Abstract
A socio-neurocognitive approach to augmentative and alternative communication (AAC) shows several underlying domains of communicative competence: Attention, perception, cognition, memory, orientation, socio-emotional development, motor skills, and language. To determine developmental markers of these underlying core domains of communicative competence in children with communication support needs, we developed a new screening instrument. The present article consists of three consecutive studies. In study 1, we constructed the first version of the screening instrument based on a sample of both children without disabilities and children with Down syndrome. In study 2, we confirmed the reliability (i.e., internal consistency) of the screening instrument in a new group of young children with typical development and established concurrent validity with the Early Language Scale. In study 3, we established concurrent validity with the Communication Matrix in a clinical sample of children with communication support needs. The screening instrument can be used in clinical practice as part of AAC assessment to provide comprehensive insights into strengths and weaknesses in the underlying core domains of communicative competence of children with communication support needs.
Individuals with communication support needs would benefit more from interventions tailored to strengths and weaknesses in critical zones of their overall development (Neil & Jones, Citation2016). Individuals with communication support needs, often referred to as complex communication needs, are people who cannot rely on speech alone to be heard and understood, and to understand their communication partners. Therefore, they cannot use speech as their primary means of expression and are in need of access to augmentative and alternative communication (AAC). To realize the full benefit of AAC interventions, a detailed client-, social- and context-related assessment is required to achieve an appropriate overview of developmental challenges and opportunities leading to suitable recommendations for and decisions on communication and language strategies in AAC (Beukelman & Light, Citation2020; Van Balkom et al., Citation2017). Clinical decision making in AAC should be based on a theoretically and clinically driven model that helps integrate information about a myriad of underlying and contributing factors that may affect communicative competence (Rowland et al., Citation2012). This enables verification (replicability) and validation of the reasoning and decision-making processes, its reliability and appropriateness. However, the lack of this type of instruments and theoretical insights make that most practitioners base their decisions on clinical judgment from experience (Schlosser & Raghavendra, Citation2004), which still is the case in AAC clinical practice. A related difficulty is the limited practical guidelines for communication and language assessment and decision making (Dietz et al., Citation2012) besides the earlier mentioned lack of comprehensive assessment techniques (Andzik et al., Citation2019) mainly related to the complex interwovenness of physical, intellectual, and sensory impairments of children with communication support needs which confounds standardized testing. The present article presents such a theoretically and clinically driven model and contains of three consecutive studies describing the development of a screening instrument for underlying developmental domains of communicative competence in children with communication support needs.
Communicative competence enables a person to express needs and wants, to learn and to socialize with others in or out of language (McLeod & Threats, Citation2008). Compromised development of communicative competence leads to developmental language disorders and impediments in development, learning and participation (Raghavendra et al., Citation2012). Communicative competence was first defined by Hymes (Citation1972) as the capacity and conventional knowledge to integrate and apply language planning, processing, understanding and functional use in an intentional way to other participants in communication. Communicative competence is seen as the result of a reciprocal process of mutual understanding of exchanged information between a sender and receiver in which the responses from the receiver attune with the intentions of the sender (Clark, Citation1996; Van Langendonck et al., Citation2018). To understand each other, communication partners need to synchronize their intentional behavior’s, linguistic and nonlinguistic acts. This requires (shared) attention and willingness to accept and respect each other’s roles and contributions (Clark, Citation1996; Tomasello, Citation2008).
Light (Citation1989) defined communicative competence related to AAC as “a relative and dynamic, interpersonal construct based on functionality of communication, adequacy of communication, and sufficiency of knowledge, judgment and skill in four interrelated domains: linguistic competence, operational competence, social competence, and strategic competence” (p. 137). Defining communicative competence provides a useful framework for describing how people who use AAC communicate (Light & McNaughton, Citation2014), especially for goal setting in AAC interventions directed toward the different communicative competences. The model on communicative competence of Light is most often used as a descriptive framework of skills pertaining to current communication skills and AAC use. Clinicians in AAC often face challenging questions during clinical decision making in determining the best matching AAC solutions for the individual child with communication support needs, such as: Where does the individual need for communication support and AAC stems from? How can AAC be used to steer and support broader development and learning? As Loncke (Citation2022) mentions, the provision of best matching AAC solutions accelerates development and unlocks cognitive potential. Therefore, insight is needed in what drives communicative competence and underlies communication support needs.
Whether an individual will gain and grow in these competencies is, according to Light and McNaughton (Citation2014) impacted by personal factors such as motivation, attitude, confidence, and resilience. Next to these personal factors, underlying communicative competence is an ensemble of perceptual, neurocognitive and behavioral regulation processes (Bishop, Citation2014; Tomasello, Citation2008). These processes are effectuated by a neural network infrastructure for communication and language. Understanding these underlying processes provides insight in the overall developmental and learning potentials of the child and the role of the environment (Simeonsson & Rosenthal, Citation2001). It is a clinical challenge to unravel the entanglement of these mutually reinforcing processes and factors that impact the development of communicative competence. Therefore, Van Balkom et al. (Citation2017) operationalized the principle that communicative competence is a multi-dimensional construct, enriching and adding extra “layers” underneath the more behavioral and practical level of Light’s framework of communicative competence.
In the present study we follow this socio-neurocognitive perspective on communicative competence as a reasoning and explanatory model to assessment and clinical decision making in AAC as proposed by Van Balkom et al. (Citation2017). In this perspective, communicative competence and language development are the outcome of a complex network of the following socio-neurocognitive developmental domains: Attention, perception, memory, cognition, orientation, social-emotional development, and motor skills. Recent brain studies namely show that communicative competence emerges from a complex neural network of nonlinear interdependencies between underlying processes (e.g., Friederici, Citation2011; Hagoort, Citation2017; MacDonald, Citation2017; Willems & Varley, Citation2010). According to these and other authors, knowledge about the development of a neural network for communication and language in the brain provides insight in the overall learning and development capacities of the child in the context of personal and environmental factors, in relation to communicative competence.
Communicative competence seen from this socio-neurocognitive perspective is related to sequential information processing, described in more detail in relation to AAC assessment and intervention by Van Balkom et al. (Citation2017): the route from input, storage, processing, to output. The following components constitute an integrated model of developmental core domains underlying communicative competence: (1) Input relates to attention regulation, arousal and perception; (2) Storage refers to memory functions; (3) Processing includes socio-emotional regulation, cognitive functions, and orientation; (4) Output comprises praxis, mobility, motor movements/coordination and the motor plans for expressive modes, and the integral influence of all core domains on language functions (vocabulary, meaning attribution, language comprehension, language production).
These developmental core domains do not merely work in sequence, but they form a robust neural network in which the interconnectedness allows for interchangeable and substitutable compensation and restructuring within and between all the underlying processes involved (Van Balkom et al., Citation2017). Any disruption in one of the domains leads to malfunctioning of all the others, as described in experimental and clinical case-studies (e.g., Mahone et al., Citation2008; Rauch et al., Citation2012). More specifically, strong, or healthy processes (i.e., neural connections) may become exploited to compensate for the impaired ones, referred to as neuroplasticity (Hengst et al., Citation2019; Pasquini et al., Citation2022, van Balkom, Citation2022). Where children with communication support needs experience impairments in numerous developmental core domains and processes, the cause of their communication problems and weakened levels of communicative competence is not easily determined. The socio-neurocognitive model for communicative competence provides a conceptual framework to describe, analyze, and explain the various underlying and interrelated processes within and across the separate core domains. As such, the socio-neurocognitive perspective on communicative competence underlying the present study is not in contrast, but should be seen as complementary in discussing and assessing communicative competence in children with communication support needs.
