?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Preschool children with cerebral palsy (CP) with no or unintelligible speech need augmentative and alternative communication (AAC), but not all children needing AAC have access to it. This study describes the use and perceived benefit of AAC and explores factors associated with receiving AAC interventions. Using a cross-sectional design, we combined parent-reported data with data from the Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP). Communication, speech and hand function was classified according to the Communication Function Classification System (CFCS), Viking Speech Scale (VSS), and Manual Ability Classification System (MACS), accordingly. The need for AAC was defined as Levels III–V on the CFCS, without simultaneous classification at VSS Level I, and/or Levels III–IV on VSS. Parents reported on child- and family-directed AAC interventions using the Habilitation Services Questionnaire. Of the 95 children (42 females) with CP (M = 39.4 months, SD = 10.3), 14 had communication aids. Of the 35 children (31.4%) defined as needing AAC, 11 had been provided with communication aids. Parents of children with a communication aid reported satisfaction with and frequent use of the aid. Children at MACS Level III–V (OR = 3.4, p = .02) or with epilepsy (OR = 8.9, p < .01) were most likely to have received an AAC intervention. The low proportion of children receiving communication aids indicates an unmet need for AAC interventions among preschool children with CP.
Almost all human activity involves communication; hence, communication provides opportunities for activity and participation in the social world, learning activities, and games and play (Goldbart & Marshall, Citation2004; King et al., Citation2014). Children with cerebral palsy (CP) comprise a heterogeneous group with motor impairments ranging from minor to severe, often accompanied by perceptual, cognitive, and communication impairments and epilepsy (Himmelmann et al., Citation2006; Hollung et al., Citation2017; Rosenbaum et al., Citation2007). Based on the predominant neuromotor symptoms, CP is clinically categorized into the spastic (bilateral or unilateral), dyskinetic, and ataxic subtypes (Rosenbaum et al., Citation2007). To describe the motor functioning of a child with CP, the Gross Motor Function Classification System (GMFCS) (Palisano et al., Citation1997) and the Manual Ability Classification System (MACS) (Eliasson et al., Citation2006) are frequently utilized.
More than half of children with CP have a motor speech impairment (Hollung et al., Citation2020; Nordberg et al., Citation2013). These children often have more severe gross motor and manual ability limitations and cognitive impairments than other children with CP; nevertheless, the impairments of speech and communication may restrict their social participation to a larger extent than the motor impairments (Himmelmann et al., Citation2013; Mei et al., Citation2014, Citation2015) and be a risk factor for psychiatric disorders (Bjorgaas et al., Citation2012). To describe children’s communication and speech, classification systems like the Communication Function Classification System (CFCS) and the Viking Speech Scale (VSS) are commonly used (Hidecker et al., Citation2011; Pennington et al., Citation2013).
Children with limited or no intelligible speech can benefit from augmentative and alternative communication (AAC) interventions. Children below school age who communicate with the use of AAC and have motor impairments typically use communication aids such as boards, books, and electronic speech-generating devices with graphic symbols (Beukelman & Light, Citation2020; von Tetzchner & Martinsen, Citation2000).
It is estimated that between 20% and 80% of children with CP have communication impairments and could benefit from AAC training and the use of a communication aid (i.e., the provision of an AAC intervention) (Andersen et al., Citation2010; Chan et al., Citation2005; Creer et al., Citation2016; Pennington et al., Citation2005). AAC gives children a language, provides access to learning, and enables active participation (Batorowicz et al., Citation2018; Murray & Goldbart, Citation2009; von Tetzchner et al., Citation2018). To promote a child’s communication, AAC should be introduced at an early age and available and supported for use during all everyday activities. Moreover, there should be collaboration and interaction between the child, family, and an interdisciplinary team wherein the various contexts of the child’s everyday life are taken into account (Goldbart & Marshall, Citation2004; Joginder Singh et al., Citation2017; McNaughton et al., Citation2008). Not providing AAC to children needing it may hamper their language development (Romski et al., Citation2010). This might, in turn, influence not only language and communication but also functioning in other areas, as deficits in one area might have “cascading effects on numerous domains over development” (D'Souza & Karmiloff‐Smith, Citation2017). Therefore, AAC must be provided to children with no or unintelligible speech.
Previous studies describing children’s use of communication aids found that children tended to use their communication aid more often at school than at home (Cockerill et al., Citation2014; Erickson et al., Citation2017). Reasons for the limited use at home may include the parents being able to understand their child without using the communication aid (Huer et al., Citation2001) or the family wanting to communicate more intimately, intuitively, and rapidly than they felt was possible through the use of a communication aid (McCord & Soto, Citation2004). Despite the increased recognition of the importance of communication in children’s lives, research on communication function and the use of communication aids in children with disabilities is still limited (Hidecker et al., Citation2018).
In Norway, the health care and educational systems are public. All children with CP are offered systematic monitoring through the Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP), a registry that includes clinician-reported data on communication, speech, and cognition (Andersen et al., Citation2022). The NorCP includes over 90% of children with CP in Norway and thus provides a unique overview of the population (Alriksson-Schmidt et al., Citation2020; Andersen et al., Citation2022). Norwegian preschool-aged children who need AAC have a legal right both to get appropriate communication aids and to be taught to use AAC (Barnehageloven, Citation2018, §39). However, even though children with CP are systematically followed and access to AAC is the legal right of those in need, data from the NorCP show that only about half of the Norwegian children with CP receive the AAC interventions they need (Andersen et al., Citation2010, Citation2022). The reasons for this large unmet need are not well documented.
To enable the provision of AAC to all children with CP in need and improve the clinical follow-up of children with CP who use AAC, it is necessary to understand why AAC is provided, which children with CP get access to it, and how AAC interventions are perceived by families. Therefore, this study aimed to (a) investigate whether preschool children with CP who need AAC are provided with AAC interventions; (b) describe the parent-reported benefits and use of AAC aids and training; and (c) explore factors associated with the likelihood of being provided with AAC interventions.
Method
Participants and recruitment
This study is part of a larger cohort study of young children with CP and their parents (Habilitation Trajectories, Interventions and Services for Young Children with Cerebral Palsy; CPHAB) (Kalleson et al., Citation2022). Data collection for the CPHAB study took place from 2012 through 2015. Three inclusion criteria were set for the study, with the first two pertaining to the CPHAB cohort in general and the third being specific to this study. The inclusion criteria were:
Children diagnosed with CP and included in the NorCP by the age of 4 years or below from January 2012 through December 2014.
