Robert I. Gregerman, MD, a luminary in endocrine research and a pioneering investigator of the metabolic aspects of aging, died October 6, 2021, in San Antonio, Texas, at age 91 years. At the time of his death, following a protracted illness, he was at home, with family and hospice care members by his side. Dr. Gregerman leaves behind a distinguished legacy of academic accomplishment embodied in 60 years of innovative contributions to the medical literature and in generations of trainees who have themselves become leaders in the fields of endocrinology and biomedical gerontology.
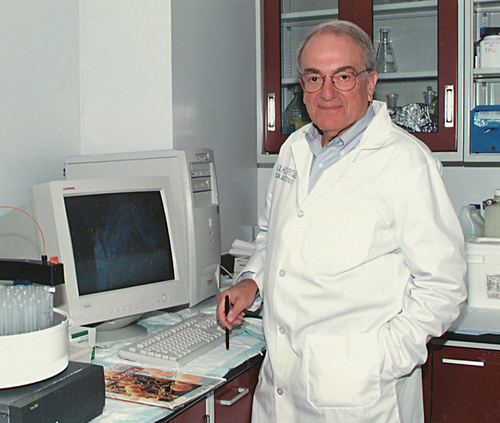
Robert (Bob) Gregerman () will be remembered as among the inaugural group of gifted scientists presciently recruited by Nathan W. Shock, PhD (1907–1989), to “grow” the first inter-disciplinary program on aging research at the National Institutes of Health (NIH). In 1956, as a newly minted commissioned officer in the United States Public Health Service (USPHS), Bob arrived at Dr. Shock’s brainchild, then known as the Gerontology Branch of the National Heart Institute and a uniquely creative hybrid of a research enterprise–operating administratively as a unit within the NIH, housed on the grounds of the Baltimore City Hospitals (BCH) and affiliated academically with the Johns Hopkins University School of Medicine several miles away. By 1961, Bob had become the founding chief of the Endocrine Section within the Gerontology Branch, which in 1968 moved into its own NIH-financed building, designated the Gerontology Research Center (GRC), on the BCH campus, and subsequently matured into the intramural research program of the National Institute on Aging (NIA) established in 1974. Bob Gregerman’s laboratory at the GRC remained at the forefront of investigations into the endocrinology of aging for another two decades, during which time he was promoted to Professor of Medicine at Johns Hopkins. Then, in 1994, following retirement from the USPHS he moved with his wife Marjorie to San Antonio, Texas (), to direct the research programs of the San Antonio Geriatric Research, Education and Clinical Center (GRECC) at the Audie L. Murphy Memorial Veterans Hospital, and with an appointment as Professor of Medicine at the affiliated University of Texas Health Science Center at San Antonio (UTHSCSA). In San Antonio, he extended the research inquiries he had long pursued in Baltimore, until formal retirement in 2011 afforded him time and opportunity for his favored activities, namely, visiting the UTHSCSA medical library to keep abreast of the literature and conferring with former trainees and colleagues over advances in the biology and endocrinology of aging. Many years earlier, he had written, “my field always serves as a reminder of the finiteness of time.”Citation1 In the last years of his life (), then, when his scientific endeavors, and his delight in pursuing them, did recede under the assaults of time, it likely came to him with regret but as no great surprise.
For those who admired Bob Gregerman and considered his influence a constant in their lives, there remains the science, the work, the striving for a kind of benevolent truth. The substance of his scientific contributions represents a progression of illuminating discoveries anticipating, and in many cases directly generating, research trends in endocrinology and aging. Over many years, for example, his research focus on thyroid physiology introduced findings that continue to inform concepts of thyroid hormone metabolism during aging and illness. In early collaboration with Nathan Shock, Bob conducted kinetic studies of thyroxine (T4) turnover in healthy men, demonstrating a 50% decrease of T4 degradation over the adult age span of 20–80 years.Citation2 He reasoned that this finding, together with earlier observations of generally stable T4 blood levels yet reduced thyroid accumulation of radioiodide with age, in turn implied that levothyroxine replacement dosage requirement for hypothyroidism should be decreased in older individuals – an hypothesis subsequently confirmed in multiple clinical studies and discussed under current guidelines for the treatment of hypothyroidism in the elderly.Citation3–5
In later work, Bob extended his studies of thyroid hormone metabolism in humans to states of nonthyroidal illness, showing that, unlike the case with aging, peripheral disposal of T4 is accelerated (if not invariably so) during the course of acute infectious illnesses.Citation6,Citation7 The same studies revealed infection-related increases in circulating concentrations of free T4 (FT4) unassociated with changes in concentrations of thyroid hormone-binding proteins, suggesting the appearance of inhibitors of T4 binding during the stress of infection.Citation7 Other findings from the Gregerman laboratory implicated inhibition of T4 binding by small molecular weight compounds circulating at elevated concentrations in disease states, such as chronic renal failure.Citation8 And in a landmark report in 1985,Citation9 Bob and his colleagues were the first to demonstrate convincingly that suppressed pituitary secretion of thyrotropin plays a primary role in contributing to reduced circulating levels of thyroid hormones observed in critical illness. The three alterations in thyroid hormone economy – accelerated T4 degradation, inhibition of T4 binding to thyroid hormone-binding proteins, and suppression of thyrotropin – that Bob Gregerman described in association with infection and severe illness have, over the years, become recognized as among the principal phenomena underlying the multiplicity of abnormal thyroid functions occurring in patients with nonthyroidal illness and termed the nonthyroidal illness syndrome (NTIS).Citation10 In a later study appearing in Endocrine Research,Citation11 Bob reported on patients with a subset of NTIS occurring during acute psychiatric illness, mainly depression, and in whom elevated thyroid hormone levels appeared to result from centrally mediated thyrotropin hypersecretion.