AAC solutions should not only be targeted and chosen on the output level (i.e., AAC as a means for conveying a message and to make up for speech impairments), as is still often done. AAC solutions should “function as an extended enforcement of natural adaptation and compensatory strategies in cases of impaired communication” (Van Balkom et al., Citation2017, p. 426). In other words, in clinical decision making, choices for unaided AAC (i.e., body signals, manual sign systems), aided AAC (technology, i.e., computerized speech generating devices), or combinations of both as well as the selection of intervention strategies should be based on comprehensive assessment results founded in a socio-neurocognitive perspective. The model has been used to steer AAC decision making and intervention planning in the past two decades in the Netherlands and gained considerable practice-based evidence (Stoep et al., Citation2012; Van Balkom et al., Citation2014). It is beyond the scope of the present article to discuss all these domains in detail. We refer to Van Balkom et al. (Citation2017) for more information on all domains and a case study on how to use these domains in clinical decision making in AAC. Here, we briefly highlight the domain of memory. In the discussion, the developmental domains are linked to a range of AAC solutions and strategies. Memory is an important domain in AAC. For example, in order to navigate through pages of a communication device, the person needs to remember where messages are stored, when no motor memory has been build up yet (Loncke, Citation2022) as well as remembering the internal message that the person wants to utter via the aided AAC device while actively searching for the words on the device, relating directly to working memory skills.
Table 1. Core domains and underlying constructs of communicative competence.
A thorough assessment of children with communication support needs on all these core domains would be highly time consuming. Next, assessing these children is challenging, since motor, sensory and/or cognitive characteristics may heavily impede traditional, standardized testing (Rowland & Fried-Oken, Citation2010). Parental reports and questionnaires have proven to be reliable and valid estimates of communication and language development of children with communication support needs, and more specifically children with Down syndrome (Deckers et al., Citation2016a; Miller et al., Citation1995). The present article describes the development of a screening instrument, to be used as parental questionnaire or checklist/observation tool, to determine the developmental markers of underlying core domains of communicative competence in children with communication support needs (see Van Balkom et al., Citation2017).
The overall research question of this article is: Is the proposed screening questionnaire a reliable and valid instrument to determine developmental markers of the core domains for communicative competence? Three studies were conducted to answer this question. Study 1 focuses on the construction of the screening instrument in samples of children with typical development (age 1–4 years old) and children with Down syndrome (age 1–7 years old). Study 2 concerns confirmation of reliability measures and the concurrent validity of the screening instrument on language development in children with typical development, and study 3 focused on the concurrent validity of the screening instrument on communicative skills (i.e., Communication Matrix) in a clinical sample of children with communication support needs, all with an intellectual disability.
Study 1: development of the screening instrument
Most of the developmental core domains are studied within their own research field, for example, for domains like attention and memory large theoretical grounds exist describing and studying the development, functioning and relation to brain functions. All domains can be further divided in underlying constructs. For attention, for example, constructs as focused attention, shifted attention, sustained attention, and joint attention are often identified. A screening instrument for developmental markers in core domains underlying communicative competence should contain all the important underlying constructs of that domain. All constructs should be represented in the instrument by at least one item. As a starting point for developing the instrument, we used the International Classification of Functioning-Child and Youth version (ICF-CY), an extensive framework for classifying health and health-related issues developed by the World Health Organization (WHO, Citation2007). Regarding domains for which the ICF-CY functions proved too superficial, underlying constructs described in neurocognitive and developmental literature and/or classifications according to developmental tests as the Bayley-III were adopted. This was the case for cognition where the ICF-CY merely distinguishes “basic cognitive functions” versus “higher cognitive functions” and for social-emotional development. shows the core domains, definitions, and underlying constructs that were the start of development of the screening instrument.
Table 2. Characteristics of the participants.
In addition to children with typical development we included children with Down syndrome in study 1. Down syndrome is the most common genetic cause of intellectual disability (Sherman et al., Citation2007). Communication problems are highly prevalent, due to expressive language difficulties and poor speech motor control (Zampini & D'Odorico, Citation2013), and a specific physiological and anatomical profile including a smaller than average oral cavity (Miller et al., Citation1999). Poor intelligibility and significantly delayed onset of speech are two primary reasons to introduce AAC to children with Down syndrome (Brady, Citation2008). In addition, they experience cognitive, sensory and/or motor disabilities (Fidler, Citation2005), that need to be accounted for in AAC interventions. Owing to its homogeneous etiology, but heterogeneous patterns of functioning, children with Down syndrome are among the most valid reference groups for research in individuals with intellectual disabilities (Van Duijn et al., Citation2010), and therefore they can be used as a valid reference group for children with communication support needs, who experience weakened levels of communicative competence (Abbeduto et al., Citation2007).
Method
Participants
Data from two groups of children were gathered over time, from 2014 to 2020. More than 90% of the assessments of children with typical development dated from 2017 or later. The assessments of children with Down syndrome took place in 2014 and 2015.
In this study, 295 children with typical development were included, 48.5% girls, 51.2% boys, and 0.3% missing gender. The children were filtered on age, between 1;0 and 3;11 years of age. This age range was chosen because communicative competence changes rapidly in typical development from 1 to 4 years, which is the age at which children in the Netherlands start school. Exclusion criteria were presence or suspicion of developmental delay or disabilities, both cognitive, language and/or motor. The mean age was 2;5 year (SD = 10 months). More details on the age groups are provided in .
Table 3. Total test statistics per core domain in study 1.
In addition, 133 children with Down syndrome took part in this study, 39.8% girls and 60.2% boys. The children with Down syndrome were between 1;0 and 6;11 years of age. The mean age was 3;2 year (SD = 18 months). The children with Down syndrome fell within a broader age range than the children with typical development, as development of underlying developmental domains of communicative competence is delayed in children with Down syndrome. No exclusion criteria were employed. The “typical” type of Down syndrome, trisomy 21, was present in 91.0% of the children, 4 children had mosaicism, 4 children had translocation, 1 child had a combination of trisomy 21 and translocation, and for 3 children the specific type of Down syndrome was unknown.
We used maternal education as a proxy for Social Economic Status (SES), which was divided into three groups: low (elementary school and vocational secondary school), medium (senior secondary vocational education up to pre-university education) and high ((applied) university), see . SES was comparable across both groups in the present study. The percentages pointed to an overrepresentation of mothers from high social economic status. The percentage of women, within the age range of 25 to 55 years, with high educational levels was around 48% in the Netherlands in 2020 (Centraal Bureau voor de Statistiek [CBS], Citation2020).
Procedure
All parents signed an informed consent form prior to participating. Parents from children with typical development were recruited through convenience sampling (e.g., by social media and via day care centers). Parents from children with Down syndrome were recruited through a parent organization. Parents received a printed copy of the extensive questionnaire and were asked to fill this out for their child. Ethical approval for all three studies was given by the ethical review board of the university.
