Abstract
Existing research suggests the provision of communication aids for children with complex communication needs can have significant positive impacts on health and quality-of-life. The process of clinical decision-making related to the recommendation of high-tech communication aids is not well documented or evaluated, and research evidence related to the provision of these aids remains limited. This study aimed to understand the factors that specialized AAC professionals in the UK consider when recommending high-tech communication aids. Purposive sampling was used to recruit teams to six focus groups, each of which centred on a team’s recent recommendation process (i.e. a discussion following a real-time assessment session, where the team attempted to arrive at an agreed recommendation for a specific child). Thematic network analysis was used to interpret data from the focus group discussions. Participants identified a wide range of child characteristics, access features, and communication aid attributes in weighing up decisions for individual children. Findings suggest that specialized AAC professionals in the UK prioritize access features over language considerations in their communication aid recommendations. An explanatory model was developed to illustrate the interaction effect that several competing considerations may have on decision-making. Implications for clinical practice and future research are discussed.
Children with complex communication needs may benefit from augmentative and alternative communication (AAC) (Ryan et al., Citation2015; Smith, Citation2015), which includes both aided and unaided systems (Murray & Goldbart, Citation2009). Graphic symbol-based systems are often recommended for young children whose literacy skills are still developing (Ryan et al., Citation2015). When successfully matched to the needs of the individual child, one type of aided AAC, high-tech communication aids, can have wide-ranging positive impacts on the development, health, and quality-of-life of children (Bryen, Chung, & Lever, Citation2010). Decisions about high-tech communication aids that are made when children are young can affect their communication ability, language development, social participation, education, and future employment (Milner & Kelly, Citation2009; Smith, Citation2015). However, choosing the most appropriate high-tech communication aid for a child can be challenging for a number of reasons.
AAC practice has evolved over time, with a wider range of children with varying abilities, preferences, and challenges now accessing services (Light & McNaughton, Citation2012). Developing and maintaining professional skills to provide quality services to such a diverse group of children can be difficult. In addition, the range of dedicated and non-dedicated technology available has increased considerably (Light & McNaughton, Citation2012). Professionals need to stay abreast of the latest technology to identify the most appropriate communication aids for children (Van Niekerk, Dada, & Tonsing, Citation2017). An additional challenge in making communication aid recommendations for children is that the system chosen must not only support expressive and receptive communication, but also facilitate the process of language acquisition that is underway. Consideration of how the communication aid will assist the child to engage with the structures of language is critical to realizing linguistic potential (Smith, Citation2015). Increasingly varied child profiles and a wider range of technology and supports to consider, along with the requirement to support multiple needs, makes recommending a communication aid a complex process.
Communication aid recommendations are usually based on processes of collating, sifting, and prioritizing data from a range of sources to identify the best fit of an AAC system for a child and his or her family (Beukelman & Mirenda, Citation2013; Gambrill, Citation2012). The process includes an assessment of the child’s capabilities, preferences, and motivators; an evaluation of the environment; communication partner resources; and progress to date, aiming to identify both current and predicted needs of the child (Beukelman & Mirenda, Citation2013). A process of feature-matching a child’s abilities with the attributes of specific communication aids often underpins recommendations (Van Niekerk et al., Citation2017). The success of communication aid recommendation processes relies, at least in part, on the professional team’s competencies and knowledge to make clinical decisions within the recommendation process. Yet little is known and understood about decision-making processes employed by AAC professionals in recommending communication aids (Baxter, Enderby, Evans, & Judge, Citation2012; McFadd & Wilkinson, Citation2010).
Three recent studies were identified in the international literature that shed light on clinical decision-making processes in communication aid recommendation. In the US, Dietz, Quach, Lund, and McKelvey (Citation2012) conducted semi-structured interviews with 25 Speech-language pathologists (SLPs) (in three groups: generalist, specialist, and research SLPs) to explore their approach to AAC assessment and decision-making. Interview questions focused on both the SLP’s general approach to AAC assessment and a memorable case of their choosing. The authors found differences in the approach and work practices of generalist SLPs and specialist/research SLPs. Generalist SLPs engaged in information gathering processes with a focus on speech and language deficits. Specialist SLPs had a focus on functional communication and motivators to communicate. Specialist SLPs recognized the value of working in teams, but tended to consult other team members on an as needed basis, but typically worked independently. In a follow-up study, eight of the specialist and research SLPs were given case reports and shown videos of two children with different presentations (Lund, Quach, Weissling, McKelvey, & Dietz, Citation2017). In semi-structured interviews, the participants were asked to explain the clinical decisions they would make for these children. The results showed that the specialist SLPs approached the AAC assessment differently for each of the two children; focusing on facilitating language development for the child with cerebral palsy, and on the purposes and motivation to communicate for the child with autism spectrum condition (ASC). Finally, Dada, Murphy, and Tönsing (Citation2017) conducted an online survey of 121 South African SLPs on their perceptions of their AAC prescribing practices. In contrast to the two previous studies (Dietz et al., Citation2012; Lund et al., Citation2017), Dada et al. (Citation2017) reported that most respondents indicated they worked in teams and used a combination of standardized assessment and functional communication tasks to inform their decisions. Research evidence had a limited influence on their choices, whereas available resources and the clinical expertise of colleagues had a strong influence. Respondents indicated that they used ecological inventories, family preferences, and word lists to inform their vocabulary choices; and expressed a preference for more iconic symbols over less iconic symbols.
Across the literature reviewed, no UK study relating to clinical decision-making in communication aid recommendation was identified; the specific service context in the UK is likely to influence research findings. For example, in England, AAC services are provided through a Hub and Spoke model1 commissioned by the National Health Service (NHS). High-tech AAC services are provided to ∼10% of children and adults who need AAC through specialized Hub services, with the majority of people accessing AAC services through the local Spoke services (National Health Service, Citation2018). Children accessing specialized services must meet a range of referral criteria, including the presence of a receptive-expressive language gap, the ability to combine concepts, the need for graphic symbols to communicate through high-tech systems, or the need for a complex access solution to use high-tech (National Health Service, Citation2018). In other parts of the UK, AAC specialized services have referral criteria that enable local practitioners to refer any child with any type of AAC need. To date, there have been no published studies of how teams within the UK arrive at decisions for communication aid recommendation. International studies have primarily focused on single-discipline clinicians (e.g., SLPs) and their role in communication aid recommendation, with limited consideration of team-based decision-making.
