Abstract
Objective: The development and evaluation of the Professor Hippo-on-Campus Student Mental Health Education Program, a mental health literacy intervention for post-secondary faculty and staff, is described. It includes 3-hour virtual, asynchronous e-modules and an optional 2-hour, synchronous workshop. Participants: All faculty and staff in a single university were invited to participate (February 2020–January 2021). Methods: Pre-and post-module and post-workshop surveys were conducted, assessing knowledge, attitudes, stigma, behavioral intentions, and confidence. Paired t-tests and regressions assessed change. Satisfaction was assessed through closed and open-ended questions, analyzed descriptively and through qualitative content analysis. Results: Four hundred and fifty staff and faculty completed the pre-survey, 262 completed the post-survey, and 122 completed a workshop survey. Participation resulted in improvements in knowledge, attitudes, stigma, and confidence with high levels of satisfaction. Conclusion: The program provides tailored student mental health training to post-secondary staff and faculty, which appears to increase their mental health literacy.
Introduction
Among emerging adults and post-secondary students, the prevalence of psychological distress and mental health disorders is high and appears to be growing, even prior to the COVID-19 pandemic.Citation1–7 Disorders that are present or emerge during this developmental phase can have significant and persistent personal, academic, occupational, and economic consequences, particularly if untreated.Citation6,Citation8–13 Suicide, while rare, is the second leading cause of death in this age group, and alcohol-related deaths are also considerable.Citation14,Citation15 While stigma appears to be decreasing, and awareness of mental health issues and rates of help-seeking are increasing, many emerging adults and students still do not seek or receive the help they need or want.Citation5,Citation16–21
Youth mental health concerns have been labeled a “global public-health challenge,” a situation likely exacerbated by the COVID-19 pandemic.Citation22 As mental health is understood through this lens and with increased understanding of the social determinants of health and mental health, interest in promotion and prevention is growing.Citation13 University campuses are being recognized as an essential site for mental health promotion and prevention, suicide prevention, and early intervention, however evidence-based programming tailored to this setting and population remain limited.Citation23–30
Gatekeeper training involves educating individuals (typically non-professionals) who frequently interact with community members, to identify, communicate, and connect individuals experiencing distress or mental health symptoms to support and care. Faculty and staff on post-secondary campuses have been identified as potential gatekeepers, given their frequent interactions with students and roles as educators, mentors, supervisors, and service-providers.Citation31 While they are well-positioned to support students, many do not feel prepared or that they have sufficient education or training, despite wanting it.Citation7,Citation32–34 Institutions may not have sufficient, clear or well-understood processes for identifying and supporting students in distress, and the gatekeeper training literature has often targeted only specific groups of campus staff, such as residence advisors.Citation35 The need for accessible gatekeeper training, specific to post-secondary staff and faculty and the post-secondary environment and culture, is being recognized as a priority for institutions globally, and research is needed to determine feasibility, efficacy, and effectiveness.
Gatekeeper training typically aims to enhance mental health literacy (MHL). The concept of MHL, and programs to build it, has been evolving since the 1990s, with the first large-scale program being Mental Health First Aid (MHFA), which has been adapted across countries.Citation36–38 MHL can be defined as: understanding mental health and mental disorders (improving knowledge); decreasing stigma (improving attitudes); and enhancing help-seeking efficacy (improving behaviors or confidence).Citation39 Programs have been designed to improve MHL, many inspired by MHFA, with some focused on secondary school educators and post-secondary students, staff, and faculty.Citation29,Citation40–45 Such programs have been shown to increase knowledge, reduce stigma, and increase confidence and intent to intervene among participants, however, sustained program benefits are unclear.Citation29,Citation40–45 Additionally, there are a number of programs specifically designed to provide suicide prevention and intervention training (e.g., SafeTalk), which have also demonstrated positive changes in knowledge, skills, and attitudes, with diminishing effects over time.Citation46,Citation47 These programs have typically been delivered and evaluated face-to-face and synchronously, not asynchronously, virtually or in the COVID context.
It has been noted that MHL programs need to be context-specific, co-created with the target audience, developmentally appropriate, and integrated into existing organizations, such as schools and community organizations.Citation39,Citation45 Although some programs are being implemented in post-secondary settings (e.g., MHFA, SafeTalk), these programs were not designed with post-secondary students or environments in mind. Additionally, while social determinants of mental health and considerations of equity, diversity, inclusion, and accessibility are increasingly recognized as essential to informed discussions of mental health and well-being, such topics have not typically been addressed in existing programs; nor have other important topics, such as understanding academic accommodations for mental health-related disabilities.Citation19,Citation48 Existing MHL programs have focused largely on symptom identification, suicidality, mental health disorders, and resources. These programs have not addressed student mental health and emotional, psychological, and social well-being broadly in the post-secondary context and culture. Recognition of specific post-secondary stresses and challenges than can be mitigated creates opportunities to potentially reduce the prevalence, severity, chronicity, or consequences of mental health problems.