Parents with sufficient language skills in either Norwegian or English to complete the questionnaires.
Children classified with a CFCS level and/or registered as provided with an AAC intervention.
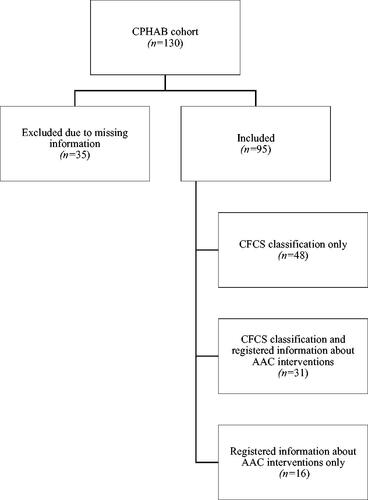
An AAC intervention was defined as a child being provided with AAC training and/or a communication aid and/or parents receiving education through an AAC course. Communication aids included both paper-based aids, such as communication books, and speech-generating devices. Of the 130 children included in the CPHAB cohort, 95 fulfilled the inclusion criteria for this study (see ). CFCS levels were defined for 79 children, information about AAC interventions (but not CFCS) was available for 16 children, and information about both CFCS and AAC interventions was present for 31 children. The 95 included children did not differ significantly from the 35 excluded children with regard to gender and age (see ).
Table 1. Characteristics of 95 children included and 35 children not included in the study.
The study was approved by the Regional Committee for Medical and Health Research Ethics of South-Eastern Norway (#2019/152-3) and the Data Protection Officer of Oslo University Hospital. Approval to use data from the NorCP was granted by its publication board.
The CPHAB study was developed through a close collaboration between a multidisciplinary team of health-care professionals and the Norwegian Cerebral Palsy Association, which is a user organization for persons with CP and their relatives. The user organization is also on the advisory board of the NorCP, and thus, involved in discussions about ongoing and future projects.
Measures and materials
The study included parent-reported data (from a questionnaire) specifically collected through the CPHAB study and clinical data retrieved from the NorCP.
Parent-reported training and use of AAC
The Habilitation Services Questionnaire (HabServ) was developed for the CPHAB study and is freely available in Norwegian and English (Kalleson, Citation2021; Klevberg et al., Citation2017). HabServ includes parent-reported data on several types of services and interventions relevant to children with CP and their families, including (a) provision of AAC training and/or communication aids, (b) perceived benefit of training in AAC, (c) use and type of communication aids, (d) settings where the communication aids were used (at home, in kindergarten, other), (e) frequency/duration of use of the communication aids (less than once a day/1–4 times a week/most of the day), (f) perceived benefit of use of the communication aids, and (g) perceived benefit of parent-directed education in AAC. The parents reported the benefits of the training and use of the communication aids on a five-point Likert scale.
HabServ has been used in several previous studies (Kalleson et al., Citation2020, Citation2022; Klevberg et al., Citation2017; Myrhaug et al., Citation2016; Myrhaug & Østensjø, Citation2014). The face validity of HabServ was assessed by a multidisciplinary expert panel and pilot-tested on 19 parents (Myrhaug & Østensjø, Citation2014).
Background information about the child and family
Data on the children’s CP-related accompanying impairments such as epilepsy and impairments in cognitive functioning and perception were parent-reported and retrieved from HabServ. Information about age, gender, CP subtype, levels of speech, communication, and motor functioning was retrieved from the NorCP and reported by health professionals. The CP subtype was classified according to the Surveillance of Cerebral Palsy in Europe recommendations (Cans, Citation2007). Parts of the Norwegian version of The Parental Account of Children’s Symptoms (Taylor et al., Citation1986) provided information about the parents’ educational background and occupational status.
Classification instruments
The children’s functional classification levels were retrieved from the NorCP. Communication function was classified according to the CFCS, which classifies the child’s daily communication functioning when communicating with known (family and friends) and unknown persons. The CFCS has a five-level scale, where Level I denotes the most efficient communication ability, as described in . The CFCS provides a valid and reliable tool for the classification of the communication performance of children older than 2 years (Hidecker et al., Citation2011; Hidecker et al., Citation2018).
Table 2. Description of Communication Function Classification System and Viking Speech Scale.
The children’s speech was classified according to the VSS. The VSS classifies the way the child normally uses speech on a four-level scale, where Level I is used when speech ability is not affected by motor impairment, as described in . The VSS is validated for children from the age of 4 years (Pennington et al., Citation2013).
Needing AAC was defined as having a communication and/or speech impairment, indicated by classification at Levels III–V on the CFCS, without simultaneous classification at VSS Level I, and/or classification at VSS Levels III–IV. The definition was based on previous studies showing that among children classified at CFCS Levels III–V, a significant proportion (≥54%) have a speech impairment, the minority (23%) communicate using only speech, and AAC is commonly used as either an alternative or a supplement to speech (Hidecker et al., Citation2018; Himmelmann et al., Citation2013).
Manual abilities were classified according to the MACS and Mini-MACS (the Mini-MACS was used for children aged <4 years and the MACS for children aged ≥4 years) (Eliasson et al., Citation2006, Citation2017). The children’s manual ability was rated on a five-level scale, where Level I denotes the least impaired performance. Both the Mini-MACS and MACS classify children’s ability to handle objects in age-relevant everyday activities. The psychometric properties of the Mini-MACS and MACS are considered good to excellent (Eliasson et al., Citation2006; Öhrvall et al., Citation2014). In this study, the term MACS is used for both classification systems.
Gross motor function was classified according to the extended and revised version of the GMFCS (Palisano et al., Citation2008). The GMFCS is rated on a five-level scale, where Level I denotes the least impaired performance. The psychometric properties of GMFCS are considered excellent (Rosenbaum et al., Citation2014).
Statistical analysis
Bivariate analyses using Chi-square tests were performed to assess whether associations were present between AAC interventions (AAC training and/or the use of communication aids) and the child’s age, manual abilities (MACS), cognitive functioning, epilepsy, vision, speech (VSS), and communication functioning (CFCS). A multiple logistic regression model was developed based on the results of the bivariate analyses and implemented to assess the impact of selected factors on the likelihood that parents would report an AAC intervention for the children. The multiple logistic regression model contained three independent variables (age, epilepsy, and MACS). For variables where the parents could respond “don’t know” to a question, this response was added to the missing data and coded as “unknown.” The level of significance was set at p < .05 for all analyses, and data were analyzed using IBM SPSS version 26.
