, actigraphy: b = 0.53, p < .01), but those with lower amounts of total work time did not have later bedtime (sleep diary: b = −0.12, p = .45, actigraphy: b = −0.17, p = .33). Workload did not affect bedtime, neither assessed by sleep diary (lower category: b = −0.22, p = .20, higher category: b = 0.22, p = .27) nor actigraphy (lower category: b = −0.31, p = .10, higher category: b = 0.35, p = .10). According to the sleep diary data only, workers spent less time in bed during the summer as compared to the winter season (p = .03). During summer, those with higher workload spent less time in bed compared to those with medium workload (b = −0.61, p = .02), but not compared to those with lower workload (b = −0.24, p = .31). There was no difference regarding time in bed between the total work time categories (lower category: b = 0.40, p = .07, higher category: b = −0.13, p = .56). In addition, there was no significant difference between the winter season and summer season in terms of wake-up time, wake after sleep onset, sleep efficiency, or total sleep time. [, near here]
Table 1. Descriptive characteristics of sleep variables across three weeks during winter season and summer season
Table 2. Estimates and standard scores for sleep variables between winter season and summer season workweek, and during the week before work, the workweek, and the week after work
Sleep over three weeks during the winter season
Bedtime was significantly later during the workweek, compared to the week before (sleep diary and actigraphy: p < .001) and after work (sleep diary: p = .01, actigraphy: p < .001; ). Wake-up time was later during the workweek, compared to the week before (sleep diary and actigraph: p < .001) and after work (sleep diary and actigraphy: p < .001). Time in bed was longer during the workweek, compared to the week before work (sleep diary: p < .001, actigraphy: p < .01), but only significant for sleep diary after work (p < .001). Wake after sleep onset was higher during the workweek, compared to the week before (sleep diary and actigraphy: p < .001) and after work (sleep diary and actigraphy: p < .01). For actigraphy data only, sleep efficiency was lower during the workweek, compared to the week before (p < .01) and after work (p < .01). Exclusively for sleep diary data, total sleep time was longer during the workweek, compared to the week before (p < .001) and after work (p = .02).
Sleep over three weeks during the summer season
Bedtime was significantly later during the workweek, compared to the week before (sleep diary and actigraphy: p < .001; ) and after work (sleep diary and actigraphy: p < .001). Wake-up time was later during the workweek, compared to the week before (sleep diary and actigraph: p < .001) and after work (sleep diary and actigraphy: p < .001). Time in bed was longer during the workweek, compared to the week before (sleep diary: p < .01, actigraphy: p < .001), but not the week after work. Wake after sleep onset was higher during the workweek, compared to the week before (sleep diary: p < .01, actigraphy: p < .001) and after work (sleep diary: p < .01, actigraphy: p < .001). In line with actigraphy (not sleep diary) data, sleep efficiency was lower during the workweek, compared to the week before (p < .001) and after work (p < .001). There was no significant difference in total sleep time between the three weeks.
Discussion
In the present study, we examined sleep in pilots and HCM, comparing two workweeks, one in the winter and one in the summer season. Additionally, we also investigated sleep over 3 consecutive weeks; the week before work, the workweek, and the week after work, during both seasons.
During the workweeks, workers went to bed later and spent less time in bed in the summer compared to the winter season. Several factors can explain this. The general Norwegian population has been found to be 14% more active during the summer than during the winter season (Hansen et al. Citation2015), which could lead to more accidents and thus more missions and active work hours for the pilots and HCM. Later bedtime and less time in bed could thus be due to missions appearing at late hours, and therefore delay bedtime. This is also reflected by our findings showing a higher prevalence of missions, workload, and total work time during the summer compared to the winter season. More specifically, we found that total work time was positively associated with bedtime. Workload was inversely associated with time in bed. Considering bedtime, previous studies on seasonal change in sleep show mixed results. Some studies have found later bedtime in the winter season (Friborg et al. Citation2012; Hashizaki et al. Citation2018), whereas other corroborate the present findings, showing later bedtime during summer (Garde et al. Citation2014; Quante et al. Citation2019). However, it should be noted the samples of the above-mentioned studies, in contrast to the sample in the current study, were mainly comprised of daytime workers and adolescents. It can be assumed that lack of morning light in the winter as well as evening light exposure in the summer may delay the circadian rhythm (Khalsa et al. Citation2003). Hence, differences in timing of light exposure and latitude may explain the previous conflicting results. As there are large variations in hours of daylight across the country, in both seasons, there could be more pronounced seasonal effects for the workers living and working in areas with particularly reduced or increased hours of daylight. Future studies should therefore explore if the impact of season on sleep is moderated by latitude. In the present study, the latest mean bedtime recorded by actigraphy was 01:13 h during the summer season. Consequently, the overall bedtime is not very late regarding the work setting. Considering seasonal variation related to time in bed, previous studies indicate more time spent in bed during winter, corroborating the present findings (O’Connell et al. Citation2014).
