Abstract
The study explored how common non-disclosure of suicidal ideation is in a sample of adult psychiatric inpatients (N = 171) plus associated patient characteristics. A large percentage (51.5%) withheld some information on suicidal ideation during admission. In multivariable analyses, correlates of non-disclosure included a diagnosis of emotionally unstable personality disorder, low satisfaction with stay, and symptoms of the suicide crisis syndrome. In univariate analyses, therapists’ emotional response to the patient was also a correlate. Findings indicate that among acute psychiatric inpatients, non-disclosure of suicidal ideation is quite common, requiring awareness from clinicians relying on this parameter in suicide risk assessments.
Suicidal ideation (SI) has been associated with an increased risk of suicide attempts (Bebbington et al., Citation2010), as well as actual suicide (Hubers et al., Citation2018). Questions concerning SI are often prominent aspects of clinicians’ suicide risk assessments (American Psychiatric Association, Citation2003; Bolton et al., Citation2015; Norwegian Directorate of Health and Social Affairs, Citation2008). Many patients who later died by suicide, however, denied SI when last questioned by a clinician (Berman, Citation2018). Although some people who attempt suicide may not experience SI until minutes prior to the attempt (Deisenhammer et al., Citation2009), others have SI but withhold this information from health care professionals (Richards et al., Citation2019). Recent research has described reasons why SI might remain undisclosed, such as fear of hospitalization or feelings of shame (Blanchard & Farber, Citation2020; Fulginiti & Frey, Citation2019; Richards et al., Citation2019). Consequently, the question of how common such non-disclosure of SI is, especially among those at high risk for suicide, is gaining attention.
The population of adult psychiatric patients in need of admission has a greatly elevated suicide risk (Hjorthøj et al., Citation2014). To the extent that suicide risk assessments focus upon patient-reported SI, such assessments are dependent upon the patients’ accurate and honest self-disclosure of any SI they may be experiencing.
An increasing number of studies have reported prevalence rates of non-disclosure of SI within different populations, e.g., students (Drum et al., Citation2009; Eskin et al., Citation2015) and the general community (Calear & Batterham, Citation2019; Husky et al., Citation2016). Studies have explored disclosure or non-disclosure of SI among mental health patients in non-hospital settings (Blanchard & Farber, Citation2020; Cukrowicz et al., Citation2014; Fulginiti & Frey, Citation2019; Fulginiti et al., Citation2016; Orf, Citation2014; Way et al., Citation2013). Among prisoners receiving mental health care in a correctional facilities outpatient clinic (Way et al., Citation2013), 42% stated they were not likely to report SI. Among current or former patients in psychotherapy (Blanchard & Farber, Citation2016), 31% indicated having not been honest about their suicidal thoughts. Among patients 60 years and older and diagnosed with depression who acknowledged SI during the past month, only 50% reported having shared that information with a health care professional (Cukrowicz et al., Citation2014).
To our knowledge, there are few published studies on non-disclosure of SI in inpatient psychiatric settings. Much that has been published does not address our specific research question and is many decades old (e.g., Fowler et al., Citation1979; Wolk‐Wasserman, Citation1986). The primary aim of this study, therefore, is to describe the rates of non-disclosure of SI in a sample of adult inpatients admitted to an acute psychiatric department.
The secondary aim is to explore patient factors associated with non-disclosure. Previous studies in the general population have reported demographic and clinical correlates of non-disclosure, including male sex, older age, poor social connectedness, and lower level of education (Husky et al., Citation2016). Among patients with depression, lower quality of life and previous psychiatric treatment were associated with a higher probability of disclosure (Cukrowicz et al., Citation2014). The severity of psychiatric symptoms has both shown no association to intent to disclose SI (Fulginiti et al., Citation2016) and a positive association with disclosure among persons who later died from suicide (Zhou & Jia, Citation2012). We investigated the association between non-disclosure of SI and the possible correlates of age, sex, satisfaction with inpatient stay, as well as with two novel suicide-specific risk parameters, the suicide crisis syndrome (Galynker, Citation2017) and therapist emotional response (Galynker, Citation2017).
The suicide crisis syndrome is an acute, hyper-aroused, negative affect state, primarily characterized by feelings of entrapment, and hypothesized to precede suicidal attempts. Loss of cognitive control, involving intense rumination and repeated but unsuccessful attempts to suppress negative thoughts, is also prominent. Together, these symptoms are posited to leave the patient with the perception that suicide provides the only means of escape from an intolerable situation. Indeed, past studies have shown the suicide crisis syndrome to be associated with an increased risk of suicidal behavior in psychiatric patient’s post-discharge (Yaseen et al., Citation2019).