Results
The sample of 95 children (M = 39.4 months, SD = 10.3, range: 15–61) included 42 females (44%). There was an almost equal distribution of children classified as having unilateral CP and bilateral CP. Most children (87%) lived with both their mother and father. Concerning education, a larger proportion of mothers (72%) had more than 12 years of education compared to fathers (49%). As for employment, 80% of fathers were employed compared to 46% of mothers.
The children were classified across all levels of the CFCS, VSS, MACS, and GMFCS. Of the 79 children classified with the CFCS, 36 (46%) were classified at Levels III–V. The proportion of children classified at CFCS Levels III–V was 60% in the age group of 15–24 months, 56% in the age group of 25–36 months, and 36% in the age group of 37–61 months (see ). Of the 95 children, 53 (56%) were classified with both the CFCS and VSS (see ). Among these 53 children, 25 (47%) were classified at CFCS Levels III–V. Three children classified at CFCS Levels III–V were classified at VSS Level I and thus not regarded as needing AAC. Two children classified at CFCS Level II and VSS Level III were regarded as needing AAC. This brings the total number of children in need of AAC to 35 (37%) in our sample of 95 participants (see ).
Figure 2. Children’s need of augmentative and alternative communication (AAC)1 (n = 95), based upon classification on Communication Function Classification System (CFCS) and Viking Speech Scale (VSS), and provision of a communication aid (n = 14). 1Need for AAC was defined as a classification at CFCS Levels III–V without simultaneous classification at VSS Level I, and/or classification at VSS Levels III–IV.
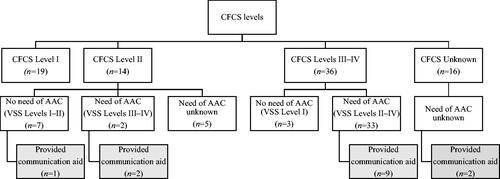
Table 3. Distribution of children classified with Communication Function Classification System (CFCS) in relation to their age.
Table 4. Distribution of children (n = 53) classified with Communication Function Classification System (CFCS) and Viking Speech Scale (VSS), children provided with a communication aid and defined as in need of augmentative and alternative communication (AAC).
The parents of 37 of the 95 participating children reported that their child had taken part in AAC training. The frequency and benefits of AAC training and settings and the frequency of use of communication aids are reported in . Fourteen children (aged 18–57 months) had been provided with at least one communication aid. These 14 children included only four from the group of 24 children who were classified with both the VSS and CFCS and defined as needing AAC. The other 10 were not classified with either the CFCS or VSS (n = 2), only classified with the CFCS (n = 6, of whom five were classified at Levels IV and V and one at Level II), only classified with the VSS (n = 1, classified at Level II), or classified as not needing AAC (n = 1, CFCS Level II and VSS Level I). Overall, 11 of the 35 children (31.4%) defined as needing AAC had been provided with a communication aid (see ).
Table 5. Provision, frequency, setting, and child benefits of AAC interventions.
A Chi-squared test for independence indicated significant associations between receiving an AAC intervention and the children’s manual ability (MACS), presence of epilepsy, and communication function (CFCS; see ). Other characteristics of the child, such as the presence of cognitive or visual impairments, and the parents’ level of education were not associated.
Table 6. Associations between receiving an AAC intervention and characteristics of the child and parent’s education.
The associations between the children’s characteristics and the likelihood of parents reporting an AAC intervention are presented in . The multiple logistic regression model contained three independent variables (age, epilepsy, and MACS). The full model containing all predictors was statistically significant, (3, n = 88) = 22.96, p < .001; this indicated that the model could distinguish between respondents who reported that their children had participated in AAC training and/or received a communication aid and those who did not. As shown in , two of the independent variables made a unique statistically significant contribution to the model (MACS III–V and epilepsy).
Table 7. Association between child characteristics and the likelihood of parents to report receiving an AAC intervention.Table Footnotea
Discussion
In our sample of 95 preschool-aged children with CP, 35 children (37%) were defined as having a communication and/or speech impairment of severity that indicated a need for AAC, a finding that is in line with previous epidemiological studies from Norway (Andersen et al., Citation2010). Children classified as having a speech or communication impairment should be referred for AAC evaluations as early as possible (Hidecker et al., Citation2018). Therefore, the first aim of our study was to determine whether young children with CP and in need of AAC were provided with AAC interventions. In our study, only 11 of the 35 children (31%) defined as needing AAC had been provided with a communication aid. Although these children may have been provided with other forms of AAC, given that the majority of children with CP who need AAC have severe motor impairments and our definition of communication aids included both paper-based and technological aids, it is disturbing that the majority did not have access to aid. These results not only support previous research in Norway showing that approximately half the children with CP in need of AAC did not have access to it (Andersen et al., Citation2010) but also are more serious, indicating an urgent need for more attention to this area in research, education, and clinical practice (Chan et al., Citation2005; Hidecker et al., Citation2018).
Children who need an AAC intervention and do not receive it may get frustrated and experience communication breakdowns. According to Hodge (Citation2007), AAC must be introduced at an early age and used developmentally to improve educational opportunities in life. Furthermore, for children with motor impairments who need AAC, aided language might be regarded as a form of language development (von Tetzchner, Citation2018). Possibly, AAC interventions may not be provided to all children with CP at an early age, as indicated by our results, because parents are reported to focus more on mobility and daily life activities, like eating and dressing, and less on communication (Chiarello et al., Citation2010). A finding from our study supporting this interpretation is that while GMFCS and MACS classifications are missing for just one child, the CFCS classification is missing for 16. This tradition of focusing on motor functioning is challenged by adults with CP who express that participation in life does not depend on being able to walk but on communication (Moll & Cott, Citation2013). Chiarello et al. (Citation2010) and Alghamdi et al. (Citation2017) showed similar findings in their studies of children, reporting that communication functioning made a greater contribution than gross motor function toward explaining participation in social activities.
AAC interventions may also be delayed because parents hope for speech to emerge or find it difficult to accept the need for AAC (Joginder Singh et al., Citation2017; McCord & Soto, Citation2004). However, AAC strategies and communication aids have the potential to not only promote children’s language development (Romski et al., Citation2010) but also improve independence and facilitate the development of social relationships (Johnston et al., Citation2004). For these reasons, it is important to implement an AAC evaluation for children at CFCS Levels II–V at an early age.
