Abstract
Objective
The present study focuses on factors that predict sexual risk behaviors and sexual health screening behaviors in a sample of university students in Lebanon.
Participants
A convenience sample of 250 undergraduate students was recruited at a private university in Beirut, Lebanon.
Methods
Students completed measures of religiosity, psychological distress, contraceptives usage, human immunodeficiency virus (HIV)/sexually transmitted infections (STI) screening, and sexual risk behaviors.
Results
Religiosity was negatively associated with a range of risky sexual behaviors whereas psychological distress was positively associated with these behaviors. Sex under the influence of alcohol/drugs, discussing methods of contraception, and engaging in sexual activities later regretted had significant effects on having had condomless vaginal sex. Gender (being female) and sex under the influence of alcohol had significant effects on STIs screening.
Conclusion
Interventions that focus on managing drug and alcohol use in students, unwanted pregnancy, religion, stigma related to screening, and sexual health education are recommended.
Introduction
Effective sexual health promotion requires an understanding of sexual risk and sexual health screening behaviors in key populations. As a relatively young sexually active population, university students must be one focus of research into sexual health in Lebanon.Citation1 Individuals may not have sufficient levels of awareness and understanding of sexual health issues which can lead to increased risk-taking and lower levels of screening.Citation2–4 Furthermore, social psychological factors, such as group memberships and psychological wellbeing, are related to sexual decision-making and can shape sexual risk and screening behaviors.Citation5
There are very few studies from the Middle East on HIV knowledge, and attitudes, extramarital relationships (that is, both sexual contact outside of marriage and infidelity), fear of sexually transmitted infections (STIs), premarital testing, among Arab university students. In the United Arab Emirates, religion was stated as a reason to avoid extramarital relationships by 91% of respondents. Males scored higher on knowledge and reported more fear of getting an STI, and on fear and stigma from society and family in case they caught an STI. On the other hand, females showed greater compassion and interest in premarital testing and education to protect themselves.Citation6 In Turkey, the authors reported sexual myths among young people at risk and low sexual health information.Citation7 However, Lebanese society is different from neighboring countries because of its religious diversity including Christians and Muslims, and the different norms and customs within these religious groups.Citation1,Citation8 We argue based on the religious and cultural differences that findings from Lebanese context may differ from those of neighboring countries. The present study focuses on the factors that predict sexual risk behaviors and sexual health screening behaviors in a sample of university students in Lebanon. Given that academic institutions in the US and other Western societies are also culturally and religiously diverse, this insight into sexual risk behaviors and sexual health screening in Lebanon may also be useful for better understanding diverse student populations in other countries.
Gender differences in sexual behavior
In Lebanon, the incidence and prevalence of STIs in the general population are not reported and most previous studies have generally focused on STI rates in key high-risk populations, such as men who have sex with men.Citation8,Citation9 In fact, studies about sexual health among Lebanese heterosexuals and university students are scarce. Little is known about HIV or STI screening rates in heterosexual university students. However, a difference in sexual behavior between men and women has been reported in this population.Citation1 Yet, the study was largely descriptive and did not examine the social psychological correlates of sexual risk behavior. In this study, higher condom use was reported by men (86.1%) than by women (75.6%). Moreover, it was reported that Lebanese men have more sexual freedom compared to women due to the stigma of female sexuality,Citation10,Citation11 which may also lead women to be more skeptical about seeking sexual health screening than men.Citation12
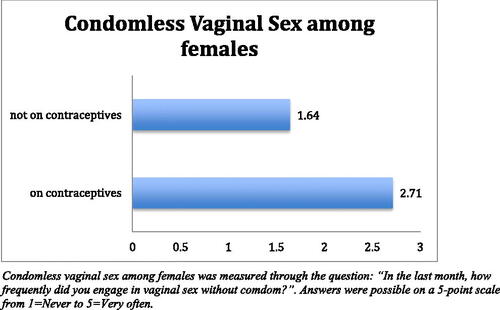
Condom use is reported to be lower in Lebanese female university students, compared to males.Citation1,Citation13 Moreover, in their study of contraceptive practice among university students in Lebanon, Barbour and SalamehCitation1 report lower levels of knowledge of contraception in females. Based on the findings of these studies, we hypothesize that women who use contraceptives are more likely to engage in condomless vaginal sex due to a lack of knowledge about contraception.