There were some novel findings between the workweek and off weeks (before and after) in both seasons, showing workers delayed the sleep period during both workweeks. As previously discussed, missions in the evening and night can contribute to later bedtimes. One could also speculate that absence of early morning missions could enable the workers to sleep in, explaining this delay. Yet, the evidence suggests there were not many night missions (mean number 1.8 per workweek in the winter season and 1.6 per workweek in the summer season). The social effect of living together with colleagues on the base could also affect sleep habits in the absence of missions and social obligations from the family, where the crew could delay their sleep period similar to what normal daytime workers are able to do on the weekends (Petersen et al. Citation2017).
For both the winter and summer season, longer wake time after sleep onset and lower sleep efficiency were reported during the workweek compared to off weeks. Although the number of night missions was low, the crew still received potential missions and calls that would wake them during the night, thus contributing to more frequent nocturnal awakenings and lower sleep efficiency. Additionally, results from on-call experimental field studies have indicated that wake after sleep onset increases and sleep efficiency decreases in on-call groups, even when calls did not occur, probably because their mere anticipation (i.e., of missions) increased wakefulness (Wuyts et al. Citation2012; Ziebertz et al. Citation2017). Receiving calls that are cancelled and the mere possibility of calls on base could hence explain our results. However, we do not have data on received calls on base. Further, the results for sleep efficiency were found only for actigraphic data; thus, these results must be interpreted with prudence.
Despite delaying the sleep period, experiencing increased wake after sleep onset, and decreased sleep efficiency, the workers reported higher total sleep time during their workweek. This is opposite to what one might expect considering the literature linking shift work to reduced sleep length (Härmä et al. Citation2018; Swanson et al. Citation2011). However, prolonged sleep was only found for the winter season, where the number of missions was lower compared to the summer season. Fewer missions and less daylight could enable the workers to sleep in if early morning missions or calls were absent. This is contrary to previous studies where no difference between seasons was reported regarding sleep duration (Friborg et al. Citation2012; Garde et al. Citation2014), while a literature review of clinical reports concluded mixed results concerning the effect of season on sleep duration (Jay et al. Citation2015). More missions and daylight during the summer season may diminish the difference in sleep length between the workweek and off weeks, which might explain why sleep duration was found to be elevated during the workweek during winter, only. One could further speculate that more missions lead to more rumination, which has been found to explain the association between work stressors and poor sleep in the Dutch HEMS (Radstaak et al. Citation2014). If workers experienced more rumination during their busier summer than winter season, this could explain why the difference between the off weeks and workweek was not evident during the summer season. However, the total amount of sleep the workers obtained in the summer season was 7:03 h, indicating the sleep duration was within normal limits (Hirshkowitz et al. Citation2015). It should also be noted this finding was only evident in the sleep diary data, and the difference in total sleep time between the two workweeks was only 14 min. The self-reported sleep need was 7 h and 12 min. When we analyzed the total sleep time obtained across the 3 weeks in both seasons from the sleep diary (), it was evident the workers obtained the least amount of sleep during the week before work. The workweek and week after work were more alike in terms of total sleep time. Interestingly, the workers slept longer than their self-reported sleep need during the workweek in the winter season. The findings suggest the workweek did not reduce total sleep time, when comparing it to the weeks at home.