The second aim of our study was to describe how parents of children provided with communication aids reported on their use and benefits. An encouraging finding is that nearly all parents of the 14 children who had communication aids reported that the communication aids were used both at home and in kindergarten, as seen in . Moreover, 10 of the parents reported use of the communication aid several times a day, which is more than in previous studies (Angelo, Citation2000; Clarke et al., Citation2007; Cockerill et al., Citation2014; Hidecker, Citation2010; Joginder Singh et al., Citation2017; Jonsson et al., Citation2011; McCord & Soto, Citation2004; von Tetzchner, Citation2018). Furthermore, over 50% of the parents whose children had participated in AAC training or received AAC aid reported this to be of a large or very large benefit for the child. This speaks to the importance of providing information about and training in AAC as part of family-centered interventions (Stadskleiv, Citation2017).
Finally, we explored factors that were associated with being provided an AAC intervention. We found that children classified at MACS Levels III–V or diagnosed with epilepsy were the most likely to have participated in AAC interventions, a finding that complies with previous studies showing an increased risk for communication impairments in children with epilepsy and severe motor impairments (Andersen et al., Citation2010; Hidecker et al., Citation2018; Parkes et al., Citation2010). Finding that children with the most severe challenges were the ones most likely to receive AAC interventions might indicate that clinicians detect and follow up on AAC needs in the part of the CP population with the most debilitating functional impairments, which is encouraging.
Four children had speech not affected by motor disorder (VSS I) yet were classified at CFCS Levels II–V. As their speech was classified as unaffected, we had not defined these children as needing AAC. One of these children was among the 14 who had been provided with a communication aid. The parents of this child, who was close to 3 years of age and did not have very severe motor impairments (GMFCS and MACS levels below III), reported that this was a high-tech aid that was used several times a day and that they themselves had received AAC training. The parents reported both the communication aid and the AAC training to be highly beneficial.
This case serves as a reminder that communication impairment in children with CP is not only associated with severe motor impairments. Cognition is also an important factor associated with language impairment in children with CP (Mei et al., Citation2016). Additionally, although motor speech impairments are explained by the degree of general motor limitations, there is no one-to-one relationship between cognitive and motor functioning in children with CP (Geytenbeek, Citation2016; Stadskleiv, Citation2020). Intellectual disability is found in children with unilateral CP who most commonly do not need AAC (Andersen et al., Citation2008; Himmelmann et al., Citation2006; Stadskleiv et al., Citation2018), and more severe speech impairment correlates with more severe intellectual disability (Påhlman et al., Citation2019). Therefore, it was somewhat surprising that cognitive impairment was not among the factors associated with the provision of AAC interventions. A possible reason is that the presence of epilepsy and cognitive impairment are highly associated in children with CP (Ballester-Plané et al., Citation2018; Sigurdardottir et al., Citation2008), which might have statistically masked the effect. Furthermore, knowledge of this increased risk, wherein the presence of epilepsy serves as an indicator of possible cognitive challenges, combined with knowledge about the correlation between speech and motor functioning (Andersen et al., Citation2010) may prompt clinicians to instigate AAC interventions for this group of children with CP. However, it is also possible that cognitive impairments are not sufficiently addressed, especially at young ages. This interpretation is supported by our finding that cognitive functioning was reported as unknown by as many as 36% of the parents. This implies that the need for AAC might be overlooked if the child does not have severe motor impairments or epilepsy but has cognitive challenges.
Another surprising finding was that the degree of speech impairment was not associated with receiving an AAC intervention. A simple classification of speech functioning could be expected to be a very useful indicator of the need for AAC. However, speech functioning in children with CP correlates with both motor and communicative functioning (Choi et al., Citation2018) and this was the classification instrument with the most missing data in our study, which might explain why speech did not make a unique contribution.
Clinical implications
Data for this study came from participants aged 15 months to 5 years and were collected between 2012 and 2015 for the birth years 2008 through 2013. The material was thus collected a few years ago. However, the findings of this study, that only 31% of preschool-aged children needing AAC have access to a communication aid, are still highly relevant. One of the quality indicators of the NorCP is the number of children classified at VSS Levels III and IV who are using AAC. In 2021, this was only 53% (245 out of 458 children), including both preschool-aged children and children of school age (Andersen et al., Citation2022; NorCP, Citation2021). Taken together, our study and these more recent national registry data reflect an urgent need to focus more on communication and the need for AAC in the CP follow-up programs in which the children participate.
In particular, this study highlights the need to be aware of possible communication impairments in children with less severe motor impairments. This might be of particular importance when the child presents with comorbid disorders, such as intellectual disability, epilepsy, autism spectrum disorders, and psychiatric disorders (Bjorgaas et al., Citation2012; Mei et al., Citation2020; Påhlman et al., Citation2019); however, the study also has implications for practice regarding children with more complex motor impairments. The observed several instances of data being reported as unknown or missing may indicate that despite being part of a national surveillance registry, children may not always receive an adequate multidisciplinary assessment during the preschool years. This might be because assessing and untangling diagnoses such as sensory impairments, intellectual disability, language and communication impairments, and autism spectrum disorders might be perceived as particularly challenging when children also have severe motor impairments (Christensen et al., 2014; Geytenbeek et al., Citation2010; Stadskleiv, Citation2020). Nevertheless, such assessments of a child’s functioning are necessary to provide individually tailored AAC interventions (Beukelman & Light, Citation2020; Lynch et al., Citation2019; von Tetzchner & Martinsen, Citation2000).
Limitations and future directions
The purpose of this study was to investigate the early provision of AAC to children with CP who were identified as having suboptimal speech and communicative functioning. Therefore, the inclusion criteria specified that the children should be below 4 years of age at the time of inclusion in the NorCP. While the CFCS has been validated for children as young as 2 years, the VSS is validated for children from 4 years of age. Lacking a validated tool for the easy classification of speech in children under 4 years of age is a methodological limitation. In clinical practice, this seems to be less of a concern. Twenty-two of the 63 children classified with the VSS by the clinicians reporting data to the NorCP were younger than 4 years at the time of classification. This finding suggests that clinicians find it meaningful to describe a child’s speech with the four levels of the VSS also before the age of 4 years, which is not surprising given that children typically start using speech in the first half of their second year of life (Clark, Citation2016).
Among the 14 children who had been provided with a communication aid, five had been classified with both the CFCS and VSS; four of these five were classified as needing AAC and one as not needing AAC. Among the nine of the 14 not yet classified with both the CFCS and the VSS, six had been classified with only CFCS. One probable cause for the lack of VSS classification for three of the six participants is young age, as they were 18, 25, and 38 months (see Lillehaug, Citation2020). However, even if the children had not been formally classified with the VSS, the clinicians still must have evaluated their current speech and probable speech development and found it to be of concern, given that they had all been provided with a communication aid. The finding that one of the 14 participants provided with a communication aid was younger than 2 years (i.e., below the age that the CFCS is validated for) suggests that in some cases, the evaluation of a need for AAC precedes formal classification and that at least some clinicians acknowledge the need to provide communication aids at the earliest age possible (Romski et al., Citation2015).