Therapist emotional response pertains to clinicians’ emotional response to the patient and represents a novel tool in the assessment of imminent suicide risk. The informative nature of clinicians’ emotional responses to patients as part of suicide risk assessments have been indicated by past research and negative emotional responses on the part of the therapist have been associated with patients’ near-term suicidal behaviors (Barzilay et al., Citation2018). The fact that neither construct is reliant on SI in providing suicide risk estimates makes them especially relevant for the present study. To the extent that non-disclosure of SI is a significant barrier to appropriate care, it is important to investigate the relationship between predictors of suicide risk that do not rely on SI and SI non-disclosure. To our knowledge, the relationship between the suicide crisis syndrome, therapists’ emotional response to patients and non-disclosure of SI has not yet been addressed.
Method
The present cross-sectional study was part of a larger, prospective cohort study exploring multiple predictors of affective impulsivity in acute psychiatric inpatients conducted between January 2016 and June 2017 in the acute psychiatric emergency unit at the St. Olavs Hospital, Trondheim University Hospital, Norway. The acute psychiatric emergency unit is a locked-door unit and had, during the inclusion period, 40 beds. This unit receives voluntary and involuntary admissions 24 hours per day (Hustoft et al., Citation2018). The patients admitted are characterized by severe clinical conditions and are often in need of acute psychopharmacological treatment, detoxification, and/or supervision. There are no other units of this kind in the catchment area. Hospital staff are available 24/7 and all patients are assigned a primary nursing staff contact person for each shift. A psychiatrist or clinical psychologist is responsible for the treatment throughout admission.
Participants
During the study period, 1,231 patients were admitted to the acute units and 347 included in the larger prospective cohort study. Participation in the research project was voluntary and required written informed consent. The study exclusion criterion was if a psychiatrist or clinical psychologist assessed the patient as being unable to provide informed consent. As many as 33% of admissions to the units have a duration of less than 2 days (data from 2016). This represents a possible explanation for the small number of patients included in the larger prospective study compared to the total patient population.
The sample for the current study included 171 patients who provided answers about non-disclosure of SI. The non-disclosure item, specifically, was answered at discharge as part of a larger evaluation form. Discharges often occurred at short notice and during times of peak activity for hospital staff. This might have led to fewer patients answering the non-disclosure item and might explain the reduced sample size for the present study compared to the larger prospective cohort study.
shows the demographic and clinical characteristics of the study sample. The distributions of age and sex in this study sample were similar to the patients from the larger cohort study.
Table 1 Demographic and clinical description of study sample (N = 171).
Measures
The non-disclosure item was: “Did you have thoughts about hurting yourself or ending your own life without telling it to a nurse or clinician?” answered on a 100 mm Visual Analog Scale (VAS) from not at all (0) to to a very large extent (100), with a higher score indicating higher degree of non-disclosure. Patients made an X-mark on the line, and research staff subsequently translated the X into a number using a ruler. To provide an indication of how many patients, categorically, reported non-disclosure of SI, a cutoff off ≥5 was used. The cutoff was chosen to reflect responders who marked their non-disclosure response at what was deemed to be a reliable distance from the 0-anchor (5 mm and beyond).
The Satisfaction with stay item was: “How satisfied are you with the help you received for your problems?” Answers were on a VAS scale from very dissatisfied (0) to very satisfied (100).
The Suicide Trigger Scale-Short Form (STS-SF; Calati et al., Citation2020; Hawes et al., Citation2017) is an eight-item scale addressing symptoms of the suicide crisis syndrome in terms of feelings of entrapment and somatic distress due to excessive thoughts. Answers are on a scale from 0 (not at all) to 4 (extremely). Patients completed the STS-SF as part of the initial assessment interview with a psychiatrist or clinical psychologist. Preliminary data screening showed that two items (addressing fear of dying) did not correlate well with the remaining scale items and were therefore not included in the STS-SF used in the analysis. The version of the STS-SF referred to in the remainder of this paper therefore included six items. Cronbach’s alpha for the six-item version of the STS-SF was satisfactory, α = .80.
Therapist Response Questionnaire-Short Form (TRQ-SF; Calati et al., Citation2020; Hawes et al., Citation2017) includes 10 statements about the therapist’s emotional responses upon meeting the patient and was completed after the initial clinical interview. Items were answered on a scale from 0 (not at all) to 4 (extremely), with the total score reflecting the degree of negative emotional response. Cronbach`s alpha for the TRQ-SF in this sample was .81. A sample item from the TRQ-SF is “I felt dismissed or devalued” (Calati et al., Citation2020).