During Bob’s “thyroid” years, as during the entirety of his investigative career, he provided his trainees a research environment promoting individualized creativity, free from dogma. He encouraged his postdoctoral fellows to seek out their own independent interests, and yet their subsequent research accomplishments – predictably maturing over many years following their period of formal training – often as not reflected unexpected consequences of their early work in Bob’s laboratory. One of the authors of this reminiscence (P.J.D.) has recollected that, when he entered his postdoctoral fellowship with Bob Gregerman, “there wasn’t any way to prepare for how interested Bob would be in trainees as individual people. Or how interested he was in sound, beyond party-line, concepts. He was conceptual and he wanted us to be conceptual and it was good to be out-of-the-box.”Footnotea The author further recalls that his studies in the Gregerman laboratory characterizing properties of thyroid hormone-binding proteinsCitation12,Citation13 introduced him to tetraiodothyroacetic acid (tetrac), a thyroxine metabolite bound to prealbumin (now termed transthyretin, TTE) in the circulation, and laid the groundwork for identifying the cancer cell surface integrin αvβ3 receptor for thyroid hormone analogues; observations that native and modified tetrac formulations exert anti-cancer actions at αvβ3Citation14 have in turn led to the development of a tetrac-based chemotherapeutic agent currently in Phase 1 clinical testing against glioblastoma. Bob’s nonparty-line way of thinking, and its influence on his colleagues, was particularly evident in his clinical approach to thyroid nodules: while the late-twentieth century literature on thyroid nodules developed generally in directions of increasingly zealous diagnostic and treatment protocols, Bob Gregerman – in his writings,Citation15,Citation16 lectures, and interactions with trainees in his endocrine teaching clinic at the BCH – fostered a more conservative and tailored approach to thyroid nodules that recognized the clinically nonaggressive nature of most differentiated thyroid cancers. As one of Bob’s trainees (J.D.S.) was to describe his clinical influence, “I thank him frequently when I recall his adage that the job of the endocrinologist is to keep patients from thyroid surgeons.” (On a more serious note, the same trainee went on to describe Bob as “a brilliant thinker and a first-class educator.”) It is tempting to think that some of the more nuanced approaches to the management of thyroid nodules emerging in the 21st century (including observation of low-risk thyroid cancers) may reflect, even if indirectly, the influence of seasoned thyroidologists like Bob Gregerman, calling for caution and clinical practices that “do no harm.”
Along the way, Bob applied his clinical and biochemical expertise to other substantive advances in the understanding of human aging, disease, diagnostic testing, and therapeutics. In a 1971 publication in the New England Journal of Medicine, he described water intoxication in five older patients treated for type 2 diabetes mellitus with sulfonylurea (chlorpropamide). Not only was this the first example of drug-induced syndrome of inappropriate diuresis (SIAD) to enter the literature, but the fact that all of the affected patients were elderly also prompted Bob and his coauthors to hypothesize that regulation of vasopressin secretion from the posterior pituitary might be disrupted during aging.Citation17 In subsequent investigations prompted by Bob’s clinical report, colleagues at the GRC determined that vasopressin secretion by osmolar loading was greater in old subjects than in young, confirming Bob’s earlier suggestion of altered osmoreceptor sensitivity during aging.Citation18 In other studies Bob developed an early plasma renin activity (PRA) assay,Citation19 the principles of which have generally been incorporated over the years into current clinical laboratory measurements of PRA widely used in the investigation of primary (and secondary) aldosteronism. Related research into biochemical markers for hypertension led Bob to publish a fluorescence assay for the histidylleucine dipeptide cleaved from angiotensin I by the enzyme angiotensin converting enzyme (ACE) in the production of angiotensin II.Citation20 This assay was subsequently employed by the pharmaceutical industry to evaluate and develop compounds inhibitory to the converting enzyme, including the ACE inhibitor class of drugs that have become a mainstay in the treatment of hypertension and heart failure.Citation21,Footnoteb