Development of Professor Hippo-on-Campus
These gaps in training and research led us to create and evaluate a new mental health literacy training program—the Professor Hippo-on-Campus: Student Mental Health Education Program for Educators and Navigators at McMaster University. McMaster is a mid-sized university of approximately 36,000 students across 6 faculties in Hamilton, Canada. The Professor Hippo-on-Campus program was inspired by an institutional mental health strategy-identified need and priority to increase desired and needed training.Citation49 The title references the brain structure, the hippocampus, as well as one of the key characters in the modules, Professor Hippo. The program was designed to address the notable gaps outlined above. The first version of the program was developed in 2017 with funding from an educational grant (eCampus Ontario). Program development involved detailed literature reviews and extensive stakeholder consultation. The development team included those with expertise in pedagogy and building online/virtual educational materials, graphic design, content (faculty, staff, students), policy and processes, and mental health (psychiatry, social work, nursing, health promotion). To increase accessibility and acceptability, the program was designed to be brief and flexible with 3 hours of asynchronous online modules and a 2-hour synchronous workshop. Eight modules were created using Articulate software,Citation50 beta-tested with faculty and staff, refined and published on a curricular platform (Avenue to Learn [A2L]).Citation51
The 5 R protocol
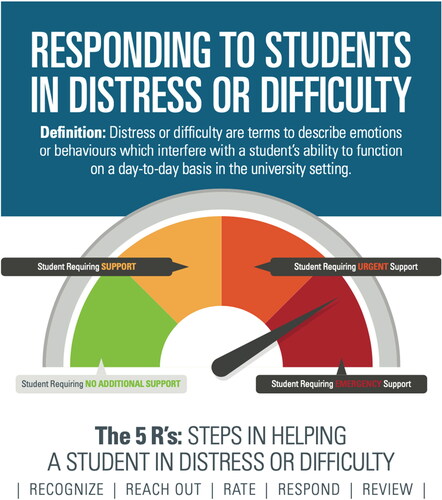
Parallel to the development of the Professor Hippo-on-Campus program, a campus-wide protocol, “Responding to Students in Distress and Difficulty” was created, herein called the 5 R protocol. The 5 Rs represent key steps in supporting a student in stress or difficulty which include: (1) Recognize (signs of difficulty or distress); (2) Reach out (to the student or identify an alternative helper); (3) Rate (the level of student distress or difficulty as no additional support (green), support (yellow), urgent (orange), or emergency (red); (4) Respond (recommend, refer or accompany, act); and (5) Review (student and supporter needs).Citation52 The protocol and “rate” steps are presented visually, like a speedometer (See ), to help faculty and staff to understand and rate the level of severity and to intervene accordingly, providing examples and suggested language. This protocol forms the basis of a key module within the Professor Hippo-on-Campus program and the workshop discussions (Module 6).
Initial feasibility study and current module development process
A feasibility study was performed in which faculty (n = 103) were recruited and randomly assigned to receive the virtual modules only (n = 35), virtual modules and in-person workshop (n = 36), or links to usual campus resources (n = 32). A mixed methods evaluation was undertaken using pre-post surveys, focus groups, and interviews.Citation53 From pre to post, increases in knowledge and confidence, and reductions in stigma across groups were observed. Over 80% of participants found the program engaging and effective at increasing knowledge, awareness, and interest in student mental health. Almost all participants (98%) recommended this training for all staff and faculty at McMaster. Focus groups and interviews further triangulated the acceptability of the e-learning component with regards to accessibility, style, engagement, flexibility, importance, and impact on confidence in responding to student mental health concerns and making changes in the classroom. Results highlighted greater satisfaction among those with access to in-person training and a strong desire for in-person training to supplement the e-learning modules. The participants also provided recommendations for further improvements to the modules and in-person training.
In 2019, the modules were updated and modified, retaining the original structure of 8 asynchronous e-modules (see ). Additional resources, links, and accessibility options were added (e.g., written- and audio-only versions, closed captioning, image description). The workshop curriculum was also redesigned to focus on reinforcing and applying the module content. The redesigned workshop focuses on engaging and information-sharing with faculty and staff about their role and perspectives on student mental health issues, discussing how to create mental health-positive and inclusive learning environments, applying the 5 Rs protocol to student case studies, and reviewing campus resources. The online modules take approximately 3 hours to complete independently, and the workshop is 2 hours in length following module completion. The synchronous workshops were held in person initially, then modified to be offered virtually on the Zoom platform when the COVID-19 pandemic hit.
Table 1. Professor Hippo-on-Campus module descriptions.
Objectives
This paper describes a naturalistic, pragmatic, mixed-methods evaluationCitation55 of the feasibility and acceptability of the revised Professor Hippo-on-Campus modules and workshops. Feasibility outcomesCitation56 include process and resource outcomes (e.g., recruitment, retention, and survey completion) and scientific outcomes, including changes in mental health-related knowledge, stigma, attitudes, and behavioral intentions and confidence. Acceptability is assessed through satisfaction and experience with the program.Citation57 Reporting follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.Citation58
Methods
Recruitment and study flow
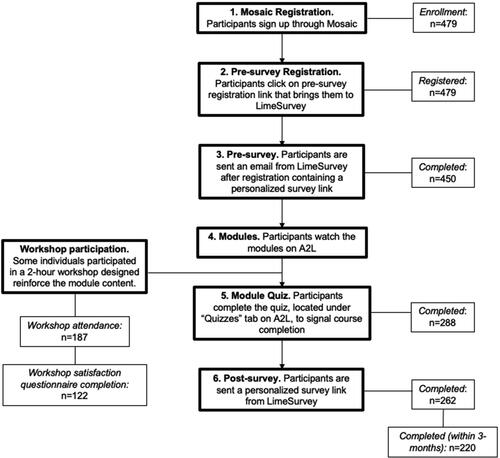
Any staff or faculty member of the institution was able to participate. Participants were recruited through various approaches, including advertisements (e.g., posters, an institution-wide email, social media campaigns), direct recruitment by administrators or supervisors including faculty deans, and presentations to faculty and staff groups regarding the program. Participants self-registered via the institution’s online portal (Mosaic) in order to gain access to the course on the Avenue to Learn (A2L) platform (n = 479, between February 4th, 2020 to January 15th, 2021). They were then sent an email to complete the pre-survey (n = 450, 94%). Participants were then prompted to complete the e-modules within 3 months. Out of those who had not completed the program at the time of this analysis, 26 were still within their 3-month period (thus, the denominator for completion is n = 427). The workshop was a voluntary program supplement (n = 187, 44%), and all workshop attendees were asked to complete a post-workshop specific survey (n = 122, 65%). Of those who completed the post-module survey (n = 262, 61%), 220 participants completed e-modules within the specified 3-month period (while 42 participants completed outside of 3-months) and 44 had attended a workshop (24% post-survey response rate among workshop attendees). The median time to completion was 32 days. Reminders were sent to complete the pre-survey, the modules, and the post-survey approximately every 3 weeks. Upon completion, participants were issued a certificate and a digital badge and given indefinite access to the program modules. An exemption from ethics review was granted by the Hamilton Integrated Research Ethics Board. See for a program flow chart.