Materials
An extensive questionnaire was administered to all participants. For this purpose, a comprehensive item pool was created (Deckers & van Zaalen, Citation2018). The intent of this item pool was to cover all relevant developmental stages important to early communicative development for children up to six years of age. The questionnaire was based on several validated and normed tests and questionnaires such as the Bayley-III-NL (Van Baar et al., Citation2015), the Communication and Symbolic Behavior Scales (Wetherby & Prizant, Citation2002), Vineland Screener for the adaptive level of functioning (Van Duijn et al., Citation2009), the Behavior Rating Inventory of Executive functions Preschool version (BRIEF; Huizinga & Smidts, Citation2012), the Child Behavior Checklist 1½ − 5 (CBCL; Achenbach & Rescorla, Citation2000), and the Gross Motor Function Measure (Ketelaar, Citation2002). In addition, items from an early intervention program for children with Down Syndrome were also added to the item pool (Small Steps, Early Intervention Program; Pieterse & Treloar, Citation2009). The questionnaire sought to be exhaustive, rather than concise. Small steps in development were described. An expert panel consisting of experts from different fields such as (developmental) psychology, physiotherapy and speech and language therapy judged the questionnaire on its completeness and wording in three consecutive rounds.
The total item pool related to the underlying developmental domains of communicative competence consisted of 361 content items. An additional 18 items assessed child, health and parental characteristics and family background. The content items covered the following core domains: attention (23 items), perception (57 items), memory (15 items), cognition (73 items), orientation (23 items), social-emotional development (45 items), and motor skills (125 items). The content-items were written as a dichotomous statement and could be answered with either a “yes” or a “no” (e.g., “The child can match objects based on shape”). Preliminary analyses were run after the questionnaire was filled out for 110 typically developed children, in 2018. Items of the domain Perception didn’t discriminate, and internal consistency was low. Therefore, we added questions for Perception to the item pool, based on the (Infant/Toddler) Sensory Profile (Dunn, Citation2013).
Missing data
The data on the first set of Perception items was removed from the analysis (110 children with typical development). The revised items were only filled out for 185 children with typical development. Unfortunately, we were not able to recruit more parents of children with Down syndrome after the revision of the questionnaire. Therefore, the data of children with Down syndrome on the Perception items are missing by design as well.
Only 44 responses, which is less than .0005%, were missing because parents did not answer the question (i.e., they missed to score a single item). Each missing response involved a different child, and almost always different items. These incidental missing responses were coded as “no”. We assumed that the parents could not answer these questions as the child probably did not show the behavior that the question stated. In addition, the number of missing responses was so low, that the method of handling of missing data would have a neglectable effect.
Analytical approach
The items were scored as 0/1 items, with the 1 score indicating a skill as developed. Around 10% of the items were reversed coded, that is, a positive response was scored as 0. Items for subscales of each domain were included, using both statistical (Classical Test Theory, Allen & Yen, Citation1997) and theoretically based criteria. The key content related criterium ensured a coverage of all underlying constructs of a domain. In addition, the item with the better measurement properties was selected from items stating similar behaviors. On closer inspection, some items were reassigned to a different domain.
The statistical criteria were based on the average score (p-value), the correlation of the item to the score on the remaining items (Rir) and the correlation of positive responses with age in months (Rage): (a) P-value in typical development group at least 0.20, and at most 0.90, (b) P-value in down syndrome group at most 0.80, (c) Rir in typical development group at least 0.20, (d) Rage in typical development group at least 0.20, and (e) Rir in down syndrome group at least 0.30. In addition, statistical criteria were formulated for the total test, using the mean p-values of the items and the reliability estimate coefficient alpha (Cronbach, Citation1951): (f) Mean p-value in typical development group at least 0.50, (g) Mean p-value in down syndrome group at most 0.50, (h) Alpha in typical development group at least 0.80, and (i) Alpha in down syndrome group at least 0.70. Slightly different criteria have been used for both groups. If we would have used the same statistical criteria in both groups, too many items would have dropped out that would fit the children with Down syndrome, but not the children with typical development, since most children in the latter group already developed this skill. Multiple items were too easy for the children with typical development, but are within the range for Down syndrome. Since the instrument was intended to be developed for children with communication support needs, we adapted the criteria for the children with Down syndrome.
In an iterative way, following these criteria, items were selected accordingly. Given the goal to include at least one item per underlying construct, it was impossible to meet all criteria at the same time. In total 95 items were included. The statements of the items can be found in Supplementary Appendix A. All statistical properties can be found in Supplementary Appendix B. Of these items, 6 items failed on one statistical criterium, and 1 item on two statistical criteria. Because of content related criteria (i.e., item belongs to an underlying construct (see ) for which no other item could be selected) and excellent other statistics, these items were still included. For two underlying constructs, no items with acceptable statistical properties could be found, the only available items were too easy (p-value in down syndrome group larger than 0.80). This was the case for the episodic buffer for Memory and social referencing for Social-Emotional development.
The subscale of cognition items has a mean p-value of 0.48, missing statistical criterium (f). This selection was not altered as no easier items with similar or better other properties were available. The total test statistics are listed in .
Table 4. Mokken scale statistics per core domain.
Results
The scale selection was evaluated in several ways. The internal consistency was checked by classical reliability estimates and fitted Item Response Theory (IRT) models on the subscales. The construct validity was evaluated by the correlational structure of the subscales and the distribution of the scores given the age of children.
Reliability
The reliability (Cronbach, Citation1951) was computed for each subscale, both in the group of children with typical development and in the group of children with Down syndrome. The results can be found in . Alpha exceeded 0.80 in the first group for all but one subscale. The reliability estimate was 0.79 for the subscale Attention. Alpha exceeded 0.70 in the latter group for all subscales. No reliability estimate could be computed in the group of children with Down syndrome for the subscale Perception, for lack of data.
IRT fit statistics
A Rasch model (Rasch, Citation1960) was fitted to each subscale. The data of both groups were analyzed using the dexter library in R (Maris et al., Citation2022). To check the fit of the items, children were grouped within each population on their ability estimate. Within each ability group, a chiquare test was computed on the observed and expected p-value. The results were aggregated per item. The number of subgroups of sufficient size determined the number of degrees of freedom for the aggregated chisquare test. This method is called the Si-test in Verhelst (Citation1993). It is similar to Yen’s Q1 (1981). The results per item are presented in Supplementary Appendix C. Out of the 95 items, only 11 items had a p-value less than 0.001, indicating a misfit to the Rasch model. An inspection of the item response curves in both groups indicated that the misfit occurred in three ways: differential item functioning (DIF) between the two groups of children (attention09, fine_motor04, memory6, social_emotional08, social_emotional10), a lower discrimination between low and high scoring children than expected by the Rasch model (cognition02, cognition14, social_emotional02, orientation1, gross_motor09), or a higher discrimination between low and high scoring children than expected (cognition01). A two-parameter IRT-model would have fitted the data better. However, the number of observations per group was too small to obtain stable estimates of a 2 parameter IRT-model.
In line with the limited number of observations, the fit of a nonparametric IRT model (Mokken, Citation1971) was evaluated on the data of both subgroups of children. The homogeneity index H is computed at three levels in Mokken Scale Analysis (MSA): pairwise, at the item level and at test level. All pairwise Hij-indices were positive, indicating positive correlations between all pairs of items. The values of the scalability index Hi is presented per item in Supplementary Appendix C. The smallest Hi-indices at item level per subscale were all at least 0.11 (), indicating positive coherence between each item and the remaining items in a subscale. The H-values per subscale were 0.40 or larger, indicating medium strong to strong scales (Koopman et al., Citation2022). The only exception is the Attention scale, where H equals 0.38. Any Hi value above 0 indicates positive coherence. Only 3 items had a Hi-value lower than 0.30; values lower than 0.4 occurred mainly in the attention subscale. This was also the subscale with the lowest test H-value.