Furthermore, prior studies have examined professionals’ reports of their decision-making processes in case studies, but not looked at real-time decision-making in communication aid assessments (Lund et al., Citation2017). The aim of the present study was to identify how characteristics of individual children, as well as access features and attributes of communication aids, might influence specialist team decisions regarding communication aid recommendations. The research question addressed was: What characteristics and attributes related to the child, and high-tech communication aids, do professionals consider important in making decisions about communication aid provision?
Method
Design
This exploratory study utilized an ethnographic, qualitative approach to gain insight into the recurring processes underpinning professionals’ decision-making in communication aid recommendations. It formed part of a more extensive research project exploring clinical decision-making in communication aid recommendation in the UK. Ethical approval was obtained from Manchester Metropolitan University and the relevant NHS Research Ethics Committee (REC reference 6/NW/0165).
Participants
Professional teams
Six teams of professionals were recruited to the study. The managers of designated specialized communication aid services from across the UK were contacted in writing and invited to participate. Purposive sampling was used to ensure the specialized services recruited had different funding structures (e.g., government-funded public services and charitable organizations) and were from across the UK. Inclusion criteria were that participants be (a) professional team members (e.g., Speech and Language Therapists (SLT), occupational therapists (OT)) involved in making a communication aid recommendation for an identified child aged 0–18 years referred to a specialized service; and (b) employed directly by the specialized service or by local services supporting the individual child. All professional team members involved in the clinical decision-making for a particular child were invited to participate, and all gave written consent.
A total of six focus groups were completed and ranged in size from two to 13 participants with a mean of five. While a typical focus group size ranges from five to 10 participants (Barbour, Citation2008), focus group size in the present study was determined by service structure and delivery processes (see ). The focus groups included one specialized team operating a prescription review model of decision-making (Lindsay, Citation2010), where two children were discussed. In this model, representatives from the specialized service conduct a communication aid assessment with the local professional team and the family. At a date following the local assessment process, the specialized team representatives meet with their wider specialized clinical team to discuss their provisional decisions for that child. In this way, the whole specialized team contributed to decision-making. This focus group captured the specialized services consensus in decision-making for two children.
Table 1. Focus group demographics.
Children and families
Purposive sampling was used to recruit the children and families who were the focus of the team discussions about communication aid recommendations. Each participating team of professionals identified families referred to the specialized service for an assessment recommendation. These families were contacted and provided with study information. They were asked to give written consent to their consultation being the focus of discussion. The researchers provided the specialized teams with broad demographic characteristics to support diversity in those invited to take part according to child characteristics. Thus, the purposive sampling of children included a range of profiles in terms of age, sex, medical diagnosis, abilities and challenges, and stage of communication aid use that are eligible for UK specialized services (). The characteristics complemented those discussed in any preceding focus groups.
Table 2. Demographics of the children discussed by focus group participants (all names are pseudonyms).
Procedure
This study used well-established focus group procedures. Focus groups are valuable tools for understanding decision-making processes and are particularly useful when exploring professional practices (Barbour, Citation2008). One appointment within a communication aid assessment acted as the starting point for each focus group discussion. The focus group took place immediately after the appointment. However, the two researchers conducting the focus group were not present during the appointment to reduce the likelihood of the discussions being influenced by their assumptions drawn from observing the appointment. The focus groups were audio recorded and lasted from 45–75 min. These two researchers moderated the discussion using a semi-structured format that included open-ended questions related to decision-making used during the assessment appointment and in practice more generally (see Supplementary Appendix A). Follow-up questions were used for clarification and to encourage more in-depth discussion. The focus groups were transcribed orthographically, and all identifying information was removed. Participants were offered a transcript copy to check at the time of the focus group and in a follow-up email. None of the participants asked to see their transcript.
Data analysis
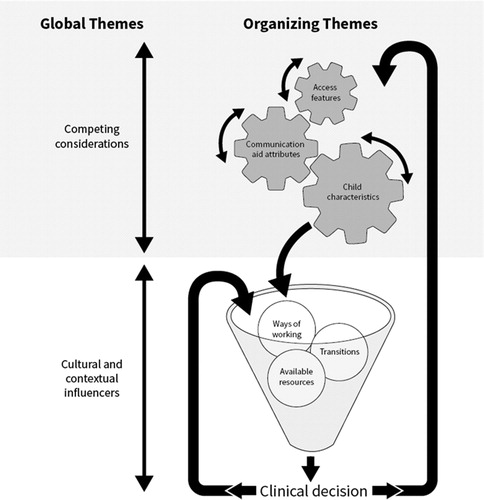
Focus group transcripts were imported into NVIVO10™ software for data management purposes. An inductive thematic analysis (Braun & Clarke, Citation2006) approach to coding was used. Initially, the first and second authors read and re-read the transcripts to gain an overall sense of the data. These two researchers then independently re-read the transcripts, assigning initial codes to meaningful segments of the data to capture their impressions, followed by discussion and some preliminary consensus on coding. Next, core research group members (the first, second, third, fourth, and seventh authors) met to share coding and discuss their reflections on the data. Individual assumptions were discussed and noted. An iterative process of code refinement was undertaken by the first two authors to develop the thematic network, grouping basic codes into meaningful organizing themes and then global themes. Finally, the networks were illustrated with quotes from the data and presented to the wider research group for sense checking and to establish credibility and transferability. In addition, two researchers external to the core research group provided independent coding reliability reviews, to offer impartial input to reduce the impact of researcher bias and assumptions. The NVIVO10™ software provided an audit trail and supported credibility. All organizing themes were coded from the analysis of each focus group transcript, with between 15 and 109 references per organizing theme recorded across the whole data set. In the final stage of analysis, the thematic network of findings addressed the research question (see ).
Table 3. Global themes, organizing themes, and basic codes.
Results
The thematic network was comprised of two global themes and contained six organizing themes and 38 basic codes (). The global themes were Competing Considerations and Cultural and Contextual Influencers. The range of elements within the network is indicative of the myriad of interactive factors considered in communication aid recommendation. The first global theme contained three organizing themes: Child characteristics, Access features, and Communication aid attributes. The second global theme encapsulated three organizing themes: Ways of working, Transitions, and Available resources. This second global theme included cultural and contextual factors outside of the child characteristics, access features, and communication aid attributes that influenced decision-making and captured the influences of work processes and team structures, resources, and the wider social context. To allow adequate discussion of the thematic network, the current study details only the findings related to the first global theme. The second global theme is discussed in detail in the companion paper in this issue (see Lynch et al., Citation2019). In the sections that follow, basic codes are presented alphabetically, but this ordering does not reflect a hierarchy of importance. All names are pseudonyms, and commercial products have been de-identified and labeled as [named software].