The workers increased their time spent in bed during both workweeks, where the difference was more distinct when comparing the workweek to the week at home before work. This supports the finding for sleep duration during the workweek in the winter season. Considering the summer season, spending more time in bed despite no difference between the weeks in terms of sleep length could indicate that the workers were busier and had somewhat more disrupted sleep during the workweek of this season. Nonetheless, they still spent 8 h in bed, sleeping 7 of these during the summer season. The average nocturnal sleep duration for Norwegian men is 6:52 h (Ursin et al. Citation2005), suggesting that adequate amounts of sleep seemed to have been obtained. A previous study comparing Norwegian and Austrian HEMS pilots found that 24% of the Austrian and 71% of Norwegian pilots report using sleep as a mitigating measure against sleepiness, suggesting on-duty Norwegian pilots are better at using sleep facilities when needed (Zakariassen et al. Citation2019). Additionally, 78% of the workers in the present study had children living at home and 40% kept a second job during their weeks off work. Living on the base during the workweek could, therefore, possibly protect against such domestic, social, and work obligations at home. Given the selection criteria (educational and health) required to fulfill the job demands in this occupation, these workers represent a highly selected group. Further, workers also had ~9 y of experience, which could indicate they are tolerant to the demands of this unique occupation and thus be representative of a survival cohort, and as such may serve as a mitigating effect. This, together with well-equipped and separate sleep-facilities, could help preserve sleep despite the potential effect of pending calls and other mission-related activities during the night.
In summary, the HEMS workers seemed to be well adjusted to the work setting despite sleep being affected to some extent. This is in line with other studies suggesting that workers adapt to work settings that require changes in sleeping conditions and location (Bjorvatn et al. Citation2006; Forberg et al. Citation2010). However, one needs to be aware of workers who have short and fragmented sleep. Thus, there is a need in operative occupations for constant development of fatigue risk management systems that may detect and mitigate the risk for these cases. Hence, fatigue risk management systems should continue to develop in order to minimize the potential harm that work schedules and settings pose for the crew and patients’ safety.
Strengths and limitations
Several strengths and limitations of the present study deserve mention. The sample was predominantly male, with only one female participant. This was expected, as the HEMS is a male-dominant occupation. However, one must take caution generalizing the findings to other populations with higher numbers of females. Also, as the crew live and work together during their workweek, it would be also of interest to measure social interaction and its potential effect on sleep. Of all 9 bases in the study, one was located in the north of Norway, while the remaining was located in the south. There are large variations in hours of daylight between north and south, thus potential differences in this regard are unaccounted for in the analyzes. However, as we wanted to examine this occupational group collectively, use of data from all bases was deemed essential. Thus, the results must be interpreted with cation. Another limitation is lack of information about home versus base location, between which there could be variations in daylight, potentially affecting our findings. Further, the findings in the present study could also be influenced by the “healthy worker effect”, as the workers are a cohort who cope well with the shift schedule and are individuals who are not assumed to self-select out of this work setting. Being workers in the air ambulance services, an additional resilience could be present given the choice of the air ambulance work compared to other types of work. The focus of the present study was to investigate how sleep at the group level was influenced by work and free periods as well as season. We acknowledge that in the occupational group studied there might be individual differences in sleep in general and also when it comes to the impact of work and free periods as well as season. Future studies should, therefore, investigate individual differences regarding this. The coherence between sleep diaries and the actigraphic recordings was not always good. There were discrepancies, both minor and major. Compared to the sleep diary data, actigraphy measures were consistently later for bedtime, earlier for wake-up time, and higher for wake after sleep onset and the number of awakenings, and lower for time in bed, total sleep time, and sleep efficiency. Such discrepancies have been reported previously by others (Curtis et al. Citation2019; Matthews et al. Citation2018). The actigraph scores sleep solely based on movement and could, therefore, affect how well it detects sleep and wakefulness. Generally, studies show that actigraphy has reasonably good sensitivity (ability to detect sleep), but rather poor specificity (ability to detect wake) (Sivertsen et al. Citation2006), although this is dependent both on the nature of the hardware and software (interpretative algorithms) used to the derive sleep parameters (Haghayegh et al. Citation2019). The threshold settings could also affect correspondence with diary data, where for the former we applied the default threshold. However, it is difficult to know which parameters, actigraphy or diary, have the largest bias. For this reason, the combination of both can provide valuable insight into sleep and awake periods. Further, the scoring of the actigraphs was based on bedtimes/rise times from the sleep diary data when event marker on the actigraphs were lacking. Although this was done according to guidelines that have been used in previous studies (Biddle et al. Citation2015), one could argue that actigraphy data by this process become less objective. However, the actigraph is still a widely used method for investigation of sleep and can be useful as long as one takes caution when interpreting the findings (Ancoli-Israel et al. Citation2003). The use of both subjective and objective measures is also regarded as a strength, as it provides a more nuanced insight into the workers’ sleep. Further, including objective sleep measures could help compensate for potential response biases in participants’ self-reported measures. Longitudinal data collection over 6 weeks in total represents another asset of the present study, as it enabled an investigation of sleep across several weeks before, during, and after work across two seasons. This field study also provided insight into an occupational group that is challenging to study, which represents an important ad-on to the literature.