Another factor that might have contributed to missing data on the VSS is that it was not published until 2013 (see Pennington et al., Citation2013). Although it was available for clinical use before that time, it might not have been as well known as the CFCS. Recent data from the NorCP support this interpretation, as 95% of children with CP in the registry are now classified with the VSS (Andersen et al., Citation2022).
This study is based on parental reports of received services and devices, which might potentially pose a risk of bias. The children may have been provided with some form of AAC in the kindergartens that the parents were not aware of. We would argue that the extent of these interventions is most probably limited, as parents would have to sign a written consent form if any personalized communication aid for a child is applied for (Folketrygdloven, 1997, §10–17).
The relatively small sample size limited the possibility of using some statistical analyses such as multinominal logistic regression, which would have more specifically pointed to other variables that could predict AAC intervention. Missing data in key areas, such as cognitive functioning, also limited the variables that could be explored. The included classification instruments did not account for language comprehension or cognition (Rosenbaum et al., Citation2014); therefore, we lacked information about the child’s functioning in these areas. The family’s socioeconomic status was also unknown; however, this factor should not impact service provision in Norway, as interventions and communication aids are provided free of charge for all children with an identified need (Alriksson-Schmidt et al., Citation2021). The finding that the parents’ level of education did not predict the provision of AAC interventions strengthens this assumption.
Another limitation of this study is the exclusion of parents with a non-Norwegian- or non-English-speaking background. A larger sample size that better represents and describes cultural and sociodemographic variability, as well as a wider spectrum of variables, should be considered in future research. Furthermore, we recommend that future studies should include a wider exploration of contextual factors, such as the economical and professional resources available in healthcare services and the qualifications of relevant professionals.
Conclusion
This study documents a large unmet need for the provision of communication aids and AAC interventions to young children with CP. The findings suggest that at an early age, the need for AAC might be overlooked in children with CP who have milder motor impairments and do not have epilepsy but possibly have undocumented cognitive challenges. Since early interventions are important for providing access to language, it seems imperative not to delay the introduction of AAC in this group. Further studies that follow the children over time are necessary to ascertain if the need for AAC is being met. The children who are provided with AAC interventions need them. Finding that parents reported the interventions to be beneficial and that communication aids were used several times a day and in multiple arenas is promising for the communicative development of the children.
Author contributions
The authors would like to thank the families participating in the Habilitation Trajectories, Interventions and Services for Young Children with Cerebral Palsy (CPHAB) registry.
The study was conducted as part of Lillehaug’s master’s thesis at Oslo Metropolitan University. The CPHAB study was funded by the Sophies Minde Foundation, an NGO funding research and activities pertaining to movement disorders. Klevberg and Stadskleiv are employed at the NorCP as part of their employment at Oslo University Hospital. The authors do not have any financial or non-financial conflicts of interest.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Alghamdi, M. S., Chiarello, L. A., Palisano, R. J., & McCoy, S. W. (2017). Understanding participation of children with cerebral palsy in family and recreational activities. Research in Developmental Disabilities, 69, 96–104. doi:10.1016/j.ridd.2017.07.006
- Alriksson-Schmidt, A. I., Jeglinsky, I., Jonsdottir, G., Kedir Seid, A., Klevberg, G., Buschmann, E., & Jahnsen, R. (2021). Living life with cerebral palsy? A description of the social safety nets for individuals with cerebral palsy in the Nordic countries. Scandinavian Journal of Public Health, 49(6), 653–665. doi:10.1177/1403494820974564
- Alriksson-Schmidt, A. I., Jeglinsky-Kankainen, I. F., Jahnsen, R. B., Hollung, S. J., Andersen, G. L., & Hägglund, G. V. (2020). Flaunting our assets. Making the most of the Nordic registry goldmine: Cerebral palsy as an example. Scandinavian Journal of Public Health, 48(1), 113–118. doi:10.1177/1403494819829338
- Andersen, G. L., Hollung, S. J., Klevberg, G. L., Kløve, N., Jahnsen, R., Stadskleiv, K. (2022). Norsk kvalitets- og oppfølgingsregister for cerebral parese (NorCP). Årsrapport for 2021 med plan for forbedringstiltak. [Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP). Annual report for 2021 with improvement measures]. Vestfold Hospital Trust. https://www.siv.no/seksjon/CP-registeret_/Documents/Arsrapporter/NorCP%202021%20%C3%85rsrapport.pdf
- Andersen, G. L., Irgens, L. M., Haagaas, I., Skranes, J. S., Meberg, A. E., & Vik, T. (2008). Cerebral palsy in Norway: Prevalence, subtypes and severity. European Journal of Paediatric Neurology, 12(1), 4–13. doi:10.1016/j.ejpn.2007.05.001
- Andersen, G., Mjøen, T. R., & Vik, T. (2010). Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: A registry-based study in Norway. Perspectives on Augmentative and Alternative Communication, 19(1), 12–20. doi:10.1044/aac19.1.12
- Angelo, D. (2000). Impact of augmentative and alternative communication devices on families. Augmentative and Alternative Communication, 16(1), 37–47. doi:10.1080/07434610012331278894
- Ballester-Plané, J., Laporta-Hoyos, O., Macaya, A., Póo, P., Meléndez-Plumed, M., Toro-Tamargo, E., Gimeno, F., Narberhaus, A., Segarra, D., & Pueyo, R. (2018). Cognitive functioning in dyskinetic cerebral palsy: Its relation to motor function, communication and epilepsy. European Journal of Paediatric Neurology, 22(1), 102–112. doi:10.1016/j.ejpn.2017.10.006
- Barnehageloven. (2018). [The Kindergarten Act] Lov om barnehager (LOV-2005-06-17-64). Lovdata. https://lovdata.no/dokument/NL/lov/2005-06-17-64?q=barnehageloven
- Batorowicz, B., Stadskleiv, K., Renner, G., Sandberg, A. D., & von Tetzchner, S. (2018). Assessment of aided language comprehension and use in children and adolescents with severe speech and motor impairments. Augmentative and Alternative Communication, 34(1), 54–67. doi:10.1080/07434618.2017.1420689
- Beukelman, D. R., & Light, J. C. (2020). Augmentative and alternative communication: Supporting children and adults with complex communication needs (5th ed.). Brookes Publishing Company.