Consistent with the gender differences in sexual behavior among university students, Ghandour et al.Citation14 (2014) reported that having consumed alcohol or taken drugs at sexual debut was associated with being male, less religious, non-Arab, and having lived alone and/or abroad. Another study of students from 17 universities across Lebanon revealed a low percentage of condom use (36.3%), and risky sexual behavior positively correlated with alcohol consumption among males.Citation13
Religiosity and psychological distress
Psychological distress can be defined as the ‘unpleasant emotional experience of a psychological (i.e. cognitive, behavioral, emotional) and/or social nature that interferes with an individual’s ability to effectively cope with a given situation’Citation15. In research in other populations, it has been found that psychological distress is associated with sexual risk behavior.Citation16,Citation17 Second, significant group memberships (such as religion) have been found to be protective against sexual risk in some populations,Citation18,Citation19 although this has not been studied in the Lebanese population. Religiosity in Lebanon plays an important role in people’s lives and is protective against poor mental health outcomes in students.Citation20
Sexual minorities
Lebanese studies tend to focus exclusively on heterosexual students, rather than sexual minorities (namely lesbian, gay, bisexual and transgender [LGBT] individuals). There has been no previous study of HIV or STI screening rates comparing heterosexuals and sexual minorities. However, sexual minorities in Lebanon have easy access to sexual health services through LGBT-friendly civil organizations that allow free and anonymous HIV screening.Citation9
Hypotheses
On the basis of previous research, the following hypotheses were proposed and tested in this study:
Men are more likely to screen for HIV and STIs than women.
Men are more likely to engage in sexual activities under the influence of alcohol compared with women.
Women who use contraceptives are more likely to engage in condomless vaginal sex.
Psychological distress is associated with more sexual risk behaviors whereas religiosity is negatively associated with sexual risk behaviors but also with STI screening.
Sexual minorities will have higher HIV screening compared with heterosexuals.
Material and methods
Participants
One major challenge while conducting sexual health studies in Lebanon resides in the ability to obtain representative samples partly because of the stigma associated with the topic. This makes convenience sampling an appropriate sampling strategy for such research in Lebanon. The COVID-19 health crisis has also presented additional challenges to accessing adequate samples of the target population. Furthermore, this study is intended to provide preliminary insight into sexual risk and screening behaviors, which will hopefully stimulate further research in this important area. Consequently, a convenience sample of 250 undergraduate students at a private university in Beirut, Lebanon participated in an online survey of psychological distress and sexual risk taking. Participants provided electronic consent, were debriefed and thanked for their time. They were not incentivized financially for participating in the study.
Participants were aged between 18 and 36 (M = 20.9, SD= 2.38). There were 169 (67.6%) females, 77 (30.8%) males and 4 (1.6%) non-binary individuals in the sample. There were 161 (64.4%) heterosexuals and 89 (35.6%) sexual minorities. This exploratory study set out to examine differences between heterosexuals and sexual minorities in the first instance. There were 140 (59.3%) Christians and 96 (40.7%) Muslims. The majority of the sample reported being single (N = 173, 69.2%) with the remaining reportedly being in a relationship (N = 77, 30.8%). Due to the convenience sampling approach employed, our sample may not be representative of the university population. However, we did recruit a relatively even distribution of Christians and Muslims – the two main religious groups in Lebanon – and a sizeable number of sexual minorities, which allowed for comparisons in risk and screening behavior between heterosexuals and sexual minorities. provides a full description of the participant sample.
Table 1. Sociodemographic profile of the sample.