Survey
The pre-survey included demographic variables and measures capturing knowledge, stigma, attitudes, and confidence. The post-module survey re-assessed all outcome measures and asked about self-attributed changes in knowledge, skills, and behavioral intentions. The post-module survey also included questions about satisfaction with the program including closed and open-ended questions related to overall satisfaction and experience, as well as changes in knowledge, attitudes, and behavioral intentions. Post-workshop satisfaction surveys were also completed, with both closed- and open-ended questions.
Knowledge about student mental health
Knowledge was measured using questions developed for the study about 4 scenario-based vignettes (2 questions per scenario), designed to capture participant ability to apply the Responding to Students in Difficulty and Distress protocol described above (minimum 0, maximum 8).
Mental health related stigma
Stigma was measured using the Reported and Intended Behaviors Scale (RIBS), which includes 4-items capturing past and 4-items capturing current behavioral inclusion or discrimination toward people with mental health problems.Citation59 Items 1–4 rate past behaviors as yes, no, or uncertain and are reported descriptively. Items 5–8 assess intended behaviors (e.g., willing to live with or nearby, work or teach, or be friends with someone with a mental health problem) scored on a 5-point Likert scale reflecting how strongly a person disagrees/agrees that they could engage in the specified behavior. For our analysis, the RIBS was recoded so that a higher score indicated higher levels of stigma (1 = agree strongly and 5 = disagree strongly) with a minimum score of 4 and maximum of 20 (a = 0.78).
Negative attitudes toward post-secondary student mental health and difficulty
Attitudes toward student mental health were adapted from the Opening Minds Stigma Scale: Postsecondary Environment (Heather Stuart, email communication, February 21, 2018), including 13-items assessing postsecondary faculty members’ attitudes toward students with mental health problems (e.g., students with mental health difficulties interfere with social interactions at the university) and beliefs and intentions regarding their role in supporting students with mental health problems (e.g., I would not want to teach or work with a student who has been treated for a mental health difficulty). Items were rated from strongly disagree (1) to strongly agree (5) and scores were summed with a minimum score of 13 and a maximum score of 65 (Cronbach alpha [a] = 0.84).
Confidence in identifying and responding to a student in distress and difficulty
Confidence was measured using self-report items on a 1–10 rating scale based on Bandura’s General Self-Efficacy Scale.Citation60 There were 2 sets of confidence questions: (1) 10 items capturing general self-confidence in identifying and responding to students in need, with a maximum aggregated score of 100 (a = 0.91); and (2) 12 scenario-based confidence questions (i.e., 4 scenarios, 3 questions each) focused on confidence in communication with the described student and making decisions about the level of support needed, with a maximum aggregated score of 120 (a = 0.94).
Self-reported changes in knowledge, skills, and behavioral intentions
Self-reported changes in knowledge and skills were quantitatively measured using 13 self-report items on a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). Items capture perceived changes in knowledge about student mental health (e.g., stress, etiology, signs and indicators) and their own mental health, resources available for students and staff (e.g., mental health supports, academic accommodations), and intentions to apply skills regarding their role in supporting and addressing student mental health (e.g., communication strategies, noticing and checking in on students, creating positive and inclusive learning environments, responding to urgent or emergent mental health situations). Scores are reported as the percentage of the sample endorsing agree or strongly agree for each item and the total summed score of perceived changes, whereby there is a maximum score of 65 (a = 0.90). Post-workshop surveys also asked similar questions regarding perceived changes related to students specific to workshop participation.
Satisfaction
Program satisfaction since completing the e-modules was measured using 6 self-report items on a 1–10 rating scale focused on the perceived effectiveness of the program, overall enjoyment, impact on their role at the university, likelihood to recommend the program to others, thoughts around whether all staff and faculty should take the program, and perceived benefit of in-person workshops. Scores are reported as the percentage of the sample endorsing agree or strongly agree for each item and the total summed score (except perceived benefit of workshops), whereby there is a maximum score of 50 (a = 0.94). The post-workshop surveys also included similar satisfaction questions specific to workshop participation.
Statistical analysis
Quantitative analysis
Descriptive statistics were conducted for demographics and outcome variables. Paired T-tests were used to assess global pre-post changes in outcomes related to knowledge, stigma, attitudes, and confidence. Multiple linear regression was used to determine whether post-scores were predicted by demographic variables or workshop attendance, after adjusting for baseline scores.Citation61 A statistically significant effect was defined as a p-value of less than 0.05. Only complete cases were analyzed. To provide further evidence of effectiveness, we sought ≥70% of individuals self-reporting positive changes in knowledge, skills, and attitudes. Acceptability was evaluated through satisfaction scores of agree or strongly agree for ≥70% of participants.