- Bjorgaas, H. M., Hysing, M., & Elgen, I. B. (2012). Psychiatric disorders among children with cerebral palsy at school starting age. Research in Developmental Disabilities, 33(4), 1287–1293. doi:10.1016/j.ridd.2012.02.024
- Cans, C. (2007). Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers. Developmental Medicine & Child Neurology, 42(12), 816–824. doi:10.1111/j.1469-8749.2000.tb00695.x
- Chan, H., Lau, P., Fong, K., Poon, D., & Lam, C. (2005). Neuroimpairment, activity limitation, and participation restriction among children with cerebral palsy in Hong Kong. Hong Kong Medical Journal, 11(5), 342–350.
- Chiarello, L. A., Palisano, R. J., Maggs, J. M., Orlin, M. N., Almasri, N., Kang, L.-J., & Chang, H.-J. (2010). Family priorities for activity and participation of children and youth with cerebral palsy. Physical Therapy, 90(9), 1254–1264. doi:10.2522/ptj.20090388
- Choi, J. Y., Park, J., Choi, Y. S., Goh, Y-r., & Park, E. S. (2018). Functional communication profiles in children with cerebral palsy in relation to gross motor function and manual and intellectual ability. Yonsei Medical Journal, 59(5), 677–685. doi:10.3349/ymj.2018.59.5.677
- Christensen, D., Van Naarden Braun, K., Doernberg, N. S., Maenner, M. J., Arneson, C. L., Durkin, M. S., Benedict, R. E., Kirby, R. S., Wingate, M. S., Fitzgerald, R., & Yeargin-Allsopp, M. (2014). Prevalence of cerebral palsy, co‐occurring autism spectrum disorders, and motor functioning–Autism and Developmental Disabilities Monitoring Network, USA, 2008. Developmental Medicine and Child Neurology, 56(1), 59–65. doi:10.1111/dmcn.12268
- Clark, E. V. (2016). Language in children (1st ed.). Routledge.
- Clarke, M., Donlan, C., Lister, C., Wright, J., Newton, C., & Cherguit, J. (2007). The provision of communication aids to children in England: An analysis of applications to the Communication Aids Project. Child: Care, Health and Development, 33(5), 569–575. doi:10.1111/j.1365-2214.2006.00712.x
- Cockerill, H., Elbourne, D., Allen, E., Scrutton, D., Will, E., McNee, A., Fairhurst, C., & Baird, G. (2014). Speech, communication and use of augmentative communication in young people with cerebral palsy: The SH & PE population study. Child: Care, Health and Development, 40(2), 149–157. doi:10.1111/cch.12066
- Creer, S., Enderby, P., Judge, S., & John, A. (2016). Prevalence of people who could benefit from augmentative and alternative communication (AAC) in the UK: Determining the need. International Journal of Language & Communication Disorders, 51(6), 639–653. doi:10.1111/1460-6984.12235
- D'Souza, H., & Karmiloff‐Smith, A. (2017). Neurodevelopmental disorders. Cognitive Science, 8(1–2), e1398. doi:10.1002/wcs.1398
- Eliasson, A. C., Ullenhag, A., Wahlström, U., & Krumlinde‐Sundholm, L. (2017). Mini‐MACS: Development of the manual ability classification system for children younger than 4 years of age with signs of cerebral palsy. Developmental Medicine and Child Neurology, 59(1), 72–78. doi:10.1111/dmcn.13162
- Eliasson, A.-C., Krumlinde-Sundholm, L., Rösblad, B., Beckung, E., Arner, M., Öhrvall, A.-M., & Rosenbaum, P. (2006). The manual ability classification system (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Developmental Medicine and Child Neurology, 48(7), 549–554. doi:10.1017/S0012162206001162
- Erickson, K., Geist, L., & Hatch, P. (2017). AAC Buy-In at Home: Carefully assessing how a device can meet communication needs is key to promoting its use with a client’s family and friends. The ASHA Leader, 22(2), 46–51. doi:10.1044/leader.FTR1.22022017.46
- Folketrygdloven. (1997). [National Insurancey Act] Lov om folketrygd (LOV-1997-02-28-19). Lovdata. https://lovdata.no/dokument/NL/lov/1997-02-28-19?q=folketrygd
- Geytenbeek, J. (2016). Differentiating between language domains, cognition, and communication in children with cerebral palsy. Developmental Medicine & Child Neurology, 58(6), e536–536. doi:10.1111/dmcn.12990
- Geytenbeek, J. J. M., Harlaar, L., Stam, M., Ket, H., Becher, J. G., Oostrom, K., & Vermeulen, R. J. (2010). Utility of language comprehension tests for unintelligible or non‐speaking children with cerebral palsy: A systematic review. Developmental Medicine & Child Neurology, 52(12), e267–e277. doi:10.1111/j.1469-8749.2010.03833.x
- Goldbart, J., & Marshall, J. (2004). Pushes and pulls on the parents of children who use AAC. Augmentative and Alternative Communication, 20(4), 194–208. doi:10.1080/07434610400010960
- Hidecker, M. J. C. (2010). AAC use by young children at home. Perspectives on Augmentative and Alternative Communication, 19(1), 5–11. doi:10.1044/aac19.1.5
- Hidecker, M. J. C., Paneth, N., Rosenbaum, P. L., Kent, R. D., Lillie, J., Eulenberg, J. B., Chester, K., Johnson, B., Michalsen, L., Evatt, M., & Taylor, K. (2011). Developing and validating the communication function classification system for individuals with cerebral palsy. Developmental Medicine and Child Neurology, 53(8), 704–710. doi:10.1111/j.1469-8749.2011.03996.x|
- Hidecker, M. J. C., Slaughter, J., Abeysekara, P., Ho, N. T., Dodge, N., Hurvitz, E. A., Workinger, M. S., Kent, R. D., Rosenbaum, P., Lenski, M., Vanderbeek, S. B., DeRoos, S., & Paneth, N. (2018). Early predictors and correlates of communication function in children with cerebral palsy. Journal of Child Neurology, 33(4), 275–285. doi:10.1177/0883073817754006
- Himmelmann, K., Beckung, E., Hagberg, G., & Uvebrant, P. (2006). Gross and fine motor function and accompanying impairments in cerebral palsy. Developmental Medicine and Child Neurology, 48(6), 417–423. doi:10.1017/S0012162206000922
- Himmelmann, K., Lindh, K., & Hidecker, M. J. C. (2013). Communication ability in cerebral palsy: A study from the CP register of western Sweden. European Journal of Paediatric Neurology, 17(6), 568–574. doi:10.1016/j.ejpn.2013.04.005
- Hodge, S. (2007). Why is the potential of augmentative and alternative communication not being realized? Exploring the experiences of people who use communication aids. Disability & Society, 22(5), 457–471. doi:10.1080/09687590701427552
- Hollung, S. J., Bakken, I. J., Vik, T., Lydersen, S., Wiik, R., Aaberg, K. M., & Andersen, G. L. (2020). Comorbidities in cerebral palsy: A patient registry study. Developmental Medicine and Child Neurology, 62(1), 97–103. doi:10.1111/dmcn.14307