In the 1970s Bob Gregerman directed his attention to the study of age-related alterations of hormone action. At the time, a series of discoveries had recently opened up, or were in the process of enabling, vast avenues of inquiry into molecular mechanisms underlying the cellular actions of hormones – a field of cell biology that would become known as “signal transduction.” In 1971, Earl Sutherland had been awarded the Nobel Prize in Physiology or Medicine for his discovery of cyclic adenosine monophosphate (cyclic AMP), the intracellular “second messenger” mediating the actions of a multiplicity of hormones and neurotransmitters (as “first” messengers) acting through as yet uncharacterized receptors on the plasma membrane of target cells. Martin Rodbell and colleagues, who had just published a highly sensitive assay for the adenylate cyclase enzyme found to generate cyclic AMP from ATP,Citation22,Footnotec reported that hormone actions on adenylate cyclase were modulated by guanine nucleotides. This observation, together with Alfred G. Gilman’s independent identification of a guanine nucleotide dependent “regulatory component” of adenylate cyclase, led to the discovery of guanine nucleotide-binding proteins (G proteins) and their role in signal transduction (and for which Rodbell and Gilman shared the Nobel Prize in Physiology or Medicine in 1994). At the same time Robert J. Lefkowitz was just beginning his studies of β-adrenergic receptors (β-ARs) that would earn him, together with his former fellow Brian Kobilka, the 2012 Nobel Prize in Chemistry for their elucidation of the structure and workings of a family of G protein-coupled receptors typified by the β2-AR. Amid the excitement generated by the burgeoning field of signal transduction in the 1970s and thereafter, Bob Gregerman understood that the impact of aging on hormone action was, for the first time, an area amenable to critical study. His laboratory in those years is remembered by his trainees and colleagues of the time as a place of heady excitement and possibility.
Bob was not averse to descriptive “phenomenology”; but neither was he an advocate of applying technology merely to catalog age-related changes in hormone action across multiple systems, indiscriminately or without analytical rigor. Nor was he put off by complexity, rather he embraced it: as a colleague (S.M.H.) later commented, Bob would caution that “one should not always be satisfied with the simplest explanation.” Nowhere were these traits more evident than in his contributions to the literature on hormone action during aging, focused largely on adenylate cyclase-linked signal transduction pathways underlying metabolic functions in fat cells and liver. As the first to apply the Salomon assay of adenylate cyclase to studies of aging,Footnoted he demonstrated in early experiments with rat adipocytes three distinct patterns of enzyme stimulation by lipolytic agents during aging – different rates of decline over the life span in adenylate cyclase responses to ACTH and glucagon, respectively, but without evident age-related change in enzyme responsiveness to the mixed (i.e., acting at both β- and α-ARs) catecholamine epinephrine.Citation3,Citation24 In contrast, data emerging from the Gregerman laboratory and others showed that epinephrine stimulation of lipolysis, unlike adenylate cyclase, in rat adipocytes did decline with age; and Bob devoted subsequent efforts to defining the signaling loci responsible for the loss of lipolytic response to catecholamine.Citation25 Work from his laboratory ultimately clarified just how complex the explanation might be for an aging phenomenon such as loss of epinephrine stimulated lipolysis in rat adipocytes. In an experimental study accompanied by a MiniReview published in the Journal of Gerontology,Citation26,Citation27 he laid out evidence for multifactorial, fat depot-specific signaling changes mediating reduced epinephrine responsiveness during aging. On the one hand, the decreased response in epididymal fat cells appeared to reflect the emergence with age of an epinephrine sensitive inhibitory pathway acting via α-AR inhibition of adenylate cyclase (notably, experimental conditions in previous studies had likely prevented detection of α-AR mediated enzyme inhibition). In perirenal adipocytes, however, reduced catecholamine response appeared to be due to an age-related defect in the distal lipolytic pathway, namely, in the action of cyclic AMP on triglyceride lipase; a similar defect had been reported by others in human subcutaneous fat cells during aging.Citation28 Bob Gregerman’s work on catecholamine action in rat fat cells during aging, especially his MiniReviewCitation27 reconciling the disparate findings in the literature on this subject, is a model of coherence and highlights the principles he and his early contemporaries at the GRC developed to recognize and deal with the confounders confronting biomedical research on aging – distinctions between maturation and senescence; observations specific to animal species and strain, tissue (including localization, in the case of fat), and/or experimental conditions; and the tenuousness of extrapolating from animal “models” to human aging (see also ref. 3). In this latter regard, the degree to which changes in hormone action demonstrated in rat fat mirror those occurring with age in humans remains to be fully explored.