Qualitative analysis
A qualitative content analysis was conducted.Citation62,Citation63 The responses to the module post-survey open response questions were reviewed and similar concepts were grouped together into preliminary topic codes and categories, independently done by two research assistants (AX and MBS). Following discussion between AX, MBS, JH, and CM, overarching themes were established, codes refined, and data recoded. The evolving thematic scheme was regularly presented back to the team to incorporate multiple viewpoints in order to further validate the final themes to ensure consensus was achieved. Using this final coding scheme, the workshop post-surveys were then independently coded, adding additional topic codes and categories where applicable and following a similar process of inductive reasoning. Overarching themes were similar across both surveys, with some distinct categories only applicable to the workshop or modules. The final results are organized into themes and subthemes with quotes to illustrate key concepts.
Results
Sample characteristics
On average, participants completing the baseline were 36 years of age (SD = 12) and mostly female (76%). Of those participating, 53% indicated they were staff and 25% faculty, with the remaining being student employees such as teaching assistants. Many reported no prior mental health training as part of their formal academic training (72%) or through training courses or certifications (60%). Almost half (48%) of participants reported that the primary nature of their interactions with students was in a teaching or supervisory role. Based on a typical 3-month period, 75% of participants reported interacting face-to-face with students more than once a week and 51% reported interacting with students experiencing stress, distress, or having mental health difficulties more than once a month.
Based on logistic regressions, completing the post-survey was more likely among those who were older (odds ratio [OR] = 1.02) and lacked previous academic-related mental health training (OR = 2.63); missingness was less likely among those spending more time interacting with students (OR = 0.88) and with higher scenario knowledge (OR = 0.83). Of those completing the post-survey, workshop attendance was more common among those with more years of work experience (OR = 1.06), older (1.04), more interactions with students (any interactions OR = 1.85; students in distress OR = 1.63), higher baseline confidence (OR = 1.02), and among staff (OR = 1.98) or faculty (OR = 2.4). Further sample characteristics are in .
Knowledge, stigma, attitudes, and confidence
Scores for stigma and negative attitudes were generally low at both baseline and post-survey, while scores for general confidence, scenario-based confidence, and scenario-based knowledge were generally high at both baseline and post-survey. Reported behaviors according to the RIBS indicated that at baseline: 63% do or have lived with someone with a mental health problem, 60% do or have taught/supervised/worked with someone with a mental health problem, and 79% do or have had a close friend with a mental health problem. Paired t-tests assessing changes in outcome scores from baseline to program completion showed that there were significant decreases in negative attitudes and stigma, increases in general confidence scores and scenario confidence scores, and increases in knowledge scores (See ). Of note, most differences were of small magnitude (change <5% of total possible scores) and may not reflect meaningful differences. Meaningful increases in global confidence (15-point increase, 15% of the total possible score) and scenario confidence (20-point increase, 22% of the total possible score) were detected. There were no meaningful differences in outcomes based on demographics or for those who attended a workshop compared to those who did not.
Table 2. Sample characteristics.
Table 3. Key outcomes pre and post program completion.
Self-reported changes in knowledge and skills
Perceptions in changes after completing the program were generally high, with more than 80% of participants reporting that the program increased knowledge of various aspects of student mental health, resources available, and increased knowledge and confidence regarding their role in supporting and addressing student mental health (on both post-module and post-workshop surveys). More than 70% of participants reported that their awareness of and knowledge about their own mental health and supports available was improved after completing the program. On the post-workshop surveys (n = 122), 96% agreed they were glad they attended the workshop/enjoyed the program, with 97% indicating they would recommend the workshop to other staff or faculty.
Satisfaction
Satisfaction scores were generally high with an overall mean score of 22 (SD = 3.3) out of a maximum possible score of 25, with similar satisfaction scores (p = 0.110) for those attending a workshop (mean = 21, SD = 5) and the e-module only participants (mean = 22, SD = 3). Overall: 96% of participants believed the program was effective in enhancing learning, 91% enjoyed the program, 94% believed the program would be helpful in their role at the university, 96% would recommend this program to other faculty/staff at the university, 94% believed that this program should be mandatory for all faculty/staff who interact with students. On the post-modules survey, 66% of those completing e-modules only and the 77% of those attending a workshop (n = 44) agreed or strongly agreed that a scenario-based workshop would be or was helpful. On the post-workshop surveys (n = 122), 96% agreed they were glad they attended the workshop/enjoyed the program with 97% indicating they would recommend the workshop to other staff or faculty.
Qualitative themes
On post-surveys, 90% of respondents provided at least one response across open-ended questions, with 83% answering 5 or more open-ended questions (out of 8). On post-workshop surveys, 96% of participants provided a response. Five main themes emerged including: (1) Knowledge and understanding of student mental health issues; (2) Confidence and changes in behavior; (3) Attitudes and perspectives; (4) Quality of the program content and delivery; and (5) Desire for additional support and training. See for a summary of themes.
Table 4. Summary of all qualitative themes and subthemes.
Regarding knowledge and understanding of student mental health issues, sub-themes included: better understanding of mental health concepts, for example, “Mental health issues come in various forms and severities and they all need to be paid attention to” and an increased awareness of mental health challenges and the mental health system within the institution, for example, “It has broadened my knowledge of the network of resources (mental health services, student accessibility services, other Hippo-on-campus certified faculty and staff).”