Measures
The variables measured in this study are summarized in , along with the number of items for each variable, example items, and the response categories. Religiosity and Psychological distress were measured using the Abbreviated Santa Clara Strength of Religious Faith QuestionnaireCitation21 and the 18-item Brief Symptom Inventory respectivelyCitation22. Manifestations of psychological distress considered in the questionnaire include physical symptoms of depression, psychological symptoms of anxiety, and suicidal ideation. The two scales were administered in their original English language since data were collected at an English-speaking university
Table 2. List of variables collected in the questionnaire with the number of items, examples of items, and possible answers for each variable.
Ethics
The Health and Life Sciences Faculty Research Ethics Committee at De Montfort University, Leicester, UK provided ethical approval for this study.
Statistical analyses
SPSS version 25 was used to perform the analyses. First, independent samples t-tests were performed to analyze differences between the main groups in the sample for the key variables. Cohen’s ds and 95% Confidence Intervals (CIs) were reported. Second, correlational matrices were performed to examine associations between continuous variables. Third, binary logistic stepwise regressions were conducted to test which variables predict condomless vaginal sex (0= not having had condomless vaginal sex in the past month; 1 = having had condomless vaginal sex in the past month) among heterosexuals only and the screening of STIs respectively (0 = never tested, 1 = tested).
Results
Descriptive statistics
The mean scores for religiosity and psychological distress were 2.0 ± 0.84 and 2.6 ± 0.95, respectively. summarizes the sociodemographic profile of the sample.
Males vs females
Independent sample t-tests showed that compared with females, males have a higher frequency of HIV screening (M = 1.61 ± 1.06 vs 1.21 ± 0.61) [t=–3.66, p<.001; Cohen’s d=–.51; 95% CIs (–.78, −.23)], higher frequency of STI screening (M = 1.72 ± 1.13 vs 1.26 ± 0.69) [t=–3.91, p<.001; Cohen’s d=–.54; 95% CIs (–.82, −.26)], higher frequency of having sex under the influence of alcohol (M = 1.87 ± 1.25 vs 1.55 ± 0.99) [t=–2.13, p=.03; Cohen’s d=–.29; 95% CIs (–.56, −.02)], and higher frequency of condomless anal sex (M = 1.47 ± 1.01 vs 1.18 ± 0.66; p<.05) [t=–2.56, p<.05; Cohen’s d=–.35; 95% CIs (–.62, −.08)]. These results confirm Hypotheses 1 and 2.
Contraceptives
Females who have used contraceptives in the past month were significantly more likely to engage in condomless vaginal sex as compared to those who had not used contraceptives (M = 2.71 ± 1.57 vs 1.64 ± 1.25; t=–3.18; p<.01). This confirms Hypothesis 3. There were no significant associations between contraceptive use and HIV or STI screening. summarizes sexual risk-taking among females by contraceptive use.
Screening
People who screened for STIs reported lower levels of religiosity [M = 1.79 ± 0.83 vs 2.05 ± 0.84; t = 2.06; p < 0.05; Cohen’s d=.30; 95% CIs (.02,.59)] than people who did not screen, supporting Hypothesis 4).
Correlations
Religiosity was negatively associated with a range of risky sexual behaviors including condomless vaginal sex, performing oral sex without protection, sex under the influence of alcohol, having sex without a condom with someone just met, and paying for sex. Religiosity was negatively associated with discussing methods of contraception with a sexual partner, and with psychological distress.
Psychological distress was positively associated with a range of risky sexual behaviors including having sex under the influence of alcohol, and drugs, engaging in a sexual activity later regretted, and feeling forced to engage in a sexual activity respondent did not want to engage in. These results support Hypothesis 4. See for full overview of correlations.
Table 3. Results of statistically significant correlations.