Turning to studies of hormone action in liver, Bob and his colleagues determined that catecholamine stimulation of adenylate cyclase in rat liver increased with senescent aging – a unique, tissue-specific finding in that in other mammalian target organs catecholamine responsive adenylate cyclase activity has generally been found to decrease or remain unchanged with age.Citation3,Citation29 Subsequent work from the Gregerman laboratory traced the age-related increase in hepatic enzyme responsiveness to catecholamines mainly to an increase in stimulatory β-ARs, although at advanced ages β-AR numbers continued to increase without further change in adenylate cyclase activation. Evidence suggested that the “uncoupling” of β-ARs from adenylate cyclase in extreme old age may reflect changes in the physical-chemical properties of the plasma membrane in which the β-AR/G protein/adenylate cyclase complex resides.Citation30 This suggestion remains a provocative, though little explored, possibility. Nonetheless, post-maturational accumulation of hepatic β-ARs functionally linked to (stimulation of) adenylate cyclase in liver plasma membranes appears sufficient to contribute to increased β-AR agonist mediated glycogenolysis and steatosis in hepatocytes from aging rodents.Citation31,Citation32 Questions of whether these observations in rodent models of aging might translate to pathophysiological mechanisms and novel therapeutic strategies relevant to metabolic disorders of human aging, such as type 2 diabetes mellitus and nonalcoholic fatty liver disease, have informed the research of two generations of investigators influenced (directly or indirectly) by Bob Gregerman.Footnotee
In late-career Bob extended his work on hormone responsiveness of adipocytes during aging to investigate the regulatory control of adipocyte differentiation and its potential role in age-related disease. His group pioneered the description of adipocyte-secreted factor(s) driving differentiation of adipose tissue-derived stem cells (“preadipocytes”) into mature adipocytes.Citation33 He further demonstrated that an age-related reduction in the ability of rat preadipocytes to differentiate was due, not to an intrinsic stem cell defect, but rather to a decline with age in the production of differentiation-promoting factor(s) by adipocytes.Citation34 Although initial evidence suggested that an adipocyte-secreted protein factor was responsible for the promotion of preadipocyte differentiation, in subsequent work it became clear to him that the adipogenic effect exerted by mature fat cells was attributable to fatty acids.Citation35 In his final publication, he and his coauthors presented findings in cultured osteoblast-like cells suggesting that inhibition of fatty acid induced adipogenesis in bone marrow progenitors might play a role in the ability of melatonin to promote osteogenesis – provocative results with pathogenetic and therapeutic implications for decreased marrow stromal cell osteoblastogenesis and the development of osteoporosis with advancing age.Citation35 Although Bob’s direct contributions to the literature concerning the paracrine influence of adipocytes on adipogenic progenitors were – regrettably – to end here, his lasting influence on the field remains readily evident, e.g., in a recent, comprehensive review of the subject.Citation36
As one whose life of scientific inquiry inspired so many, Bob Gregerman had his own sources of inspiration; and in that these influences shaped the man we admired, they warrant our attention – at least to the extent that they are known. In Bob’s obituary, his family pointed out that in his youth “he was inspired to pursue a career as a scientist upon reading Sinclair Lewis’s novel Arrowsmith.”Citation37 We recall that Martin Arrowsmith endured a lifetime of professional disappointment and personal heartbreak in perpetual search of a research environment conducive to biomedical investigation, without restraint. Early on he encountered his signature research mentor, Professor Max Gottlieb. As an undergraduate at Harvard College Bob Gregerman gravitated to his own Max Gottlieb – in the person of George Wald, in whose laboratory Bob apprenticed during research electives and summer holidays. Working with Wald and colleagues Bob participated in studies identifying isomers of retinalCitation38 found to play a role in vision and thereby contributing to Wald’s discoveries on the chemistry of visual processes for which he was awarded the 1967 Nobel Prize for Physiology or Medicine. Over Bob’s entire adult life he held fond memories of learning and applying biochemistry under George Wald’s guidance. Also, whereas Bob may not have sustained the repeated disillusionments of a Martin Arrowsmith, he similarly pursued an environment in which he could conduct biomedical research without impediment. And in Bob’s case, to the degree possible in academic medicine, he probably did identify those circumstances most conducive to study endocrine systems during aging – the GRC at the NIH, and subsequently the GRECC system within the Department of Veterans Affairs. Bob was certainly a realist, however, and recognized the limitations of even the most favorable research environments. In this way, he went a step further than his literary role model, possibly emulating an influence experienced earlier in the Wald laboratory. Bob Gregerman created for his trainees and colleagues the kind of individualized, even idealized, research environment he recognized would be essential to the early growth of their creativity and their careers. One of his close colleagues (G.S.R.) recalled, “Bob was … an oasis of decency, compassion, sanity, and stability in an often indifferent, and sometimes even hostile, desert of a bureaucracy.” A postdoctoral fellow (M.R.H.) at the GRC in the ‘70s, who went on to a standout career in academic medicine, put it simply, “My NIH years were one of the happiest times of my life. [Bob was] a part of that.”