Procedure
Demographic information used for this study was collected on admission as part of a larger research intake protocol by the physician on duty, who also performed a suicide risk assessment for each patient. A second suicide risk assessment was performed by a psychiatrist or clinical psychologist within 24-hours of intake. The STS-SF and therapist emotional response measures were also administered within 24-hours of admission. The TRQ-SF was predominantly (93%) completed by a psychiatrist or clinical psychologist, and the remaining questionnaires by either a physician, psychologist, or psychiatrist-in-training (rater data missing for three TRQ-SF records). Information on any SI or behavior at the time of intake or within the last month prior to admission was collected from intake medical charts based on definitions of suicidal thoughts and behavior in the Columbia- Suicide Severity Rating Scale (C-SSRS; Posner et al., Citation2011). SI was measured as a yes/no item and suicidal behavior was coded according to the definitions of different types of behavior provided by the C-SSRS (Posner et al., Citation2011). We collapsed the suicide variable into a dichotomous variable reflecting the presence or absence. Information on duration of stay and voluntary or involuntary referral status came from medical charts. Diagnoses were reached at assessment meetings held twice a week with a minimum of two psychiatrists or clinical psychologists present and were based on ICD-10 (World Health Organization (WHO), Citation1993). The regional ethical committee approved this research project (reference number 9565).
Results
The median non-disclosure score was 5.0 (Interquartile range [IQR] = 46.7), the mean was 23.79 (SD = 31.05), and 51.5% (n = 88) had scores at 5 or above. Among patients scoring 0-4 (n = 83), 63.9% (n = 53) had medical charts reporting SI at time of admission or within the last month prior to admission and 14.3% (n = 11; 6 missing scores for suicidal behavior) had suicidal behavior during the same period. Among patients scoring 5 or above, 81.6% (n = 71; 1 missing score for SI) had medical charts reporting SI and 21.8% (n = 19; one missing score for suicidal behavior) had suicidal behavior. Chi-square test indicated a significant difference between the two groups for SI, χ2 (1, n = 170) = 6.78, p =.010 (Exact sig), Phi =.20, Exact sig =.010, but not for suicidal behavior.
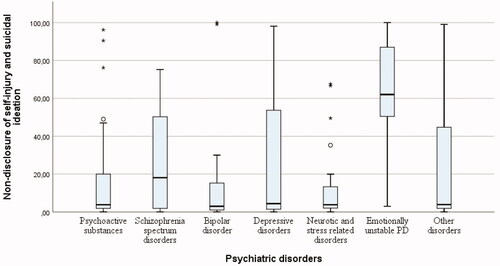
Non-disclosure was significantly correlated with age (rs = −.199, p = .009). Women (Md = 12.4, IQR = 60.0; Mann–Whitney U = 2879.5, z = −2.36, p = .018) and men (Md = 3.9, IQR = 23.3) differed significantly in non-disclosure. shows boxplots with the median non-disclosure scores according to primary diagnosis. Between-group analysis by Kruskal-Wallis test demonstrated a significant overall difference on non-disclosure between primary diagnoses, H(6) = 18.21, p =.006. Pairwise comparisons indicated that inpatients diagnosed with emotionally unstable personality disorder (EUPD; F60.3 in ICD-10) reported significantly higher non-disclosure than those with psychoactive substance use (Adjusted p = .010), bipolar disorder (Adjusted p = .002), depressive disorders (Adjusted p = .017), anxiety and stress related disorders (Adjusted p = .007), and other disorders (Adjusted p = .014). No significant difference was found between patients diagnosed with EUPD and schizophrenia spectrum disorders (Adjusted p = .432). None of the other disorders (including schizophrenia spectrum disorders) differed significantly from one another.
Figure 1. Graphical display of non-disclosure scores according to diagnostic categories.
Note: Box-plots displaying median (Md), inter-quartile range (IQR), upper-and lower 25% of scores; outliers and extreme scores. Psychoactive substances (n = 23) Md = 3.8 (IQR = 23.1); Schizophrenia spectrum disorders (n = 11) = 18.1 (52.0); Bipolar disorder (n = 25) = 3.0 (15.7); Depressive disorders (n = 40) = 4.4 (53.2); Neurotic, stress-related and somatoform disorders (n = 25) = 3.8 (14.7); Emotionally unstable personality disorder (n = 13) = 62.0 (42.2); “Other” disorders (n = 34) = 3.9 (43.8).