Conclusion
The findings indicate a few seasonal differences in sleep, albeit sleep by and large was within normal values during both seasons. Sleep seemed to be somewhat more disrupted, and the workers had lower sleep efficiency, during workweeks than on off weeks according to the actigraph data. However, workers spent more time in bed at work compared to off work periods and even slept more during the workweek compared to off time during the winter season. Despite findings that the work setting affected sleep to some extent, the sleep variables overall suggest workers coped well with the duty schedule. Nevertheless, internal fatigue risk management systems should be continuously evolving in order to detect and handle individual cases of poor sleep that may be hidden by the averages.
Data availability
The data that support the findings of this study are available from the corresponding author, TAF, upon reasonable request.
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- Accident Investigation Board Norway. 2020. Aviation. published reports. Oslo (Norway): Accident Investigation Board Norway; [accessed 2020 May 30]. https://www.aibn.no/Luftfart/Published-reports
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. 2003. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 26(3):342–392. 10.1093/sleep/26.3.342
- Biddle DJ, Robillard R, Hermens DF, Hickie IB, Glozier N. 2015. Accuracy of self-reported sleep parameters compared with actigraphy in young people with mental ill-health. Sleep Health. 1(3):214–220. doi:10.1016/j.sleh.2015.07.006
- Bjerner N, Å H, Swensson Å 1948. Om natt- och skiftarbete (on night and shift work). Stockholm (Sweden): Statens Offentliga Utredningar. Report No: 51.
- Bjorvatn B, Stangenes K, Øyane N, Forberg K, Lowden A, Holsten F, Åkerstedt T. 2006. Subjective and objective measures of adaptation and readaptation to night work on an oil rig in the North Sea. Sleep. 29(6):821–829. doi:10.1093/sleep/29.6.821
- Butler DP, Anwar I, Willett K. 2010. Is it the H or the EMS in HEMS that has an impact on trauma patient mortality? A systematic review of the evidence. Emergency Med J. 27(9):692–701. doi:10.1136/emj.2009.087486
- CamNTech Ltd. 2008. Cambridgeshire (UK). [Accessed 2020 Aug 11]. https://www.camntech.com/
- Chow CM, Wong SN, Shin M, Maddox RG, Feilds K-L, Paxton K, Hawke C, Hazell P, Steinbeck K. 2016. Defining the rest interval associated with the main sleep period in actigraph scoring. Nat Sci Sleep. 8:321. doi:10.2147/NSS.S114969
- Curtis AF, Miller MB, Boissoneault J, Robinson M, Staud R, Berry RB, McCrae CS. 2019. Discrepancies in sleep diary and actigraphy assessments in adults with fibromyalgia: associations with opioid dose and age. J Sleep Res. 28(5):e12746. doi:10.1111/jsr.12746
- Directive 2003/88/EC of the European parliament and of the council of 4 November 2003 concerning certain aspects of the organisation of working time. 2003. Offi J European Union. L299:9–11. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32003L0088
- Dong Y, Peng CYJ. 2013. Principled missing data methods for researchers. SpringerPlus. 2(1):222.10.1186/2193-1801-2-222
- Flaa TA, Harris A, Bjorvatn B, Gundersen H, Zakariassen E, Pallesen S, Waage S. 2019. Sleepiness among personnel in the Norwegian air ambulance service. Int Arch Occup Environ Health. 92(8):1121–1130. doi: 10.1007/s00420-019-10449-w
- Folkard S. 1997. Black times: temporal determinants of transport safety. Accid Anal Prev. 29(4):417–430. 10.1016/S0001-4575(97)00021-3
- Folkard S, Tucker P. 2003. Shift work, safety and productivity. Occup Med (Chic Ill). 53(2):95–101. doi:10.1093/occmed/kqg047
- Forberg K, Waage S, Moen B, Bjorvatn B. 2010. Subjective and objective sleep and sleepiness among tunnel workers in an extreme and isolated environment: 10-h shifts, 21-day working period, at 78 degrees north. Sleep Med. 11(2):185–190. doi:10.1016/j.sleep.2009.07.015
- Friborg O, Bjorvatn B, Amponsah B, Pallesen S. 2012. Associations between seasonal variations in day length (photoperiod), sleep timing, sleep quality and mood: a comparison between Ghana (5) and Norway (69). J Sleep Res. 21(2):176–184. doi:10.1111/j.1365-2869.2011.00982.x
- Garde AH, Hansen ÅM, Persson R, Österberg K, Ørbæk P, Karlson B, Olsen A, Kristiansen J. 2014. Month-to-month variation in sleep among healthy, Scandinavian daytime workers. Scand J Clin Lab Invest. 74(6):527–535. doi:10.3109/00365513.2014.913303
- Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. 2019. Performance comparison of different interpretative algorithms utilized to derive sleep parameters from wrist actigraphy data. Chronobiol Int. 36(12):1752‐1760. doi:10.1080/07420528.2019.1679826
- Hansen BH, Anderssen SA, Steene-Johannessen J, Ekelund U, Nilsen AK, Andersen ID, Dalene KE, Kolle E 2015. Fysisk aktivitet og sedat tid blant voksne og eldre i Norge – nasjonal kartlegging 2014-2015 (Physical activity and sedate time amound adults and elderly in Norway – national survey 2014–2015). Oslo (Norway): Helsedirektoratet. Report No.: IS-2367.