- Hollung, S. J., Vik, T., Wiik, R., Bakken, I. J., & Andersen, G. L. (2017). Completeness and correctness of cerebral palsy diagnoses in two health registers: Implications for estimating prevalence. Developmental Medicine and Child Neurology, 59(4), 402–406. doi:10.1111/dmcn.13341
- Huer, M. B., Parette, H. P., Jr., & Saenz, T. I. (2001). Conversations with Mexican Americans regarding children with disabilities and augmentative and alternative communication. Communication Disorders Quarterly, 22(4), 197–206. doi:10.1177/152574010102200405
- Joginder Singh, S., Hussein, N. H., Mustaffa Kamal, R., & Hassan, F. H. (2017). Reflections of Malaysian parents of children with developmental disabilities on their experiences with AAC. Augmentative and Alternative Communication, 33(2), 110–120. doi:10.1080/07434618.2017.1309457
- Johnston, S. S., Reichle, J., & Evans, J. (2004). Supporting augmentative and alternative communication use by beginning communicators with severe disabilities. American Journal of Speech-Language Pathology, 13(1), 20–30. doi:10.1044/1058-0360(2004/004)
- Jonsson, A., Kristoffersson, L., Ferm, U., & Thunberg, G. (2011). The ComAlong communication boards: Parents’ use and experiences of aided language stimulation. Augmentative and Alternative Communication, 27(2), 103–116. doi:10.3109/07434618.2011.580780
- Kalleson, R. (2021). Facets of life in families caring for a young child with cerebral palsy. A longitudinal cohort study exploring parental empowerment, child participation in real-life activities and services received by the families. (Publication No. 11250/2833012/A-21-31) [Doctoral dissertation]. Oslo Metropolitan University. https://oda.oslomet.no/oda-xmlui/bitstream/handle/11250/2833012/A-21-31-avhandling-Kalleson-publisert.pdf?sequence=1&isAllowed=y
- Kalleson, R., Jahnsen, R., & Østensjø, S. (2020). Empowerment in families raising a child with cerebral palsy during early childhood: Associations with child, family, and service characteristics. Child: Care, Health and Development, 46(1), 19–27. doi:10.1111/cch.12716
- Kalleson, R., Jahnsen, R., & Østensjø, S. (2022). Comprehensiveness, coordination and continuity in services provided to young children with cerebral palsy and their families in Norway. Child Care in Practice, 28(4), 610–624. doi:10.1080/13575279.2021.1898934
- King, G., Batorowicz, B., Rigby, P., McMain-Klein, M., Thompson, L., & Pinto, M. (2014). Development of a measure to assess youth self-reported experiences of activity settings (SEAS). International Journal of Disability, Development and Education, 61(1), 44–66. doi:10.1080/1034912X.2014.878542
- Klevberg, G. L., Østensjø, S., Elkjær, S., Kjeken, I., & Jahnsen, R. B. (2017). Hand function in young children with cerebral palsy: Current practice and parent-reported benefits. Physical & Occupational Therapy in Pediatrics, 37(2), 222–237. doi:10.3109/01942638.2016.1158221
- Lillehaug, H. A. (2020). Kommunikasjonsferdigheter og bruk av kommunikasjonshjelpemidler hos førskolebarn med cerebral parese. En populasjonsbasert tverrsnittsundersøkelse. [Communicative skills and use of communication aids in preschool-aged children with cerebral palsy. A population-based cross-sectional study]. [Master theis]. Oslo Metropolitan University.
- Lynch, Y., Murray, J., Moulam, L., Meredith, S., Goldbart, J., Smith, M., Batorowicz, B., Randall, N., & Judge, S. (2019). Decision-making in communication aid recommendations in the UK: Cultural and contextual influencers. Augmentative and Alternative Communication, 35(3), 180–192. doi:10.1080/07434618.2019.1599066
- McCord, M. S., & Soto, G. (2004). Perceptions of AAC: An ethnographic investigation of Mexican-American families. Augmentative and Alternative Communication, 20(4), 209–227. doi:10.1080/07434610400005648
- McNaughton, D., Rackensperger, T., Benedek-Wood, E., Krezman, C., Williams, M. B., & Light, J. (2008). A child needs to be given a chance to succeed”: Parents of individuals who use AAC describe the benefits and challenges of learning AAC technologies. Augmentative and Alternative Communication, 24(1), 43–55. doi:10.1080/07434610701421007
- Mei, C., Fern, B., Reilly, S., Hodgson, M., Reddihough, D., Mensah, F., & Morgan, A. (2020). Communication behaviours of children with cerebral palsy who are minimally verbal. Child: Care, Health and Development, 46(5), 617–626. doi:10.1111/cch.12792
- Mei, C., Reilly, S., Reddihough, D., Mensah, F., & Morgan, A. (2014). Motor speech impairment, activity, and participation in children with cerebral palsy. International Journal of Speech-Language Pathology, 16(4), 427–435. doi:10.3109/17549507.2014.917439
- Mei, C., Reilly, S., Reddihough, D., Mensah, F., Green, J., Pennington, L., & Morgan, A. T. (2015). Activities and participation of children with cerebral palsy: Parent perspectives. Disability and Rehabilitation, 37(23), 2164–2173. doi:10.3109/09638288.2014.999164
- Mei, C., Reilly, S., Reddihough, D., Mensah, F., Pennington, L., & Morgan, A. (2016). Language outcomes of children with cerebral palsy aged 5 years and 6 years: A population‐based study. Developmental Medicine and Child Neurology, 58(6), 605–611. doi:10.1111/dmcn.12957
- Moll, L. R., & Cott, C. A. (2013). The paradox of normalization through rehabilitation: Growing up and growing older with cerebral palsy. Disability and Rehabilitation, 35(15), 1276–1283. doi:10.3109/09638288.2012.726689
- Murray, J., & Goldbart, J. (2009). Cognitive and language acquisition in typical and aided language learning: A review of recent evidence from an aided communication perspective. Child Language Teaching and Therapy, 25(1), 31–58. doi:10.1177/0265659008098660
- Myrhaug, H. T., & Østensjø, S. (2014). Motor training and physical activity among preschoolers with cerebral palsy: A survey of parents’ experiences. Physical & Occupational Therapy in Pediatrics, 34(2), 153–167. doi:10.3109/01942638.2013.810185
- Myrhaug, H. T., Jahnsen, R., & Østensjø, S. (2016). Family-centred practices in the provision of interventions and services in primary health care: A survey of parents of preschool children with cerebral palsy. Journal of Child Health Care, 20(1), 109–119. doi:10.1177/1367493514551312
- NorCP (2021). Resultater fra Norsk kvalitets- og oppfølgingsregister for cerebral parese [Results from the Norwegian Quality and Surveillance Registry for Cerebral Palsy].