Regarding confidence and changes in behaviors, sub-themes included perceived increase in confidence in supporting student mental health, an increased ability to create a welcoming and inclusive classroom environment using Universal Design principles, greater awareness of resources, and usefulness and implementation of the 5 R’s protocol. Some examples:
“The modules have specific examples, which show me how to communicate with distressed students. Thanks to this program, I have a better idea of what I should say in an interaction with a distressed student.”
“I’ve dealt with students many times over the years, and with the basics of university policy for quite a while. So for me the stand-out feature of the program was just what services were out there, what contacts were available, and the nice contact information charts that were given."
“I really found the 5R’s (recognize, reach out, rate, respond, review) to be extremely helpful. It was a great way to break down a pretty daunting topic.”
Regarding attitudes and perspectives, sub-themes included perceived increased sense of personal responsibility, increased empathy, reaffirmed importance, and barriers to supporting student mental health. Regarding personal responsibility, one participant said, “I learned that as staff and faculty, we may be the ones to first notice changes in academic performance/behavior and may be the first people to reach out to the student who is struggling.” As an example of empathy, one participant stated, “My understanding of possible root causes has changed my perception on people having troubles.” Of note, participants expressed that student perception and the COVID-19 pandemic and transitioning to a virtual environment are perceived barriers to addressing student mental health concerns that require unique approaches. For instance, many participants expressed concern about the student’s response if they reached out about a personal matter, with some worried that reaching out could be perceived as intrusive by students. Additionally, participants explained that their busy schedules, heavy workloads, and their own personal issues or mental health concerns make it challenging to assist students. An example of a unique solution and expression of responsibility, “Moving into the virtual teaching environments, I will more closely monitor the student analytics and reach out from a place of compassion and care to check in on students more frequently who are falling behind in course material.”
Regarding the perceived quality of the program content and delivery, sub-themes included the overall importance of the program, most beneficial aspects of the program related to content and delivery, and suggested improvements related to logistics and content. Most participants expressed the importance of the program, indicating the most beneficial aspects being the evidence-based approach, case studies, institution-specific information, and small-group workshops. Regarding delivery, participants liked the flexibility (i.e., asynchronous e-modules, multiple workshops) and accessibility (i.e., closed captioning, transcripts, and audio recordings), and story-telling format using characters and dialogue between them. To improve logistics, participants suggested a more streamlined process for accessing modules, workshops, and completing surveys (i.e., as multiple platforms were used, as available in the institution) as well as shorter surveys and modules, and hard-copies of reference materials. To improve content, participants requested more case scenarios reflecting particularly difficult situations (e.g., violent behavior, large lecture classrooms) and diverse student populations (e.g., graduate students, international students, clinical health sciences students or internships). Some suggested targeted versions of the program, in keeping with their specific roles (i.e., to scale up or scale down certain topics for certain roles, such as for teaching assistants).
Lastly, many participants expressed desire for further mental health training and support (beyond these modules) as well as additional support from the institution and community such as making the e-modules mandatory training, greater allocation of resources to mental health, and improving mental health policy and advocacy. For example:
“If this type of training is not supported by the university for staff/faculty at many levels then we will continue to underserve our student population. Given the number of students experiencing mental health concerns I honestly do not think that we can afford to not offer this type of training to more people. I realize that the workshops may not be feasible, but I am hopeful that the […] training may one day become mandatory.”
Discussion
The Professor Hippo-on-Campus: Student Mental Health Education Program for Educators and Navigators is a novel, brief, virtual asynchronous and synchronous mental health literacy training program created specifically to meet the needs of student-facing post-secondary faculty and staff. The program, including content and design, was rigorously co-developed with various stakeholders and experts. This program is a unique mental health literacy curriculum in that it focuses specifically on the post-secondary setting and students, addresses social determinants of mental health, and the broader spectrum of mental health and wellbeing, beyond mental illness.
In this study, participation in Professor Hippo-on-Campus resulted in large, meaningful increases in faculty and staff confidence in identifying and responding to students experiencing distress, difficulty, or mental health problems particularly. Participation also led to small, significant improvements in stigma, attitudes, and knowledge. The synchronous workshops appear to offer added perceived value but are not essential to many of the changes in target outcomes. Participants were highly satisfied with the program and felt that their participation led to changes in their knowledge, attitudes, and intended behavior. A large majority (94%) felt the program should be mandatory for all faculty and staff at the university. Globally, faculty often report a lack of formal mental health training and a desire for increased training that is brief, self-paced, and virtual.Citation7,Citation33,Citation34 Notably, faculty and staff often indicate wanting mental health training that helps not only to identify and appropriately respond to students in distress and difficulty, but also to proactively prevent these concerns.Citation7,Citation64 Professor Hippo-on-Campus appears to begin to address these demands and needs.
Despite the program being introduced at the onset of the pandemic when there were many competing priorities, it was feasible to recruit and engage significant numbers of faculty and student-facing university staff to participate in this non-mandatory student mental health training program and evaluation. The most effective recruitment strategy appeared to be letters and prompts to Deans and Associate Deans, supported by senior leaders at the university, to invite or tap members of their faculties to participate initially, which was then followed by others hearing about the program via word-of-mouth. The program proved to be acceptable to participants, as indicated by high levels of satisfaction in survey responses and relatively high post-module completion rate (60%), far exceeding prior completion rates of MHFA programs with post-secondary staff (26%).Citation65 Participants appeared to appreciate the program ‘certificate’ and digital badge provided, and some proudly referenced or displayed these on social media. Additionally, the word-of-mouth spread of the program, endorsement by individuals who participated and went on to become program ‘champions’, ongoing registration for the program, and requests for adaptations to the program for other sub-groups and target groups (e.g., teaching assistants, health science professional faculty and staff) are notable and suggest engagement and buy-in by faculty and staff, and the need and demand for this content and program.