Global theme 1: competing considerations
The data reflect that at the heart of communication aid decision-making is the consideration of child characteristics, communication aid attributes, and the need to make tradeoffs prioritizing key communication aid attributes based on individual child characteristics. Furthermore, discussion of access was pervasive, with the term used to conceptualize the interface between the child (e.g., operational competence) and the communication aid (e.g., access methods available). Consequently, the network has three organizing themes: Child characteristics, Access features, and Communication aid attributes.
Child characteristics
Professionals described a wide range of child characteristics that influenced their decision-making, including physical characteristics, intrinsic abilities, and characteristics related to the child’s journey with AAC.
Age
The child’s chronological age was referenced as a way to frame existing or expected progress and to choose the appropriate vocabulary. For example, participants considered the age of the child as a filter to evaluate language and learning development: “So conceptually, Valerie’s really high level and she’s only five” (specialist SLT). For older children, age was considered as a potential indicator of more limited future development with aided AAC: “I don’t know what the expectations are … you know Indie is eighteen she’s got by till now” (specialist OT). Age was also a consideration in choosing the appropriate vocabulary level within a communication aid for Naraah: “Then linguistically, given what her age is, what her language looks like, [named software] set up is really tricky” (specialist SLT).
Assumed abilities
While participants indicated that information regarding the child’s language or cognitive level was important to inform decisions, they also indicated that it was not always available for a variety of reasons. In some cases, the information was not provided by referring agencies, as reported by Naraah’s team: “For those services that don’t have much AAC experience, they’re making referrals and there is no language assessment done” (specialist SLT). For others, obtaining a language or cognitive level was not possible: “And of course, at the moment, it’s very difficult to assess Noel’s cognitive skills, because he has no way of showing you what level [he is] at” (specialist SLT). Where information gaps existed, one specialized team reported using an adapted standardized assessment to assist in determining the level at which a child was functioning. In Naraah’s focus group, a participant reported: “If we do language assessments here, they tend to be based on a standardized framework, but we might adapt it quite heavily” (specialist SLT). More commonly, participants indicated that they used reported information to inform their clinical judgements: “So they [the local team] were saying, they felt Paul understood everything but hadn’t been able to assess that” (specialist SLT). Observations and evaluations from the assessment episode were another source of information:
I had to pretend that a grey felt tip pen was a spoon and Naraah was able to use the device unprompted to navigate to EQUIPMENT and say “spoon” to comment on the fact that I was pretending that the felt pen was a spoon. So, I don’t have any worries about her symbolic representation, even when it’s actually a pen (specialist healthcare scientist).
Similarly, some participants assumed a level of language or cognitive functioning based on reported or observed information. This assumed level of functioning was taken into consideration in their decision-making.
Child’s preference
During three of the assessment appointments, the children involved demonstrated a clear preference for a particular technology. For Owen, the option of having newer technology with more features appeared to influence the team’s decision: “He’s got a communication aid that is very out of date and the battery power was going on it. We found using a new communication aid – he was very much more eager to use it” (specialist SLT). For Paul, the technology was perceived to be motivating. The team discussed how he had demonstrated skills that he had not previously shown when using symbols on an Eye-gaze frame: “Because he would only use eye gaze with technology to interact” (specialist clinical scientist). Finally, Indie’s team raised concerns that her strong interest in technical aspects of the communication aid had the potential to interfere with communication: “I mean the problem being that Indie is just a bit too interested in the operation of the device” (specialist SLT).
Participants either observed children’s preferences during the assessment episode or determined what the preferences were based on what was reported by those around the child. One team used a visual summary of the decision points as a tool to capture the child’s expressed preferences in the decision-making process. The hand-drawn visual outlined Owen’s priorities in what he wanted in his communication aid (e.g., the voice and battery were particular priorities), as well as the priorities of his family and team (e.g., the ability to store messages at school to bring home). The summary allowed consideration of Owen's priorities, along with the rest of the team’s, and helped illustrate who was involved in the decision points leading to a specific recommendation. As Owen’s specialist SLT described “This is me trying to visually represent it to a certain extent for Owen so that he can keep track and we can ask his opinion, and we did sort of get his opinion”.
Communication ability
The children’s existing communication ability was discussed in terms reflecting multimodal communication, as one specialist SLT said: “they don’t really use [aided] AAC at home, but they do use vocalization, some signing, although Noel doesn’t sign”. Participants described unaided communication skills and how these might reduce a child’s inclination to use aided communication (i.e., relying on what is already working and what may be a faster means of communication). For example, a specialist SLT reported that “I think that’s where you were saying about other children in his class; they are having conversations with Mark and understand his eye pointing and his facial expression, so all of that is happening and is working for him”. Participants discussed how the chosen communication aid could support communication skill development. Goals ranged from making self-directed choices to interacting and communicating more, using more communicative functions, and increasing the complexity of expressive output, as noted by a specialist SLT: “I think if Naraah can increase the range of functions that she communicates about”.
Cognitive skills
Most children in this study were perceived to have broadly age-appropriate language skills. However, the participants agreed that additional cognitive issues were likely to impact on the communication aid recommendation. These related to skills often considered under the umbrella term of executive functioning (Murray & Goldbart, Citation2011). Participants referred to difficulties attending to and persevering with tasks, shifting attention from a preferred activity or object to interaction and back again, retaining information (e.g., the location of vocabulary), and distractibility. For example, “Mark is not necessarily retaining those sequences” (local SLT).
Diagnosis
The child’s medical diagnosis as described in the initial referral information appeared to influence participants’ expectations and choices, in that diagnosis-specific characteristics were taken into account within their appointment planning and preparation. The specific characteristics associated with a diagnosis that were considered included physical abilities and physical function, sensory abilities, and reflex responses: “Owen’s condition means that fatigue is a key issue and keeping his energy up … is a real issue for him” (specialist OT).