Non-disclosure was also significantly correlated with satisfaction with stay, rs = −.187, p =.014, STS-SF, rs =.206, p = .008, and TRQ-SF, rs = .194, p = .016. In other words, higher levels of non-disclosure were associated with younger age, female sex, less satisfaction with the inpatient stay, more intense symptoms of the suicide crisis syndrome, and eliciting a more negative emotional response from one’s clinician. All aforementioned variables were included in the multiple regression analysis, as well as diagnosis of EUPD, as univariate analyses identified it as a significant correlate of non-disclosure of SI.
presents the results of the regression analysis on log-transformed continuous non-disclosure scores. The adjusted R2 of the model was .25. Satisfaction with inpatient stay, EUPD, and STS-SF were each independently associated with non-disclosure of SI. Patient age, sex, and TRQ-SF score did not reach significance.
Table 2. Multiple linear regression analysis of patient factors on non-disclosure of suicidal ideation (N = 151).
Discussion
Findings from this study indicated that non-disclosure of SI was quite common in a sample of acute psychiatric patients, and that distinct patient characteristics are associated with non-disclosure. It has been pointed out that the question of disclosure versus non-disclosure of SI might be more complex than what is captured by a yes/no answer (Hom et al., Citation2017). Allowing patients to report on a continuous scale, such as the one used for this study, may have resulted in a more clinically valid picture of the extent patients perceive they are letting clinicians “in on” their experience of current SI.
Half of the patients surveyed in this study (51.5%) reported non-disclosure of SI (score ≥5). In terms of observed rates of non-disclosure, a comparison of the current findings with past rates is complicated by the use of different measures. However, the rates of non-disclosure reported in this study are higher than previously reported in a study that asked prison inmates receiving psychiatric treatment to indicate the likelihood of non-disclosure (42% and 31%; Way et al., Citation2013). Present rates are comparable to the rates presented among patients with depression at about 50% (Cukrowicz et al., Citation2014).
Possible explanations for the high rates reported among the patients in this study cannot be gleaned directly from the data but may be suggested by prior research and literature. Prior studies on non-disclosure or concealment in therapy settings have demonstrated the importance of shame as a reason for non-disclosure of symptoms of depression (Hook & Andrews, Citation2005) and SI (Blanchard & Farber, Citation2020). Similarly, feelings of shame concerning SI might have contributed to the observed rates. Fear of being hospitalized has also been cited as a reason for non-disclosure of SI in psychotherapy (Blanchard & Farber, Citation2020). Among psychiatric inpatients in this study, fear of not being discharged or of a delay in the discharge process might be a possible explanation why patients chose not to disclose SI. As the non-disclosure item did not distinguish between SI and non-suicidal self-harm, this might also have increased the rates of reported non-disclosure when comparing with studies asking about disclosure of SI only. Concerning therapist related factors, Quinnett (Citation2019) argued that therapist factors such as fear of a confirmative answer about SI and the language used by clinicians implicitly eliminates or limits the extent to which patients elaborate about SI. The Quinnett (Citation2019) arguments regarding the impact of language builds on prior research showing clinicians’ excessive use of closed- and negatively worded questions when asking about SI (e.g., McCabe et al., Citation2017) and how seldom SI was discussed in clinical encounters (Vannoy & Robins, Citation2011).
In the current study, non-disclosure was reported across all psychiatric disorders. The highest median non-disclosure scores were reported by patients diagnosed with EUPD. Patients diagnosed with bipolar disorder, anxiety and stress-related disorders (F40–48), and disorders due to psychoactive substances reported the lowest median scores. In a study from the general population in France, the presence of certain disorders (depression, certain anxiety disorders, and drug dependence), having several disorders, and suicidal behavior, were associated with higher probability of disclosing SI to both family or friends and health care professionals (Husky et al., Citation2016). This corresponds to the finding from the present study showing low non-disclosure scores among persons with substance abuse disorders and anxiety disorders.
In univariate analyses, we found associations between higher non-disclosure and younger age, female sex, and lower satisfaction with the help received during the admission. The results also showed associations between higher non-disclosure scores and more negative emotional responses from therapists as well as more severe suicide crisis symptoms. Multiple regression analysis demonstrated that having a primary or secondary diagnosis of EUPD, low satisfaction with help received during the stay, and symptoms of the suicide crisis syndrome were individually associated with non-disclosure.