- Härmä M, Karhula K, Puttonen S, Ropponen A, Koskinen A, Ojajärvi A, Kivimäki M. 2018. Shift work with and without night work as a risk factor for fatigue and changes in sleep length: a cohort study with linkage to records on daily working hours. J Sleep Res. 28(3):e12658. doi:10.1111/jsr.12658
- Harrington JM. 2001. Health effects of shift work and extended hours of work. Occup Environ Med. 58(1):68–72. doi:10.1136/oem.58.1.68
- Hashizaki M, Nakajima H, Shiga T, Tsutsumi M, Kume K. 2018. A longitudinal large-scale objective sleep data analysis revealed a seasonal sleep variation in the Japanese population. Chronobiol Int. 35(7):933–945. doi:10.1080/07420528.2018.1443118
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, et al. 2015. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 1(1):40–43. doi:10.1016/j.sleh.2014.12.010.
- Jay SM, Aisbett B, Sprajcer M, Ferguson SA. 2015. Sleeping at work: not all about location, location, location. Sleep Med Rev. 19:59–66.10.1016/j.smrv.2014.04.003
- Kecklund G, Axelsson J. 2016. Health consequences of shift work and insufficient sleep. Bmj. 355:i5210. doi:10.1136/bmj.i5210
- Khalsa SBS, Jewett ME, Cajochen C, Czeisler CA. 2003. A phase response curve to single bright light pulses in human subjects. J Physiol. 549(3):945–952. doi:10.1113/jphysiol.2003.040477
- Litwiller B, Snyder LA, Taylor WD, Steele LM. 2017. The relationship between sleep and work: A meta-analysis. J Appl Psychol. 102(4):682. doi:10.1037/apl0000169
- Luftambulansetjenesten. 2020. 2020 01 Flytid totalt. [accessed 2020 Feb 27]. http://www.luftambulanse.no/system/files/internett-vedlegg/2020_01_flytid_totalt.pdf.
- Manfredini R, Manfredini F, Boari B, Bergami E, Mari E, Gamberini S, Salmi R, Gallerani M. 2009. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am J Emerg Med. 27(9):1097–1103. doi:10.1016/j.ajem.2008.08.009
- Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, Hall MH. 2018. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 4(1):96–103. doi:10.1016/j.sleh.2017.10.011
- Medic G, Wille M, Hemels ME. 2017. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep. 9:151. doi:10.2147/NSS.S134864
- Monk TH, Folkard S. 1992. Making shiftwork tolerable. London(UK): Taylor & Francis.
- Morin CM. 1993. Insomnia: psychological assessment and management. New York (NY): Guilford Press.
- National Air Ambulance Service of Norway. 2015. Annual report 2015. Bodø (Norway). [accessed 2020 May 30]. http://www.luftambulanse.no/system/files/internett-vedlegg/arsrapport_2015.pdf. National Air Ambulance Service of Norway.