In some discussions it was apparent that the child’s diagnosis influenced the choice of vocabulary organization and expectations of progress with the recommended communication aid:
… We can read all the research that we like about visual scenes and how potentially important they are for someone with autism … but actually, how are we practically going to use them when Naraah is transitioning to a new environment? (specialist SLT).
Expectations and aspirations
Consideration of potential developmental pathways appeared to shape participants’ decisions. They discussed how they envisioned the children would be communicating in the future, and used this envisioning to guide their present-day decisions. The communication aid recommendation and intervention plans were described as a link or path to the desired communication competence it was felt the child could achieve: “So you think that Valerie will end up using literacy with symbol support, so what’s the bridge to that?” (specialist clinical scientist). This suggested literacy was the desired end goal and the aim of the recommendation would be to support Valerie in becoming literate. Expectations and aspirations appeared to relate to child characteristics (such as cognitive and communication abilities that were assessed or assumed to be at a particular level of functioning) and progress with AAC to date: “If he is cognitively age-appropriate he’ll probably switch to literacy anyway, so [named software] is better” (specialist SLT).
Participants’ expectations and aspirations for the child’s future aided communication abilities were closely linked to the goal for AAC: “My idea is that, when Noel gets into school, he’ll be using the system to interact and to do some of the social stuff with it” (specialist SLT). The goal of AAC varied across the children discussed, and appeared related to child-specific characteristics, including speech skills, cognitive and language skills: “Valerie is definitely a speaking child first, and then I thought maybe she’d use it as a backup but [named software] doesn’t really have enough in there for that” (specialist SLT). Participants discussed different goals for different settings: “So, in school I would see the high-tech being used as mainly an education opportunity for Noel, doing pieces of work, maybe a couple of times a day with his support worker” (specialist SLT). Participants recognized that, in addition to their own expectations and aspirations, the expectations of others involved in the process of decision-making had to be taken into account, and could be an influential factor in relation to the success of communication aid implementation. Participants described the need to manage both limited and overly-optimistic expectations to ensure success: “Before I took Noel over, (the team around the child) were tending to underestimate his abilities, and were just a little bit resistant, to be honest, to me trying higher level things with him” (specialist SLT).
Linguistic level
The linguistic level of the children was discussed in general terms and included the use of the terms “age-appropriate” and “low level”. Consideration of linguistic level appeared to focus on the children’s receptive rather than expressive language skills. Across the focus groups, limited reference was made to formal or informal language assessments, with more reliance on reported and observed linguistic information: “I think receptively Mark is kind of age-appropriate, I would say, there’s probably some [language] concepts which he’s not great on” (specialist SLT). This quote exemplified a recurring feature of the data that it was not entirely clear who was deemed responsible for determining formal language levels at the point of the clinical decision-making recommendation (i.e., the local or specialist SLT). Indeed, participants attempting to determine the child’s language level formally as part of the process of recommendation recognized that it was often less well defined than other aspects of the process for individual children.
Motor abilities
Challenges related to children’s motor abilities reportedly had a substantial influence on the recommendation process: “Noel’s physical impairment has been one of the biggest things that has influenced our choices” (specialist SLT). Participants noted the potential impact of motor challenges on progress and motivation: “His physical challenges make progress slow; it’s taken Mark time to get used to focusing his attention and persevering with a task” (local SLT). These examples suggested motor abilities have broad-ranging influences on decisions related to both communication aid recommendation and implementation. The impact of motor abilities on communication aid access is considered in more detail in the access features organizing theme.
Personality and temperament
Many child personality and temperament factors were considered during the communication aid recommendation process and in vocabulary selection. Personality and temperament characteristics were viewed as having both a positive and negative impact on progress with aided AAC. For some of the children discussed, lack of confidence and frustration were considered to be barriers to progress: “You can see the frustration in Mark, he knows that he knows something, but he can’t get it out, because he can’t access that” (local teaching assistant). Positive emotion also sometimes presented challenges: “He is very excited, trying very hard, but then excitement makes it more difficult for Noel to hunt for words” (specialist SLT). Some positive characteristics were considered significant in a child’s journey, facilitating progress. For example, one participant commented: “He is a very determined little character. … It’s Mark’s way, not in a bad way; he’s actually got very clear ideas on what he wants to do” (local SLT). The need for a communication aid to support the expression of personality traits was also discussed: “Owen is very quick picking up jokes and wanting to have fun with people. He is very eager to communicate with you” (specialist SLT).
Progress and communication opportunities
Participants considered the child’s maturation and development as important considerations and indicated that conducting a more extended assessment process had benefits in allowing skill development over time. For Noel, the recommendation process had taken ∼1 year, and this timeframe was seen as positive, as his specialist SLT explained:
It’s actually been of benefit that it has been a slow process because Noel’s matured and it’s meant that I could work on the side-skills like scanning at the same time while the considerations are happening. So, I think he’s probably developed skills that have helped us make the decision over that time.
Participants referred to the child’s progress to date as being an important consideration in decision-making, specifically in relation to predicting how he or she might use aided communication in the future. As one specialist SLT noted, the rate of progress influenced decision-making: “Valerie learned it quickly; it’s only two weeks of learning”. The child’s progress was also used as an indicator of whether to continue with a particular course of action. It was unclear whether one young boy might benefit from a high-tech system, but his progress over the initial trial period helped to determine whether it was worth continuing: “I’m encouraged by the amount of progress Paul has made in the 8 weeks since that first video” (specialist SLT). Progress being slow also influenced decisions. For Mark, developing literacy was challenging, a factor that was explored as decisions were made about whether to change the graphic representation on his communication aid: “He is learning to read and spell, but I do think it’s a struggle, isn’t it?” (specialist SLT). The decision process centred on whether to switch to less abstract symbols to facilitate progress, or to continue with more abstract symbols, as it was felt the latter might offer him more opportunities should literacy remain a challenge.
Although rate of progress emerged as an important consideration in decision-making, it was weighed against the child’s communication opportunities. For example, Paul had made progress during a trial period with a device, but was not yet meeting the criteria for communication aid funding. The team considered his progress in the context of the opportunities he had experienced, and concluded that an extended loan period was warranted: “ If we’re saying we want to see some spontaneous communication, we’ve got to give him that opportunity to practice using it so that we can see that” (specialist SLT).