Among characteristics associated with non-disclosure, having a diagnosis of EUPD, the diagnostic category in ICD-10 corresponding to borderline personality disorder, appeared in the forefront. Clinical characteristics of EUPD in combination with the context of this study (an inpatient psychiatric acute emergency unit) might provide some insights for these findings. Suicidality and self-injury are frequent among patients with a diagnosis of borderline personality disorder (Black et al., Citation2004). In terms of unplanned admissions to acute psychiatric units, suicidal behavior might be the reason why these patients are referred to admission. Moreover, the topics which patients choose not to disclose can relate to symptoms central to their disorder, as indicated by a finding showing that 42% of patients treated for depression reported non-disclosure of information related to their depression (Hook & Andrews, Citation2005). To the extent that this applies to other disorders, because suicidality might be so prevalent among psychiatric inpatients diagnosed with EUPD, this might have increased the probability of information on SI not being disclosed. Furthermore, such patients are hypersensitive to perceived rejection or invalidation (Linehan, Citation1993), and such feelings might have occurred during the stay, undermining open self-disclosure to staff.
Satisfaction with the help one had received during the admission was also associated with non-disclosure. Reporting less satisfaction might have reflected a lack of therapeutic alliance with members of the hospital staff and/or clinicians. In line with this, a past study has shown a positive association between disclosure of SI and working alliance (Orf, Citation2014).
Another interesting finding is that the greater severity of suicide crisis symptoms was associated with non-disclosure of SI. Prior research demonstrated how an acute psychiatric state, with clinical elements seemingly corresponding to the suicide crisis state, affected patients’ ability to recognize thoughts related to ending their life while in the acute state. The recognition of having experienced SI came only afterward, as the patient recovered (Fredriksen et al., Citation2017). This might also have been the case for the patients in the present study, with the intensity and severity of SI experienced during admission becoming more apparent as they approached discharge and thus, recovery. A second possible explanation for the finding on suicidal crisis symptoms and non-disclosure concerns the main characteristic of entrapment. For patients already experiencing intense feelings of entrapment, commitment in a locked ward could exacerbate these feelings, providing strong disincentive to disclose SI and thereby possibly delay discharge. A third explanation pertains to the previously established association between the suicide crisis state and future suicidal behavior (Yaseen et al., Citation2019). Patients may have withheld information on their SI to prevent staff from interfering with any suicidal plans they might have had (Simon & Gutheil, Citation2009).
Consistent with our finding in univariate analyses that therapist emotional response to patients correlated with non-disclosure, prior research has demonstrated that the way clinicians asked about SI (i.e., in a “biased” or “awkward” manner) was negatively associated with disclosure of SI (Orf, Citation2014). Despite reaching significance in univariate analysis, the association between therapist negative emotional responses and non-disclosure did not retain significance in multivariable analyses. This was surprising and not consistent with prior research showing a relationship between therapist response and other suicide parameters, such as suicidal risk (Calati et al., Citation2020) and clinical decision making (Barzilay et al., Citation2019). There may be several reasons for this. First, prior research has documented a relationship between personality disorders and therapist countertransference (Michaud et al., Citation2020). As a diagnosis of EUPD had a strong relationship to SI non-disclosure, it might have masked the impact of therapist emotional response on non-disclosure. Future research could examine this in more detail; however, the small cell size of EUPD in our sample limited such analyses in this study. Second, there may be differences across study sites in therapists’ comfort level in disclosing negative feelings toward their patients. Moreover, this study was conducted in a different country than was prior research on the TRQ-SF. Future research could explore the effect of clinician training on the sensitivity of the TRQ-SF to a wide range of suicide parameters, including non-disclosure.
This study has some notable strengths, perhaps the most prominent relating to the clinical inpatient setting where the study was conducted, representing initial exploration of non-disclosure of SI among severely ill psychiatric inpatients. However, some limitations should be mentioned. One limitation concerns the inability to identify whether patients denied SI when asked (Cukrowicz et al., Citation2014) or whether they failed to communicate SI spontaneously as the thoughts appeared throughout the admission. It remains unknown to what extent the patients may have disclosed SI at one-point and not disclosed at another point during the stay. The inherent difference between non-disclosure and concealment is worth addressing in this regard. Non-disclosure pertains to something simply not communicated, and concealment pertains to efforts of keeping something hidden (Frey et al., Citation2020). This distinction is subtle, but important. In the present study, we cannot determine the proportion of responses that may have referred to concealment; that is, active efforts to keep the SI from clinicians or staff. Also, as the non-disclosure item referred to both SI and non-suicidal, self-harm, it is not possible to determine the types of self-harm the patients had in mind when providing their answer. The lack of a control group (e.g., an outpatient control group) to assess whether the reported non-disclosure scores are specific to psychiatric inpatients, also constitutes a limitation. Finally, the relatively small sample size reduced the sensitivity to the effects of variables with relatively low cell sizes. Another important limitation is that non-disclosure and satisfaction were only one item each.