- Nordberg, A., Miniscalco, C., Lohmander, A., & Himmelmann, K. (2013). Speech problems affect more than one in two children with cerebral palsy: Swedish population‐based study. Acta Paediatrica, 102(2), 161–166. doi:10.1111/apa.12076
- Öhrvall, A. M., Krumlinde‐Sundholm, L., & Eliasson, A. C. (2014). The stability of the manual ability classification system over time. Developmental Medicine and Child Neurology, 56(2), 185–189. doi:10.1111/dmcn.12348
- Påhlman, M., Gillberg, C., & Himmelmann, K. (2019). One‐third of school‐aged children with cerebral palsy have neuropsychiatric impairments in a population‐based study. Acta Paediatrica, 108(11), 2048–2055. doi:10.1111/apa.14844
- Palisano, R. J., Rosenbaum, P., Bartlett, D., & Livingston, M. H. (2008). Content validity of the expanded and revised gross motor function classification system. Developmental Medicine and Child Neurology, 50(10), 744–750. doi:10.1111/j.1469-8749.2008.03089.x
- Palisano, R., Rosenbaum, P., Walter, S., Russell, D., Wood, E., & Galuppi, B. (1997). Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine and Child Neurology, 39(4), 214–223. doi:10.1111/j.1469-8749.1997.tb07414.x|
- Parkes, J., Hill, N., Platt, M. J., & Donnelly, C. (2010). Oromotor dysfunction and communication impairments in children with cerebral palsy: A register study. Developmental Medicine and Child Neurology, 52(12), 1113–1119. doi:10.1111/j.1469-8749.2010.03765.x
- Pennington, L., Goldbart, J., & Marshall, J. (2005). Direct speech and language therapy for children with cerebral palsy: Findings from a systematic review. Developmental Medicine and Child Neurology, 47(1), 57–63. doi:10.1017/S0012162205000101
- Pennington, L., Virella, D., Mjøen, T., da Graça Andrada, M., Murray, J., Colver, A., Himmelmann, K., Rackauskaite, G., Greitane, A., Prasauskiene, A., Andersen, G., & de la Cruz, J. (2013). Development of The Viking Speech Scale to classify the speech of children with cerebral palsy. Research in Developmental Disabilities, 34(10), 3202–3210. doi:10.1016/j.ridd.2013.06.035
- Romski, M., Sevcik, R. A., Adamson, L. B., Cheslock, M., Smith, A., Barker, R. M., & Bakeman, R. (2010). Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. Journal of Speech, Language, and Hearing Research, 53(2), 350–364. doi:10.1044/1092-4388(2009/08-0156)
- Romski, M., Sevcik, R. A., Barton-Hulsey, A., & Whitmore, A. S. (2015). Early intervention and AAC: What a difference 30 years makes. Augmentative and Alternative Communication, 31(3), 181–202. doi:10.3109/07434618.2015.1064163
- Rosenbaum, P., Eliasson, A.-C., Hidecker, M. J. C., & Palisano, R. J. (2014). Classification in childhood disability: Focusing on function in the 21st century. Journal of Child Neurology, 29(8), 1036–1045. doi:10.1177/0883073814533008
- Rosenbaum, P., Paneth, N., Leviton, A., Goldstein, M., Bax, M., Damiano, D., Dan, B., & Jacobsson, B. (2007). A report: The definition and classification of cerebral palsy April 2006. Developmental Medicine & Child Neurology, 109(Suppl 109), 8–14. doi:10.1111/j.1469-8749.2007.tb12610.x
- Sigurdardottir, S., Eiriksdottir, A., Gunnarsdottir, E., Meintema, M., Arnadottir, U., & Vik, T. (2008). Cognitive profile in young Icelandic children with cerebral palsy. Developmental Medicine and Child Neurology, 50(5), 357–362. doi:10.1111/j.1469-8749.2008.02046.x
- Stadskleiv, K. (2017). Experiences from a support group for families of preschool children in the expressive AAC user group. Augmentative and Alternative Communication, 33(1), 3–13. doi:10.1080/07434618.2016.1276960
- Stadskleiv, K. (2020). Cognitive functioning in children with cerebral palsy. Developmental Medicine and Child Neurology, 62(3), 283–289. doi:10.1111/dmcn.14463
- Stadskleiv, K., Jahnsen, R., Andersen, G. L., & von Tetzchner, S. (2018). Neuropsychological profiles of children with cerebral palsy. Developmental Neurorehabilitation, 21(2), 108–120. doi:10.1080/17518423.2017.1282054
- Taylor, E., Schachar, R., Thorley, G., & Wieselberg, M. (1986). Parental account of children’s symptoms. The British Journal of Psychiatry, 149, 760–767. doi:10.1192/bjp.149.6.760
- von Tetzchner, S. (2018). Introduction to the special issue on aided language processes, development, and use: An international perspective. Augmentative and Alternative Communication, 34(1), 1–15. doi:10.1080/07434618.2017.1422020
- von Tetzchner, S., & Martinsen, H. (2000). Introduction to augmentative and alternative communication (2nd ed.). Whurr/Wiley.
- von Tetzchner, S., Launonen, K., Batorowicz, B., Nunes, L. R. d O. d P., Walter, C. C. d F., Oxley, J., Massaro, M., Stadskleiv, K., Yang, C.-K., & Deliberato, D. (2018). Communication aid provision and use among children and adolescents developing aided communication: An international survey. Augmentative and Alternative Communication, 34(1), 79–91. doi:10.1080/07434618.2017.1422019