In summary, participants considered many child characteristics in their decision-making. They took physical characteristics such as motor abilities and operational competence, age, and medical diagnosis into account. These characteristics were often at the forefront in the decision-making process, as it was recognized that children could not demonstrate their abilities unless a reliable access method could be identified. The participants also considered linguistic level, cognitive abilities, and communication ability, as well as personality traits and temperament. Although they valued information regarding the level of functioning to inform decisions, where functional assessments had not been completed prior to referral, teams sometimes had to rely on assumptions regarding a child’s abilities. Linguistic levels, specifically receptive language and cognitive ability, were factors perceived to influence vocabulary package selection. However, at times, the participants appeared to rely on partial information to infer the ability level of a child within an assessment episode.
A final set of child characteristics in the analytic themes related to the child’s history with AAC before the recommendation. Participants evaluated the child’s progress in light of the communication opportunities the child had experienced and how their skills had developed. They used this information to predict the likely expected rate of progress. Future expectations and aspirations for the child appeared to influence choices concerning language organization and graphic representation in particular.
Access features
Access features considered included the child’s access method as well as mounting of the communication aid and positioning of the child and aid.
Access method
Participants discussed access methods at length for most children. Finding a suitable access method was often regarded as the first consideration in the recommendation process: In Indie’s focus group, one participant noted: “Access is typically where we start”. In Mark’s focus group the need to develop good access skills before focusing on language and communication was discussed: “Until access is sorted, it’s a massive variable which is hard to unpick from the language. If access is really hard, that impacts on motivation” (specialist OT). Some participants also perceived that the child’s access to the communication aid was the more complex part of the recommendation process. As one specialist OT noted, “Indie doesn’t have any challenges with her physical access to technology, which guides the assessment that would usually make it a little bit easier because we are focusing on vocabulary”.
For children with direct access who had difficulty accessing displays with a greater number of symbols, participants considered both software features (e.g., magnifying features) and hardware accessories (e.g., key guards) that were needed to enhance accuracy in using direct access. The availability of software features and hardware accessories influenced the choice of communication aid for these children. Valerie used a software package that had a feature to facilitate her access; however, her team felt that another piece of software might better support her communication abilities – reflecting some tension in the decision-making process. The participants considered whether the access feature could be recreated in software that would be more supportive of her communication development: “If access is the constraint, you could always use a magnify function and have a similar zoom feature, using other software, and have a similar kind of effect” (specialist clinical scientist). For Naraah, the available key guard directly impacted the vocabulary trialled during the appointment episode: “We don’t have the key guard for the vocabulary set that they had trialled. So, we used our closest equivalent to have a look at her access, which we’re all happy with” (specialist healthcare scientist).
Developing good access skills was seen as pivotal. However, some participants highlighted the challenges of providing children with opportunities to develop access skills so they could demonstrate their potential to use high-tech equipment. Receiving input from specialized services in some areas of the UK is predicated on demonstrating an existing level of proficiency with AAC. However, developing skills can be challenging in the absence of opportunities to practice, as one specialist SLT said: “I don’t think we’ve really addressed his communication needs in terms of high-tech. We’re still building up his access, building up his understanding of what he’s doing”. Across all of the focus groups where the children had access challenges, participants faced dilemmas with the tradeoffs required in balancing the demands of access while making sufficient vocabulary available. Professionals indicated that sometimes they had to accept offering the child fewer language functions or less vocabulary to keep access demands manageable, as explained by a specialist SLT:
I got rid of the message window, because if you have a message window then either you have to programme in everything to clear before the next thing is said, or you have to have a clear button, which takes up space on your screen as well, which then makes everything else smaller … If Noel were to totally rely on high-tech then we would be offering him a very complicated layered system with far too many navigations.
Low-tech systems were seen as potentially allowing children to develop linguistic and communication skills with fewer demands: “If Noel had on his low-tech simpler access, fewer physical demands on him and fewer cognitive demands on him, he can cope with more on his selection sets” (specialist SLT). Participants discussed a further tradeoff for Owen, where they had to choose between a smaller communication aid, and his need for larger symbols to support access and vision requirements: “The size of the device was quite nice for him, but the size of the icons on the screen was just too small, and with the question around his vision, it was just teeny [tiny]” (specialist OT).
Mounting and positioning
The need to consider positioning for using a communication aid was highlighted in the focus group discussions. For example, one specialist SLT commented:
Noel has this very nice neck support, which I have seen him using with the eye gaze once. It did keep his head positioned nicely, but either the neck support or the headrest needs to be adapted for [it to work together]. It might have helped him today if he’d had that on.
There was much discussion about supporting children to have access to the communication opportunities they needed while facing access and equipment constraints. There was also discussion about how other equipment and environmental settings affected access. In particular, for children who required their communication aid to be mounted, participants were concerned with the aid being available across different contexts: “I would like to see the device mounted to her powered chair so that Naraah’s got as much opportunity to use it in as many contexts as possible” (specialist healthcare scientist). For Naraah, however, the weight of the preferred communication aid exceeded what could be mounted on her wheelchair, posing a dilemma for the team in balancing preferences with access needs.
In sum, teams identified access as one of the most time-consuming considerations, and said that addressing it was often where the process of communication aid recommendation began. Participants considered a hierarchy of access options and sought to minimize operational demands on the children. There was recognition of the particular importance of low-tech systems to support communication as access skills developed. Considerable focus was also given to positioning the child and the communication aid, and mounting of the aid, to ensure systems were available throughout the day and across settings.
Communication aid attributes
Many aspects of a communication aid itself were taken into account in the focus group discussions, including hardware and software attributes.
Hardware aesthetics
Aesthetic considerations, including the look of the communication aid, were perceived to have an impact on buy-in by Owen: “The device that he’s got is quite old and naff looking (unfashionable), and the new devices do look sleeker” (specialist SLT). The voice quality and ability to control the volume was also taken into account for Owen as he had some concerns about the voice on his current device in terms of: “The volume [was limited] and was very robotic and Americanized. I think it was a mixture of all those three things together, not just one” (specialist SLT).