Findings from the present study indicate that among inpatients at an acute psychiatric emergency unit, withholding information on SI is quite common and observed across psychiatric disorders. Implications include a necessary awareness among clinicians and staff working at such units of the relative frequency of non-disclosure of SI in this patient population and the inherent limitations of relying on self-disclosed SI as a substantial part of the suicide risk assessment. Furthermore, in exploring the presence of SI, we recommend that clinicians attend to their manner of assessing suicidal risk, such as using open-ended rather than close-ended questions and using follow-up probes when high-risk patients such as those with EUPD deny SI, to ensure fuller self-disclosure by their patients (McCabe et al., Citation2017; Vannoy & Robins, Citation2011). Further, clinicians should be mindful of patients’ potential fears related to disclosing SI (Richards et al., Citation2019). Finally, the high rates of non-disclosure demonstrated in this study support previous recommendations of broadening the scope of suicide risk assessments from screenings of SI to more state-dependent assessment procedures (e.g., Simon Citation2008), such as those assessing the suicide crisis syndrome. Given the limited research on non-disclosure of SI among psychiatric inpatients, future studies should continue to explore the rates of this phenomenon, and also seek to further elucidate the nature of non-disclosure (i.e., non-disclosure vs. concealment) as well as the reasons behind this lack of communication, as seen from the perspective of the patients.
Acknowledgements
Authors thank psychologist Kåre Sivertsen for discussions in preparation for this paper, and Kjetil Sørensen and Kamilla Medås for data collection.
Additional information
Funding
References
- American Psychiatric Association. (2003). Practice guideline for the assessment and treatment of patients with suicidal behaviors. American Psychiatric Association. https://psychiatryonline.org/guidelines
- Barzilay, S., Yaseen, Z. S., Hawes, M., Gorman, B., Altman, R., Foster, A., Apter, A., Rosenfield, P., & Galynker, I. (2018). Emotional responses to suicidal patients: Factor structure, construct, and predictive validity of the Therapist Response Questionnaire-Suicide Form. Frontiers in Psychiatry, 9, 104. https://doi.org/https://doi.org/10.3389/fpsyt.2018.00104
- Barzilay, S., Yaseen, Z. S., Hawes, M., Kopeykina, I., Ardalan, F., Rosenfield, P., Murrough, J., & Galynker, I. (2019). Determinants and predictive value of clinician assessment of short-term suicide risk. Suicide and Life-Threatening Behavior, 49(2), 614–626. https://doi.org/https://doi.org/10.1111/sltb.12462
- Bebbington, P. E., Minot, S., Cooper, C., Dennis, M., Meltzer, H., Jenkins, R., & Brugha, T. (2010). Suicidal ideation, self-harm and attempted suicide: Results from the British psychiatric morbidity survey 2000. European Psychiatry, 25(7), 427–431. https://doi.org/https://doi.org/10.1016/j.eurpsy.2009.12.004
- Berman, A. L. (2018). Risk factors proximate to suicide and suicide risk assessment in the context of denied suicide ideation. Suicide and Life-Threatening Behavior, 48(3), 340–352. https://doi.org/https://doi.org/10.1111/sltb.12351
- Black, D. W., Blum, N., Pfohl, B., & Hale, N. (2004). Suicidal behavior in borderline personality disorder: Prevalence, risk factors, prediction, and prevention. Journal of Personality Disorders, 18(3), 226–239. https://doi.org/https://doi.org/10.1521/pedi.18.3.226.35445
- Blanchard, M., & Farber, B. A. (2016). Lying in psychotherapy: Why and what clients don’t tell their therapist about therapy and their relationship. Counselling Psychology Quarterly, 29(1), 90–112. https://doi.org/https://doi.org/10.1080/09515070.2015.1085365
- Blanchard, M., & Farber, B. A. (2020). "It is never okay to talk about suicide": Patients' reasons for concealing suicidal ideation in psychotherapy. Psychotherapy Research, 30(1), 124–136. https://doi.org/https://doi.org/10.1080/10503307.2018.1543977
- Bolton, J. M., Gunnell, D., & Turecki, G. (2015). Suicide risk assessment and intervention in people with mental illness. BMJ (Clinical Research Edition), 351, h4978 https://doi.org/https://doi.org/10.1136/bmj.h4978
- Calati, R., Cohen, L. J., Schuck, A., Levy, D., Bloch-Elkouby, S., Barzilay, S., Rosenfield, P. J., & Galynker, I. (2020). The Modular Assessment of Risk for Imminent Suicide (MARIS): A validation study of a novel tool for suicide risk assessment. Journal of Affective Disorders, 263, 121–128. https://doi.org/https://doi.org/10.1016/j.jad.2019.12.001
- Calear, A. L., & Batterham, P. J. (2019). Suicidal ideation disclosure: Patterns, correlates and outcome. Psychiatry Research, 278, 1–6. https://doi.org/https://doi.org/10.1016/j.psychres.2019.05.024