Table 5. Latent correlations between the subscales in children with typical development (above diagonal) and Down syndrome (below diagonal) groups.
Correlations between the subscales
Observed correlations are limited by the reliability of the two variables for which the correlation is computed. Latent correlation estimates indicate the correlations between the underlying constructs, without being limited. Fitting Rasch models to each of the core domains enabled an estimation of the latent correlations of the subscales. The function latent_cor of the R-package dexter (Maris et al., Citation2022) was used to compute the latent correlations in . The latent correlations were computed in both groups separately. The latent correlations were in general at least 0.80, indicating strong positive coherence between the core domains. The exceptions were the correlations of the subscales Attention and Perception with some of the other subscales, although these two subscales correlated 0.81 with each other in the group of children with typical development. In general, the latent correlations were larger for children with Down syndrome. However, Attention and Gross motor skills correlated less with the other subscales in these children compared to the group of children with typical development.
Table 6. Total test statistics per core domain in study 2 and 3.
Distribution of scores by age
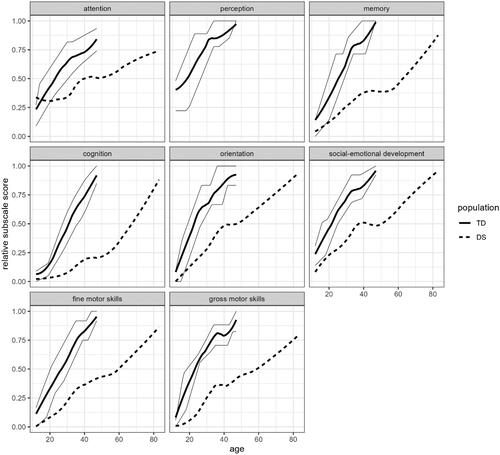
In , a locally estimated regression of the mean scores in both groups are plotted versus age (in months), for each subscale. The mean score of the children with Down syndrome is lower than the mean score of the group of children with typical development, at all ages. Around the line of the mean score in the latter group, lines are plotted that indicate the 25th and 75th percentile in the group of children with typical development. The mean scores clearly correlate with age for both groups, as all items correlated positively with age. The mean scores vary between 0 and attain almost the maximum of the subscale in both groups within the age limits of the respective groups.
Conclusion
A parental questionnaire was developed by performing an item reduction on an extensive questionnaire. The remaining questionnaire consists of 95 items, distributed over eight core developmental domains. Within the domains, items are well distributed to cover theoretical underlying constructs of the core domain (see ). The subscales of each domain had good measurement properties, as confirmed by Cronbach’s alpha, IRT fit statistics, a positive correlational structure and a positive relation with age within each group. We used both children with typical development and children with Down syndrome to make sure that items were not too easy or too difficult, leaving a questionnaire that seems both theoretically and statistically sound to be used for the determined goal. The distributions of scores in both groups show that the questionnaire is useful for children with typical development until the age of 3;6 − 4 years. The children with Down syndrome in the current study reached the same levels around the age of 6;6 years. The curves for all core domains seem to show a delayed development in the children with Down syndrome relative to patterns of typical development. This is in line with studies showing the rather delayed than deviant nature of development in children with Down syndrome (e.g., Deckers et al., Citation2019; Polišenská & Kapalková, Citation2014).
Study 2: reliability and concurrent validity in children with typical development
For the development of this novel instrument and the applicability for AAC clinical practice, we wanted to study the reliability and validity in more detail. Therefore, in study 2 we aimed to confirm the reliability (i.e., internal consistency) of the screening instrument in a new group of young children with typical development. Furthermore, we studied the concurrent validity of the screening instrument by including a measurement on language development. For children with typical development the underlying processes and core domains that constitute communicative competence drive language acquisition (Friederici, Citation2017; Simeonsson & Rosenthal, Citation2001; Van Balkom et al., Citation2017). This also holds for children with developmental language disorder (Bishop, Citation2014). Early language development follows the established neural network for communicative competence (Hagoort, Citation2017; Johnson & de Haan, Citation2011). This is what makes language a phenomenon of communication. Hagoort (Citation2005) argues that language functions are part of a dynamically adjusting infrastructural network in the brain that do not reside in a specific brain region. All core domains have an integral influence on the development of communicative competence and ultimately also on language functions, self-care, self-reliance, and autonomy (Van Balkom et al., Citation2017). In study 2 we therefore aimed to determine whether the core domains, measured by the screening instrument from study 1, correlated with a measurement of language development in children with typical development (age 1–4 years).
Method
Participants
The parents of 232 children filled out the screening instrument and the Early Language Scale. Mean age of the children was 2;6 years (SD = 11 months) with a normal distribution of age in the group (see ). Slightly more girls participated in the present study (n = 124, 53.4%). SES is mostly high in the total sample, showing an overrepresentation of highly educated parents.
Procedure and materials
Parents from children with typical development were recruited through convenient sampling (e.g., by social media and via day care centers). They received a letter explaining the nature of the study and a link to an online questionnaire. The online questionnaire consisted of a digital version of the screening instrument and the validated Dutch version of the Early Language Scale (ELS, Visser-Bochane et al., Citation2020). The ELS measures language development in 26 observable items by parents, covering the full range of early language development of children from 1 to 6 years of age. Statements are provided on which parents need to indicate a “yes” or “no” answer. For example, “Does your child understand 3 word sentences?” or “Does your child make sentences with “because”? All parents signed an informed consent form, integrated in the online system, prior to participating.
Analytical approach
As in study 1, the latent correlations were estimated between the subscales measuring the core domains, and the ELS. The correlations indicate the degree to which the core domains correlate with language development.
Results and conclusions
The reliability estimates of the subscales and the latent correlations with the ELS can be found in . The reliabilities of the subscales in this second group of children with typical development were in general comparable to those in study 1 (). For some subscales the reliability was slightly lower than in study 1. A slightly smaller and less diverse population (variability in age groups and SES) than in study 1 might explain the somewhat lower value of Cronbach’s alpha, next to the relatively small number of items in the scales of Memory and Orientation. The latent correlations of the subscales with the ELS () were all but one at least 0.89. The only core domain that did not correlate that much with Language was Perception.
Table 7. Latent correlations with the ELS in study 2 and 3, and observed correlation with CM in study 3.
Table 8. AAC strategies connected to underlying domains of communicative competence.
The reliability (i.e., internal consistency) of the screening instrument was found to be reasonable to good in a second sample of children with typical development between 1 and 4 years of age. The concurrent validity was established with the Early Language Scale, showing high correlations between the subscales for the underlying core domains of communicative competence and the measurement of language development ELS.
Study 3: concurrent validity of the screening instrument in children with communication support needs
In study 2 we showed the concurrent validity of the screening instrument in children with typical development. The goal of this research project was to develop a screening instrument for developmental markers of core domains underlying communicative competence in children with communication support needs. In study 3 we therefore investigated the concurrent validity of the screening instrument on communicative skills in a clinical sample of children with communication support needs.
Method
Participants
Participants for study 3 were recruited from the Milo AAC center in the Netherlands. In the Netherlands, Stichting Milo is the only AAC center that works throughout the whole country and which is known for working with the socio-neurocognitive model. Therefore, not mentioning the name of the center would not prevent readers from identifying the research to be related to the Milo AAC center. Given no information is provided on individual children, participants remain anonymous. Study 3 thus is based on a clinical sample of 85 children of at most 12;0 years of age with communication support needs and their parents who received AAC assessment and interventions (see for information on distribution across age groups). All participating children had an intellectual disability and did not rely on natural speech. The developmental, adaptive age, assessed by the Vineland Screener, varied between 6 and 62 months with a mean of 22 months. Therefore, the mean developmental, adaptive age is lower than the chronological age of the children with typical development in study 1 and 2.