Hardware reliability
The reliability of the communication aid and the issue of unreliable systems needing repairs was a concern for some participants: as one said “Indie’s aid had frequent hardware issues and needing to be sent back for repair, which would take a long time. Then they’d almost be starting from scratch again, to teach her, when it came back to school” (local SLT). The time taken to repair communication aids appeared to be of particular concern because it interrupted the learning process: “Mark’s joystick was acting up, and that’s fairly typical because you know things can go wrong with machines and repairs always take up a bit of time” (local SLT). The communication aid’s capacity to withstand being dropped or knocked was also a consideration: “Owen worries that he will get into trouble for dropping and breaking it, so we want something that we can reassure him that if it tumbles, it will be okay” (specialist SLT).
Hardware data storage and processing
The device’s memory capacity, ease of storing, and potential to run multimedia files were additional factors to consider for each child: “There’s all these kind of techy things, like … It’s not going to die if you put video clips into it …, which Noel would probably quite enjoy” (specialist SLT).
Software consistency and intuitiveness of design
Participants valued the extent to which software was perceived to be intuitive. More intuitive software was considered to support children to find vocabulary themselves and offer opportunities for independent exploration rather than reliance on intervention to learn the systems: “For Naraah, if it is a bit more intuitive, it’s a bit easier to navigate through” (specialist SLT).
Software ease of editing
Ease of editing was a consideration, and some participants reported that this was the reason why they chose a particular software over another: “For Paul, I went for [named software] in the end. Why did I choose it? It was a lot to do with the editing” (specialist SLT).
A further consideration in the participants’ decision-making was the quantity of editing required. If relatively little editing was likely to be needed, participants indicated they might choose a software package that was less user-friendly from an editing perspective, as long as it was best suited to the child’s needs. However, if a lot of editing was likely to be required, they placed greater weight on consideration of the ease of editing for communication partners. For example, in Noel’s focus group, one specialist SLT reported:
If you want to make a bespoke [customized] layout or tweak a layout, it’s not as user-friendly. It is fine if you use one of their packages straight off the shelf, and personalize it with a person’s name and stuff like that.
Software graphic representation
In the focus group discussions, some consideration was given to the nature of graphic representations within specific communication aids, but there were mixed views on the relative importance of the type of symbols chosen. Symbol type emerged as being important, particularly concerning the potential memory load for children and people supporting them: “Mark is the only child that I am currently working with who is using this symbol set, so I’m rusty, I have to refresh my memory every time” (local SLT).
Other participants reported that the type of graphic representation was a low priority in their decision-making for children who demonstrated good symbolic understanding. These participants indicated that the child they were discussing was in transition across different types of graphic representation systems, and therefore retaining and drawing upon previous learning was not a critical concern: “I have been very aware that we have been mixing-and-matching symbol sets for Noel, but he has managed” (specialist SLT). One aspect of the representational form of graphic symbols that emerged in some discussions was the importance of choosing symbol sets that referenced concepts and ideas in the child’s experience and that included localized UK content. For example, for Owen, a priority was including: “more UK-type words” (specialist SLT). For other participants, choices of symbol systems were limited by local policies, as one Specialist SLT outlined:
I think that [named symbols] might be the best symbol system to start him with … but the speech therapists were very against it, because the local area have a policy where they’ve ranked all the symbol communication systems in order of iconicity, and they’ve put [named symbols] at the bottom, and for that reason they won’t use it in schools.
Software vocabulary
Participants emphasized choosing software that incorporated core vocabulary (i.e., vocabulary that is frequently occurring in spoken language). For example, “They tried [named software] with Naraah because it uses that nice core vocabulary approach” (specialist SLT). There was one exception for a child whose communication aid was intended to augment her spoken output. The priority for her team was identifying software that provided a large fringe vocabulary (i.e., vocabulary that is used less frequently and pertains to specific topics, individuals, or environments) to provide context to her spoken output:
Valerie almost doesn’t need a core vocabulary that much because she uses a lot of gesture and a bit of speech, so you could sort of maybe grasp that bit, but then it’s those more difficult and less predictable words she wouldn’t [be able to convey] (specialist SLT).
In some cases, another consideration was choosing layouts that supported automaticity in locating vocabulary: “Indie is definitely relying on a little bit of motor planning in her organization. When you hit one button and everything changes, you lose that, and we want this to be as fixed as possible” (specialist OT). For some young children, the importance of age-appropriate vocabulary was stressed:
It felt that by looking at Naraah today this [named set up] was slightly more appropriate. The other one does give you an awful lot of extra vocabulary, a large amount of which is not useful for a five-year-old (specialist clinical scientist).
Future vocabulary needs also emerged as an influential factor in deciding current vocabulary choices. In Paul’s focus group, the team expressed a preference for choosing vocabularies where masking vocabulary elements can be used in the early stages, rather than vocabularies where the child progresses through levels: “You are almost better to start them on a higher level and just delete and hide things” (specialist clinical scientist). The rationale given was that masking items of vocabulary in the introductory stages enabled a motor pattern to be learned for retrieval of the visible vocabulary items. As masked items are revealed, the child retains learning gained through established motor patterns, while learning new motor patterns to retrieve the un-masked items.
In summary, participants considered and made tradeoffs across many communication aid attributes. For particular children, specific hardware attributes were prioritized, some of which were considered in relation to the children’s physical characteristics. For example, communication aid size and weight were important for very small children and for children who were ambulatory. Child preferences also influenced which communication aid attributes were given precedence, that is, child priorities about communication aid appearance and voice quality were accommodated in one decision-making process. Reliability and ruggedness became more salient for those teams that had previously experienced communication aid breakdown. Professionals recognized the negative influence on learning and buy-in when communication aids were not available for long periods due to protracted repair processes. There was limited discussion of other hardware attributes (e.g., battery life and additional assistive technology features). The software attributes prioritized reflected both the needs of the child and those providing support. Professionals prioritized consistent layouts, intuitive design, and vocabulary packages to support the child’s current and future needs. Vocabulary package selection was influenced by predicted progress, literacy development expectations, and the intended use of the communication aid. There was limited consideration of the type of vocabulary layout (e.g., semantic-syntactic or pragmatic organization), and of the type of graphic representation. For some professionals, ease of editing for those supporting the child was a key consideration.
To summarize the collective findings, those charged with the responsibility for proposing specific communication aids face a complex task that includes identifying the particular child characteristics, access features, and communication aid attributes that must be considered in their recommendations for each child. These are not separate, fixed components of the decision-making process, but are constantly moving, with some being more fluid and others more stable as teams reach their decisions.