Bob Gregerman’s approach to science and medicine, and to a lifetime of inquiry, was – we suspect – further an expression of his earliest upbringing and familial traditions. Born in Boston in 1930, he was the third son of Russian Jewish immigrant parents. In this context, his rigorous curiosity, intellectual honesty, and dedication to mentoring those under his tutelage all appear to us to exemplify the Talmudic principle of tikkun olam, generally translated as “repairing the world,” the obligation to attempt to make the world a better place. This characteristic, while not unique to Bob Gregerman (it appears among descriptions of the influences guiding the careers of other prominent contemporary medical scientists [see, e.g., ref. Citation39]), serves to highlight his academic career and achievements within a broader framework of respect for humanity, i.e., to understand, explain and apply natural phenomena will ultimately serve to improve society and alleviate suffering. Bob’s investigations into biological phenomena, then, were integral to a life of conscience and response to injustice, whether taking up for an individual laboratory intern subjected to rough interrogation by local authorities or advocating for a generation of Soviet Jewish scientists seeking freedom to emigrate. As a longtime friend (S.M.H.) wrote at the time of Bob’s death, “I never remember him becoming angry except at injustice.” We see Bob Gregerman as equally obligated, above all and without ego, to the integrity of the objective truths he sought in science. When a colleague (G.S.R.) observed that “Bob never received the credit he deserved” (for research that was “well ahead of the curve”), another (S.M.H.) countered, “While that is certainly true, I don’t think it bothered him much. What he cared about was getting it right, not who got the kudos.”
In the Foreword to her book on the artist Niki de Saint Phalle, Nicole Rudick writes on the nature of memoir and biography: she notes that “the accounting of a life is not the simple accounting of facts,” and asks, “What is the truth of a person anyway?”; she recalls a biographical work that is, “ … more than the story of one man’s life; it is also the story … of the deep, often invisible connectedness of one life to many others.”Citation40 In like manner, and as must be obvious, we feel that the importance of Bob Gregerman’s influence on the endocrinology of aging is not to be found solely in his publications summarized in this reminiscence, but rather more generally in the role he played in the professional, and personal, lives connected to his. Quoting again from a close colleague (G.S.R.), “his insightful creativity and lessons in objectivity, critical thinking, and scientific rigor will always live on in the work of those he touched, and those who follow us.”
The “connectedness,” or conduit, through which Bob touched so many was exerted, in the end, through those aspects of his nature perhaps best exemplified by his humor and his decency. Many of the e-mailed memories elicited at the time of Bob’s death recalled his humor – as examples only, “I admired his intellect and humor immensely” (W.B.G.); “I loved his humor punctuated often by a wry smile and glimmer in his eyes” (J.F.N.); “one thing in particular that I found endearing was his unique little laugh” (R.J.W.); “I admired Bob for … his infectious capability of laughing at himself” (D.D.S.). Bob’s wit ran from archly ironic to screwball ridiculous, never at another’s expense, however, and never mean-spirited. On his office wall, he kept a photograph of Alec Guinness as prisoner-of-war Colonel Nicholson in the 1957 film The Bridge on the River Kwai – the actor depicted in tattered officer’s garb, with the caption (a quote from the commandant of the POW camp in the film), “BE HAPPY IN YOUR WORK.” At the other end of the spectrum, in a late telephone conversation with one of the authors of this article (M.S.K.), Bob chuckled over an image retained from his ‘30s childhood – the nameless, bearded Little Hitchhiker from Gene Ahern’s syndicated comic The Squirrel Cage, never wavering from a single, inscrutable utterance, “Nov shmoz ka pop?”Citation41 Bob’s humor was most prominently, and publicly, displayed in 1969, when the author of the present reminiscence (P.J.D.) and he published a tongue-in-cheek “Special Article” in the New England Journal of Medicine parsing the productivity, even the entire careers, of medical investigators to two-digit decimal numbersCitation42; while not generally known for its sense of humor, the Journal went on in 1995 to publish the same authors’ follow-up piece on “parse analysis II,”Citation43 in which additional, seemingly nonsensical, analyses were introduced to account for contingencies arising in the quarter century following the original opinion piece.Footnotef
E-mailed condolences also focused on Bob’s humanity and kindness. Typical among shared memories were his “care for others” (J.F.N.) and his “warmth and generosity of spirit” (Z.L.); one colleague wrote, “He was my mentor, colleague, and most of all he was my dear friend” (Z.L.). Bob was a magnificent listener and observer, and he had an instinct for offering unobtrusive yet frank help to those in need. In this regard what was left unsaid by the many correspondents sharing thoughts electronically at the time of Bob’s death was most telling; his humanity, we believe, lay in the grateful memories held privately by all those who benefited from it. One understated comment encapsulated a basic “truth” that was Bob Gregerman: “A soft spoken man whose statements were of great value and import” (J.D.S.).