- Cukrowicz, K. C., Duberstein, P. R., Vannoy, S. D., Lin, E. H., & Unützer, J. (2014). What factors determine disclosure of suicide ideation in adults 60 and older to a treatment provider? Suicide Life Threat Behav, 44(3), 331–337. https://doi.org/https://doi.org/10.1111/sltb.12075
- Deisenhammer, E. A., Ing, C.- M., Strauss, R., Kemmler, G., Hinterhuber, H., & Weiss, E. M. (2009). The duration of the suicidal process: how much time is left for intervention between consideration and accomplishment of a suicide attempt? The Journal of Clinical Psychiatry, 70(1), 19–24. https://doi.org/https://doi.org/10.4088/JCP.07m03904
- Drum, D. J., Brownson, C., Burton Denmark, A., & Smith, S. E. (2009). New data on the nature of suicidal crises in college students: Shifting the paradigm. Professional Psychology: Research and Practice, 40(3), 213–222. https://doi.org/https://doi.org/10.1037/a0014465
- Eskin, M., Schild, A., Öncü, B., Stieger, S., & Voracek, M. (2015). A cross-cultural investigation of suicidal disclosures and attitudes in Austrian and Turkish university students. Death Studies, 39(10), 584–591. https://doi.org/https://doi.org/10.1080/07481187.2015.1037971
- Fowler, R. C., Tsuang, M. T., & Kronfol, Z. (1979). Communication of suicidal intent and suicide in unipolar depression: A forty year follow-up. Journal of Affective Disorders, 1(3), 219–225. https://doi.org/https://doi.org/10.1016/0165-0327(79)90007-7
- Fredriksen, K. J., Schoeyen, H. K., Johannessen, J. O., Walby, F. A., Davidson, L., & Schaufel, M. A. (2017). Psychotic depression and suicidal behavior. Psychiatry, 80(1), 17–29. https://doi.org/https://doi.org/10.1080/00332747.2016.1208002
- Frey, L. M., Fulginiti, A., Sheehan, L., Oexle, N., Stage, D. L., & Stohlmann-Rainey, J. (2020). What`s in a word? Clarifying terminology on suicide. Death Studies, 44(12), 808–818. https://doi.org/https://doi.org/10.1080/07481187.2019.1614111
- Fulginiti, A., & Frey, L. M. (2019). Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Studies, 43(9), 562–569. https://doi.org/https://doi.org/10.1080/07481187.2018.1504349
- Fulginiti, A., Pahwa, R., Frey, L. M., Rice, E., & Brekke, J. S. (2016). What factors influence the decision to share suicidal thoughts? A multilevel social network analysis of disclosure among individuals with serious mental illness. Suicide and Life-Threatening Behavior, 46(4), 398–412. https://doi.org/https://doi.org/10.1111/sltb.12224
- Galynker, I. (2017). The suicidal crisis: Clinical guide to the assessment of imminent suicide risk. Oxford University Press.
- Hawes, M., Yaseen, Z., Briggs, J., & Galynker, I. (2017). The Modular Assessment of Risk for Imminent Suicide (MARIS): A proof of concept for a multi-informant tool for evaluation of short-term suicide risk. Comprehensive Psychiatry, 72, 88–96. https://doi.org/https://doi.org/10.1016/j.comppsych.2016.10.002
- Hjorthøj, C. R., Madsen, T., Agerbo, E., & Nordentoft, M. (2014). Risk of suicide according to level of psychiatric treatment: A nationwide nested case-control study. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1357–1365. https://doi.org/https://doi.org/10.1007/s00127-014-0860-x
- Hom, M. A., Stanley, I. H., Podlogar, M. C., & Joiner, T. E. Jr., (2017). “Are you having thoughts of suicide?" Examining experiences with disclosing and denying suicidal ideation. Journal of Clinical Psychology, 73(10), 1382–1392. https://doi.org/https://doi.org/10.1002/jclp.22440
- Hook, A., & Andrews, B. (2005). The relationship of non-disclosure in therapy to shame and depression. British Journal of Clinical Psychology, 44(3), 425–438. https://doi.org/https://doi.org/10.1348/014466505X34165
- Hubers, A. A. M., Moaddine, S., Peersmann, S. H. M., Stijnen, T., van Duijn, E., van der Mast, R. C., Dekkers, O. M., & Giltay, E. J. (2018). Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: A meta-analysis. Epidemiology and Psychiatric Sciences, 27(2), 186–198. https://doi.org/https://doi.org/10.1017/S2045796016001049
- Husky, M. M., Zablith, I., Fernandez, V. A., & Kovess-Masfety, V. (2016). Factors associated with suicidal ideation disclosure: Results from a large population-based study. Journal of Affective Disorders, 205, 36–43. https://doi.org/https://doi.org/10.1016/j.jad.2016.06.054
- Hustoft, K., Larsen, T. K., Brønnick, K., Joa, I., Johannessen, J. O., & Ruud, T. (2018). Voluntary or involuntary acute psychiatric hospitalization in Norway: A 24h follow up study. International Journal of Law and Psychiatry, 56, 27–34. https://doi.org/https://doi.org/10.1016/j.ijlp.2017.10.011
- Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. The Guilford Press.