Discussion
This study, the first in the UK to focus on clinical decision-making during real-time recommendation processes, highlights the fundamental complexities in those decisions. AAC practice has evolved over time, with a wider range of children benefiting from communication aid technologies (Light & McNaughton, Citation2012). To reach the point of recommendation, teams work through multiple layers of consideration to identify the best fit of AAC (Beukelman & Mirenda, Citation2013; Smith, Citation2015; Van Niekerk et al., Citation2017). While there is limited research on clinical decision-making in AAC (Baxter et al, Citation2012), that which does exist suggests that specialist and generalist SLPs differ in their focus of AAC enquiry during the decision-making process (e.g., describing language deficits compared with communicative competence) (Dietz et al., Citation2012; Lund et al., Citation2017). To our knowledge, studies have not explored the decisions made when a multi-professional team weighs up the best AAC options for a child immediately following an actual AAC assessment. These findings offer insight into inter-professional dialogue during the AAC decision-making process.
Clinical implications
This study has a number of clinical implications. First, while the children represented a small section of the broader AAC community (as determined by the referral criteria for specialized services), each child discussed had a unique set of abilities, attributes, and resources. This highlighted the individualized nature of the decision-making process in recommending a communication aid. Viewing the findings collectively, the expansive breadth of factors that came into play as team members attempted to reach an agreed recommendation for a specific child highlights the complexity of the process. While related studies have indicated that non-specialist practitioners face challenges in making effective AAC recommendations (Dietz et al., Citation2012), the present study suggests that, even for experienced professionals, the breadth of factors is likely to be challenging (see ). Development of additional resources, such as decision-making supports, or heuristics is warranted.
Second, the study identified different priority considerations for AAC team members than have been reported in previous research. In the present study, professionals prioritized children’s unique physical characteristics and the access features of specific devices in their decision-making. Access was often viewed as the starting point and the most complicated aspect of the recommendation process. These considerations appeared more prominently in the present study, in contrast to Dietz et al. (Citation2012) and Lund et al. (Citation2017), which also described access features as a lesser consideration in thematic networks. Furthermore, findings of our research suggest that there was relatively little focus on the individual’s language and communication abilities, as a factor for consideration. In particular, there was little evidence of a requirement for formal assessment of these abilities, and, instead, there was a tendency to rely on informal observations or assumptions about a child’s intrinsic abilities in these domains. These differences in emphasis may reflect the responsibility that all UK specialized services have to support children with highly complex access issues. Alternatively, it may also reflect the broader range of participants’ professional backgrounds, in that this study incorporated a range of professionals involved in AAC services, not just speech-language therapists. It may also suggest that, in real-time, the factors considered may be different from those reported in hypothetical situations or in retrospective reports where professionals have more opportunity to reflect on their decision-making. This finding further supports the potential value of developing heuristic tools to aid professionals in the challenging task of mapping all relevant domains involved in making appropriate communication aid recommendations.
Third, participants gave prominence to the child’s progress with AAC, in light of the communication opportunities that had been available up to the point of the assessment episode. Therefore, it is critical that the opportunities offered to children in need of AAC are high quality maximizing the child’s chances to demonstrate potential. It is noted that different specialist service referral criteria exist across the countries of the UK; for example, the England and Wales specialized service model referral criteria require that children are able to demonstrate ability with AAC. Therefore, it is important that children who show slower progress in the early stages of their AAC journey, and who do not meet service referral criteria, have access to alternative, appropriate pathways to achieve their potential. Furthermore, the findings suggest that a perceived difficulty in developing access skills can be a significant barrier to language and communication experiences. Our findings suggest that developing access was often deemed to be a precursor to communicative use of an aided system. During the process of developing consistent access, consideration of how to support language and communicative development may merit greater prioritization (Smith, Citation2015). More research is needed to understand developmental trajectories in AAC to better inform system trial periods.
Finally, the communication aid attributes considered by the participants in this study highlight similarities and differences with previous research findings. For example, reliability and ease of editing were important considerations for both the current UK participants and their Canadian counterparts (Lindsay, Citation2010). In contrast, consideration of graphic representational forms seems to differ from those found in a recent South African study (Dada et al., Citation2017). The participants in this UK study favoured more abstract symbols for children with higher cognitive abilities, whereas South African SLTs favoured more iconic symbols that were easier to learn. Across both studies, professionals prioritized selection of core vocabulary. However, the South African SLTs indicated a preference for category-based vocabulary organization, whereas there was limited discussion of layout organization in the present study.
The explanatory model in provides a schematic representation of the complexity of the decision-making process that professionals consider important. Professionals debated the possible combinations of attributes and features that were relevant to individual children until they reached consensus on a prioritized set of communication aid attributes that were the best fit for that child. The label “competing considerations” was chosen for this global theme as it denotes the interaction between child characteristics, access features, and communication aid attributes. The label indicates the need to choose the best fit based on a series of tradeoffs rather than perfect options. In the explanatory model, these competing considerations are illustrated by the cogwheels. The interaction of the elements of the child, access, and communication aid, is shown by the potential of the cogwheels to rotate in both directions, as the team debate and consider issues within the decision and ultimately move towards consensus. The cog-wheel interplay indicates an intensity to the tradeoff between one decision made related to either a characteristic, feature, or attribute and how that instantly impacts on the interlinked cogs which depict the remaining two organizing themes. Once a decision is made about these factors, the decision can be influenced by issues external to the child or the aid. In this study, we found that environmental factors related to both the child’s culture and context and the professional’s work setting influenced decision-making. These cultural and contextual influencers, as visualized by the funnel and its contents, denote factors that further influenced clinical decision-making outside the feature matching process. The role of these cultural and contextualizing influencers are discussed in detail in the companion paper (Lynch et al., Citation2019). Finally, while the model denotes the two global themes, the arrows are indicative of the fluid and iterative process of decision-making.
The findings indicate that the decision-making consensus used by specialist professionals in communication aid recommendation processes are complex and encompass a wide array of child characteristics, access, and aid-attribute factors.