So we remember Bob Gregerman – for his scholarship, his creativity, his mentorship, and his menschlichkeit. We each carry him within us: whenever we reason with deliberation, or approach a question with objectivity and humility, or speak or write with clarity, or when we laugh with another or extend a hand in our shared existence, we are grateful for Bob’s guidance. Even in continued sadness over his loss, we celebrate his life, lived with joyful curiosity and essential decency.
Acknowledgments
The authors thank Marjorie Gregerman and daughters Lisa Gregerman and Debra Gregerman, whose eloquent obituary for Bob Gregerman provided source material for this reminiscence, and for sharing family memories, photographs, articles, and notes that were also essential in the preparation of this manuscript. We are grateful to Bob Gregerman’s (and our) colleagues and friends–Marsha C. Bol, Arthur Chernoff, Elizabeth M. Dax, William B. Greenough III, Marc R. Hammerman, S. Mitchell Harman, Erik L. Hewlett, Thomas M. Kelly, James L. Kirkland, Zhongding Lu, James F. Nelson, George S. Roth, Michele J. Saunders, Douglas D. Schocken, John D. Sorkin, Robert J. Workman—whose shared memories at the time of Bob’s death we have quoted extensively; we regret only not being able to incorporate more of their fond recollections. We acknowledge Sabine Schulze-Steele for allowing us access to her copy of Nicole Rudick’s book on Niki de Saint Phalle (ref. Citation40) and its insights into the nature of biography. We are also indebted to Christine Gaspard, Associate Director for Liaison Services, UT Health Briscoe Library, San Antonio, TX, for help in assembling Bob Gregerman’s bibliography and citations (with only minimal parsing).
Disclosure statement
The authors report there are no competing interests to declare.
Notes
a This and subsequent quotations are from e-mail communications circulated among Bob Gregerman’s former fellows, other colleagues, and friends on the occasion of his death on October 6, 2021, and in some cases from earlier messages celebrating his 91st birthday on April 18, 2021. Attributions of other quotations in this manuscript are shown in parentheses by initials of individual correspondents whose names are included under Acknowledgments.
b The interested reader is referred to reference 21, an in-depth profile of Dr. Gregerman with interview, also for additional details of his life, career, and research accomplishments extending those described in the present manuscript.
c The adenylate cyclase assay developed in Rodbell’s laboratory came to be known colloquially as “the Salomon assay”, after Yoram Salomon, the first author of the paper describing the assay, and to distinguish it from earlier, less sensitive assays.
d It should be noted here that, in setting up the Salomon assay in his laboratory, Bob Gregerman directed his initial experiments with this methodology to demonstrate guanine nucleotide dependence of epinephrine sensitive adenylate cyclase in human adipocytes.Citation23 To our knowledge, this was the first such demonstration in human cells.
e See reference Citation32 and reference citations contained therein to earlier work by the same authors.
f Although “parse analysis”, as originally detailed by Davis and Gregerman,Citation42 was intended as parody, it turned out to be prophetic in that subsequent scholarly analyses of authors’ contributions to the medical literature – in some cases citing the parse piece as serious precedent (!) – have over time led to present day methodologies reducing published research productivity to formulaic simplifications used in evaluating medical faculty, e.g., for promotion and tenure. Interestingly, “parse analysis II”Citation43 humorously accommodated to developing issues of multi-authorship, proliferation of scientific journals (including those published electronically), and publication fraud – all presaging by many years very real dilemmas now faced by readers of research publications.
References
- Gregerman RI. Robert Isaac Gregerman. Harvard Class of 1951 25th Anniversary Report. Harvard University Alumni Publications: Boston, MA. 1976. 372–374.
- Gregerman RI, Gaffney GW, Shock NW. Thyroxine turnover in euthyroid man with special reference to changes with age. J Clin Invest. 1962;41(11):2065–2074. doi:10.1172/JCI104664. PMID: 13950233.
- Gregerman RI. Mechanisms of age-related alterations of hormone secretion and action. An overview of 30 years of progress. Exp Gerontol. 1986;21(4–5):345–365. doi:10.1016/0531-5565(86)90042-2. PMID: 3028848.
- Davis FB, LaMantia RX, Spaulding SW, Wehmann RE, Davis PJ. Estimation of a physiologic replacement dose of levothyroxine in elderly patients with hypothyroidism. Arch Intern Med. 1984;144(9):1752–1754. doi:10.1001/archinte.1984.00350210064009. PMID: 6433829.
- Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism. Prepared by the American Thyroid Association Task Force on Thyroid Hormone Replacement. Thyroid. 2014;24(12):1670–1751. doi:10.1089/thy.2014.0028. PMID: 25266247.
- Gregerman RI, Solomon N. Acceleration of thyroxine turnover during bacterial pulmonary infections and fever: implications for the functional state of the thyroid during stress and in senescence. J Clin Endocrinol Metab. 1967;27(1):93–105. doi:10.1210/jcem-27-1-93. PMID: 4163768.