About 25% of the children had a genetic syndrome, of which Down syndrome, Angelman syndrome, and Rett syndrome were the most occurring. Ten children were known with deletion and/or duplication of specific genes. Five children were known with cerebral palsy with intellectual disability, and seven with autism spectrum disorder with intellectual disability. In about 25% of the cases unknown causes for the intellectual disorders in combination with developmental language and speech disorders were reported. Of the participants about 1 in 5 had a severe motoric disability (wheelchair bound), about 35% had mild to severe visual impairments amongst which Cerebral Visual Impairment, and about 15% had (mild to severe) auditory impairments.
Procedure
The screening instrument from study 1, the Early Language Scale (ELS) used in study 2 (Visser-Bochane et al., Citation2020) and the Communication Matrix (Rowland & Fried-Oken, Citation2010) are administered for all clients of the AAC center as part of their regular, care-as-usual AAC assessment. Parents of children signed an informed consent for using their data for scientific research. A decision of parents not to sign had no influence on the AAC assessment and interventions they received, since the professionals carrying out the assessment and interventions were not made aware of this decision.
Children for whom more than eight questions of the screening instrument were not answered, were not included in the study. This was the case for 5 children for which data was retrieved. The remaining missing responses were interpreted as a negative answer. That is, the parent probably could not establish whether the child displayed the mentioned behavior. Most of the included children (n = 64) had no missing values, 9 children had one missing value, 5 children had two missing values and the remaining 7 children had up to seven missing values. Missings seem to be at random, since these were not clustered within one domain, nor were there specific items that weren’t answered for multiple children. In addition, three children had a missing value on one ELS question each. These were scored as negative responses as well. The CM total score was missing for 8 out of the 85 children.
Materials
Parents of children with communication support needs received the screening instrument from study 1 and the Early Language Scale used in study 2 on paper. Furthermore, the Communication Matrix was administered in an interview between a professional and the parents of the children. The professionals (i.e., speech language pathologist, psychologist) all had experience in working with children with communication support needs, AAC, and the used instruments. The Communication Matrix is a communication skills assessment, which accommodates any type of communication behavior including AAC. It covers the development of communication skills during the earliest stages of communication. The Matrix emphasizes the functional use of communication in a social world, and therefore takes a socio-pragmatic approach. The Communication Matrix maps the reasons people communicate and the ways they behave to communicate those reasons (Rowland & Fried-Oken, Citation2010).
Analytical approach
First, the reliabilities and the latent correlations of the subscales of the screening instrument and the ELS were calculated as in Study 2. We used the total score on the Communication Matrix (CM) as measurement of communication skills. As only the total score on the CM was known, the observed correlations between the CM, the ELS, the subscale, and total score on the screening instrument were calculated.
Results and conclusions
The reliabilities of the subscales of the screening instrument () were in the same order of magnitude in this study with children with communication support needs, as in the group of children with typical development in study 2, with Orientation being the only exception. This shows a good overall internal consistency of the questionnaire in use with children with communication support needs. The mean p-value of all subscales falls well between 0.1 and 0.9, showing that the scales as such are not too difficult or easy for the children with communication support needs in the present study. The mean p shows however that some subscales may contain a relatively high number of difficult items (i.e., the subscale of cognition with a mean p-value just above .2). The latent correlations of the core domains with Language (ELS) are somewhat lower for most of the core domains than in study 2, especially for the subscales Attention, Perception and Gross motor skills, which most likely reflects the heterogeneous nature and the prevalence of motoric and sensory difficulties of the group children with communication support needs in the present study. The other subscales correlate high with Language. Based on the subgroup of children with a CM score (N = 77), the latent correlation of the screening instrument and the ELS and the observed correlation of the screening instrument with CM are presented in . All are highly significant (p < 0.01). The correlations are again the lowest for the subscales Attention, Perception and Gross motor skills. Overall, this study shows that all developmental domains have a significant relationship with Language and Communication outcomes, both for children with typical development (study 1 and 2), children with Down syndrome (study 1), and the children with communication support needs (study 3).
General discussion
The aim of the present study was to develop a parental questionnaire for underlying domains of communicative competence in children with communication support needs. In study 1, the questionnaire was developed and evaluated in a typically developing group. The final version of the questionnaire consists of 92 items in total, divided over the developmental domains of attention, perception, memory, cognition, orientation, social-emotional development, and motor skills. These domains underlying to communicative competence and language development (Friederici, Citation2011; Hagoort, Citation2017; Tomasello, Citation2008; Willems & Varley, Citation2010). All domains in the final questionnaire were found to be unidimensional with high internal consistency, and with all underlying theoretical constructs present, except for social referencing and episodic buffer. This shows the comprehensive nature of the parental questionnaire and suggests a high content validity. The reliability was found to be (reasonably) high, both in study 1 and 2. Concurrent validity is shown in children with typical development with the ELS and in children with communication support needs with the ELS and the CM. The correlations with these other instruments are medium to high, but not too high, which indicates that the developed questionnaire measures different constructs than the ELS and CM. Given the theory-driven approach in establishing the item pool for the questionnaire (see ), making use of validated instruments, it seems reasonable to conclude the developed instrument gives insight into the targeted core domains of communicative competence. Even more importantly, we showed the relationship between all the developmental domains and language and communication measures in children with communication support needs, informing clinical practice to look at AAC assessment in a broader developmental perspective than often done.
Strengths and limitations
The present study is the first study to assess all core domains underlying communicative competence and communication and language skills (based on the socio-neurocognitive model issued by Van Balkom et al., Citation2017) at the same moment in time for children with communication support needs. The screening questionnaire is developed for the (chronological or developmental) age range until 4 years. “Given the particularly high plasticity of development during the first 3 years of life, there is an urgent need for scalable, … validated instruments to monitor child development in this specific developmental period” (Waldman et al., Citation2021, p. 369).
In study 2, we see high correlations between the language scale and most of the core domains. While this might point to issues with measuring clear factors per core domain, it is not surprising giving recent insights that language levels at age 3 in typical development drive the development of executive functions (i.e., cognition, memory, inhibition) (Romeo et al., Citation2022). Conceptually, indicators of expressive language often tap into children’s cognitive abilities, by asking them to describe complex constructs or explain and make sense of (social, emotional, problem-solving) situations (Waldman et al., Citation2021).
Although our findings suggest favorable evidence for reliability and validity, potential users should consider several limitations. Our sample of children with communication support needs was obtained by convenience, by using clinically gathered data from children receiving AAC assessment and intervention. Important to note is that we therefore included a subset of the group “communication support needs”, mainly those with intellectual disabilities, often in combination with motor and/or sensory disabilities. Given the clinical nature of the sample, we do think it represents the heterogeneous nature of communication support needs as often seen in AAC clinical practice.
Another limitation of the current study is that the theoretical constructs of social referencing (domain social-emotional development) and the episodic buffer (domain memory) are not represented in the final questionnaire after following item reduction rules. When using the current questionnaire in clinical practice, we suggest adding items for these constructs, like “the child adjusts its behavior to reactions of a familiar adult” for social referencing. Items for the episodic buffer may be too difficult for most of the children in the present study, given development of the episodic buffer (especially) after the age of 4–6 years (for an overview see Henry, Citation2010).