- McCabe, R., Sterno, I., Priebe, S., Barnes, R., & Byng, R. (2017). How do healthcare professionals interview patients to assess suicide risk? BMC Psychiatry, 17(1), 122 https://doi.org/https://doi.org/10.1186/s12888-017-1212-7
- Michaud, L., Ligier, F., Bourquin, C., Corbeil, S., Saraga, M., Stiefel, F., Séguin, M., Turecki, G., & Richard-Devantoy, S. (2020). Differences and similarities in instant countertransference towards patients with suicidal ideation and personality disorders. Journal of Affective Disorders, 265, 669–678. https://doi.org/https://doi.org/10.1016/j.jad.2019.11.115
- Norwegian Directorate of Health and Social Affairs (2008). National guidelines for the prevention of suicide in mental health care. The Norwegian Directorate of Health and Social Affairs.
- Orf, R. W. (2014). Factors that promote and inhibit client disclosure of suicidal ideation [Doctoral dissertation, Antioch University]. https://aura.antioch.edu/etds/191
- Posner, K., Brown, G. K., Stanley, B., Brent, D. A., Yershova, K. V., Oquendo, M. A., Currier, G. W., Melvin, G. A., Greenhill, L., Shen, S., & Mann, J. J. (2011). The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American Journal of Psychiatry, 168(12), 1266–1277. https://doi.org/https://doi.org/10.1176/appi.ajp.2011.10111704
- Quinnett, P. (2019). The role of clinician fear in interviewing suicidal patients. Crisis, 40(5), 355–359. https://doi.org/https://doi.org/10.1027/0227-5910/a000555
- Richards, J. E., Whiteside, U., Ludman, E. J., Pabiniak, C., Kirlin, B., Hidalgo, R., & Simon, G. (2019). Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: A qualitative study. Psychiatric Services, 70(1), 40–45. https://doi.org/https://doi.org/10.1176/appi.ps.201800342
- Simon, R. I. (2008). Behavioral risk assessment of the guarded suicidal patient. Suicide and Life-Threatening Behavior, 38(5), 517–522. https://doi.org/https://doi.org/10.1521/suli.2008.38.5.517
- Simon, R., & Gutheil, T. G. (2009). Sudden improvement among high-risk suicidal patients: Should it be trusted? Psychiatric Services, 60(3), 387–389. https://doi.org/https://doi.org/10.1176/ps.2009.60.3.387
- Vannoy, S. D., & Robins, L. S. (2011). Suicide-related discussions with depressed primary care patients in the USA: Gender and quality gaps. A mixed methods analysis. BMJ Open, 2, e000198.
- Way, B. B., Kaufman, A. R., Knoll, J. L., & Chlebowski, S. M. (2013). Suicidal ideation among inmate-patients in state prison: Prevalence, reluctance to report, and treatment preferences. Behavioral Sciences and the Law, 31(2), 230–238. https://doi.org/https://doi.org/10.1002/bsl.2055
- Wolk‐Wasserman, D. (1986). Suicidal communication of persons attempting suicide and responses of significant others. Acta Psychiatrica Scandinavica, 73, 481–499.
- World Health Organization (WHO) (1993). The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic criteria for research. World Health Organization.
- Yaseen, Z. S., Hawes, M., Barzilay, S., & Galynker, I. (2019). Predictive validity of proposed diagnostic criteria for the suicide crisis syndrome: an acute presuicidal state. Suicide and Life-Threatening Behavior, 49(4), 1124–1135. https://doi.org/https://doi.org/10.1111/sltb.12495
- Zhou, X. M., & Jia, S. H. (2012). Suicidal communication signifies suicidal intent in Chinese completed suicides. Social Psychiatry and Psychiatric Epidemiology, 47(11), 1845–1854. https://doi.org/https://doi.org/10.1007/s00127-012-0488-7