The asynchronous virtual modules are most feasible to develop, offer, and maintain in an ongoing way, with the synchronous workshops being more time- and resource-intensive. Continued access to the e-modules and content after completion are provided, so participants can revisit and review materials (which may help with retention of benefits) and the modules can easily be updated as needed. However, despite requiring more resources, there is a strong appetite for scenario-based workshops as indicated by: (1) participants in the initial feasibility study strongly recommending in-person (synchronous) training; (2) two thirds of participants in the current pilot who completed e-modules only indicating a workshop would have been helpful; and (3) nearly half of participants choosing to participate in the voluntary workshop with almost all (97%) of those attending indicating they would recommend it to other staff and faculty. Additionally, there may be unmeasured benefits to workshop participation such as encouraging module completion in anticipation of workshops, building social networks and connections among faculty and staff, changing culture through workshops, and the capacity to engage in continuous quality improvement of curricula through informal feedback.
Given the enthusiastic response to the Professor Hippo-on-Campus program and in response to participant suggestions and the challenges of teaching and learning virtually and during the pandemic, a 30-minute additional module “Virtual Learning Environments - Lessons from COVID-19” was launched in October 2021, with a focus on the student perspective of learning during the pandemic, virtual teaching tips, and evidence-based self-care tips for faculty and staff during this time. A targeted 1-hour e-module and 2-hour workshop for Teaching Assistants has also been developed in Summer-Fall 2021 and is currently being offered and evaluated (Winter 2022). Discussions are ongoing regarding the development of additional modules and workshops to address mental health challenges facing specific faculties or groups of students, including health professional trainees and graduate students. Additionally, in the pandemic particularly, increased demand for post-secondary faculty and staff well-being and mental health resources and curricula has been observed, and will be important to address more comprehensively in future trainings.Citation64
Limitations
While there were apparent significant and meaningful short-term changes as a result of program participation, there are limitations to consider. This was an open, pragmatic, uncontrolled study; participants were not randomly selected to participate, which likely led to some selection bias and limits generalizability, as there was no comparison or control condition. Thus, the effect sizes may be underestimated due to ceiling effects suggested by high levels of knowledge and positive attitudes and low levels of stigma at baseline. The feasibility, acceptability, and positive impacts of the program in this effectiveness study merit up-scaling the evaluation to a larger cluster-randomized efficacy trial or comparing repeated campus-wide surveys pre- and post- widespread implementation of the program (for example, the institution regularly participates in the National College Health Assessment). However, additional efforts will be needed to increase post-survey completion, as missing data may bias results. Additionally, there were no long-term outcomes measured to capture maintenance of effects, or other outcomes measured, such as student experience of staff and faculty or referrals to on-campus services. There are similar limitations in the broader field of mental health literacy programs, where few studies report on actual behaviors (such as changes in rates of student help-seeking or referral to resources), changes in student-reported mental health, or changes in suicide rates. There are also challenges in measuring the efficacy of interventions like this, and a need for psychometrically sound measures of mental health literacy appropriate to the context and program. Despite these limitations, we are not aware of other mental health literacy or gatekeeper training programs at this time targeting university faculty and staff which have been subject to more rigorous study.
Conclusion
This novel program demonstrates feasibility, high levels of satisfaction, and potential to improve mental health literacy among large numbers of post-secondary faculty and staff with a brief intervention designed specifically for the post-secondary student population and environment. In the COVID-19 environment, given the growing popularity and adoption of virtual training, and the growing interest in and demand for mental health literacy training, the Professor Hippo-on-Campus program holds promise and would benefit from further application and study in colleges and universities.
Conflict of interest disclosure
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of Canada and received an exemption from the Hamilton Integrated Research Ethics Board.
Data availability statement
Researchers can request access to the data used in this study by emailing Catharine Munn [email protected]
Additional information
Funding
References
- Arria AM, Caldeira KM, Allen HK, Bugbee BA, Vincent KB, O’Grady KE. Prevalence and incidence of drug use among college students: an 8-year longitudinal analysis. Am J Drug Alcohol Abuse. 2017;43(6):711–718. doi:10.1080/00952990.2017.1310219.
- Auerbach RP, Alonso J, Axinn WG, et al. Mental disorders among college students in the World Health Organization world mental health surveys. Psychol Med. 2016;46(14):2955–2970. doi:10.1017/S0033291716001665.
- Blanco C, Okuda M, Wright C, et al. Mental health of college students and their non–college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Arch Gen Psychiatry. 2008;65(12):1429–1437. doi:10.1001/archpsyc.65.12.1429.
- Cvetkovski S, Reavley NJ, Jorm AF. The prevalence and correlates of psychological distress in Australian tertiary students compared to their community peers. Aust N Z J Psychiatry. 2012;46(5):457–467. doi:10.1177/0004867411435290.
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3–10. doi:10.1016/j.jadohealth.2009.08.008.
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi:10.1001/archpsyc.62.6.593.
- Lipson SK. The role of faculty in student mental health. 2021. https://marychristieinstitute.org/wp-content/uploads/2021/04/The-Role-of-Faculty-in-Student-Mental-Health.pdf. Accessed March 7, 2022.