Heterosexuals vs sexual minorities
In view of the small numbers of lesbian, gay and bisexual participants (see ), it was not possible to examine differences between them. Therefore, all of the participants who identified as lesbian, gay or bisexual were categorized as ‘sexual minorities’. Independent samples t-tests were conducted to examine differences between sexual minorities and heterosexuals and showed statistically significant differences between heterosexuals and sexual minorities for HIV screening (M = 1.55 ± 1.0 vs 1.23 ± 0.64) [t=–2.98, p<.005; Cohen’s d=–.39; 95% CIs (–.66, −.13)], STI screening (M = 1.55 ± 0.98 vs 1.34 ± 0.81) [t=–1.75, p=.08; Cohen’s d=–.23; 95% CIs (–.49, .03)], and discussing contraceptive methods with sexual partners (M = 2.41 ± 1.51 vs 2.03 ± 1.36) [t = 1.98, p<.05; Cohen’s d=.26; 95% CIs (.002, .52)]. These results confirm Hypothesis 4.
Multiple regression models
First, a binary logistic stepwise regression was conducted to examine which variables predict the variance of condomless vaginal intercourse among heterosexuals only (N = 161). The variables of discussing contraception; feeling forced to engage in a sexual activity; engaging in a sexual activity later regretted; sex under the influence of alcohol; sex under the influence of drugs; and religiosity were inserted as predictors, and having had condomless vaginal sex in the past month was inserted as the dependent variable. The dependent variable was recoded as a dichotomous variable (having had condomless vaginal sex in the past month = 1 vs not having had sex in the past month = 0). The model was statistically significant for condomless vaginal sex (χ2(6)=58.84, p<.001) and explained 30% of the variance. Of all of the predictors, sex under the influence of alcohol (β = 1.02, p<.001) and drugs/substances (β = 0.56, p<.01), discussing methods of contraception (β = 0.30 p<.01), and willingly engaging in sexual activities later regretted (β=–0.55, p<.01) had significant effects on the variance of having had condomless vaginal sex in the past month.
Second, a binary logistic stepwise regression was conducted to examine which variables predict the variance in screening for STIs in the entire sample. The variables of condomless vaginal sex; condomless anal sex; discussing contraception; discussing sexual health; sex under the influence of alcohol; sex under the influence of drugs; gender; sexual orientation; and religiosity and psychological distress scales were inserted as predictors. The dependent variable was recoded as a dichotomous variable (0 = never tested, 1 = tested). The regression model was statistically significant for HIV screening (χ2(6)=41.04, p<.01) and explained almost 16% of the variance in this outcome. Of all variables, gender (β=.98, p<.01) and sex under the influence of alcohol (β=.47, p<.01) were significant predictors of screening for STIs.
Discussion
Both engagement in sexual risk and sexual health screening behaviors are important determinants of sexual health. This preliminary study of university students in Lebanon sheds light on key risk factors for poor sexual health in this population.
Gender differences
Gender plays a significant role. Although men are more likely to engage in sexual behavior while under the influence of alcohol, they are also more likely to screen for STIs and HIV than women, suggesting that infections may be more rapidly detected and treated in this group. Furthermore, female students appear to face an additional risk factor, namely the false sense of protection that is provided by oral contraceptives which in turn is associated with decreased condom use.Citation23 Oral contraceptives are of course protective only against unwanted pregnancy – not STIs. Indeed, in previous research, it has been found that students may conceptualize sexual health in terms of avoiding unwanted pregnancy and, thus, perceive oral contraceptives as an adequate sexual health protection strategy.Citation24 Yet, women who use contraceptives are no more likely to screen for STIs, despite their elevated risk behavior, suggesting that they may be especially vulnerable to undiagnosed STIs.
Religiosity and psychological distress
Religion continues to play an important role in Lebanese society and can shape moral beliefs, personal values, and behaviors.Citation13,Citation25 In our sample, religiosity does appear to be protective against psychological distress and negatively associated with a variety of sexual risk behaviors. Similar results have been reported in other Middle Eastern countries, such as Kuwait, in which religiosity was positively correlated with better physical and mental health outcomes.Citation26 Psychological distress appears to be associated with different types of sexual risk behavior, which is consistent with previous research in this area.Citation16,Citation17 Yet, religiosity was negatively associated with discussing contraception with sexual partners, which suggests that this identity may also constitute a barrier to negotiating the type of sex that individuals have and the level of risk that is acceptable to them. This could partially be attributed to the fact that pre-marital sex and contraception are generally rejected across key religious groups in Lebanon.Citation27 Consequently, avoiding pre-marital pregnancy by taking oral contraceptives may be prioritized over STI prevention. Moreover, behavioral interventions to promote condom use should focus on increasing awareness about condom effectiveness against not only unwanted pregnancy but also STIs.