Clinical implications
The screening questionnaire is designed to be a self-report measure. The new parental questionnaire can be incorporated into clinical practice efficiently, as the questionnaire obtained in the current study is comprehensive, but also short, and therefore not highly time-consuming. A parental questionnaire provides efficient and quick insights into relative strengths and weaknesses of the individual child (Miller et al., Citation1995). Prior research shows that parental reports in children with Down syndrome can be a reliable estimate of the child’s development (Deckers et al., Citation2016a). The simple act of interviewing caregivers in measuring their child’s development may help the caregivers to become more aware of and attentive to their children’s behaviors and milestone attainment (Altafim et al., Citation2020). The new parental questionnaire can form a starting point for practitioners on which to base care and treatment. The list provides insights into strengths and weaknesses of the individual child but is not norm-referenced, meaning that scores between children cannot be compared. As the group of children with Down syndrome is very heterogeneous (e.g., Karmiloff-Smith et al., Citation2016), as is true for children with communication support needs in general as portrait by the nature of the clinical sample in the present study, information on the individual child is often more insightful than comparing scores between children.
Loncke (Citation2022) states that the main focus of AAC assessment and evaluation should be the future: how can a person be helped with AAC in general, and more specifically what kind of AAC intervention has a good chance to help the person? In other words, it is not only about how a good fit can be found between characteristics of the person and AAC solutions, but also about how these AAC solutions impact and support the development of the underlying core domains of communicative competence. Important to stress, a certain development in the underlying domains of communicative competence measured by the developed instrument is no prerequisite to start to use AAC. It is the other way around, AAC can and should be used as soon as possible in children with communication support needs, to support weaknesses and increase strengths in these domains (see for an overview of possible AAC solutions related to each of the domains). For example, when filling out the screening instrument, the clinician could find out relative weak attention skills. Then AAC solutions should be chosen that directly support attention functions of the child.
Family and close staff members should take a central role in the decision-making process, in choosing and implementing AAC solutions (Lynch & Murray, Citation2023). From clinical experience with using the developed questionnaire and discussing core domains with family and staff members, we have seen that it increases motivation and longer-lasting AAC use in the families and schools. An important reason is that everybody involved in AAC intervention has a better notion of why this is the best-fit of AAC, why using AAC themselves as communication partners supports the child in decreasing communication support needs, and also why these AAC solutions may impact communicative competence and future development. The screening instrument is a good starting point for practitioners. Clinically, it will help to describe individual strengths and weaknesses, but we would like to stress that the clinical then in AAC intervention shouldn’t target that specific skill. We must still assess an individual’s unique and specific skills within each of these domains in addition to administering the screening instrument, since clinicians need to know exactly what the child with communication support needs can and cannot do in order to make appropriate decisions about things such as AAC access methods.
We are aware that underlying and contributing factors to communicative competence and clinical decision making in AAC also include contextual, environmental, and personal factors. Communicative competence is impacted not only by factors intrinsic to the individual with communication support needs (e.g., linguistic, operational, social and strategic skills as well as psychosocial factors such as motivation, attitude, confidence and resilience), but also by extrinsic factors, including barriers in the environment that may impede communicative competence, and environmental supports that may enhance communicative competence (Light et al., Citation2003). Ultimately, communication is an interpersonal process where meaning is created in partnership (Teachman & Gibson, Citation2014). As a result, intervention to enhance communicative competence necessitates a focus on not only the individual with communication support needs but also partners in the environment, to reduce barriers and ensure appropriate supports as required (Soto, Citation2012). Therefore, when administering the developed questionnaire in clinical practice in our AAC center, we directly map barriers and facilitators from the environment to the core domains they impact (f.e., see Deckers et al., Citation2016b), based on observations in all communicative contexts of the child, direct and dynamic assessment, and interviews with all important communication partners in the social network. We strongly recommend pairing the screening questionnaire with information derived from these observations, interviews, and other forms of (dynamic) assessment, and not use the questionnaire solitary to determine the child’s skills or plan AAC interventions. Clinical decision-making in AAC relies on this total overview (see Van Balkom et al., Citation2017 for this Communication Competence Profile, CCP). The interdependence of core domains in early language and communication development indicates that interventions targeted at this development should give attention to all core domains. An immersive intervention designed to stimulate early language, communication, and early literacy, while taking the individual and contextual strengths and weaknesses of children with communication support needs and their communication partners into account, resulted in greater vocabulary and syntax development for the children in the intervention group than children in a control group that did not receive AAC intervention based on this socio-neurocognitive approach (Van der Schuit et al., Citation2011).
Future directions
Future directions in research are looking at the predictive validity of the screening questionnaire, if the questionnaire can measure changes (i.e., development during intervention) over time, and how it is used in clinical decision making in AAC clinical practice. Furthermore, we aim to look more into the interconnected and dynamic nature of all domains and language and communication development. In the present study we only looked at correlations, but we aim to do network modeling analyses when we gathered more data from a clinical sample, to investigate how all domains together interact with each other and with language and communication outcomes.
Supplemental Material
Download MS Word (30.9 KB)Supplemental Material
Download MS Word (35.3 KB)Supplemental Material
Download MS Word (32.4 KB)Disclosure statement
The authors have no relevant conflicts of interest to disclose.
Additional information
Funding
References
- Abbeduto, L., Warren, S. F., & Conners, F. A. (2007). Language development in Down syndrome: From the prelinguistic period to the acquisition of literacy. Mental Retardation and Developmental Disabilities Research Reviews, 13(3), 247–261. https://doi.org/10.1002/mrdd.20158
- Achenbach, T. M., & Rescorla, L. (2000). ASEBA preschool forms & profiles: An integrated system of multi-informant assessment. Aseba.
- Allen, M. J., & Yen, W. M. (1997). Introduction to measurement theory. Waveland Press.
- Altafim, E. R. P., McCoy, D. C., Brentani, A., de Ulhôa Escobar, A. M., Grisi, S. J., & Fink, G. (2020). Measuring early childhood development in Brazil: Validation of the caregiver reported early development instruments (CREDI). Jornal De Pediatria, 96(1), 66–75. https://doi.org/10.1016/j.jped.2018.07.008
- Andzik, N. R., Chung, Y. C., Doneski-Nicol, J., & Dollarhide, C. T. (2019). AAC services in schools: A special educator’s perspective. International Journal of Developmental Disabilities, 65(2), 89–97. https://doi.org/10.1080/20473869.2017.1368909
- Beukelman, D., & Light, J. (2020). Augmentative and alternative communication: Supporting children and adults with complex communication needs (5th ed.). Paul H. Brookes.
- Bishop, D. V. (2014). Uncommon understanding (classic edition): Development and disorders of language comprehension in children. Psychology Press.
- Brady, N. C. (2008). AAC for children with Down syndrome and children with fragile X syndrome. In Roberts, J. E., Chapman, R. S., & Warren, S. F. (Eds.), Speech and language development and intervention in Down syndrome and fragile X syndrome (pp. 255–274). Paul H. Brookes.
- Centraal Bureau voor de Statistiek (2020). Bevolking; onderwijsniveau [Population; level of education]. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82275NED/table?fromstatweb
- Clark, H. H. (1996). Using language. Cambridge University Press.
- Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. https://doi.org/10.1007/BF02310555
- Deckers, S. R. J. M., & van Zaalen, Y. (2018). Woordenschatontwikkeling in relatie tot neurosociocognitieve kerndomeinen bij downsyndroom [Vocabulary development related to socio-neurocognitive core developmental domains in Down syndrome]. Neuropraxis, 22(2), 52–59. https://doi.org/10.1007/s12474-018-0180-0
- Deckers, S. R. J. M., Van Zaalen, Y., Mens, E. J. M., Van Balkom, H., & Verhoeven, L. (2016a). The concurrent and predictive validity of the Dutch version of the Communicative Development Inventory in children with Down syndrome for the assessment of expressive vocabulary in verbal and signed modalities. Research in Developmental Disabilities, 56, 99–107. https://doi.org/10.1016/j.ridd.2016.05.017
- Deckers, S. R. J. M., Van Zaalen, Y., Stoep, J., Van Balkom, H., & Verhoeven, L. (2016b). Communication performance of children with Down Syndrome: An ICF-CY based multiple case study. Child Language Teaching and Therapy, 32(3), 293–311. https://doi.org/10.1177/0265659016630775
- Deckers, S. R. J. M., Van Zaalen, Y., Van Balkom, H., & Verhoeven, L. (2019). Predictors of receptive and expressive vocabulary development in children with Down syndrome. International Journal of Speech-Language Pathology, 21(1), 10–22. https://doi.org/10.1080/17549507.2017.1363290
- Dietz, A., Quach, W., Lund, S. K., & McKelvey, M. (2012). AAC assessment and clinical-decision making: The impact of experience. Augmentative and Alternative Communication, 28(3), 148–159. https://doi.org/10.3109/07434618.2012.704521
- Dunn, W. (2013). Sensory profile. Pearson Clinical.
- Fidler, D. J. (2005). The emerging Down syndrome behavioral phenotype in early childhood: Implications for practice. Infants & Young Children, 18(2), 86–103. https://doi.org/10.1097/00001163-200504000-00003
- Friederici, A. D. (2011). The brain basis of language processing: From structure to function. Physiological Reviews, 91(4), 1357–1392. https://doi.org/10.1152/physrev.00006.2011
- Friederici, A. D. (2017). Language in our brain: The origins of a uniquely human capacity. MIT Press.
- Hagoort, P. (2005). On Broca, brain, and binding: A new framework. Trends in Cognitive Sciences, 9(9), 416–423. https://doi.org/10.1016/j.tics.2005.07.004
- Hagoort, P. (2017). The core and beyond in the language-ready brain. Neuroscience & Biobehavioral Reviews, 81, 194–204. https://doi.org/10.1016/j.neubiorev.2017.01.048
- Hengst, J. A., Duff, M. C., & Jones, T. A. (2019). Enriching communicative environments: Leveraging advances in neuroplasticity for improving outcomes in neurogenic communication disorders. American Journal of Speech-Language Pathology, 28(1S), 216–229. https://doi.org/10.1044/2018_AJSLP-17-0157
- Henry, L. A. (2010). The episodic buffer in children with intellectual disabilities: An exploratory study. Research in Developmental Disabilities, 31(6), 1609–1614. https://doi.org/10.1016/j.ridd.2010.04.025
- Huizinga, M., & Smidts, D. P. (2012). BRIEF Vragenlijst executieve functies voor 5-tot 18-jarigen. Hogrefe Uitgevers.
- Hymes, D. (1972). On communicative competence. In JB Pride & J. Holmes (Eds.), Sociolinguistics. Selected Readings (pp 269–293). Harmondsworth.
- Johnson, M. H., & de Haan, M. (2011). The biology of change. Developmental Cognitive Neuroscience, 3, 1–22.
- Karmiloff-Smith, A., Al-Janabi, T., D'Souza, H., Groet, J., Massand, E., Mok, K., Startin, C., Fisher, E., Hardy, J., Nizetic, D., Tybulewicz, V., & Strydom, A. (2016). The importance of understanding individual differences in Down syndrome. F1000Research, 5, 389. https://doi.org/10.12688/f1000research.7506.1
- Ketelaar, M. (2002). Gross motor function measure (GMFM). Pelican Creative Communication.
- Koopman, L., Zijlstra, B. J. H., & Van der Ark, L. A. (2022). A two-step, test-guided Mokken scale analysis, for nonclustered and clustered data. Quality of Life Research, 31(1), 25–36. https://doi.org/10.1007/s11136-021-02840-2
- Light, J. C., Beukelman, D. R., & Reichle, J. (Eds.). (2003). Communicative competence for individuals who use AAC: From research to effective practice (Vol. 3). Paul H Brookes.
- Light, J. (1989). Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augmentative and Alternative Communication, 5(2), 137–144. https://doi.org/10.1080/07434618912331275126
- Light, J., & McNaughton, D. (2014). Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication? Augmentative and Alternative Communication, 30(1), 1–18. https://doi.org/10.3109/07434618.2014.885080
- Lynch, Y., & Murray, J. (2023). The I-ASC Explanatory Model as a Support for AAC Assessment Planning: A Case Report. In Martine M. Smith (Ed), Clinical Cases in Augmentative and Alternative Communication (pp. 12–26). Routledge.
- Loncke, F. (2022). Augmentative and alternative communication: Models and applications. Plural Publishing.
- MacDonald, S. (2017). Introducing the model of cognitive-communication competence: A model to guide evidence-based communication interventions after brain injury. Brain Injury, 31(13–14), 1760–1780. https://doi.org/10.1080/02699052.2017.1379613
- Mahone, E. M., Slomine, B. S., & Zabel, T. A. (2008). Neurodevelopmental disorders. Textbook of Clinical Neuropsychology, 105–127.
- Maris, G., Bechger, T., Koops, J., Partchev, I. (2022). dexter: Data management and analysis of tests, R package version 1.2.2 [Software]. https://dexter-psychometrics.github.io/dexter/
- McLeod, S., & Threats, T. T. (2008). The ICF-CY and children with communication disabilities. International Journal of Speech-Language Pathology, 10(1–2), 92–109. https://doi.org/10.1080/17549500701834690
- Miller, J. F., Leddy, M., & Leavitt, L. A. (1999). Improving the communication of people with Down syndrome. Paul H. Brookes.
- Miller, J. F., Sedey, A. L., & Miolo, G. (1995). Validity of parent report measures of vocabulary development for children with Down syndrome. Journal of Speech, Language, and Hearing Research, 38(5), 1037–1044. https://doi.org/10.1044/jshr.3805.1037
- Mokken, R. J. (1971). A theory and procedure of scale analysis with applications in political research. De Gruyter Mouton.
- Neil, N., & Jones, E. A. (2016). Communication intervention for individuals with Down syndrome: Systematic review and meta-analysis. Developmental Neurorehabilitation, 21(1), 1–12. https://doi.org/10.1080/17518423.2016.1212947
- Pasquini, L., Di Napoli, A., Rossi-Espagnet, M. C., Visconti, E., Napolitano, A., Romano, A., Bozzao, A., Peck, K. K., & Holodny, A. I. (2022). Understanding language reorganization with neuroimaging: How language adapts to different focal lesions and insights into clinical applications. Frontiers in Human Neuroscience, 16, 747215. https://doi.org/10.3389/fnhum.2022.747215
- Pieterse, M., & Treloar, R. (2009). Kleine stapjes. Early intervention [Small steps]. Stichting Downsyndroom.