- Lutz JH, Gregerman RI, Spaulding SW, Hornick RB, Alberts AT. Thyroxine binding proteins, free thyroxine and thyroxine turnover interrelationships during acute infectious illness in man 1. J Clin Endocrinol Metab. 1972;35(2):230–249. doi:10.1210/jcem-35-2-230. PMID: 4627324.
- Spaulding SW, Gregerman RI. Free thyroxine in serum by equilibrium dialysis: effects of dilution, specific ions and inhibitors of binding. J Clin Endocrinol Metab. 1972;34(6):974–982. doi:10.1210/jcem-34-6-974. PMID: 5020425.
- Wehmann RE, Gregerman RI, Burns WH, Saral R, Santos GW. Suppression of thyrotropin in the low-thyroxine state of severe nonthyroidial illness. N Engl J Med. 1985;312(9):546–552. doi:10.1056/NEJM198502283120904. PMID: 3881675.
- Boelen A, Langouche L, Wiersinga W, Van den Berghe G. Nonthyroidal illness syndrome. In: Braverman LE, Cooper DS, Kopp PA, eds. Werner & Ingbar’s The Thyroid. A Fundamental and Clinical Text. 11th ed. Baltimore, MD: Wolters Kluwer; 2021:214–229.
- Roca RP, Blackman MR, Ackerley MB, Harman SM, Gregerman RI. Thyroid hormone elevations during acute psychiatric illness: relationship to severity and distinction from hyperthyroidism. Endocr Res. 1990;16(4):415–447. doi:10.1080/07435809009107116. PMID: 2129342.
- Davis PJ, Spaulding SW, Gregerman RI. The three thyroxine-binding proteins in rat serum: binding capacities and effects of binding inhibitors. J Clin Endocrinol Metab. 1970;87(5) :978–986. doi:10.1210/endo-87-5-978. PMID: 4991673.
- Davis PJ, Handwerger BS, Gregerman RI. Thyroid hormone binding by human serum prealbumin (TBPA). J Clin Invest. 1972;51(3):515–521. doi:10.1172/JCI106839. PMID: 4110898.
- Davis PJ, Mousa SA, Lin H-Y. Nongenomic actions of thyroid hormone: the integrin component. Physiol Rev. 2021;101(1):319–352. doi:10.1152/physrev.00038.2019. PMID: 32584192.
- Gregerman RI. Solitary thyroid nodules. N Engl J Med. 1993;329(5):360. doi:10.1056/NEJM199307293290514. PMID: 8321268
- Gregerman RI. Thyroid disorders. In: Barker LR, Burton JR, Zieve PD, eds. Principles of Ambulatory Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:1230–1263.
- Weissman PN, Shenkman L, Gregerman RI. Chlorpropamide hyponatremia. Drug-induced inappropriate antidiuretic-hormone activity. N Engl J Med. 1971;284(2):65–71. doi:10.1056/NEJM197101142840202. PMID: 5538636.
- Helderman JH, Vestal RE, Rowe JE, Tobin JD, Andres R, Robertson GL. The response of arginine vasopressin to intravenous ethanol and hypertonic saline in man: the impact of aging. J Gerontol. 1978;33(1):39–47. doi:10.1093/geronj/33.1.39. PMID: 618965.
- Gregerman RI, Kowatch MA. Double isotope derivative assay for angiotensin I: use for renin measurement. J Clin Endocrinol Metab. 1971;32(1):110–114. doi:10.1210/jcem-32-1-110. PMID: 4321495.
- Gregerman RI. Identification of histidylleucine and other histidyl peptides as normal constituents of human urine. Biochem Med. 1967;1(2):151–167. doi:10.1016/0006-2944(67)90004-X.
- Robert I. Gregerman. Advancing Gerontology Research. U.S. Medicine. 2000(Aug):38–39
- Salomon Y, Londos C, Rodbell M. A highly sensitive adenylate cyclase assay. Anal Biochem. 1974;58(2):541–548. doi:10.1016/0003-2697(74)90222-x. PMID: 4827395.
- Cooper B, Partilla JS, Gregerman RI. Adenylate cyclase of human fat cells. Expression of epinephrine-sensitive activation revealed by 5’-guanylyl-imidodiphosphate. J Clin Invest. 1975;56(5):1350–1353. doi:10.1016/0005-2744(76)90177-7. PMID: 8140.
- Cooper B, Gregerman RI. Hormone-sensitive fat cell adenylate cyclase in the rat. Influences of growth, cell size, and aging. J Clin Invest. 1976;57(1):161–168. doi:10.1172/JCI108256. PMID: 173740.