Limitations and future directions
Although the focus groups provided a snapshot of clinical processes in real time, which allowed a concentrated examination of specific decision-making processes, the method may have precluded reflection on how decisions could change over time. In addition, the families at the center of the discussions were excluded to avoid any undue influence on the services they received. Families are core AAC team members and including their perspectives would most likely have provided further insights into the decision-making processes of the team. All but one focus group contained members of more than one profession, and the number and ratio of professional perspectives varied across the focus groups. Had the groups been of a uniform membership, it is possible that different or further themes might have been identified. Finally, the thematic network and explanatory model cannot be considered exhaustive as the themes pertained to particular children with specific characteristics and diagnoses. Each child appeared to have an individualized assessment process, and children with other profiles may have processes that include consideration of additional characteristics, features, and attributes. Further research is warranted to examine the impact of the decision-making process over time, to take account of child and family priorities, and to explore decision-making for children with different profiles. Furthermore, research is warranted to understand the rationale underpinning the decision-making related to communication aid recommendations and how these decisions impact on children’s communication and educational outcomes. Finally, the elements of child, access, and communication aid considered here should not be viewed in isolation from the cultural and contextual influencers that impact upon clinical decision-making (Lynch et al., Citation2019).
Conclusion
This study presents a conceptualization of the interactive effects of the child characteristics, access features, and aid attributes on decision-making in communication aid recommendations. Findings suggest that recommending communication aids is multifaceted, requiring effective interaction between local and specialized services. Identification of all characteristics, features, and attributes as relevant to individual children is complex and results in a unique set of considerations for each child. Furthermore, the findings indicate that teams must make tradeoffs when selecting the most appropriate aid, based on a prioritized set of attributes that are the best fit with the child’s current and predicted needs.
2018-0066_Appendix_for_T_F_March_16.docx
Download MS Word (18.5 KB)Acknowledgements
Our thanks to the I-ASC advisory group, Chris Sherlock, Helen Whittle, and Beata Batorowicz for their input into the study.
Disclosure statement
The authors report no conflicts of interest.
Note
Additional information
Funding
Notes
1 The Hub and Spoke model of AAC service provision was commissioned by NHS England. The “Hubs” are specialized high-tech AAC assessment services whose personnel provide consultative services to children and adults who have especially complex requirements. The Hubs also have a responsibility to support service development for local, or “Spoke”, services that provide assessment and intervention to the majority of people who need AAC. This model does not exist in other parts of the UK.
References
- Barbour, R. (2008). Doing focus groups. London, UK: Sage Publishing.
- Baxter, S., Enderby, P., Evans, P., & Judge, S. (2012). Barriers and facilitators to the use of high-technology augmentative and alternative communication devices: A systematic review and qualitative synthesis. International Journal of Language & Communication Disorders, 47, 115–129. doi:10.1111/j.1460-6984.2011.00090.x
- Beukelman, D., & Mirenda, P. (Eds.). (2013). Augmentative and alternative communication supporting children and adults with complex communication needs (4th ed.). Baltimore, MD: Paul H. Brookes.
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. doi:10.1191/1478088706qp063oa
- Bryen, D., Chung, Y., & Lever, S. (2010). What you might not find in a typical transition plan! Some important lessons from adults who rely on augmentative and alternative communication. Perspectives on Augmentative and Alternative Communication, 19, 32–40. doi:10.1044/aac19.2.32
- Dada, S., Murphy, Y., & Tönsing, K. (2017). Augmentative and alternative communication practices: A descriptive study of the perceptions of South African speech-language therapists. Augmentative and Alternative Communication, 33, 189–200. doi:10.1080/07434618.2017.1375979
- Dietz, A., Quach, W., Lund, S., & McKelvey, M. (2012). AAC assessment and clinical decision-making: The impact of experience. Augmentative and Alternative Communication, 28, 148–159. doi:10.3109/07434618.2012.704521
- Gambrill, E. (2012). Critical thinking in clinical practice: Improving the quality of judgments and decisions (3rd ed.). London, UK: Wiley-Blackwell.
- Light, J., & McNaughton, D. (2012). Supporting the communication, language, and literacy development of children with complex communication needs: State of the science and future research priorities. Assistive Technology, 24, 34–44. doi:10.1080/10400435.2011.648717
- Lindsay, S. (2010). Perceptions of health care workers prescribing augmentative and alternative communication devices to children. Disability and Rehabilitation: Assistive Technology, 5, 209–222. doi:10.3109/17483101003718195
- Lund, S., Quach, W., Weissling, K., McKelvey, M., & Dietz, A. (2017). Assessment with children who need augmentative and alternative communication (AAC): Clinical decisions of AAC specialists. Language, Speech, and Hearing Services in Schools, 48, 56–68. doi:10.1044/2016_LSHSS-15-0086
- Lynch, Y., Murray, J., Moulam, L., Meredith, S., Goldbart, J., Smith, M., … Judge, S. (2019). Decision making in communication aid recommendations in the UK: Cultural and contextual influencers. Augmentative and Alternative Communication,
- McFadd, E., & Wilkinson, K. (2010). Qualitative analysis of decision making by speech-language pathologists in designing aided visual displays. Augmentative and Alternative Communication, 26, 136–147. doi:10.3109/07434618.2010.481089
- Milner, P., & Kelly, B. (2009). Community participation and inclusion: People with disabilities defining their place. Disability and Society, 24, 47–62. doi:10.1080/09687590802535410
- Murray, J., & Goldbart, J. (2009). Augmentative and alternative communication: A review of current issues. Paediatrics and Child Health, 19, 464–468. doi:10.1016/j.paed.2009.05.003
- Murray, J., & Goldbart, J. (2011). Emergence of working memory in children using aided communication. Journal of Assistive Technologies, 5, 213–232. doi:10.1108/17549451111190623
- National Health Service. (2018). Service specifications for complex disability equipment: Communication aids. Retrieved from https://www.england.nhs.uk/commissioning/spec-services/npc-crg/group-d/d01/
- Ryan, S., Shepherd, T., Renzoni, A., Anderson, C., Barber, M., Kingsnorth, S., & Ward, K. (2015). Towards advancing knowledge translation of AAC outcomes research for children and youth with complex communication needs. Augmentative and Alternative Communication, 31, 137–147. doi:10.3109/07434618.2015.1030038
- Smith, M. (2015). Language development of individuals who require aided communication: Reflections on state of the science and future research directions. Augmentative and Alternative Communication, 31, 215–233. doi:10.3109/07434618.2015.1062553
- Van Niekerk, K., Dada, S., & Tonsing, K. (2017). Influences on selection of assistive technology for young children in South Africa: Perspectives from rehabilitation professionals. Disability and Rehabilitation, 41. doi:10.1080/09638288.2017.1416500