- Arria AM, Caldeira KM, Vincent KB, Winick ER, Baron RA, O’Grady KE. Discontinuous college enrollment: associations with substance use and mental health. Psychiatr Serv. 2013;64(2):165–172. doi:10.1176/appi.ps.201200106.
- Breslau J, Lane M, Sampson N, Kessler RC. Mental disorders and subsequent educational attainment in a US national sample. J Psychiatr Res. 2008;42(9):708–716. doi:10.1016/j.jpsychires.2008.01.016.
- Gibb SJ, Fergusson DM, Horwood LJ. Burden of psychiatric disorder in young adulthood and life outcomes at age 30. Br J Psychiatry. 2010;197(2):122–127. doi:10.1192/bjp.bp.109.076570.
- Hunt J, Eisenberg D, Kilbourne AM. Consequences of receipt of a psychiatric diagnosis for completion of college. Psychiatr Serv. 2010;61(4):399–404. doi:10.1176/ps.2010.61.4.399.
- Kessler RC, Heeringa S, Lakoma MD, et al. Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. Am J Psychiatry. 2008;165(6):703–711. doi:10.1176/appi.ajp.2008.08010126.
- McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 2011;24(4):301–306. doi:10.1097/YCO.0b013e3283477a09.
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18-24, 1998-2005. J Stud Alcohol Drugs Suppl. 2009;(16):12–20. doi:10.15288/jsads.2009.s16.12.
- Schwartz AJ. College student suicide in the United States: 1990-1991 through 2003-2004. J Am Coll Health. 2006;54(6):341–352. doi:10.3200/JACH.54.6.341-352.
- Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev. 2009;66(5):522–541. doi:10.1177/1077558709335173.
- Eisenberg D, Hunt J, Speer N. Help seeking for mental health on college campuses: Review of evidence and next steps for research and practice. Harv Rev Psychiatry. 2012;20(4):222–232. doi:10.3109/10673229.2012.712839.
- Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatr Serv. 2008;59(4):392–399. doi:10.1176/ps.2008.59.4.392.
- Hunt JB, Eisenberg D, Lu L, Gathright M. Racial/ethnic disparities in mental health care utilization among US college students: applying the institution of medicine definition of health care disparities. Acad Psychiatry. 2015;39(5):520–526. doi:10.1007/s40596-014-0148-1.
- Lipson SK, Gaddis SM, Heinze J, Beck K, Eisenberg D. Variations in student mental health and treatment utilization across US colleges and universities. J Am Coll Health. 2015;63(6):388–396. doi:10.1080/07448481.2015.1040411.
- Lipson SK, Zhou S, Wagner IB, Beck K, Eisenberg D. Major differences: variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J College Stud Psychother. 2016;30(1):23–41. doi:10.1080/87568225.2016.1105657.
- Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: A global public-health challenge. Lancet. 2007;369(9569):1302–1313. doi:10.1016/S0140-6736(07)60368-7.
- Conley CS, Durlak JA, Dickson DA. An evaluative review of outcome research on universal mental health promotion and prevention programs for higher education students. J Am Coll Health. 2013;61(5):286–301. doi:10.1080/07448481.2013.802237.
- Conley CS, Durlak JA, Kirsch AC. A meta-analysis of universal mental health prevention programs for higher education students. Prev Sci. 2015;16(4):487–507. doi:10.1007/s11121-015-0543-1.
- Fernandez A, Howse E, Rubio-Valera M, et al. Setting-based interventions to promote mental health at the university: a systematic review. Int J Public Health. 2016;61(7):797–807. doi:10.1007/s00038-016-0846-4.
- Harrod CS, Goss CW, Stallones L, DiGuiseppi C. Interventions for primary prevention of suicide in university and other post‐secondary educational settings. Cochrane Database Syst Rev. 2014;10:CD009439. doi:10.1002/14651858.CD009439.pub2.
- Lo K, Gupta T, Keating JL. Interventions to promote mental health literacy in university students and their clinical educators: a systematic review of randomised control trials. Health Prof. Educ. 2018;4(3):161–175. doi:10.1016/j.hpe.2017.08.001.
- Reavley N, Jorm AF. Prevention and early intervention to improve mental health in higher education students: a review. Early Interv Psychiatry. 2010;4(2):132–142. doi:10.1111/j.1751-7893.2010.00167.x.
- El-Den S, Moles R, Choong H-J, O’Reilly C. Mental Health First Aid training and assessment among university students: a systematic review. J Am Pharm Assoc (2003). 2020;60(5):e81–e95. doi:10.1016/j.japh.2019.12.017.
- International Conference on Health Promoting Universities & Colleges (7th). Okanagan Charter: An International Charter for Health Promoting Universities and Colleges. Kelowna, BC; 2015. doi:10.14288/1.013275.
- Di Placito-De Rango ML. Situating the post-secondary instructor in a supportive role for the mental health and well-being of students. Int J Ment Health Addiction. 2018;16(2):284–290. doi:10.1007/s11469-017-9740-4.
- Di Placito-De Rango ML. Acknowledge the barriers to better the practices: support for student mental health in higher education. CJSoTL 2016;7(2):2. doi:10.5206/cjsotl-rcacea.2016.2.2.
- Gulliver A, Farrer L, Bennett K, et al. University staff experiences of students with mental health problems and their perceptions of staff training needs. J Ment Health. 2018;27(3):247–256. doi:10.1080/09638237.2018.1466042.
- Margrove KL, Gustowska M, Grove LS. Provision of support for psychological distress by university staff, and receptiveness to mental health training. J Furth High Educ. 2014;38(1):90–106. doi:10.1080/0309877X.2012.699518.