- Dax EM, Partilla JS, Gregerman RI. Mechanism of the age-related decrease of epinephrine-stimulated lipolysis in isolated rat adipocytes: β-adrenergic receptor binding, adenylate cyclase activity, and cyclic AMP accumulation. J Lipid Res. 1981;22(6):934–943. doi:10.1016/S0022-2275(20)37331-4. PMID: 6268727.
- Carraro R, Li Z-h, Gregerman RI. Catecholamine-sensitive lipolysis in the rat: different loci for effect of age on the lipolytic cascade in epididymal vs perirenal fat cells. J Gerontol. 1994;49(4):B140–B143. doi:10.1093/geronj/49.4.b140. PMID: 8014385.
- Gregerman RI. MINIREVIEW. Aging and hormone-sensitive lipolysis: reconciling the literature. J Gerontol. 1994;49(4):B135–B139. doi:10.1093/geronj/49.4.b135. PMID: 8014384.
- Lonnqvist F, Nyberg B, Wahrenberg H, Arner P. Catecholamine-induced lipolysis in adipose tissue of the elderly. J Clin Invest. 1990;85(5):1614–1621. doi:10.1172/JCI114612. PMID: 2159025.
- Kalish MI, Katz MS, Pineyro MA, Gregerman RI. Epinephrine- and glucagon-sensitive adenylate cyclases of rat liver during aging. Evidence for membrane instability associated with increased enzymatic activity. Biochim Biophys Acta. 1977;483(2):452–466. doi:10.1016/0005-2744(77)90073-0. PMID: 889839.
- Dax EM, Partilla JS, Pineyro MA, Gregerman RI. β-Adrenergic receptors, glucagon receptors, and their relationship to adenylate cyclase in rat liver during aging. Endocrinology. 1987;120(4):1534–1541. doi:10.1016/0005-2744(77)90073-0. PMID: 889839.
- Katz MS, Dax EM, Gregerman RI. Beta adrenergic regulation of rat liver glycogenolysis during aging. Exp Gerontol. 1993;28(4–5):329–340. doi:10.1016/0531-5565(93)90060-q. PMID: 8224032.
- Shi Y, Pizzini J, Wang H, et al. β2 -Adrenergic receptor agonist induced hepatic steatosis in mice: modeling nonalcoholic fatty liver disease in hyperadrenergic states. Am J Physiol Endocrinol Metab. 2021;321(1):E90–E104. doi:10.1152/ajpendo.00651.2020. PMID: 34029162.
- Li Z-H, Lu ZD, Kirkland JL, Gregerman RI. Preadipocyte stimulating factor in rat serum: evidence for a discrete 63 kDa protein that promotes cell differentiation of rat preadipocytes in primary cultures. J Cell Physiol. 1989;141(3):543–557. doi:10.1002/jcp.1041410313. PMID: 2687298.
- Carraro R, Li Z-H, Johnson JE, Gregerman RI. Adipocytes of old rats produce a decreased amount of differentiation factor for preadipocytes derived from adipose tissue islets. J Gerontol. 1992;47(6):B195–B201. doi:10.1093/geronj/47.6.b198. PMID: 1430848.
- Sanchez-Hidalgo M, Lu Z, Tan D-X, Maldonado MD, Reiter RJ, Gregerman RI. Melatonin inhibits fatty acid-induced triglyceride accumulation in ROS17/2.8 cells: implications for osteoblast differentiation and osteoporosis. Am J Physiol Regul Integr Comp Physiol. 2007;292(6):R2208–R2215. doi:10.1152/ajpregu.00013.2007. PMID: 17379847.
- Haylett WL, Ferris WF. Adipocyte-progenitor cell communication that influences adipogenesis. Cell Mol Life Sci. 2020;77(1):115–128. doi:10.1007/s00018-019-03256-5. PMID: 31352534.
- Obituary: Gregerman, Dr. Robert Isaac. The Baltimore Sun. Oct 9, 2021; 11.
- Hubbard R, Gregerman RI, Wald G. Geometrical isomers of retinene. J Gen Physiol. 1953;36(3):415–429. doi:10.1085/jgp.36.3.415. PMID: 13022935.
- Rieland R. Giants of the genome field. Johns Hopkins Magazine. 2022; 74(Spring, No. 1):38–45.
- Rudick N. What Is Now Known Was Once Only Imagined: An (Auto)biography of Niki de Saint Phalle. Catskill, NY: siglio. 2022:9–14.
- Spiegelman A. Foolish questions. New York Rev Books. 2020; 67(No. 4):9–12.
- Davis PJ, Gregerman RI. Parse analysis: a new method for the evaluation of investigators’ bibliographies. N Engl J Med. 1969;281(18):989–990. doi:10.1056/NEJM196910302811805. PMID: 5824741.
- Davis PJ, Gregerman RI. Parse analysis II. A revised model that accounts for phi. N Engl J Med. 1995;332(14):965–966. doi:10.1056/NEJM199504063321421. PMID: 7877668.