- O’Connell SE, Griffiths PL, Clemes SA. 2014. Seasonal variation in physical activity, sedentary behaviour and sleep in a sample of UK adults. Ann Hum Biol. 41(1):1–8. doi:10.3109/03014460.2013.827737
- Petersen H, Kecklund G, D’Onofrio P, Axelsson J, Åkerstedt T. 2017. Thank god it’s Friday–sleep improved. J Sleep Res. 26(5):567–571. doi:10.1111/jsr.12538
- Portaluppi F, Smolensky MH, Touitou Y. 2010. Ethics and methods for biological rhythm research on animals and human beings. Chronobiol Int. 27(9–10):1911–1929. doi:10.3109/07420528.2010.516381
- Quante M, Wang R, Weng J, Kaplan ER, Rueschman M, Taveras EM, Rifas-Shiman SL, Gillman MW, Redline S. 2019. Seasonal and weather variation of sleep and physical activity in 12–14-year-old children. Behav Sleep Med. 17(4):398–410. doi:10.1080/15402002.2017.1376206
- Radstaak M, Geurts SA, Beckers DG, Brosschot JF, Kompier MA. 2014. Work stressors, perseverative cognition and objective sleep quality: A longitudinal study among dutch helicopter emergency medical service (HEMS) pilots. J Occup Health. 56(6):469–477. doi:10.1539/joh.14-0118-OA
- Rhéaume A, Mullen J. 2018. The impact of long work hours and shift work on cognitive errors in nurses. J Nurs Manag. 26(1):26–32. doi:10.1111/jonm.12513
- Rosenwasser AM, Turek FW. 2015. Neurobiology of circadian rhythm regulation. Sleep Med Clin. 10(4):403–412. doi:10.1016/j.jsmc.2015.08.003
- Sadeh A. 2011. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 15(4): 259–267. doi:10.1016/j.smrv.2010.10.001
- Sallinen M, Kecklund G. 2010. Shift work, sleep, and sleepiness—differences between shift schedules and systems. Scand J Work Environ Health. 36(2):121–133. 10.5271/sjweh.2900
- Sallinen M, Laukkanen-Nevala P, Olkinuora A, Puttonen S, Vanttola P, Virkkunen I 2018. Working hours, sleep and alertness in HEMS personnel in Finland. Lecture presented at: Biomedicum Helsinki, Helsinki, Finland.
- Sivertsen B, Omvik S, Havik OE, Pallesen S, Bjorvatn B, Nielsen GH, Straume S, Nordhus IH. 2006. A comparison of actigraphy and polysomnography in older adults treated for chronic primary insomnia. Sleep. 29(10):1353–1358. doi:10.1093/sleep/29.10.1353
- Smolensky MH, Portaluppi F, Manfredini R, Hermida RC, Tiseo R, Sackett-Lundeen LL, Haus EL 2015. Diurnal and twenty-four hour patterning of human diseases: cardiac, vascular, and respiratory diseases, conditions, and syndromes. Sleep Med Rev. 21(3–11). doi:10.1016/j.smrv.2014.07.001
- Stone KL, Ancoli-Israel S. 2011. Actigraphy. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. St. Louis, Missouri: Elsevier Saunders. p. 1668–1675.
- Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. 2011. Sleep disorders and work performance: findings from the 2008 national sleep foundation sleep in America poll. J Sleep Res. 20(3):487–494. doi:10.1111/j.1365-2869.2010.00890.x
- Taylor CB, Stevenson M, Jan S, Liu B, Tall G, Middleton PM, Fitzharris M, Myburgh J. 2011. An investigation into the cost, coverage and activities of helicopter emergency medical services in the state of New South Wales, Australia. Injury. 42(10):1088–1094. doi:10.1016/j.injury.2011.02.013
- Ursin R, Bjorvatn B, Holsten F. 2005. Sleep duration, subjective sleep need, and sleep habits of 40-to 45-year-olds in the Hordaland health study. Sleep. 28(10):1260–1269. 10.1093/sleep/28.10.1260
- West BT, Welch KB, Galecki AT. 2014. Linear mixed models. 2nd ed ed. Arbor (MI): CRC Press.
- Wuyts J, De Valck E, Vandekerckhove M, Pattyn N, Exadaktylos V, Haex B, Maes J, Verbraecken J, Cluydts R. 2012. Effects of pre-sleep simulated on-call instructions on subsequent sleep. Biol Psychol. 91(3):383–388. doi:10.1016/j.biopsycho.2012.09.003
- Zakariassen E, Waage S, Harris A, Gatterbauer-Trischler P, Lang B, Voelckel W, Pallesen S, Bjorvatn B. 2019. Causes and management of sleepiness among pilots iN a Norwegian and an Austrian air ambulance service—a comparative study. Air Med J. 38(1):25–29. doi:10.1016/j.amj.2018.11.002
- Ziebertz CM, Beckers DG, Van Hooff ML, Kompier MA, Geurts SA. 2017. The effect on sleep of being on‐call: an experimental field study. J Sleep Res. 26(6):809–815. doi:10.1111/jsr.12519