- Jaworska N, De Somma E, Fonseka B, Heck E, MacQueen GM. Mental health services for students at postsecondary institutions: a national survey. Can J Psychiatry. 2016;61(12):766–775. doi:10.1177/0706743716640752.
- Jorm AF. Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177(5):396–401. doi:10.1192/bjp.177.5.396.
- Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–243. doi:10.1037/a0025957.
- Jorm AF, Barney LJ, Christensen H, Highet NJ, Kelly CM, Kitchener BA. Research on mental health literacy: what we know and what we still need to know. Aust N Z J Psychiatry. 2006;40(1):3–5. doi:10.1080/j.1440-1614.2006.01734.x.
- Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present, and future. Can J Psychiatry. 2016;61(3):154–158. doi:10.1177/0706743715616609.
- Hadlaczky G, Hökby S, Mkrtchian A, Carli V, Wasserman D. Mental health first aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: a meta-analysis. Int Rev Psychiatry. 2014;26(4):467–475. doi:10.3109/09540261.2014.924910.
- Kutcher S, Bagnell A, Wei Y. Mental health literacy in secondary schools: a Canadian approach. Child Adolesc Psychiatr Clin N Am. 2015;24(2):233–244. doi:10.1016/j.chc.2014.11.007.
- Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of mental health first aid training: Effects on knowledge, stigma, and helping behaviour. PLoS One. 2018;13(5):e0197102. doi:10.1371/journal.pone.0197102.
- Ashoorian D, Albrecht KL, Baxter C, et al. Evaluation of mental health first aid skills in an Australian university population. Early Interv Psychiatry. 2019;13(5):1121–1128. doi:10.1111/eip.12742.
- Lipson SK, Speer N, Brunwasser S, Hahn E, Eisenberg D. Gatekeeper training and access to mental health care at universities and colleges. J Adolesc Health. 2014;55(5):612–619. doi:10.1016/j.jadohealth.2014.05.009.
- Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(S7):S26–S30. doi:10.5694/j.1326-5377.2007.tb01332.x.
- Holmes G, Clacy A, Hermens DF, Lagopoulos J. The long-term efficacy of suicide prevention gatekeeper training: a systematic review. Arch Suicide Res. 2021;25(2):177–207. doi:10.1080/13811118.2019.1690608.
- Isaac M, Elias B, Katz LY, et al. Gatekeeper training as a preventative intervention for suicide: a systematic review. Can J Psychiatry. 2009;54(4):260–268. doi:10.1177/070674370905400407.
- Lipson SK, Raifman J, Abelson S, Reisner SL. Gender minority mental health in the US: esults of a national survey on college campuses. Am J Prev Med. 2019;57(3):293–301. doi:10.1016/j.amepre.2019.04.025.
- McMaster University Student Affairs. Student mental health & well-being strategy. https://mentalhealthstrategy.mcmaster.ca/strategy/. Accessed March 7, 2022.
- Articulate 360. Storyline 360 [computer software]. https://articulate.com/360/storyline
- D2L. Brightspace [learning platform]. https://www.d2l.com/brightspace/
- McMaster University Student Affairs. Responding to students in distress or difficulty. The 5 R’s: Steps in helping a student in distress or difficulty. https://wellness.mcmaster.ca/app/uploads/2019/11/Responding-to-Student-in-DistressNov2019-final.pdf. Updated November 2019. Accessed March 7, 2022.
- Munn C, Fein A. Professor Hippo-on-Campus Final Report for eCampus Ontario: Evaluating the Effectiveness of an Online Mental Health Course on the Knowledge and Confidence to Act of Faculty and Staff in the Postsecondary Setting. Hamilton, ON: McMaster University; 2018.
- Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–222. doi:10.2307/3090197.
- O’Cathain A, Hoddinott P, Lewin S, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: Guidance for researchers. Pilot Feasibility Stud. 2015;1(1):1–13. doi:10.1186/s40814-015-0026-y.
- Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1. doi:10.1186/1471-2288-10-1.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88. doi:10.1186/s12913-017-2031-8.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85(11):867–872. doi:10.2471/blt.07.045120.
- Evans-Lacko S, Rose D, Little K, et al. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011;20(3):263–271. doi:10.1017/s2045796011000308.
- Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self-efficacy scale: construction and validation. Psychol Rep. 1982;51(2):663–671. doi:10.2466/pr0.1982.51.2.663.
- Clifton L, Clifton DA. The correlation between baseline score and post-intervention score, and its implications for statistical analysis. Trials 2019;20(1):43. doi:10.1186/s13063-018-3108-3.
- Luciani M, Campbell K, Orr E, et al. How to design a qualitative health research study. Part 2: data generation and analysis considerations. Prof Inferm. 2019;72(3):221–231. PMID: 31883573
- Percy WH, Kostere K, Kostere S. Generic qualitative research in psychology. Qual Rep. 2015;20(2):76–85. doi:10.46743/2160-3715/2015.2097.
- Brewster L, Jones E, Priestley M, Wilbraham SJ, Spanner L, Hughes G. Look after the staff and they would look after the students’ cultures of wellbeing and mental health in the university setting. J Furth High Ed. 2022:46(4):548–560. doi:10.1080/0309877X.2021.1986473.
- Carpini JA, Chandra J, Lin J, et al. Mental health first aid by Australian tertiary staff: application rates, modes, content, and outcomes. Early Interv Psychiatry. 2021;15(5):1234–1242. doi:10.1111/eip.13072.