- Polišenská, K., & Kapalková, S. (2014). Language profiles in children with Down syndrome and children with language impairment: Implications for early intervention. Research in Developmental Disabilities, 35(2), 373–382. https://doi.org/10.1016/j.ridd.2013.11.022
- Raghavendra, P., Olsson, C., Sampson, J., Mcinerney, R., & Connell, T. (2012). School participation and social networks of children with complex communication needs, physical disabilities, and typically developing peers. Augmentative and Alternative Communication (Baltimore, Md.: 1985), 28(1), 33–43. https://doi.org/10.3109/07434618.2011.653604
- Rasch, G. (1960). Probabilistic models for some intelligence and attainment tests. Danish Institute for Educational Research.
- Rauch, A., Wieczorek, D., Graf, E., Wieland, T., Endele, S., Schwarzmayr, T., Albrecht, B., Bartholdi, D., Beygo, J., Di Donato, N., Dufke, A., Cremer, K., Hempel, M., Horn, D., Hoyer, J., Joset, P., Röpke, A., Moog, U., Riess, A., & Strom, T. M. (2012). Range of genetic mutations associated with severe non-syndromic sporadic intellectual disability: An exome sequencing study. Lancet (London, England), 380(9854), 1674–1682. https://doi.org/10.1016/S0140-6736(12)61480-9
- Romeo, R. R., Flournoy, J. C., McLaughlin, K. A., & Lengua, L. J. (2022). Language development as a mechanism linking socioeconomic status to executive functioning development in preschool. Developmental Science, 25(5), e13227. https://doi.org/10.1111/desc.13227
- Rowland, C., & Fried-Oken, M. (2010). Communication matrix: A clinical and research assessment tool targeting children with severe communication disorders. Journal of Pediatric Rehabilitation Medicine, 3(4), 319–329. https://doi.org/10.3233/PRM-2010-0144
- Rowland, C., Fried-Oken, M., Steiner, S. A., Lollar, D., Phelps, R., Simeonsson, R. J., & Granlund, M. (2012). Developing the ICF-CY for AAC profile and code set for children who rely on AAC. Augmentative and Alternative Communication, 28(1), 21–32. https://doi.org/10.3109/07434618.2012.654510
- Schlosser, R. W., & Raghavendra, P. (2004). Evidence-based practice in augmentative and alternative communication. Augmentative and Alternative Communication, 20(1), 1–21. https://doi.org/10.1080/07434610310001621083
- Sherman, S. L., Allen, E. G., Bean, L. H., & Freeman, S. B. (2007). Epidemiology of Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews, 13(3), 221–227. https://doi.org/10.1002/mrdd.20157
- Simeonsson, R. J., & Rosenthal, S. L. (Eds.). (2001). Psychological and developmental assessment: Children with disabilities and chronic conditions. Guilford Press.
- Soto, G. (2012). Training partners in AAC in culturally diverse families. Perspectives on Augmentative and Alternative Communication, 21(4), 144–150. https://doi.org/10.1044/aac21.4.144
- Stoep, J., Deckers, S. R. J. M., Van Zaalen, Y., Van Balkom, H., & Verhoeven, L. (2012). Profiling communicative competence: A neurosociocognitive reasoning model for AAC assessment [Paper presentation]. ISAAC 2012 Conference, Pittsburgh, USA.
- Teachman, G., & Gibson, B. E. (2014). Communicative competence’ in the field of augmentative and alternative communication: A review and critique. International Journal of Language & Communication Disorders, 49(1), 1–14. https://doi.org/10.1111/1460-6984.12055
- Tomasello, M. (2008). Origins of human communication. MIT Press.
- Van Baar, A. L., Steenis, L. J. P., Verhoeven, M., Hessen, D. J., & Smits-Engelsman, B. C. M. (2015). Bayley-III-NL, Technische Handleiding [Technical Manual]. Pearson Assessment and Information B.V.
- Van Balkom, H., Deckers, S. R. J. M., & Stoep, J. (2017). Assessment of communicative competence in children with severe developmental disorders. In E. Segers & P. van den Broek (Ed.), Developmental perspectives in written language and literacy: In honor of Ludo Verhoeven. (pp. 412–439). John Benjamins Publishing Company.
- Van Balkom, H., Stoep, J., Deckers, S. R. J. M., & Van der Schuit, M. (2014). Profiling communicative competence: A neurosociocognitive reasoning model to guide decision-making in AAC assessment. ISAAC 2014 Conference.
- van Balkom, L. J. M. (2022). Elephant paths point the way to augmentative and alternative communication: Exploiting natural compensation in the brains and behaviour of people with multiple communicative disabilities. Radboud University Nijmegen.
- Van der Schuit, M., Segers, E., van Balkom, H., & Verhoeven, L. (2011). Early language intervention for children with intellectual disabilities: A neurocognitive perspective. Research in Developmental Disabilities, 32(2), 705–712. https://doi.org/10.1016/j.ridd.2010.11.010
- Van Duijn, G., Dijkxhoorn, Y., Noens, I., Scholte, E., & van Berckelaer-Onnes, I. (2009). Vineland screener 0–12 years research version (NL). Constructing a screening instrument to assess adaptive behaviour. International Journal of Methods in Psychiatric Research, 18(2), 110–117. https://doi.org/10.1002/mpr.282
- Van Duijn, G., Dijkxhoorn, Y., Scholte, E. M., & Berckelaer-Onnes, V. (2010). The development of adaptive skills in young people with Down syndrome. Journal of Intellectual Disability Research, 54(11), 943–954. https://doi.org/10.1111/j.1365-2788.2010.01316.x
- Van Langendonck, F., Willems, R. M., & Hagoort, P. (2018). Taking common ground into account: Specifying the role of the mentalizing network in communicative language production. PLoS One, 13(10), e0202943. https://doi.org/10.1371/journal.pone.0202943
- Verhelst, N. (1993). Itemresponsetheorie (item response theory). In T. J. H. M. Eggen & P.F. Sanders (Eds.), Psychometrie in de praktijk (Psychometrics in practice) (pp. 83–178). Cito.
- Visser-Bochane, M. I., Reijneveld, S. A., Krijnen, W. P., Van der Schans, C. P., & Luinge, M., R. (2020). Identifying milestones in language development for young children ages 1 to 6 years. Academic Pediatrics, 20(3), 421–429. https://doi.org/10.1016/j.acap.2019.07.003
- Waldman, M., McCoy, D. C., Seiden, J., Cuartas, J., & Fink, G., CREDI Field Team. (2021). Validation of motor, cognitive, language, and socio-emotional subscales using the caregiver reported early development instruments: An application of multidimensional item factor analysis. International Journal of Behavioral Development, 45(4), 368–377. https://doi.org/10.1177/01650254211005560
- Wetherby, A. M., & Prizant, B. M. (2002). Communication and symbolic behaviour scales: Developmental profile. Paul H Brookes Publishing.
- Willems, R. M., & Varley, R. (2010). Neural insights into the relation between language and communication. Frontiers in Human Neuroscience, 4(203), 203. https://doi.org/10.3389/fnhum.2010.00203
- World Health Organization (2007). International classification of functioning, disability, and health: Children and youth version: ICF-CY. World Health Organization.
- Yen, W. M. (1981). Using simultaneous results to choose a latent trait model. Applied Psychological Measurement, 5(2), 245–262. https://doi.org/10.1177/014662168100500212
- Zampini, L., & D'Odorico, L. (2013). Vocabulary development in children with Down syndrome: Longitudinal and cross-sectional data. Journal of Intellectual & Developmental Disability, 38(4), 310–317. https://doi.org/10.3109/13668250.2013.828833