Sex under the influence of alcohol
The first regression model demonstrated significant effects of alcohol and drug use on condomless vaginal sex in the last month among heterosexuals.Citation14,Citation28,Citation29 When controlling for discussing contraception, feeling forced to engage in a sexual activity, engaging in a sexual activity later regretted, sex under the influence of alcohol, sex under the influence of drugs, and religiosity, we found that unprotected vaginal intercourse is almost 3 times more likely to occur under the influence of alcohol in our sample. Furthermore, it appears that sexual communication variables (such as discussing contraception and engaging in a behavior that is later regretted) also impact on this particular type of risk behavior. The second regression model reiterated the effect of alcohol use on STI screening behavior, indicating that alcohol use may lead people to appraise their risk inaccurately and, thus, fail to screen for STIs. The model also showed a significant effect of gender, reiterating the decreased likelihood of STI screening if one is female. This could be attributed to perceived stigma in relation to female sexuality whereby sexually active females may be labeled as immoral or promiscuous in conservative cultures, such as that of Lebanon.Citation10,Citation12
Implications for sex education
The results suggest that university students in Lebanon may be prone to distinct types of sexual risk behavior. While females tend to lack self-efficacy in relation to sexual behavior, to be coerced into behaviors they do not desire and to engage in STI screening less frequently, men appear to use substances more frequently which could lead to poor health outcomes. Furthermore, on the whole, heterosexual students engage less frequently with sexual health screening than students from sexual minorities.
It is proposed that interventions that focus on managing drug and alcohol use in students and that enhance sexual communication skills would be beneficial in enhancing sexual health outcomes in this population. Furthermore, the emphasis on unwanted pregnancy should be challenged in sexual health interventions – especially for women who appear to be less likely to use condoms if they use contraceptives. Given the largely protective role of religion and the general significance of this identity in Lebanon,Citation13,Citation25 religion may be incorporated into the design of interventions, demonstrating the compatibility of religion and good sexual health. This has been suggested by key stakeholders in the Middle East including parents, school teachers, healthcare professionals and religious scholars;Citation12,Citation30,Citation31 and may, in turn, facilitate sexual communication among religious people.
Although this preliminary study is particularly useful for shaping policy and practice in relation to sexual health promotion in Lebanon, it may have broader ramifications. First, the findings may be transferable to other societies in the Middle East and North Africa (MENA) region which share some cultural and religious similarities. Second, as universities in the US and other Western societies are increasingly diverse in terms of their student populations, the findings from this study may shed light on the social, cultural and psychological underpinnings of sexual risk and screening behaviors in students socialized in cultures associated with the MENA region.
Limitations
This preliminary study has several limitations, which should be addressed in future work. First, this cross-sectional study provides only an empirical snapshot of sexual risk behavior and sexual health screening behaviors that may occur in societies facing severe economic, political and health crises.Citation32 The current period is associated with negative affect and distressCitation33 and with lockdown measures, strict curfews and fear of infection with COVID-19 directly affecting the willingness of patients to access screening services including HIV testing.Citation34 Second, the study was conducted in one private university and the results cannot be generalized to the overall community of students in Lebanon. Third, the study included more women than men, and larger samples of male students should be recruited in future research. Yet, the study provides insight into sexual health variables of heterosexual and sexual minorities which consisted of relatively small subgroup sample sizes preventing further analysis. Finally, there may be a desirability bias in reporting due to the nature of the questions posed. For instance, a “very often” incident or sexual intercourse under the “influence of alcohol and drugs” are a subjective perception that may vary across individuals.
Notwithstanding these limitations, there does appear to be a general disengagement with sexual health services in Lebanon, with heterosexuals being less likely to screen than sexual minorities. Screening should be encouraged and the stigma associated with screening should be challenged. It should be made more available and accessible to university students and students should be provided with clear information regarding sexual health. Sexual health education should be embedded in the school or university curriculum to provide objective information about sexual health which unfortunately remains a highly stigmatized topic in Lebanon.
Disclosure statement
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of the United Kingdom and received approval from the De Montfort University's Health and Life Sciences Faculty - Research Ethics Committee.
Additional information
Funding
References
- Barbour B, Salameh P. Knowledge and practice of university students in Lebanon regarding contraception. East Mediterr Health J. 2009;15(2):387–399. https://apps.who.int/iris/handle/10665/117651 doi:10.26719/2009.15.2.387.
- Bouclaous CH, Alrazim A, Chababi J, et al. Association between sources of sexuality education, sexual beliefs and behaviours in Lebanese young adults: a university-based cross-sectional study. Sex Education. 2021;21(1):1–2. doi:10.1080/14681811.2020.1722624.
- Lally K, Nathan-V Y, Dunne S, et al. Awareness of sexually transmitted infection and protection methods among university students in Ireland. Ir J Med Sci. 2015;184(1):135–142. doi:10.1007/s11845-014-1073-8.
- Mouhanna F, DeJong J, Afifi R, Asmar K, Nazha B, Zurayk H. Student support for reproductive health education in middle schools: findings from Lebanon. Sex Education. 2017;17(2):195–208. doi:10.1080/14681811.2017.1280011.
- Kabiru CW, Orpinas P. Factors associated with sexual activity among high-school students in Nairobi, Kenya. J Adolesc. 2009;32(4):1023–1039. doi:10.1016/j.adolescence.2008.08.001.
- Gańczak M, Barss P, Alfaresi F, Almazrouei S, Muraddad A, Al-Maskari F. Break the silence: HIV/AIDS knowledge, attitudes, and educational needs among Arab university students in United Arab Emirates. Journal of Adolescent Health. 2007;40(6):572-e1–572.e8. doi:10.1016/j.jadohealth.2007.01.011.
- Evcili F, Golbasi Z. Sexual myths and sexual health knowledge levels of Turkish university students. Sexuality & Culture. 2017;21(4):976–990. doi:10.1007/s12119-017-9436-8.
- Wagner GJ, Ghosh-Dastidar B, El Khoury C, et al. Major depression among young men who have sex with men in Beirut, and its association with structural and sexual minority-related stressors, and social support. Sex Res Social Policy. 2019;16(4):513–520. doi:10.1007/s13178-018-0352-y.
- Maatouk I, Assi M, Jaspal R. How Can we Enhance Sexual Health Outcomes in Men Who Have Sex with Men in Lebanon?. BMJ Sexual & Reproductive Health; 2020. doi:10.1136/bmjsrh-2019-200415.
- Hajali M. Reproducing Violence through Reconstructing the Hymen? Gender-Based Violence against Women in Lebanon (Master's thesis, UiT Norges arktiske universitet). https://munin.uit.no/handle/10037/8241.
- Melki J, Mallat S. Lebanon: Women’s Struggle for Gender Equality and Harassment-free Newsrooms. In The Palgrave International Handbook of Women and Journalism. London: Palgrave Macmillan; 2013:432–448. doi:10.1057/9781137273246_31.
- Clark KA, Keene DE, Pachankis JE, Fattal O, Rizk N, Khoshnood KA. A qualitative analysis of multi-level barriers to HIV testing among women in Lebanon. Cult Health Sex. 2017;19(9):996–1010. doi:10.1080/13691058.2017.1282045.
- Salameh P, Zeenny R, Salamé J, et al. Attitudes towards and practice of sexuality among university students in Lebanon. J Biosoc Sci. 2016;48(2):233–248. doi:10.1017/S0021932015000139.
- Ghandour LA, Mouhanna F, Yasmine R, El Kak F. Factors associated with alcohol and/or drug use at sexual debut among sexually active university students: cross-sectional findings from Lebanon. BMC Public Health. 2014;14(1):671 doi:10.1186/1471-2458-14-671.
- Sellick SM, Edwardson AD. Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psychooncology. 2007;16(6):534–542. doi:10.1002/pon.1085.
- Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc. 2010;39(5):514–527. doi:10.1007/s10964-010-9524-7.
- Martin JS, Ghahramanlou-Holloway M, Englert DR, et al. Marital status, life stressor precipitants, and communications of distress and suicide intent in a sample of United States Air Force suicide decedents. Archives of Suicide Research. 2013;17(2):148–160. doi:10.1080/13811110701800715.
- Hjarvard S. The mediatisation of religion: Theorising religion, media and social change. Culture and Religion. 2011; 12(2):119–135. doi:10.1080/14755610.2011.579719.
- Jetten J, Haslam C, Alexander SH, editors. The Social Cure: Identity, Health and Well-Being. New York, NY: Psychology press; 2012.
- Assi M, Maatouk I, Jaspal R. Psychological distress and self-harm in a religiously diverse sample of Lebanese students. Mental Health, Religion & Culture. 2020;23(7):591–595. doi:10.1080/13674676.2020.1788524.
- Plante TG. The Santa Clara Strength of Religious Faith Questionnaire: Assessing faith engagement in a brief and nondenominational manner. Religions. 2010;1(1):3–8. doi:10.3390/rel1010003.
- Derogatis LB1. Brief Symptom Inventory 18: Administration, scoring and procedures manual. NCS Pearson. 2001;1:47.
- Mulligan K. Access to emergency contraception and its impact on fertility and sexual behavior. Health Econ. 2016;25(4):455–469. doi:10.1002/hec.3163.
- Pazol K, Kramer MR, Hogue CJ. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep. 2010;125(2):208–217. doi:10.1177/003335491012500209.
- Maatouk I, Jaspal R. Religion, Male Bisexuality and Sexual Risk in Lebanon. London: Routledge; 2019. doi:10.4324/9780429019913-9.
- Baroun KA. Relations among religiosity, health, happiness, and anxiety for Kuwaiti adolescents. Psychol Rep. 2006;99(3):717–722. doi:10.2466/PR0.99.3.717-722.
- Bteich G, Hajj M, Accaoui E, El Abed A. Sexual perception of young Lebanese students. Health. 2017;09 (02):299–316. doi:10.4236/health.2017.92021.
- Scott-Sheldon LA, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS Behav. 2010;14(4):845–853. doi:10.1007/s10461-008-9426-9.
- Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent substance use and sexual risk-taking behavior. J Adolesc Health. 2001;28(3):181–189. doi:10.1016/S1054-139X(00)00169-5.
- Al Zaabi O, Heffernan M, Holroyd E, Jackson M. Islamic parents’ attitudes and beliefs towards school-based sexual and reproductive health education programmes in Oman. Sex Education. 2019;19(5):534–550. doi:10.1080/14681811.2018.1553708.
- Horanieh N, Macdowall W, Wellings K. Abstinence versus harm reduction approaches to sexual health education: views of key stakeholders in Saudi Arabia. Sex Education. 2020;20(4):425–440. doi:10.1080/14681811.2019.1669150.
- Devi S. Lebanon faces humanitarian emergency after blast. Lancet (London. England). 2020;396(10249):456. doi:10.1016/S0140-6736(20)31750-5.
- Jaspal R, Assi M, Maatouk I. Potential impact of the COVID-19 pandemic on mental health outcomes in societies with economic and political instability: case of Lebanon. MHRJ. 2020;25(3):215–219. (in press)
- Maatouk I, Assi M, Jaspal R. The emerging impact of the COVID-19 outbreak on sexual health in Lebanon. Sex Transm Infect. 2020; doi:10.1136/sextrans-2020-054734. (in press)